Abstract
Improvements in outcomes for older adults sustaining burn injuries have lagged far behind those of younger patients. As this segment of the population grows, there has been an increasing interest in better understanding the epidemiology and outcomes of injury in older adults. The National Burn Repository (NBR) provides a unique opportunity to examine burn injuries on a national level. We aimed to characterize specific injury and outcome trends in older adult with burns through analysis of the NBR. We examined the records of all patients in the NBR aged 55 and older. To characterize age effects on injury and outcomes, patients were stratified into three age categories: 55 to 64 years, 65 to 74 years, and 75 years and older. Baseline characteristics, details of hospital treatment, mortality, and disposition were compared among these three age groups using χ2 or analysis of variance. Logistic regression analysis was performed to assess the impact of age on burn mortality. A total of 180,401 patient records were available from 1991 to 2005, of which 23,180 (14%) met age inclusion criteria. Mean burn size (9.6% TBSA) and percent with inhalation injury (11.3%) did not markedly differ by age. Men predominated overall (ratio 1.4:1), although women (4290) outnumbered men (3439) in the oldest age category. Length of stay per TBSA and median hospital charges increased with increasing age category, suggesting higher resource consumption with aging. Mean number of operations per patient, however, decreased with age. Mortality rates and discharge to nonindependent status increased with age. By logistic regression, the adjusted odds ratio for mortality was 2.3 (95% CI 2.1–2.7) in the 65 to 74 age group, and 5.4 (95% CI 4.8–6.1) in the oldest group when compared with the 55 to 64 age group. Mortality rates decreased significantly after 2001 across all age groups. This analysis demonstrates age-dependent differences in resource utilization and mortality risk within the older burn population and highlights the need for a national research agenda focused on management practices and outcomes in older adult with burns.
Advances in burn care over the past 50 years have brought about remarkable improvement in mortality rates such that survival has become an expected outcome even in patients with extensive injuries.1–4 Although these improvements have occurred in all age groups, survival in older adults still lags far behind that in younger cohorts.1,5–7 As this segment of the population grows, there has been an increasing interest in better understanding the epidemiology and outcomes of injury in older adults.
The majority of studies examining burn injury in older adults have been single-center studies1,6,8 –10. However, data from individual centers may not be generalizable to all older adults because of patient characteristics, injury patterns, and management strategies that may be unique to each center. In addition, the number of burn injuries in older adults treated at any single center may be small and therefore not allow meaningful analysis and the development of effective intervention strategies.
The National Burn Repository (NBR) was established by the American Burn Association (ABA) in 1988 as a computerized data repository for all burn care facilities in the United States and Canada.4,11–13 Following the 2005 call for data, the NBR included data on over 187,000 patients with burn injuries from 70 different institutions. Therefore, the NBR provides the unique opportunity to examine burn injuries on a national level. It has previously been used to examine the geographic distribution of burn admissions across state lines, sex differences in outcomes after injury, and the impact of obesity on outcomes.14–16 The purpose of this study was to use the NBR to characterize epidemiological patterns and outcome trends in older adults after burn injury.
METHODS
Study Overview
We performed a descriptive analysis of all patients aged 55 and older included in the NBR as of December 2006. The selection of age 55 was based on data from the National Study on Cost and Outcomes of Trauma indicating that injury outcomes begin to significantly change at age 55.17 Briefly, the NBR is a de-identified database maintained by the ABA and consists of voluntarily reported entries by 67 self-designated burn centers in the United States and three in Canada. Burn centers were eligible for inclusion if they 1) volunteered their data, 2) consented for their data to be pooled with that of other centers, and 3) participated in a burn registry. Institution names and geographical location of individual reporting burn centers were previously detailed in the 2005 NBR report.12 This study was performed after approval of the University of Washington Institutional Review Board.
Data Analysis
To study the differences in injury characteristics and outcome based on age, patients were stratified into the following age groups: 55 to 64, 65 to 74, and 75 and above. In accordance to the rules of the Health Insurance Portability and Accountability Act, patients aged 85 and older were assigned an age of 85, to help safeguard patients’ identities when a limited number of entries might permit their identification. As a result, the oldest age category in this study was designated as “patients aged 75 and above.” Baseline patient and injury characteristics, details of hospital treatment, mortality, and disposition were compared among these three age groups using χ2 for categorical variables or analysis of variance for continuous variables. The association between patient and injury characteristics and mortality was examined using multivariate logistic regression. Covariates included in this model were factors known to influence mortality risk including age, gender, burn size (% total and full-thickness burn) and presence of inhalation injury. All data analyses were performed using SAS 9.1 (Cary, NC).
RESULTS
From 1991 to 2005, 164,523 patient records were available for review in the NBR, of which 23,180 (or 14.0%) were patients aged 55 and older. As shown in Table 1, the percentage of patients aged 55 and older ranged from 11.2 (1991) to 15.2% (2003). The 55 to 64 age category had the largest number of patients (n = 9411); the 65 to 74 age category had the smallest number of patients (n = 6040).
Table 1.
Proportion of patients in the NBR who were older adults, by year of admission
| Year | Total Patients (n) | All Patients Age ≥55 (%) | 55–64 (%) | 65–74 (%) | 75 and Older (%) |
|---|---|---|---|---|---|
| 1991 | 2,395 | 11.2 | 5.0 | 3.4 | 2.8 |
| 1992 | 2,767 | 13.1 | 5.5 | 3.5 | 4.1 |
| 1993 | 3,627 | 12.7 | 5.1 | 3.6 | 4.0 |
| 1994 | 4,827 | 11.2 | 4.4 | 3.5 | 3.3 |
| 1995 | 5,957 | 13.1 | 5.8 | 3.3 | 4.0 |
| 1996 | 7,691 | 12.9 | 5.0 | 4.1 | 3.8 |
| 1997 | 9,332 | 13.7 | 5.2 | 3.9 | 4.6 |
| 1998 | 8,884 | 13.4 | 5.4 | 4.0 | 4.0 |
| 1999 | 8,406 | 14.9 | 6.2 | 4.1 | 4.6 |
| 2000 | 6,955 | 12.0 | 5.4 | 3.3 | 3.3 |
| 2001 | 7,558 | 12.6 | 5.7 | 3.4 | 3.5 |
| 2002 | 23,654 | 14.7 | 5.5 | 3.6 | 5.6 |
| 2003 | 25,741 | 15.2 | 5.9 | 3.8 | 5.5 |
| 2004 | 31,382 | 15.1 | 6.2 | 3.7 | 5.2 |
| 2005 | 15,347 | 13.9 | 6.2 | 3.3 | 4.4 |
NBR, National Burn Repository.
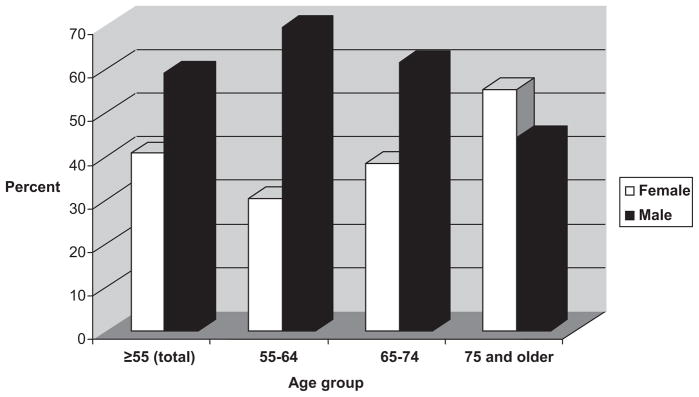
Gender and Race Distribution
Overall, men outnumbered women by a ratio of 1.4:1 (Figure 1). This male predominance, however, progressively decreased with increasing age. In the oldest age group, women (4290) outnumbered men (3439). The absolute number of male patients did not decrease with higher age group, rather the number of women with burn injuries doubled in the oldest age category compared with younger cohorts. Race distribution of burn injuries are shown in Table 2. Overall, 73.7% of patients were white, whereas 16.1% were black. Differences in race distribution across age groups were statistically significant (P < .001) although their proportions were similar from a clinical perspective (Table 2).
Figure 1.
Gender distribution, by age group.
Table 2.
Race and ethnicity distribution, by age category
| Race | n | Age ≥55 (%) | 55–64 (%) | 65–74 (%) | 75 and Older (%) | P |
|---|---|---|---|---|---|---|
| White | 18,396 | 73.7 | 71.1 | 72.9 | 77.5 | <.0001 |
| Black | 4,025 | 16.1 | 16.8 | 16.6 | 14.8 | |
| Hispanic | 1,035 | 4.2 | 5.7 | 3.9 | 2.5 | |
| Asian | 354 | 1.4 | 1.6 | 1.5 | 1.1 | |
| American Indian | 107 | 0.4 | 0.6 | 0.4 | 0.2 | |
| Other | 255 | 1 | 1.0 | 1.3 | 0.8 | |
| Not available | 794 | 3.2 | 3.2 | 3.4 | 3.0 |
Injury Characteristics
Flame burn was the most common injury etiology in patients aged 55 and older (Table 3). Scald injuries constituted the second most common listed etiology of burns. A large number of data points were missing in this category, listed as “unknown.” The percentage of cases reported as unknown increased with age category, becoming the most common listed cause in the oldest group (40% of cases).
Table 3.
Etiology of burn injuries
| Etiology | n | Age ≥55 (%) | 55–64 (%) | 65–74 (%) | 75 and Older (%) | P |
|---|---|---|---|---|---|---|
| Fire/flame | 9,396 | 37.6 | 37.5 | 42.0 | 34.4 | <.0001 |
| Scald | 5,599 | 22.4 | 24.2 | 22.5 | 20.2 | |
| Contact | 1,169 | 4.7 | 4.9 | 4.0 | 5.0 | |
| Chemical | 428 | 1.7 | 2.7 | 1.6 | 0.6 | |
| Electricity | 401 | 1.6 | 3.3 | 0.6 | 0.3 | |
| Inhalation only | 51 | 0.2 | 0.1 | 0.3 | 0.2 | |
| Radiation | 57 | 0.2 | 0.2 | 0.2 | 0.2 | |
| Unknown | 7,864 | 31.5 | 27.1 | 28.8 | 39.1 |
Overall average burn size was 9.6% TBSA, with approximately half as full-thickness injury (Table 4). A total of 11.3% of patients were diagnosed with inhalation injury. Mean burn size, and percent with inhalation injury while statistically different across age groups were clinically similar (Table 4). The majority of injuries occurred in the home (n = 13,869, or 55.6%). The incidence of burns outside the home decreased with higher age group, except for burns sustained in a residential institution, which steadily increased with age (Table 5).
Table 4.
Burn severity, according to age category
| Burn Severity | Age ≥55 | 55–64 | 65–74 | 75 and Older | P |
|---|---|---|---|---|---|
| TBSA | 9.6 | 9.5 | 10.3 | 9.3 | .001 |
| TBSA full thickness | 5.1 | 4.4 | 5.5 | 5.5 | <.0001 |
| % Inhalation injury | 11.3 | 10.4 | 12.8 | 11.3 | .2 |
Table 5.
Injury location, by age category
| Injury Site | n | Age ≥55 (%) | 55–64 (%) | 65–74 (%) | 75 and Older (%) | P |
|---|---|---|---|---|---|---|
| Home | 13,869 | 55.6 | 46.7 | 57.5 | 64.9 | <.0001 |
| Residential institution | 678 | 2.7 | 1.0 | 2.0 | 5.5 | |
| Farm or industrial site | 1,469 | 5.9 | 11.1 | 3.6 | 1.3 | |
| Place for recreation and sport | 447 | 1.8 | 2.6 | 1.8 | 0.8 | |
| Street and highway | 2,642 | 10.6 | 12.3 | 10.7 | 8.4 | |
| Public building | 443 | 1.8 | 1.8 | 1.6 | 1.9 | |
| Other specified places | 884 | 3.5 | 4.4 | 3.5 | 2.5 | |
| Unspecified place | 4,534 | 18.2 | 20.1 | 19.4 | 14.7 |
Outcomes
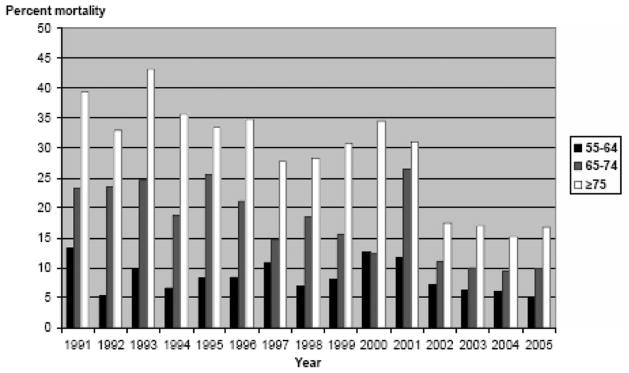
For each year from 1991 to 2005, higher age category was associated with greater mortality (Figure 2). Mortality rates decreased consistently after 2001 across all age groups. To more precisely examine the impact of age on mortality, we performed a multivariate logistic regression analysis which included a number of potential confounders of the relationship between age and mortality (Table 6). Age, percent TBSA, percent full-thickness injury, and presence of inhalation injury were all found to be independently associated with increased mortality risk. When using age 55 to 64 as the reference age group, the odds ratio for mortality was 2.3 (95% CI 2.1–2.7) in the 65 to 74 age group, and 5.4 (95% CI 4.8–6.1) in the oldest group.
Figure 2.
Mortality in older patients, by age category.
Table 6.
Adjusted odds of in-hospital mortality
| Variable | Odds Ratio | 95% Confidence Interval |
|---|---|---|
| Age group: 65–74* | 2.35 | 2.08–2.67 |
| Age group: 75 and older* | 5.44 | 4.847–6.11 |
| Male gender | 1.07 | 0.98–1.17 |
| Inhalation injury | 2.99 | 2.67–3.35 |
| TBSA | 1.06 | 1.05–1.06 |
| TBSA full-thickness component | 1.04 | 1.03–1.04 |
Reference group: age 55–64 category.
Average length of stay (LOS) was similar among age groups, but LOS indexed to TBSA (LOS/TBSA) increased with patient age (Table 7). Hospital charges also increased in older age categories. Median hospital charges for the 65 to 74 age group ($11,539) were 1.3 times higher and median charges for the 75 and older group ($17,455) were twice those of the 55 to 64 age cohort ($8693). We performed an adjusted analysis for charges in survivors, controlling for injury and treatment factors of burn size, full-thickness component, inhalation injury, and number of operations: higher age category was still strongly associated with higher charges (P < .0001). In contrast, mean number of operations was highest in the lowest age group (4.8, SD 6.1) and decreased with increasing age group (4.6 and 3.8, respectively).
Table 7.
Length of stay, operations and hospital charges
| Variable | n | Age ≥55 | 55–64 | 65–74 | 75 and Older | P |
|---|---|---|---|---|---|---|
| LOS mean (SD) | 21,010 | 13.3 (19.3) | 12.7 (19.3) | 13.9 (19.6) | 13.6 (19.0) | .001 |
| LOS/TBSA mean (SD) | 12,879 | 2.8 (5.7) | 2.5 (5.6) | 2.8 (6.0) | 3.3 (5.7) | <.0001 |
| Number of operations mean (SD) | 14,044 | 4.4 (5.4) | 4.8 (6.1) | 4.6 (5.5) | 3.8 (4.4) | <.0001 |
| Hospital charge median (IQR) | 17,308 | 12,389 (43,951) | 8,693 (41,928) | 11,539 (45,531) | 17,455 (44,892) | <.0001 |
LOS, length of stay in survivors; IQR, interquartile range.
Disposition status upon hospital discharge is shown in Table 7. The majority of older adults (51.7%) were discharged to home. However, the proportion of survivors discharged home decreased with increasing age. In the oldest category, only 32.8% of patients were discharged to home, whereas 19.4% were discharged to a skilled nursing facility or nursing home. Transfer to another acute care or rehabilitation facility also increased across age groups. Altogether, an increasing number of patients were discharged to nonindependent living with advancing age (Table 8).
Table 8.
Discharge disposition, by age category
| Discharge Disposition | n | Age ≥55 (%) | 55–64 (%) | 65–74 (%) | 75 and Older (%) | P |
|---|---|---|---|---|---|---|
| Home/other home | 12,903 | 51.7 | 66.5 | 52.6 | 32.8 | <.0001 |
| Skilled nursing facility/nursing home | 2,859 | 11.5 | 5.7 | 10.5 | 19.4 | |
| Rehabilitation-psychiatry referral | 1,852 | 7.4 | 4.3 | 7.5 | 11.3 | |
| Other acute care | 1,194 | 4.8 | 3.7 | 5.0 | 5.9 | |
| Death | 3,956 | 15.9 | 8.7 | 16.2 | 24.4 | |
| Other | 2,186 | 8.8 | 11.1 | 8.2 | 6.3 |
DISCUSSION
The NBR provides a unique opportunity to examine epidemiological trends and outcomes of older adults with burns on a national level. Several important insights can be derived from this analysis and provide a basis for future areas of study.
Burn injury constitutes a significant epidemiological problem in older adults. During the 15-year study period, older adult burns averaged 14% of admissions to burn units. Interestingly, the number of patients aged 75 and older was higher than those aged 65 to 74. Given an overall life expectancy of 77.8 years in the United States,18 one may have expected actual patient numbers to decrease with advancing age. There are several potential explanations for this observation. Although it is true that the oldest age category included a broader age interval, we postulate that the number of burn patients older than 85 was relatively small. An alternative explanation could be that burn incidence may have increased with advancing age. However, without corresponding population data (not available with the NBR since the population catchment is not defined), this second hypothesis could not be tested.
The second important finding was that burns in higher age categories were associated with higher resource consumption (increased LOS/TBSA, increased hospital charges). Although LOS was nearly equivalent among age groups, LOS indexed to TBSA increased with higher age category in the subset of patients who had both data points available (n = 12,879, Table 7). Many factors, such as the impact of comorbidities, thinner skin in older individuals, and rehabilitative challenges unique to this population, may have contributed to higher resource utilization. However, the number of operations did not seem to factor in this higher resource utilization. The number of operations actually decreased with advancing age, despite similar injury size (including full-thickness component, Table 4). This finding raises important questions as to the influence of age on burn management. For instance, institutional variations exist with respect to wound management in older adults. Whereas early wound excision and grafting has been a widely adopted practice for younger patients, similar consensus does not exist in the care of older adults6,8–10,19. Surgeons might be more reluctant to perform skin grafts over large areas because of prolonged donor site healing and the potential for graft loss, which could be life-threatening in older individuals. Clearly, further investigation is needed in this area to identify clear explanations for the observed age-dependent differences in management.
The association of age and mortality risk found in this study is consistent with previous studies on burn injury and mortality. In fact, all developed mortality prediction formulas have incorporated age as a prognostic factor.20–25 The empiric formula developed by Baux is clearly the simplest, whereby the sum of the patient’s age and burn size predicts mortality. Following Baux’s seminal contributions, additional factors were considered and complex formulas were developed using multifactorial probit and regression analysis.21,25 Regardless of the number of variables found to influence mortality, age has been consistently found to be independently associated with mortality.22,23,26,27 Similarly in this study, although burn size and inhalation injury were found to be significantly associated with mortality risk, age was found to be the strongest independent risk factor.
In this study, we used three age categories to better define the relationship between age and outcome. Our analysis demonstrated that within the older adult burn population, higher age category was associated with increased mortality risk. Although this finding is not unexpected, it does raise several important questions about the management of burn injuries with advancing age. More information would be necessary before we can determine specific factors contributing to higher mortality in older groups, such as the impacts of comorbidities, hospital complications, surgical management, and implementation of comfort care. Interestingly, we found that mortality decreased dramatically after 2001, to approximately 10% for the overall older cohort. This mortality reduction coincided with the increased reporting after the last ABA call for data (more than triple the number of entries per year), which underscores the importance of reporting to this national database.
Our analysis has mainly focused on survival. But as previously advocated by Saffle et al,10 survival should not be the sole outcome measured in older adults with burns. The impacts of preinjury health and living status, of physicians’ and systems’ practice, likely influenced outcomes, including mortality.6,10,28,29 Although we did not have these data available for our analysis, we suggest that future NBR data incorporate these important elements. Other outcomes to consider include function such as activities of daily living and return to major activities as well as psychological health, which are critical when examining the overall impact of burn injury. We also advocate that prospective evaluation is needed to better define the epidemiology and outcomes of burns in older adults. These studies may include multicenter projects to elucidate the influence of comorbidities on outcomes, surveys of physicians’ attitudes and practices, comparisons of models of care focusing on older adults with burns.
Finally, this study reinforces the utility and importance of a national burn database. Improvements in our understanding of burn injury and outcomes will be contingent on having reliable and well-populated databases. The inclusion of contributing data to the NBR as a criterion for burn center verification will hopefully increase the number of centers contributing data.30 Similar to other national health databases,31–33 a natural evolution for the NBR may be to set the benchmark for the quality of delivered burn care in the 21st century. However, if the NBR is to be used for establishing quality of care benchmarks, data completeness and quality will be critical. Missing values for patient and injury characteristics and outcomes could lead to inaccurate conclusions in epidemiological and outcome analyses.
In conclusion, the NBR data indicate that burn injury in older adults presents a significant epidemiological problem. Burns in older adults are associated with increased resource consumption and higher mortality with advancing age. Our analysis has also demonstrated that age-dependent differences in management exist within the older patient cohort. These findings highlight a need for a national research agenda focused on management practices and outcomes in older adult burns given the likely increase in older adults who will sustain burn injury in the future.
References
- 1.McGwin G, Jr, Cross JM, Ford JW, Rue LW., 3rd Long-term trends in mortality according to age among adult burn patients. J Burn Care Rehabil. 2003;24:21–5. doi: 10.1097/00004630-200301000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Merrell SW, Saffle JR, Sullivan JJ, Larsen CM, Warden GD. Increased survival after major thermal injury. A nine year review. Am J Surg. 1987;154:623–7. doi: 10.1016/0002-9610(87)90229-7. [DOI] [PubMed] [Google Scholar]
- 3.Pruitt BAJ, Wolf SE, Mason AD., Jr . Epidemiological, demographic, and outcome characteristics of burn injury. In: Herndon DN, editor. Total burn care. 3. St. Louis, MO: Elsevier; 2007. pp. 14–32. [Google Scholar]
- 4.Saffle JR, Davis B, Williams P. Recent outcomes in the treatment of burn injury in the United States: a report from the American Burn Association Patient Registry. J Burn Care Rehabil. 1995;16:219–32. doi: 10.1097/00004630-199505000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Chang EJ, Edelman LS, Morris SE, Saffle JR. Gender influences on burn outcomes in the elderly. Burns. 2005;31:31–5. doi: 10.1016/j.burns.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 6.Wibbenmeyer LA, Amelon MJ, Morgan LJ, et al. Predicting survival in an elderly burn patient population. Burns. 2001;27:583–90. doi: 10.1016/s0305-4179(01)00009-2. [DOI] [PubMed] [Google Scholar]
- 7.Pomahac B, Matros E, Semel M, et al. Predictors of survival and length of stay in burn patients older than 80 years of age: does age really matter? J Burn Care Res. 2006;27:265–9. doi: 10.1097/01.BCR.0000216795.90646.4E. [DOI] [PubMed] [Google Scholar]
- 8.Cadier MA, Shakespeare PG. Burns in octogenarians. Burns. 1995;21:200–4. doi: 10.1016/0305-4179(95)80009-d. [DOI] [PubMed] [Google Scholar]
- 9.Deitch EA. A policy of early excision and grafting in elderly burn patients shortens the hospital stay and improves survival. Burns Incl Therm Inj. 1985;12:109–14. doi: 10.1016/0305-4179(85)90036-1. [DOI] [PubMed] [Google Scholar]
- 10.Saffle JR, Larson CM, Sullivan J, Shelby J. The continuing challenge of burn care in the elderly. Surgery. 1990;108:534–43. [PubMed] [Google Scholar]
- 11.Latenser BA, Miller SF, Bessey PQ, et al. National Burn Repository 2006 Report Dataset Version 3.0. J Burn Care Res. 2007;28:645–58. doi: 10.1097/BCR.0B013E31814B25B1. [DOI] [PubMed] [Google Scholar]
- 12.Miller SF, Bessey PQ, Schurr MJ, et al. National Burn Repository 2005: a ten-year review. J Burn Care Res. 2006;27:411–36. doi: 10.1097/01.BCR.0000226260.17523.22. [DOI] [PubMed] [Google Scholar]
- 13.Saffle JR. The current status of the NATIONAL TRACS/ABA Burn Registry. J Burn Care Rehabil. 1997;18:172–5. doi: 10.1097/00004630-199703000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Carpenter AM, Hollett LP, Jeng JC, Wu J, Turner DG, Jordan MH. How long a shadow does epidemic obesity cast in the burn unit? A dietitian’s analysis of the strengths and weaknesses of the available data in the National Burn Repository. J Burn Care Res. 2008;29:97–101. doi: 10.1097/BCR.0b013e31815f59b1. [DOI] [PubMed] [Google Scholar]
- 15.Guagliardo MF, Jeng JC, Browning S, et al. Admissions across state lines: harnessing the insight of the National Burn Repository for the healthcare accessibility, fiscal, and legislative concerns facing the American Burn Association. J Burn Care Res. 2008;29:151–7. doi: 10.1097/BCR.0b013e31815fa480. [DOI] [PubMed] [Google Scholar]
- 16.Kerby JD, McGwin G, Jr, George RL, Cross JA, Chaudry IH, Rue LW., 3rd Sex differences in mortality after burn injury: results of analysis of the National Burn Repository of the American Burn Association. J Burn Care Res. 2006;27:452–6. doi: 10.1097/01.BCR.0000225957.01854.EE. [DOI] [PubMed] [Google Scholar]
- 17.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–78. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 18.Minino AM, Heron MP, Murphy SL Centers for Disease Control and Prevention National Center for Health Statistics National Vital Statistics System. Deaths: final data for 2004. Natl Vital Stat Rep. 2007;55:1–120. [PubMed] [Google Scholar]
- 19.Rao K, Ali SN, Moiemen NS. Aetiology and outcome of burns in the elderly. Burns. 2006;32:802–5. doi: 10.1016/j.burns.2006.03.024. [DOI] [PubMed] [Google Scholar]
- 20.Baux S. Contribution a l’etude du traitement local des brulures thermigues etendues. Paris, France: 1961. [Google Scholar]
- 21.Feller I, Flora JD, Jr, Bawol R. Baseline results of therapy for burned patients. JAMA. 1976;17:1943–7. [PubMed] [Google Scholar]
- 22.O’Keefe GE, Hunt JL, Purdue GF. An evaluation of risk factors for mortality after burn trauma and the identification of gender-dependent differences in outcomes. J Am Coll Surg. 2001;192:153–60. doi: 10.1016/s1072-7515(00)00785-7. [DOI] [PubMed] [Google Scholar]
- 23.Ryan CM, Schoenfeld DA, Thorpe WP, et al. Objective estimates of the probability of death from burn injuries. N Engl J Med. 1998;338:362–6. doi: 10.1056/NEJM199802053380604. [DOI] [PubMed] [Google Scholar]
- 24.Tobiasen J, Hiebert JM, Edlich RF. The abbreviated burn severity index. Ann Emerg Med. 1982;11:260–2. doi: 10.1016/s0196-0644(82)80096-6. [DOI] [PubMed] [Google Scholar]
- 25.Zawacki BE, Azen SP, Imbus SH, Chang YT. Multifactorial probit analysis of mortality in burned patients. Ann Surg. 1979;189:1–5. doi: 10.1097/00000658-197901000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Germann G, Barthold U, Lefering R, Raff T, Hartmann B. The impact of risk factors and pre-existing conditions on the mortality of burn patients and the precision of predictive admission-scoring systems. Burns. 1997;23:195–203. doi: 10.1016/s0305-4179(96)00112-x. [DOI] [PubMed] [Google Scholar]
- 27.Tobiasen J, Hiebert JH, Edlich RF. Prediction of burn mortality. Surg Gynecol Obstet. 1982;154:711–4. [PubMed] [Google Scholar]
- 28.Anous MM, Heimbach DM. Causes of death and predictors in burned patients more than 60 years of age. J Trauma. 1986;26:135–9. doi: 10.1097/00005373-198602000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Burdge JJ, Katz B, Edwards R, Ruberg R. Surgical treatment of burns in elderly patients. J Trauma. 1988;28:214–7. doi: 10.1097/00005373-198802000-00016. [DOI] [PubMed] [Google Scholar]
- 30. [accessed 8 Jan. 2008];Verification guidelines: guidelines for the operation of burn centers. available from http://www.ameriburn.org; Internet;
- 31.Factsheet. [accessed 15 Jan. 2008];Hospital performance measurement initiatives. available from http://www.leapfroggroup.org; Internet;
- 32.Kahn JM, Brake H, Steinberg KP. Intensivist physician staffing and the process of care in academic medical centres. Qual Saf Health Care. 2007;16:329–33. doi: 10.1136/qshc.2007.022376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leonardi MJ, McGory ML, Ko CY. Publicly available hospital comparison web sites: determination of useful, valid, and appropriate information for comparing surgical quality. Arch Surg. 2007;142:863–8. doi: 10.1001/archsurg.142.9.863. [DOI] [PubMed] [Google Scholar]