Abstract
Objectives
Most practitioners believe that use of two hearing aids is the ideal fitting for adults with bilateral symmetrical hearing loss. However, previous research has consistently shown that a substantial proportion of these patients actually prefer to use only one hearing aid. The current study explored whether this pattern of preferences is seen with technologically advanced hearing aids. In addition, a selection of variables that were available pre-fitting were used to attempt to predict which patients will prefer one hearing aid rather than two.
Design
The study was designed as a 12-week field trial including structured and unstructured use of one and two hearing aids. Ninety-four subjects with mild to moderate bilaterally symmetrical hearing loss were bilaterally fit with 2005-2007 era hearing aids. Potential predictors included demographic, audiometric, auditory lifestyle, personality, and binaural processing variables. After the field trial, each subject stated his/her preference for one or two hearing aids and completed three self-report outcome questionnaires for their preferred fitting.
Results
Previous research was confirmed with modern technology hearing aids: after the field trial 46% of the subjects preferred to use one hearing aid rather than two. Subjects who preferred two hearing aids tended to report better real-world outcomes than those who preferred one. Subjects who reported more hearing problems in daily life, who experienced more binaural loudness summation, and whose ears were more equivalent in dichotic listening were more likely to prefer to use two hearing aids. Contrary to conventional wisdom (ideas that are generally accepted as true), audiometric hearing loss and auditory lifestyle were not predictive of aiding preference. However, the best predictive approach from these data yielded accurate predictions for only two-thirds of subjects.
Conclusions
Evidence-based practice calls for a conscientious melding of current evidence, clinical judgment, and patient preferences. The results of this research challenge practitioners to recognize that many patients who appear to be ideal candidates for bilateral aiding will actually prefer to wear only one hearing aid. Further, at this time there is not an accurate method that will predict which patients will prefer one hearing aid rather than two. Currently, the most effective approach open to practitioners would be to conduct a candid unbiased systematic field trial allowing each patient to compare unilateral and bilateral fittings in daily life. This might necessitate more fitting sessions and could perhaps add to the practitioner's burden. This downside should be weighed against the additional patient satisfaction that can be anticipated as a result of transparency in the fitting protocol, collaboration with the patient in the treatment decisions, and the knowledge of selecting the most cost-effective patient-centered solution.
Keywords: hearing aids, binaural, field trial, outcomes
Introduction
The advantages of binaural hearing over monaural were reported more than half a century ago (Koenig, 1950) and have been extensively studied for many years. For recent reviews see Akeroyd (2006) and Colburn, et al. (2006). These advantages include reduced head shadow effect as well as benefits of binaural processing such as: improved speech understanding, especially in spatially separated noise (binaural squelch); binaural loudness summation; and improved localization. There have been numerous studies attempting to determine whether these binaural processing advantages are demonstrable in laboratory testing for bilaterally hearing-impaired persons wearing two hearing aids. Although the results have not been unanimous, many investigations report demonstrable binaural advantages for subjects wearing two hearing aids (e.g., Hawkins & Yacullo, 1984; Day, Browning, & Gatehouse, 1988; Byrne, Noble, & LePage, 1992; Freyaldenhoven, Plyler, Thelin, & Burchfield, 2006). Because data demonstrating the availability of binaural advantages appear to establish the efficacy of bilateral hearing aid fittings, it might seem logical to assume that individuals with bilateral hearing-impairment will prefer to wear two hearing aids rather than one in daily life. However, efficacy established in a laboratory setting does not ensure effectiveness in daily life. Thus, there also has been interest in scientifically establishing a preference for wearing two hearing aids, rather than one, in daily life. There have been two types of research designs that have explored advantages of bilateral hearing aid fittings in everyday life: field trials and retrospective surveys.
Several field trials addressing this topic have been reported in which patients were fitted with one or two devices and asked, after an acclimatization period, to report which arrangement they preferred. In a study of hearing-impaired military personnel Erdman and Sedge (1981) fit 30 subjects with two hearing aids and conducted a two-week field trial to systematically compare unilateral and bilateral fittings. Although most of the subjects reported a preference for two hearing aids, 20% of the subjects declared a preference for wearing only one hearing aid at the end of the trial. In a similar study, Schreurs and Olsen (1985) fit 30 subjects with two hearing aids followed by a four-week field trial with systematic comparison of unilateral and bilateral fittings. At the end of the trial most subjects preferred the bilateral fitting for listening in quiet and the unilateral fitting for listening in noise. Ultimately, 57% of the subjects purchased one hearing aid and 27% purchased two. Day, Browning, and Gatehouse (1988) reported a field trial with 51 subjects fitted with two hearing aids and re-assessed after a period of several months of unsupervised use of one or two devices. At the end of the trial, 22% of the group declared a preference for wearing only one hearing aid. Stephens et al. (1991) conducted a crossover trial with 29 subjects comparing fitting of one or two hearing aids. Each segment of the trial was 4-6 weeks in length. Forty-five percent of the subjects elected to adopt the unilateral fitting at the end of the trial. Finally, Vaughan-Jones et al. (1993) completed a crossover trial comparing unilateral and bilateral fittings in which the length of each arm was 10 weeks. Of the 64 subjects, 61% eventually chose the unilateral aided condition.
Another approach to exploring the benefits of bilateral versus unilateral hearing aid fittings in daily life is the retrospective survey. In this type of study, patients who previously have been fit with two hearing aids are queried about whether, and when, they actually use both devices or only one (or neither). Many of the published retrospective surveys were conducted in countries where hearing aids are provided under a public health umbrella. In these systems, it is typical that some selection process is used to determine which patients will receive two hearing aids, although the criteria for recommending two hearing aids rather than one are not always explicit. Therefore, the subject groups in these studies are not necessarily a random selection of typical hearing aid wearers.
Brooks and Bulmer (1981) surveyed 204 patients who had received two hearing aids through the British National Health Service at least three months earlier. Twenty-five percent of the respondents reported that they did not regularly use both hearing aids but only 3% stated a definite preference for only one device. Chung and Stephens (1986) surveyed 200 patients who had chosen to be fitted with two hearing aids at least 6 months earlier. The goal was to explore factors that influenced hearing aid use. Nineteen percent of these individuals reported that they now used only one hearing aid. Dillon, Birtles, and Lovegrove (1999) reported a wide-ranging study of hearing aid fitting outcomes in which they surveyed 4421 patients around Australia. Of those patients who had originally received two hearing aids, 20% reported wearing only one when surveyed three months later. Kobler, Rosenhall and Hansson (2001) assessed the outcomes for 144 Swedish patients who had been provided with two hearing aids at least eight months previously. They determined that 33% of the group actually used only one hearing aid.
Finally, a somewhat different but still illuminating retrospective study was reported by Boymans et al. (2009). This work described the results of a clinical program in the Netherlands in which the fitting of one or two hearing aids was decided collaboratively between the practitioner and the patient. The protocol encompassed several fitting sessions, trial periods, counseling, real ear measures and speech testing. Results accumulated across 1000 patients sampled from eight centers indicated that about 40% of patients who experienced this protocol were ultimately fitted with one hearing aid rather than two. However, after the subject group was pared down to 689 who were thought most likely to benefit from bilateral fitting (by excluding individuals with asymmetric hearing loss and those with better-ear hearing loss less than 35 dB), the proportion of subjects choosing one hearing aid rather than two was 31%.
The consensus of these studies over at least 25 years is that the majority of bilaterally impaired persons who are provided with two hearing aids do ultimately decide that the advantages of wearing two hearing aids outweigh the advantages of wearing only one. Nevertheless, it is striking that in every reported field trial and retrospective survey a substantial percent of subjects reported a preference for wearing only one hearing aid rather than two. Despite the generally positive outcomes of bilateral hearing aid fittings, there is always a substantial minority of individuals in any studied group who ultimately prefer and choose to wear only one hearing aid. The reported prevalence of this result is surprisingly high. If we assume that each of the controlled field trials produced a valid estimate of the preference for wearing one hearing aid, an average of those estimates indicates that 41% of patients preferred to wear one hearing aid rather than two. If we likewise assume that each of the retrospective surveys produced a valid estimate of the preference for wearing one hearing aid, the average of those estimates suggests that the preference occurred in 21% of patients.
Given the existence of this body of literature, it is surprising that current practitioners appear to believe strongly that bilateral fitting is the best treatment for essentially all bilaterally hearing impaired adults (e.g., Kiessling et al. 2006). The proportion of bilateral hearing aid fittings in the US has grown steadily over the past 20 years to 90% (Kochkin, 2009). The assertion of superiority for bilateral fittings is typically supported by extrapolations from the laboratory data cited earlier. Sometimes the assertion is bolstered by self-report data showing that patients wearing two hearing aids tend to have better subjective outcomes than patients who wear only one hearing aid (e.g., Kochkin & Kuk, 1997). However, this argument is not convincing unless it can be demonstrated that patients who choose to wear one hearing aid are willing and able to improve their fitting outcomes by switching to two hearing aids.
Some practitioners are aware that not all of their bilaterally impaired adult patients prefer to use two hearing aids, but they do not have a method of prospectively identifying which bilaterally impaired individuals will prefer only one hearing aid. Typical audiometric and demographic data (age, audiogram, speech recognition score, etc.) have not been useful in predicting unsuccessful bilateral fittings (Day et al. 1988; Swan, 1989; Vaughan-Jones et al. 1993; Boymans et al. 2009). The most fully explored potential predictor of unsuccessful bilateral hearing aid fitting is the presence of binaural interference. In normal binaural functioning, cues from the two ears are integrated to produce superior performance over either ear alone. When binaural interference is present the two ears do not work together to take advantage of interaural differences: there is obstruction rather than integration. As a result, bilateral performance is poorer than that with the better unilateral ear. Binaural interference and accompanying abnormalities in dichotic listening skills have been studied extensively by Jerger and colleagues (e.g., Jerger et al. 1990; Jerger et al. 1993; Jerger et al. 1995; Chmiel & Jerger, 1996; Chmiel et al. 1997). Taken as a whole, this work presents a convincing case for the presence of binaural interference and abnormally poor dichotic listening abilities in at least 10 percent of elderly hearing-impaired persons, and it demonstrates that bilateral amplification might be unsuccessful in these cases.
Based on existing estimates, it is unlikely that binaural interference accounts for all of the one-quarter or more of bilateral fittings in which one instrument is ultimately rejected (41% in field trials and 21% in retrospective surveys). Several investigators suggest that other indicators for fitting one versus two hearing aids might include a lack of binaural advantages such as binaural loudness summation and/or binaural release from masking (e.g., Swan, 1989; Stephens et al. 1991; Kobler et al. 2001; Haggard and Hall, 1982). In addition, it seems plausible that self-report variables measurable before the fitting (e.g., subjective assessment of hearing loss or personality attributes) might play a role in determining acceptance of a bilateral fitting in the long-term.
In summary, existing research including both clinical trials and descriptive studies has repeatedly shown that a substantial proportion of adults who have bilateral hearing impairment opt to wear only one hearing aid even when two devices are readily available. The implication is that a sizeable minority of hearing-impaired listeners either do not perceive the anticipated benefits of bilateral hearing aids or find that the benefits do not outweigh the drawbacks. These individuals might be better served with a unilateral fitting. It is also noteworthy that most of the reviewed studies were conducted in an era when hearing aids were technologically far inferior to current devices. Thus, it is possible that the proportional preference for two hearing aids has increased with technology improvement.
An accurate and practical method for prospectively identifying individuals who will prefer to wear one hearing aid despite their bilateral hearing impairment could be expected to result in more appropriate resource allocation, more cost-effective treatments, and more satisfied patients. Although (as reviewed above) some potential predictors of preference for one or two hearing aids have been mentioned in the literature, little effort has been made to compare pre-fitting indicators with post-fitting long-term outcomes of hearing aid fitting.
The research described here was directed towards answering two questions:
Are previous results about preference for one or two hearing aids replicated when subjects are fitted with modern high-tech devices?
How accurately can long-term preference for one or two hearing aids be predicted using a combination of pre-fitting psychoacoustic, self-report, and demographic data?
Materials and Methods
Subjects who met the inclusion criteria were administered a test battery to explore their binaural functioning, and to accumulate self report data regarding personality and auditory lifestyle. This was followed by hearing aid fitting and verification. Then, subjects began a structured three-week unilateral/bilateral device wearing schedule to ensure significant experience with both amplification choices. Next, they used both hearing aids as desired in daily life for about nine weeks, exploring the effectiveness of unilateral and bilateral fittings. Finally, they participated in an exit interview and provided subjective outcome data on the effectiveness of their preferred fitting of one or two hearing aids.
Participants
Subjects were recruited from the Mountain Home Veterans Affairs Medical Center (VAMC) and the University of Memphis Hearing Aid Research Laboratory (HARL). The VAMC recruited male patients seeking amplification. The HARL used advertisements, word of mouth, brochures, and personal letters to recruit both men and women who were interested in new hearing aids. Subjects were paid for their participation.
Inclusion criteria were: Symmetrical bilateral stable sensorineural hearing impairment, better ear pure tone average (0.5, 1.0, 2.0 kHz) of 30 – 80 dB HL, normal immittance test results, age between 50 and 85, a report of typically active lifestyle, self-rated good or excellent physical and mental health, adequate literacy and cognitive competence (by informal testing and researcher report) to respond to questionnaires, and willingness to wear hearing aids at least four hours a day during the trial. In addition, potential subjects were required to be open-minded about whether they would prefer to wear one or two hearing aids in daily life. Exclusion criteria included: an existing preference for either one or two hearing aids, observed or reported neurologic or psychiatric disorder, fluctuating hearing impairment, and chronic middle or outer ear pathology.
A priori computation of power for the study was based on pilot data using the dichotic digits test and results from Carter, Noe and Wilson (2001). It was assumed that 80% of subjects whose dichotic digits score was 3 standard deviations below the mean would prefer to use one hearing aid rather than two. In this case, 100 subjects yielded about 80% power to reject the null hypothesis (alpha=.05) that hearing aid preference was unrelated to the dichotic digits score. Thus, the targeted number of subjects was 100.
Of 98 potential subjects at the VAMC, 49 met all inclusion criteria and were enrolled in the study. Of 71 potential subjects at the HARL, 51 met all inclusion criteria and were enrolled in the study. Subsequently, six individuals withdrew for personal reasons not related to the study. A total of 94 individuals, 57 men and 37 women, (47 at each site) completed the experiment. Mean ages were: women=69 (range 51—83), men= 71 (range 58 – 83). Seventy-six subjects were classified as new hearing aid users. Of these, 10 had tried amplification briefly in the past but did not pursue it. The remaining 18 subjects owned and used (at least part time) one or two hearing aids, but did not know whether they would actually prefer to wear one or two hearing aids in daily life. Figure 1 depicts the mean audiograms of men and women subjects. Mean word recognition scores for women and men were 82% (range=42-100) and 76% (range=42-96), respectively.
Figure 1.
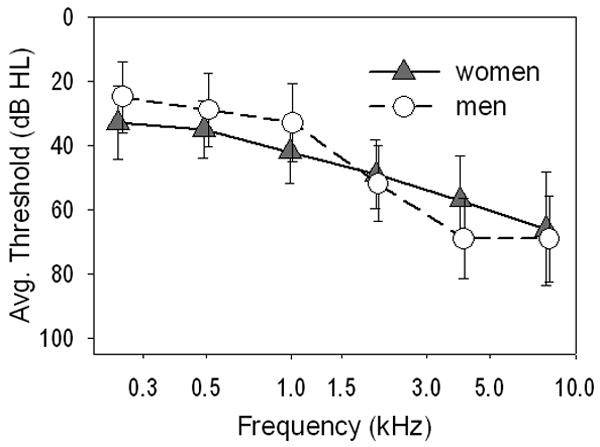
Mean audiograms for men and women enrolled in the study. Bars show one standard deviation.
Pre-fitting questionnaires
The Auditory Lifestyle and Demand Questionnaire (ALDQ) was developed by Gatehouse, Elberling, and Naylor (1999). The goal of the ALDQ is to describe the range of listening environments that are experienced by the individual in daily life and to assess the extent to which auditory requirements play a role in daily functioning. This 24-item questionnaire yields scores in two subscales: Lifestyle and Demand.
Lifestyle represents the diversity of listening situations experienced. Each Lifestyle item queries the regularity with which a given situation occurs in everyday life. It is scored on a 3 point scale: 0 = very rarely, 1 = sometimes, 2= often. The Lifestyle score was computed by summing the 24 item responses in the subscale, thus the potential raw scores ranged from 0 to 48. Demand is a combination of Lifestyle and the importance of each situation to that subject. The second set of responses provides an importance weighting for each item in the Lifestyle subscale. It includes responses on a 3 point scale: 0 = very little, 1 = some importance, 2 = very important. The Demand score was computed as follows: each item response in the Lifestyle subscale was multiplied by its corresponding importance weighting and the 24 products were summed to create the Demand score for the subject. The potential raw scores ranged from 0 to 96. Both Lifestyle and Demand subscales were converted to percentage scores.
Two dominant dimensions of personality were assessed using the Positive and Negative Affect Schedule (PANAS). The PANAS was developed by Watson, Clark, and Tellegen (1988). Positive affect is the extent to which an individual feels engaged, animated, attentive etc., whereas negative affect reflects unpleasant states such as fearfulness, irritability, pessimism, etc. The two dimensions are independent: they should not be thought of as opposite ends of the same continuum. The results of the PANAS offer a condensed view of the “big five” personality traits described by many psychology researchers (e.g., McCrae & Costa, 1997). Unpublished data from our laboratory has shown that the Negative Affect score is significantly positively correlated with the personality dimension typically labeled Neuroticism, whereas the Positive Affect score is significantly positively correlated with each of the four personality dimensions typically labeled Extraversion, Openness, Agreeableness, and Conscientiousness (Kelly & Cox, Reference Note 1). The PANAS is a 20-item scale that yields scores for Positive Affect (PA) and Negative Affect (NA). Each affect state is measured using 10 items. Each item is a word describing a mood or emotion (interested, ashamed, etc) and subjects indicate the extent to which they generally feel this way on a 5 point scale: from 1=very slightly to 5=extremely. A higher score represents a stronger level of affect. The Negative Affect score was calculated by summing the 10 scores for the negative affect items. The Positive Affect score was calculated by summing the 10 scores for the positive affect items. Thus, each score could range from 10 to 50.
Binaural Test Battery
Three types of binaural interaction were tested for this research: binaural loudness summation, binaural squelch, and binaural interference. Each test feasibly could be used as part of a pre-fit assessment in a clinical setting. The tests were chosen because they have the following characteristics which were desirable for this experiment with older hearing-impaired listeners: (1) all three involve binaural processing of speech, (2) the speech material is familiar without being too easy, (3) pilot testing revealed that all three tests result in clearly measureable binaural effects for a typical older hearing-impaired listener, (4) for symmetrical high-frequency cochlear hearing loss, they are resistant to confounding due to audibility effects (e.g., Strouse & Wilson, 1999), (5) Based on published work and pilot work in our laboratory, all three tests have been shown to be reliable (eg., Humes et al. 1996; Cox et al. 1997), (6) all three tests are readily administered in a clinical environment. Each test employed speech stimuli delivered from CD recordings routed through an audiometer and presented to the subject via ER-3A insert earphones coupled to the ears with compressible foam plugs.
Binaural Loudness Summation
The binaural loudness summation test determined the extent to which binaural listening affected the level at which speech was deemed to be comfortably loud, compared to monaural listening. Binaural summation was measured as the difference in decibels between comfortable loudness levels for each ear separately and for both ears together. It is a common clinical observation that preferred hearing aid gain is less for bilateral fittings than for unilateral fittings. This is usually assumed to be the result of binaural loudness summation (e.g., Dermody & Byrne, 1975). It is plausible that individual differences in the size of this effect are proportional to binaural integration ability in general, and possibly associated with the acceptance of bilateral amplification.
The stimuli were successive sentences from a passage of the Connected Speech Test (Cox et al., 1987) presented without competing noise. The subject was given a list of the seven loudness categories as depicted in Table 1 and instructed to verbally respond to indicate the appropriate loudness category when a sentence was presented. The goal was to determine the level judged to be “comfortable but slightly loud” (category 5). First, a practice trial was run with the stimuli presented bilaterally. Sentences were presented in ascending 5 dB steps until a category 7 level was reached. The level was then lowered 20-30 dB and the ascending 5 dB method began again and continued until a category 7 was again attained. This practice was continued until the subject responded consistently. Once the investigator was satisfied the subject understood the task, the binaural summation test began.
Table 1. Loudness categories used in the binaural loudness summation test.
| Category # | Category description |
|---|---|
| 7 | Uncomfortably Loud |
| 6 | Loud, But O.K. |
| 5 | Comfortable, But Slightly Loud |
| 4 | Comfortable |
| 3 | Comfortable, But Slightly Soft |
| 2 | Soft |
| 1 | Very Soft |
The sentences were presented to one ear with 10 dB ascending increments until a category 5 response was given. The stimulus was then decreased 10-15 dB and presented again in 2 dB ascending steps until a category 5 value was given. The test continued in this manner until two category 5 responses were given at the same dial setting. This level was the “comfortable but slightly loud” level (CSL) for that ear. The test was repeated for the other ear. After monaural CSL had been determined for each ear, the audiometer tracking was engaged so the level in the two ears would increase/decrease together, preserving any interaural difference in monaural CSL levels. Then, the binaural CSL test was conducted in the same manner as the monaural CSL test. The binaural summation score for the test was the difference between the binaural CSL level and the monaural CSL level.
The binaural CSL level was used as the stimulus level for the remaining tests in the binaural test battery. This ensured both equal loudness and appropriate audibility for both ears. In addition, using a comfortable-but-slightly-loud level presentation level ensured that the binaural interaction and binaural interference tests were presented at a level close to that which would be chosen by the subject in daily life when listening to amplified sounds using hearing aids.
Binaural Squelch
A test of binaural release from masking for speech (binaural squelch) was chosen because it was postulated that the extent to which the two ears are able to work together to improve speech intelligibility in noise would be predictive of the advantage bestowed by bilateral hearing aids in real world listening. The phenomenon of binaural squelch has been extensively studied in normal-hearing listeners, but less fully explored in listeners with hearing impairment. Published research has shown that older listeners yield smaller binaural squelch effects than do younger listeners (e.g., Grose et al. 1994). In addition, studies have indicated that hearing-impaired individuals often have smaller binaural squelch than normal-hearing persons (e.g., Noffsinger, 1982; Jerger et al. 1984). Further, it is generally observed that binaural squelch for speech varies to some extent with stimulus details (e.g., (Wilson et al. 1994; Johansson & Arlinger, 2002).
Binaural squelch was quantified as the difference between two binaural SNR-50 scores (SNR-50 is the signal-to-noise ratio which yields a speech recognition score of 50% correct). The first SNR-50 was measured with speech and noise both in-phase at the two ears. The second SNR-50 was measured with speech 180° out of phase but noise in-phase at the two ears. The stimuli were spondee words presented from the Department of Veterans Affairs compact disc entitled “Tonal & Speech Materials for Auditory Perception Assessment Disc 2.0.” Using the same test with young normal-hearing adults, Wilson, Zizz and Sperry (1994) reported mean binaural squelch values of about 8-9 dB. In a pilot study in our laboratory, we found the mean binaural squelch value for older adults with hearing loss to be about 4 dB, which is consistent with previous research showing smaller release from masking effects for hearing-impaired and older listeners.
The test comprises 10 spondee words (Wilson et al. 1982). To minimize word learning effects, the subject was given a list of the 10 words before the test began. Each spondee word was embedded in a burst of broadband noise (duration 2000ms). Stimuli were recorded at 16 signal-to-noise ratios (SNR) ranging from 0 dB to -30 dB. Four words were presented at each SNR. The test began with four words presented at 0 dB SNR. For each consecutive four word set, the SNR on the CD changed by 2 dB, making the words increasingly difficult to understand. The test continued until the subject missed all four words in a single SNR condition. The test was stopped at this point. The test score was the poorest SNR at which 50% of the spondee words were correctly repeated. The entire test was performed twice. The binaural squelch score was the difference between the average in-phase SNR and the average out-of-phase SNR.
Binaural Interference
Binaural interference was estimated using a dichotic digits test. The test materials were provided on the Department of Veterans Affairs compact disc entitled “Tonal & Speech Materials for Auditory Perception Assessment Disc 2.0.” The test presented sets of three different one-syllable digits simultaneously to the two ears, without background noise. For example, the right ear might receive “2, 10, 4” while the left ear receives “1, 8, 6.” The recorded digits were synchronized so that the onsets were simultaneous for the two digits of each right-left pair. Subjects were instructed to recall and repeat all digits from both ears (free recall) or only those from left or right ear (directed recall). They were given practice trials until they were comfortable with the tasks (usually about five trials). There were 25 trials in each test condition (directed right, directed left, and free recall). In all three conditions, the listener was presented with stimuli to both ears but instructed to repeat only the digits heard in the right ear (Directed Right condition), or the left ear (Directed Left condition) or all the digits heard in both ears (Free Recall condition).
Results may be interpreted in terms of the score differences between: (1) free and directed recall, and (2) left and right ears. In general, it is expected that the free recall task will be more difficult than the directed recall task because of the greater cognitive, attention and memory resources called upon when both ears are simultaneously monitored. In addition, it is expected that there will be a right ear advantage so that right ear scores are better than left ear scores. Published normative data for the dichotic digits confirm these expectations and show that performance declines with age (Strouse & Wilson, 1999). Further, data from this test have been reported (Carter et al. 2001) to be associated with binaural interference and unsuccessful bilateral amplification in four individual cases.
Initially, scores were computed for the free recall condition for each ear (free-right and free-left) and for the directed recall condition for each ear (direct-right and direct-left). Each score was based on the number correctly recalled from 75 digits. Four additional scores were computed to analyze the results of the test, as follows:
Right Ear Advantage Free Recall (REAfree) = free-right minus free-left
Right Ear Advantage directed Recall (REAdir) = direct-right minus direct-left
Cognitive effect right ear (Cogre) = direct-right minus free-right
Cognitive effect left ear (Cogle) = direct-left minus free-left
Hearing Aid fitting
The hearing aids used this in this study were required to meet the following criteria to be consistent with the subject audiograms and with current practice in hearing aid fitting: (1) appropriate for a 30 – 80 dB HL three-frequency average sensorineural hearing loss with a flat or sloping configuration, (2) good quality digital programmable device, (3) some form of compression, (4) a directional microphone (either fixed or adaptive technology) and (5) at least two programs (program 1 set for omni-directional and program 2 set for directional). In addition, user volume controls were required to allow subjects to adjust gain as needed for using one or two hearing aids. Also, because of the length of the experiment, it was essential that the hearing aids be acceptable to the subject for long-term use. Other allowed features were: feedback management (as long as it did not degrade the high frequency-response), digital noise reduction, and telecoil. Table 2 gives the distribution of hearing aid make/model used in the study. The hearing aids styles were chosen as appropriate for the subject and were distributed across subject ears as follows: BTE=73, ITE=18, ITC=2, CIC=1. Hearing aid features in addition to volume control and directional microphone were chosen as appropriate for the subject as follows: telecoil=158, feedback manager=20, digital noise reduction=85, low level expansion=8.
Table 2. Distribution of hearing aid models for 94 subjects.
| Manufacturer | Model | Pairs |
|---|---|---|
| Siemens | Centra | 1 |
| Siemens | Cielo | 10 |
| Unitron | Conversa | 5 |
| Starkey | Destiny | 1 |
| Phonak | Valeo | 44 |
| Phonak | Eleva | 8 |
| Oticon | Tego Pro | 25 |
For all 47 of the HARL subjects and 15 of the VA subjects, hearing aids were loaned to them for this investigation with the understanding that they would be returned at the end of the study. The remaining 32 VA subjects were fit with hearing aids purchased by the VA. It was emphasized with these 32 veterans that they would keep both hearing aids regardless of their wearing preference at the end of the study.
Hearing Aid Fitting and Verification Protocol
Hearing aids were initially programmed using the manufacturer's proprietary method and then modified based on the fitting targets. Modifications of performance and verification were completed under the guidance of probe microphone real ear measurements using a Fonix 7000 Hearing Aid Test System. The target for average speech was to amplify speech-like noise (labeled DGSP-ICRA noise) at 65 dB SPL to match the displayed NAL-R prescription within ±3 dB in the frequency range from 500 Hz to 3000 Hz. The target for loud sounds was to amplify tone bursts at 85 dB SPL to a level close to but not exceeding the displayed MPO targets. The target for soft sounds was to amplify speech-like noise at 45 dB SPL so that the 1/3-octave band levels of speech were similar to the listener's thresholds. For the Fonix test box, which analyzes speech-like noise in 79 bands each 100-Hz wide, the soft-sound target was operationalized as no more than 5 dB below displayed thresholds between 250 Hz and 1000 Hz and no more than 15 dB below displayed thresholds at 2000 Hz and 3000 Hz. After initial adjustment of the hearing aid to match real ear targets, the fitting was fine-tuned using subjective assessments in four areas: quality of own voice, bilateral loudness balance, quality of other voices, and general loudness comfort. Adjustments were made if necessary. Program 1 and program 2 were identical except for the directional microphone.
The final fittings (after all adjustments) are summarized in Figures 2, 3, and 4. Average speech is shown in Figure 2 where the mean NAL-R target is compared to the mean real ear aided response (REAR) across frequencies. Figure 2 gives the result for the right ear. The left ear result was essentially identical. Maximum output levels are summarized in Figure 3 where the average OSPL90 value prescribed using the NAL procedure (Dillon & Storey, 1998) is compared with the mean three-frequency average Real Ear Saturation Response. The audibility of soft sounds was assessed by computing the difference between displayed pure tone thresholds (similar to 1/3 octave band levels) and the measured REAR for 45 dB input (corrected to approximate 1/3 octave band levels). The soft-sound results in low-, mid-, and high-frequency bands are given in Figure 4. For some subjects, it was not possible to visualize target and ear canal levels for both MPO and soft sounds on the Fonix output. Consequently, some data are missing for these two variables.
Figure 2.
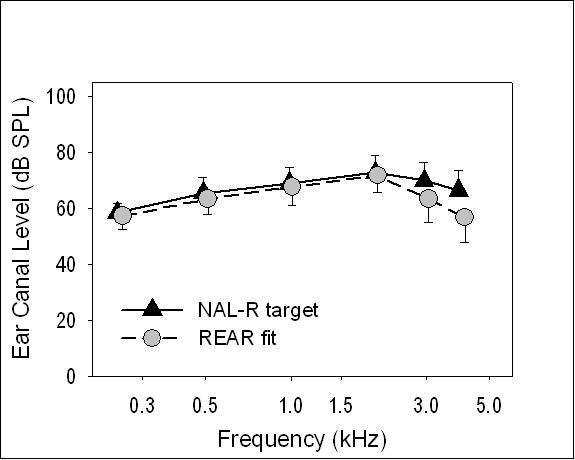
Mean NAL-R target for average speech compared to the mean real ear aided response (REAR) across frequencies. Bars show one standard deviation. Data are for the right ear.
Figure 3.
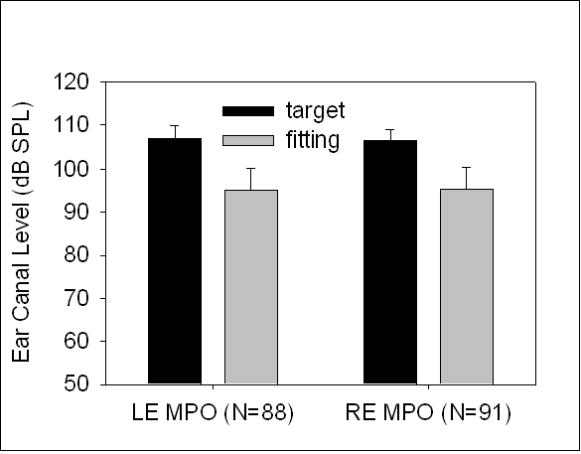
The average OSPL90 value prescribed using the NAL procedure compared with the mean three-frequency average Real Ear Saturation Response (RESR) for each ear. Bars show one standard deviation. N= number of subjects.
Figure 4.
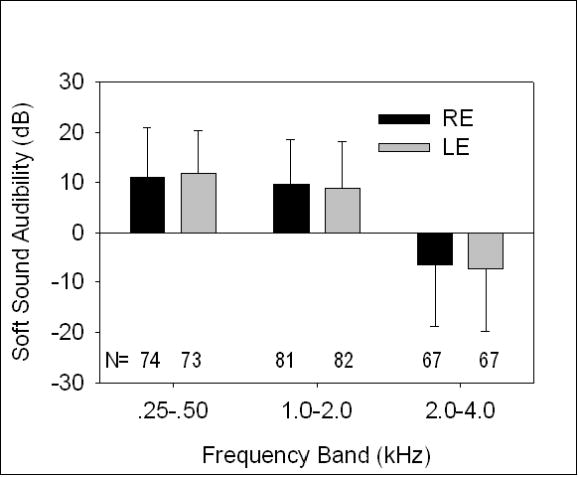
Audibility of soft sounds assessed by computing the difference between pure tone thresholds (similar to 1/3 octave band levels) and the measured REAR for 45 dB speech (in approximate 1/3 octave band levels). Results are given in each ear for low-, mid-, and high-frequency bands. Bars show one standard deviation. N= number of subjects.
After the fittings were complete, verbal instructions were provided about using the hearing aids and a hearing aid orientation booklet containing the same material was given to each subject to take home. The booklet reviewed topics such as adjusting to a hearing aid, replacing batteries, inserting and removing a hearing aid, adjusting hearing aids in noise, telephone use, and hearing aid care and maintenance. Hearing aid insertion, removal, volume and program manipulation were practiced with each subject. The subjects were reminded to wear the hearing aid(s) at least four hours a day.
Field trial and wearing schedule
Following the fitting and orientation to the hearing aids, each subject was given a three-week wearing schedule to ensure that both unilateral and bilateral amplification were experienced in a variety of daily life settings. The wearing schedule encompassed three one-week periods during which each aid was worn unilaterally for one week and both were worn bilaterally for one week. There were six possible orders of the three conditions (left, right, and both). Each block of six consecutive subjects was randomized to the six orders so that all orders were used equally often. During each one-week trial, the subject completed a daily checklist to record the hours of device use and the type of listening situations encountered. The checklists were returned to the researcher at each post-fitting visit.
Post-fit visits were scheduled at the end of weeks 1, 2, and 3. During these visits, the seven daily checklists for the corresponding week were reviewed to ensure that the procedures for the trial had been observed. Also, the appropriate hearing aid(s) were issued for the following week. If the hearing aids needed to be adjusted or repaired during the trial period, the length of the trial was extended to ensure that the intent of the trial was achieved. At the end of the three-week prescribed wearing schedule, the subject was given both hearing aids and instructed to continue to experiment with using the aids in different configurations (right ear, left ear, or both ears), and to continuing wearing the aid(s) for at least four hours a day for the next nine weeks until the final post-fit visit.
Final Session
At the end of the trial, subjects returned to the laboratory to declare their preference for wearing one or two hearing aids in daily life and to complete outcome questionnaires. For the average subject, the total length of the study from fitting to end was 94 days. Ninety percent of the subjects completed the study in the time period of 79-126 days. The shortest length was 74 days and the longest was 161 days. The time variations across subjects occurred due to personal schedules of the subjects and/or problems with the fittings that caused the trial to be extended.
The exit interview included ten verbally delivered questions covering wearing preference in different listening situations. These included: understanding speech in quiet, understanding speech in noise, hearing best over long distances, best sound of own voice, best sound quality, best loudness, best for general use, best localization, least tiring, and most comfortable sound. After these questions the subject declared whether s/he preferred to wear one or two hearing aids overall and his/her level of certainty about that preference on a four point scale from “very uncertain” to “very certain.” The subject was then asked to provide (in his/her own words) the three most important reasons for their choice of one or two hearing aids. Finally, those who preferred to wear one hearing aid completed an additional survey in which they selected from a list of 24 potential reasons derived from literature and experience to indicate any that contributed to their choice (Appendix A).
Outcome questionnaires
These questionnaires were completed following the exit interview. Subjects were instructed to complete the questionnaires to reflect performance their preferred fitting of one or two hearing aids.
International Outcome Inventory for Hearing Aids (IOI-HA)
The IOI-HA is a seven-item instrument used to provide a broad perspective of fitting outcome by sampling different outcome domains such as benefit, quality of life, etc. (Cox, et al. 2000). An eighth item was included to permit allocation of subjects into two groups based on the severity of subjective hearing problems as recommended by Cox, Alexander and Beyer (2003). To encourage the subject to consider the outcome “big picture”, this was the first questionnaire administered. Each item is given a rating of 1-5, with higher ratings indicating a better outcome. Scoring was based on two factors recommended by Cox and Alexander (2002). Factor 1 (“Advantages”) was calculated by summing the scores on four items (use, benefit, satisfaction, and quality of life) and thus had possible scores of 4-20. Factor 2 (“Limitations”) was calculated by summing scores on three items (residual activity limitations, residual participation restrictions, and impact on others) and thus had possible scores of 3-15.
Abbreviated Profile of Hearing Aid Benefit (APHAB)
The APHAB (Cox & Alexander, 1995) is a 24-item questionnaire that measures unaided and aided performance in four six-item subscales: ease of communication, reverberation, background noise, and aversiveness of sounds. In addition, the three subscales that deal with speech communication (ease of communication, reverberation, and background noise) are averaged to produce a global score. The subscales are scored using reported frequency of problems. Scores are computed for unaided and aided listening in each subscale. A higher score is a poorer outcome. In addition, benefit scores are calculated by subtracting the aided subscale score from the corresponding unaided subscale score. For benefit, a higher score is a better outcome. Subjects completed the questionnaire for both unaided and aided listening at the same time.
Device Oriented Subjective Outcome (DOSO) Scale
The DOSO (Cox, Alexander, & Xu, Reference Note 2) is composed of six subscales: speech cues, listening effort, pleasantness, quietness, convenience, and use. Two of the subscales (speech cues and listening effort) have two equivalent forms which were combined in this study to yield a total length of 40 items. The first 37 items focus on how well the hearing aid performs under specific conditions or with certain stimuli. The final three items evaluate hearing aid use. The six subscale scores are calculated by averaging the item responses in each subscale. The possible range of scores is 1-7 for the first five subscales and 1-5 for the Use subscale. A higher score is a better outcome.
At the end of this session, the 62 subjects with loaner hearing aids returned the aids to the researchers, as planned. Subjects who were using hearing aids purchased by the VA did not return them regardless of their preference.
Follow up survey of hearing aid ownership decisions
Three months after the final research session, the 62 subjects who used loaner hearing aids for the study were contacted via telephone or mail, regarding subsequent decisions and actions about obtaining hearing aids. They had not been told to expect this contact. Four subjects could not be reached. The remaining 58 subjects responded to a five-item survey: 1. Have you purchased hearing aids? 2. If yes, how many hearing aids did you purchase (one or two)? 3. If you bought two hearing aids, what percentage of the time do you wear both hearing aids together? 4. If you did not purchase hearing aids, do you plan on obtaining them in the future? 5. If you plan on getting hearing aids, do you plan to get one or two?
Results
This study included open–ended questions, standardized questionnaires, and objective tests. Several different types of analyses were used in the attempt to understand the behavior and motivations of the subjects. In assessing the results, we visually inspected the data for potential trends; computed effect sizes, where appropriate, to evaluate differences in treatment outcomes in a manner that is independent of sample size; and performed null hypothesis significance tests to evaluate the likelihood that observed differences between means would occur if the null hypothesis were true. Most of the analyses involved mixed-model analysis of variance (ANOVA) in which preference for one or two hearing aids served as the categorical factor and the examined experimental variable was the within-subject factor. If the likelihood of the observed difference was less than 5 percent (p<.05), we call that “significant”. If the likelihood was between 5 and 10 percent (p=.1 to .05), we consider that finding to be worthy of mention. All statistical tests were run with SPSS version 14.
Preference for one or two hearing aids
Of the 94 subjects enrolled in the study, 46% (43 subjects) expressed an overall preference for wearing one hearing aid rather than two hearing aids in the final interview. Subjects were asked how certain they were of their hearing aid choice. Their answers are summarized in Figure 5. More than 90% of each group (those who preferred one hearing aid and those who preferred two) was very or reasonably certain about their preference decision. Only one person was very uncertain. Of the subjects who preferred one hearing aid, 29% preferred the right ear, 40% preferred the left ear, and 31% did not have an ear preference (these data were missing for one subject). Mean reported daily hearing aid use was 7.7 hours for subjects who preferred one hearing aid and 8.1 hours for subjects who preferred two. This difference in daily use was not statistically significant. Figure 6 depicts the average audiograms for subjects who preferred one hearing aid and subjects who preferred two. There were no observable or significant differences between these audiograms. Both groups had mean unaided word recognition scores of 78.2 percent. Within the group that preferred one hearing aid, the mean age was 70.4 (sd=7.4), 86 percent were new hearing aid users, and 49 percent were women. Within the group that preferred two hearing aids, the mean age was 69.8 (sd=6.9), 76.5 percent were new hearing aid users, and 31 percent were women. Testing for the significance of difference between proportions determined that the proportions of new and experienced hearing aid users preferring one versus two hearing aids was not significantly different (p=.24, 2-tailed), suggesting that previous experience was not an influential variable in the preference decision. Additional corresponding tests determined that the difference in the proportions of women and men who chose one versus two hearing aids approached significance (p=.084, 2-tailed), suggesting that gender might be an influential variable in the preference decision.
Figure 5.
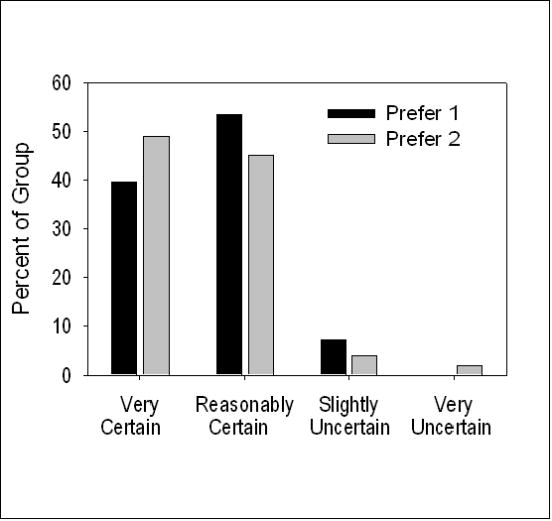
Subject preference for one hearing versus two and the level of certainly of that decision.
Figure 6.
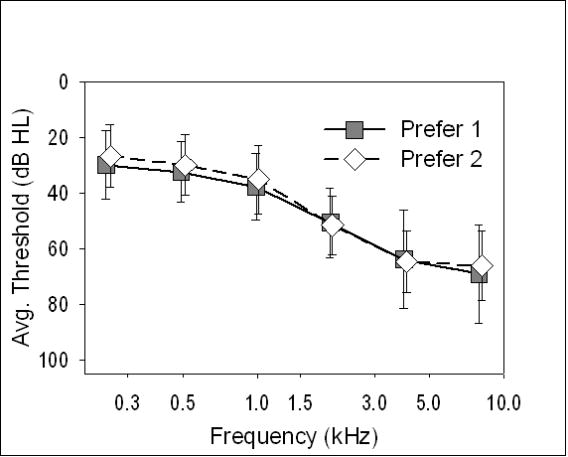
Mean audiogram depicting subjects who selected one hearing aid versus two. Bars show one standard deviation.
Potential Predictors of Preference for One or Two Hearing Aids
In addition to the variables summarized above, the battery of potential predictors of preference for one or two hearing aids comprised three standardized questionnaires measuring lifestyle (ALDQ), personality (PANAS), and subjective hearing problems (unaided APHAB), and three tests of binaural interaction (binaural loudness summation, binaural squelch, and binaural interference). To initially assess the potential leverage of each of these variables as a lone predictor of fitting preference, the performance of each preference group was compared for each predictor.
Auditory Lifestyle and Demand Questionnaire (ALDQ)
Subjects who preferred a unilateral fitting (n=43) reported mean percentages for Lifestyle and Demand of 58.5% (sd =13.6) and 48.9% (sd = 17.1), respectively. Subjects who preferred a bilateral fitting (n=51) reported mean percentages for Lifestyle and Demand of 55.5% (sd =11.3) and 46.9% (sd = 13.5), respectively. ANOVA revealed no significant differences between the two preference groups in mean scores for Lifestyle and Demand (p=.723).
Positive and Negative Affect Schedule (PANAS)
Subjects who preferred one hearing aid reported a mean PA score of 35.5 (sd =5.4) and a mean NA score of 15.2 (sd = 4.7). Subjects who preferred two hearing aids reported a mean PA score of 35.2 (sd =6.2) and a mean NA score of 17.3 (sd = 6.1). ANOVA revealed no significant differences between preference groups in mean scores for PA and NA (p=.289).
Abbreviated Profile of Hearing Aid Benefit – Unaided
The unaided scores for the four subscales of the APHAB and the Global Score (comprising Ease of Communication, Reverberation and Background Noise subscales) are reported in Figure 7 for subjects who preferred one hearing aid and for those who preferred two hearing aids. The subscales EC, RV, and BN are reported for descriptive purposes, but statistical analyses were completed using the Global score and the Aversiveness score. As Figure 7 reveals, there was a consistent pattern in which a lower frequency of problems was reported by subjects who preferred one hearing aid compared to those who preferred two hearing aids. Using ANOVA it was determined that there was a statistically significant interaction between APHAB score and preference group (F (1,92) = 4.028, p=.048). Exploration of this interaction revealed that the mean Global score was significantly higher for the group that preferred two hearing aids (F(1,92) = 5.073, p=.027). The same pattern of mean differences between groups was seen for the AV score, with statistical results approaching significance (F(1,92) = 3.24, p=.075). These results indicate that patients who report fewer unaided problems, especially in speech communication, are more likely to choose one hearing aid rather than two.
Figure 7.
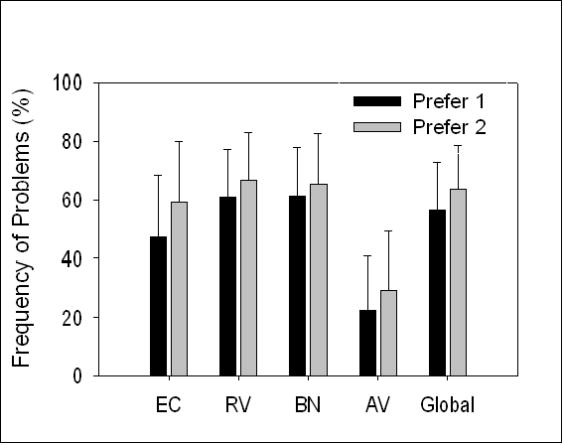
Mean scores for each subscale of the APHAB (Ease of Communication, Reverberation, Background Noise, and Aversiveness to Sounds) and the Global score for subjects who preferred one hearing aid and those who preferred two. Data are given for unaided listening. Bars show one standard deviation.
Tests of Binaural Interaction
Figure 8 summarizes the results of all tests run in the binaural test battery. The results for binaural summation and binaural squelch, scored in decibels, are displayed relative to the left axis. The scores derived from the Dichotic Digits test, scored in percentage, are displayed relative to the right axis. The average scores revealed more binaural summation and greater binaural squelch for the subjects who preferred two hearing aids, suggesting that these listeners experienced somewhat more effective binaural interaction than those who preferred one hearing aid. The statistical significance of these results was explored using ANOVA. There were no significant main effects or interactions, but the main effect of hearing aid preference approached significance (F (1,92) = 3.008, p=.086) which lends some support to the hypothesis that more effective binaural interaction might be one factor that contributes to the preference for wearing one or two hearing aids.
Figure 8.
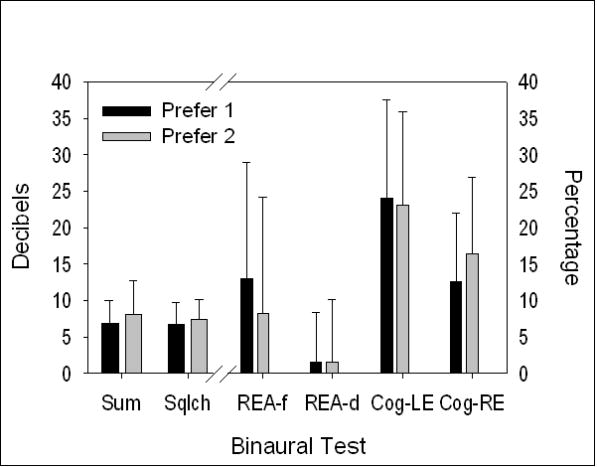
Results from the Binaural Test Battery for each preference group. Means (in dB) for Binaural Summation (SUM) and Binaural Squelch (SQLCH) are referenced to the left axis. Means (in %) for four scores from the Dichotic Digit battery are referenced to the right axis (REA-f=right ear advantage, free recall; REA-d=right ear advantage, direct recall; Cog-LE= cognitive effect, left ear; Cog-RE= cognitive effect, right ear). Bars show one standard deviation.
As described earlier, four scores were computed from the data obtained in the Dichotic Digits test. Right ear advantage (REA) was assessed for both the free recall and the direct recall conditions. The mean data in Figure 8 show that the REA in the direct recall condition was only 1-2 percent and very similar for both preference groups. In the free recall condition, the REA was approximately 10% and a larger REA was seen for subjects who preferred one hearing aid. The statistical significance of these observations was explored using ANOVA. Results indicated that, overall, REA scores were greater for the free recall condition (F(1,92) = 32.8, p<.001). However, there was not a significant main effect for preference groups and the interaction was not significant. The other type of score derived from the Dichotic Digits test was a measure of cognitive effect. The computation of this score is based on the premise that cognitive overload can limit the score in the free recall condition and this limitation can be reduced in the direct recall condition. The difference between the scores from the free and direct recall conditions in one ear is a measure of the cognitive overload effect in that ear. As Figure 8 shows, the mean cognitive effect (Cog) was between 12 and 25 percent and a larger Cog was seen in the left ear than in the right ear. The statistical significance of these observations was explored using ANOVA. Results indicated that, overall, Cog scores were greater for the left ear than for the right ear (F(1,92) = 32.8, p<.001). However, there was not a significant main effect for preference groups and the interaction was not significant.
Optimizing the Prediction of Preference for One or Two Hearing Aids
In the absence of any specific predictors of unilateral/bilateral preference, we could achieve a maximum accuracy of 54% in predicting this preference by simply predicting that all subjects prefer to wear two hearing aids. A major goal of this investigation was to improve the accuracy of this prediction. The topic was explored by determining how accurately the preference for two hearing aids could be predicted based on a combination of variables that would be available in advance of the hearing aid fitting. Although only one of the potential predictor variables discussed above (subjective hearing problems unaided) was independently significantly related to the preference for one or two hearing aids, several other variables revealed trends in the predicted direction that did not reach a significance level of p=.05. It seemed plausible that a combination of predictor variables might be successful in improving the accuracy with which a preference for bilateral fitting could be predicted in advance. Logistic regression analysis was used to examine this possibility.
Logistic regression analysis is a method for finding an optimum combination of variables to predict a dichotomous outcome (preference for one or two hearing aids). In this investigation, there were 16 potential predictor variables. Each one of them arguably could be useful in predicting preference for one or two hearing aids. However, based on the data shown above, some of them seemed more likely to be useful predictors than others. The number of predictor variables was reduced for the analysis by eliminating those that did not explain at least 1 percent of the variance in hearing aid preference. In other words, to be retained for the logistic regression, a variable was required to have a minimum correlation of 0.1 with hearing aid preference. Table 3 gives the correlation coefficient between each potential predictor variable and preference for one or two hearing aids.
Table 3. Linear correlations between potential predictor variables and preference for one or two hearing aids.
| Variable | Correlation coefficient |
|---|---|
| Pure tone average | -.082 |
| Age | -.048 |
| Hearing aid experience | .121 |
| Gender | -.178 |
| Lifestyle | -.021 |
| Demand | -.048 |
| Positive Affect | -.031 |
| Negative Affect | .185 |
| APHAB unaided Global | .229* |
| APHAB unaided AV | .173 |
| Binaural summation | .145 |
| Binaural squelch | .111 |
| REAfree | -.150 |
| REAdirect | -.003 |
| Cognitive effect LE | -.035 |
| Cognitive effect RE | .189 |
P<.05 (2-tailed)
There were nine variables with correlations of at least 0.1 with hearing aid preference. They included two demographic variables (gender and previous hearing aid experience), three subjective assessments (Negative Affect, Unaided AV, and Unaided Global) and four psychoacoustic test scores (binaural summation, binaural squelch, right ear advantage-free, and cognitive effect-right ear). These nine variables were entered into a backward stepwise logistic regression. This procedure systematically discarded variables that did not significantly improve the outcome prediction (p to remove =.1). After the process of eliminating variables that did not produce a significant improvement in the prediction, four variables remained. The logistic regression analysis determined that subject preference for two hearing aids could be predicted with 66% accuracy using these four variables: unaided AV score; unaided global score, binaural summation, and right ear advantage for the free recall portion of the dichotic digits test. Results of the logistic regression are summarized in Table 4.
Table 4. Logistic regression results. When the odds ratio is greater than one, the odds of a preference for two hearing aids increases as the predictor increases. When the odds ratio is less than one, the odds of a preference for two hearing aids decreases as the predictor increases.
| Beta (Std. Error) | Sig. | Odds Ratio | |
|---|---|---|---|
| Unaided AV | .027 (.013) | .035 | 1.027 |
| Unaided Global | .048 (.018) | .007 | 1.049 |
| Binaural Summation | .109 (.06) | .068 | 1.115 |
| REA Free Recall | -.041 (.017) | .016 | .960 |
| Constant | -3.782 (1.253) | .003 | .023 |
R2 = .17(Cox & Snell), . 27(Nagelkerke), χ2(4) =17.39, p=.002)
When these four predictor variables were combined, they accurately predicted preference for one or two hearing aids for two-thirds of the 94 subjects in the study. For one-third of the subjects, the preference prediction was wrong. Figure 9 illustrates the results for each subject. In this figure, the probability score determined from the logistic regression is given on the horizontal axis. Each symbol corresponds to a subject. Subjects who preferred 2 hearing aids are depicted with squares. Subjects who preferred one hearing aid are depicted with circles. Correct predictions are shown using black symbols. Wrong predictions are shown using grey symbols. Among the 32 wrong predictions, 14 represent subjects who preferred 2 hearing aids and 18 represent subjects who preferred one hearing aid.
Figure 9.
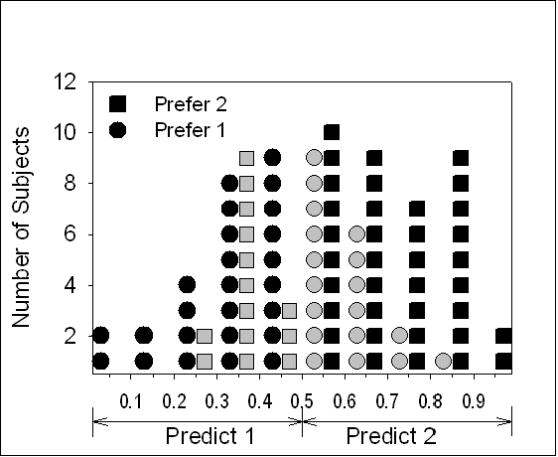
Accuracy of prediction of preference for one hearing aid versus two from the logistic regression model. Subjects who preferred one hearing aid are indicated by circles and subjects who preferred two hearing aids are indicated by squares. Correct predictions are shown with black symbols and incorrect predictions are shown with grey symbols.
Self-Report Outcomes of Preferred Fittings
Three outcome questionnaires were completed to quantify subjective performance with the preferred fitting of one or two hearing aids.
International Outcome Inventory for Hearing Aids (IOI-HA)
Responses to the IOI-HA were partitioned into two factors called Advantages and Limitations. In addition, the data were compiled separately for subjective hearing loss reports of mild-moderate (MM) problems (51 subjects) and moderately-severe or severe (MS+) problems (43 subjects) as recommended by Cox, Alexander and Beyer (2003). Figure 10 summarizes the data for both preference groups. A higher score is a better outcome. It can be seen that for both categories of subjective hearing loss (MM and MS+), the mean Advantages outcome score was higher for the subjects who preferred two hearing aids. The effect sizes (Cohen's d) were .39 and .48 for MM and MS+ categories, respectively. For the Limitations outcomes the result was different across the two subjective hearing loss categories. For the MS+ category, the mean score was higher for the subjects who preferred two hearing aids (Cohen's d=1.07), however, for the MM category the scores were essentially equal for subjects who preferred one and two hearing aids (Cohen's d= -.06). The statistical significance of these results was explored using ANOVA. For the subjects in the MM category there were no significant differences between the preference groups in either Advantages or Limitations. For the subjects in the MS+ category there were no significant differences between the preference groups in the Advantages scores, however, subjects who preferred two hearing aids reported a significantly higher mean score (F(1,41)=10.98, p=.002) for the Limitations factor.
Figure 10.
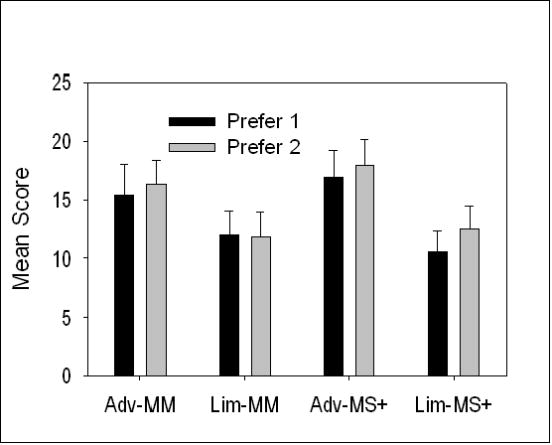
Mean IOI-HA results for subjects who preferred one hearing aid and subjects who preferred two hearing aids. MM= Mild to Moderate, MS+= Moderately-severe to Severe, Adv=Advantages, Lim= Limitations. Bars show one standard deviation.
Device Oriented Subjective Outcome (DOSO)
Responses to the DOSO, scored for each of six subscales, are illustrated in Figure 11 for each hearing aid preference group. A higher score is better. Three subjects accidentally omitted several items on this questionnaire, so the analysis is based on N=91. There is an overall trend suggesting that subjects who preferred two hearing aids reported better average outcomes on 5 of the 6 subscales: Speech Cues (Cohen's d=.32), Listening Effort (Cohen's d=.24), Pleasantness (Cohen's d=.44), Quietness (Cohen's d=.38), and Use (Cohen's d=.31). Subjects who preferred one aid reported better average outcomes on the Convenience subscale (Cohen's d=.39). The statistical significance of these observations was explored using ANOVA. The results revealed a significant interaction between preference and subscale score (F(5,445)=4.88, p=.001, ε =.82, df have been adjusted using the Greenhouse-Geisser correction). Exploration of the interaction using univariate tests indicated that subjects who preferred two hearing aids scored significantly higher on the Pleasantness subscale (F(1,89)=4.30, p=.041). Also, the differences between preference groups approached significance for two other subscales: Quietness (F(1,89)= 3.29, p=.073), and Convenience (F(1,89) = 3.32, p=.072). On the Convenience subscale the mean difference favored the subjects who preferred one hearing aid.
Figure 11.
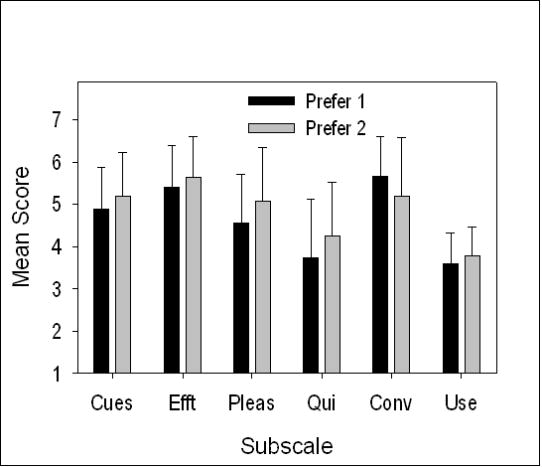
Mean scores on the DOSO for each hearing aid preference group for each subscale: Speech cues (Cues), Listening effort (Efft), Pleasantness (Pleas), Quietness (Qui), Convenience (Conv), and Use (Use). Bars show one standard deviation.
Abbreviated Profile of Hearing Aid Benefit (APHAB)
Figure 12 illustrates the benefit measured using the APHAB for each hearing aid preference group. A higher score is better. For descriptive purposes, the results are displayed for all subscales and for the Global score. The overall trend suggests that subjects who preferred two hearing aids reported greater benefit for speech communication (Cohen's d=.6) and fewer issues with sounds that may be perceived as averse (Cohen's d=.15). The statistical significance of these observations was explored using ANOVA including only the Global and Aversiveness scores. The results revealed a significant overall difference in which subjects who preferred two hearing aids reported more benefit than those who preferred one (F(1,92)=6.58, p=.012). The interaction between APHAB score and hearing aid preference was not significant.
Figure 12.
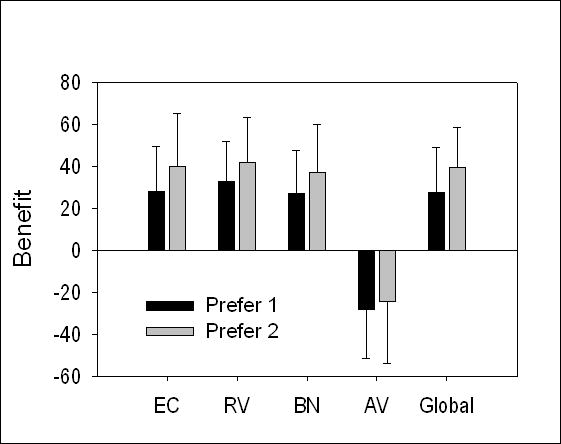
Mean benefit on the APHAB for each hearing aid preference group for each subscale (Ease of Communication, Reverberation, Background Noise, and Aversiveness to Sounds) and the Global score. Bars show one standard deviation.
Why did Some Subjects Prefer One Hearing Aid?
Three types of data were collected to explore the reasons for subjects' preferences for one or two hearing aids:
They were asked for their preference for one or two hearing aids in each of ten listening situations. These data are not further analyzed because subjects tended to give the same preference (for one or two hearing aids) in each situation as their declared overall preference.
They were asked to provide up to three reasons for their preference in their own words. These data were subjected to a content analysis to derive overall themes (Krippendorf, 2004). The results are shown in Figure 13 ordered by reasons most used for preferring one hearing aid.
If they preferred one hearing aid, they were asked to select contributing reasons for the choice from a list of 24 potential reasons (see Appendix A). Five of the reasons were endorsed by at least 50% of the subjects who preferred one hearing aid. These reasons are listed in Table 5.
Figure 13.
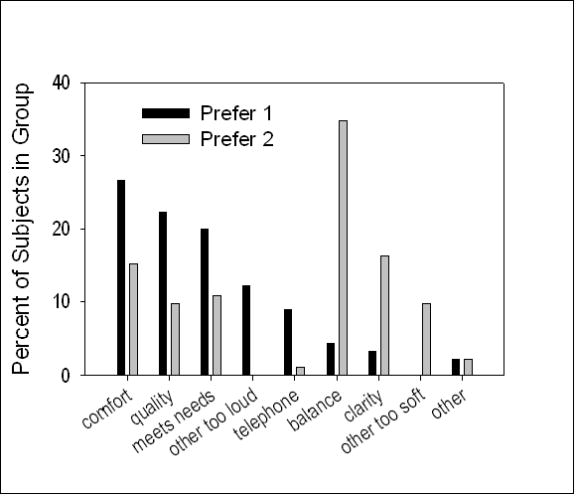
Summary of unstructured reasons given for preferring one or two hearing aids.
Table 5.
Five reasons for preferring one hearing aid that were endorsed by at least 50% of the subjects who preferred one hearing aid.
|
Were Fitting Preferences Stable over Time?
Three months after the study concluded, 58 of the 62 subjects who used loaner hearing aids responded to a short mail or telephone survey about their subsequent purchase decisions. The results are summarized in Table 6. Eight of the subjects had not made any purchase decision. Of the fifty subjects who had made a purchase decision, some had not actually purchased the hearing aids but stated their intention to do so. Among the subjects who had made a purchase decision, 80% reaffirmed their initial preference for one or two hearing aids. Of the remaining 20%, some who preferred two hearing aids actually decided to purchase one, and some who preferred one hearing aid actually decided to purchase two.
Table 6.
Purchase decisions made by 58 subjects three months after the study concluded.
| Initial Decision | |||
|---|---|---|---|
| One aid | Two aids | ||
| Purchase Decision | One aid | 22 | 4 |
| Two aids | 6 | 18 | |
| None | 5 | 3 | |
Discussion
As reviewed above, past research with bilaterally hearing impaired adults consistently has shown that a substantial percentage report a preference for wearing one hearing aid rather than two, even when two are readily available to them. Most of these studies were performed in an era when hearing aids were technologically far inferior to those available now. One goal of the present study was to determine whether this preference pattern continues when patients use devices that are typical of current technology. The hearing aids worn by subjects in this investigation were new in 2005-2007 and exemplified good quality advanced technology. Nevertheless, the pattern in which a large proportion of patients ultimately preferred to wear one hearing aid rather than two was repeated in our results. This outcome indicates that the preference observed in previous research for wearing one hearing aid was not primarily driven by technological limitations. It is also noteworthy that the percentage of subjects who ultimately preferred one hearing aid in our study, 46%, is quite similar to the average of 41% found in previous clinical trials of one versus two hearing aids.
Outcomes with bilateral versus unilateral hearing aids
The strongest argument typically used in favor of bilateral fitting is that patients who use two hearing aids tend to have better real world outcomes than those who use one. However, this claim was not generally supported in studies predating the current technology era beginning around 2000. In particular, the most highly desired benefit of bilateral fitting, improved speech understanding in noise, could not be demonstrated consistently in everyday life (for a review, see Noble, 2006). Noble and Gatehouse (2006) argued that the paucity of evidence supporting advantages of bilateral fittings in daily life was the result of an over-simplified measurement strategy. They attempted to provide a more nuanced insight into potential advantages of bilateral aiding using the Speech, Spatial and Qualities of Hearing (SSQ) questionnaire. Their data suggested that even when significant binaural advantages could not be seen in conventional situations such as speech understanding in noise, they could be seen in dynamic listening situations such as identifying movement of sounds.
The results of the current investigation with more technologically advanced hearing aids tend to support conventional wisdom (ideas that are generally accepted as true) that patients who wear two hearing aids report better real world outcomes. Note however, that in our analyses subjects were categorized based on their own preferences. It is likely that bilaterally aided subject groups in previous studies included some individuals who actually would have preferred to wear one hearing aid. We used three standardized questionnaires to quantify outcomes for subjects who preferred one or two hearing aids. The content of the questionnaires encompassed general impressions such as benefit and pleasantness of sound as well as more specific topics such as speech understanding in quiet and noise. As illustrated in Figures 10, 11, and 12, responses to all three questionnaires reveal binaural advantages in that they show a trend for better outcomes in those subjects who preferred two hearing aids. These results are consistent with some outcomes in other recent studies. For example, Kramer et al. (2002) found that scores on the Advantages subscale of the IOI-HA were significantly better for wearers of two hearing aids than for wearers of one. Although their effect size was small (d≅.2), the large number of subjects (N=505) produced a statistically significant difference. We replicated this outcome in the present study where the scores for the Advantages subscale were better for subjects who preferred two hearing aids, with an effect size d≅.4. This result was statistically significant in the present study when all subjects were pooled, even though it was not significant when subjects were partitioned into the two hearing loss groups (Figure 10). Boymans et al. (2009) reported mixed results. With one set of questionnaires, significantly greater real world benefit was seen for patients who opted for two hearing aids rather than one. However, there was not a significant advantage for bilateral fittings in the results of the IOI-HA.
The protocol followed in this investigation (as in Boymans et al, 2009) was designed to facilitate a search by each listener to identify the amplification system that would provide him/her with the most benefit and overall satisfaction, taking into account all the complexities of the individual's life, including the many circumstances that are not explored by standardized questionnaires. The results of our investigation, and the great majority of previous comparable studies, show that when faced with this decision a substantial proportion of bilaterally hearing-impaired persons decide that their optimal amplification system includes one hearing aid rather than two. Why do they make this choice, and can we predict it in advance of the fitting?
Predictors of preference for a unilateral hearing aid fitting
As seen in Table 3, there were 16 a priori potential predictors of preference for bilateral aiding in this study. They were drawn from conventional wisdom as well as from research with normal-hearing and hearing-impaired groups of listeners. The statistical exploration of these data yielded a finding that the preference for one or two hearing aids could be predicted accurately for about two-thirds of patients using four variables (Table 4). The combination of useful variables reinforced several aspects of conventional wisdom and basic research.
Conventional wisdom suggests that patients who have more hearing problems are more likely to appreciate two hearing aids. In this study, scores from the unaided APHAB quantified the extent to which the subject believed that the hearing loss caused problems in daily life. A report of more problems was associated with greater likelihood of preferring two hearing aids. This trend was also reported by previous researchers (e.g., Stephens et al, 1991; Boymans et al, 2009)
Many practitioners have argued in favor of bilateral aiding based on the well-established advantages of binaural listening for normal-hearing listeners. In this study, one of those advantages (binaural summation of loudness) was found to make a positive contribution to the preference for two hearing aids: greater binaural loudness summation was predictive of a preference for two rather than one.
Several researchers have suggested that scores obtained in dichotic listening tests can reflect interference or imbalance between ears and that this might be consistent with a deficit in binaural benefits which, in turn, limits the advantages of two hearing aids. Our finding that a greater right ear advantage in dichotic listening was associated with lower preference for two hearing aids bolsters this line of reasoning. Overall, a preference for two hearing aids rather than one was predictable from a combination of more perceived daily problems, greater binaural advantage, and less binaural imbalance.
It is also noteworthy that our investigation failed to confirm the validity of two additional variables that often have been put forward as predictive of a preference for bilateral aiding: audiometric hearing loss and auditory lifestyle. It is widely claimed that individuals with more objective hearing impairment are more likely to prefer two hearing aids. However, in this study, the mean audiogram for subjects who preferred two hearing aids was essentially identical to the mean audiogram for those who preferred one (Figure 6). In support of this, pure tone average thresholds were not significantly correlated with aiding preference (Table 3). This finding cannot be generalized beyond the scope of the specific audiograms encompassed in this study. Although our subjects represented a wide range of audiograms typical of hearing aid users with mild to moderate hearing loss, there were no subjects with severe or profound hearing loss (the poorest 3-frequency pure tone average was 60 dB HL). In addition, there were no subjects with bilaterally asymmetrical audiograms. Other studies also have reported that hearing impairment quantified using the audiogram was not predictive of a preference for one or two hearing aids (e.g., Schreurs and Olsen, 1985; Day et al. 1988; Vaughan-Jones et al. 1993). However, some researchers have observed that more hearing loss is predictive of opting for two hearing aids (Chung & Stephens, 1986; Stephens et al. 1991).
Another widely cited rationale for preferring one or two hearing aids involves the extent to which the patient's daily life calls for frequent interaction with different types of sounds (e.g., attending performances, group conversations, shopping, driving, picnics, TV, library job, children). This variable is often called auditory lifestyle (other terms that have been used include listening needs, activity index, auditory ecology, and hearing demands). Based on conventional wisdom, an individual with a more demanding auditory lifestyle will be more likely to prefer two hearing aids. Previous studies of preference for one or two hearing aids have not directly assessed this variable, although Kobler et al (2001) found some indirect support for the proposition. In the present investigation, auditory lifestyle was quantified using the Auditory Lifestyle and Demand Questionnaire. The ALDQ yields one score that reflects the variety of sounds in an individual's daily life and a second score that weights these sounds in terms of their importance for the listener. Neither of these scores provided significant leverage in predicting which subjects would prefer to use two hearing aids (Table 3). This finding indicates either that auditory lifestyle is not an important predictor of preference for two hearing aids, or that the ALDQ does not quantify the relevant aspects of auditory lifestyle. Although the ALDQ has not been widely used, research has tended to support its construct validity. ALDQ scores have been shown to be associated with preference for linear versus non-linear processing and with amplification subjective outcomes (Gatehouse et al. 1999, 2006; Vestergaard, 2006). Taking another approach to this question, Shaughnessy and Cox (Reference Note 3) explored auditory ecology using three approaches in addition to the ALDQ for a convenience sample of 34 subjects from the current study during a typical week. The three types of measures were: (1) acoustical measurements to determine the distribution of levels of speech, noise, and speech-in-noise; (2) checklist of daily listening situations; (3) checklist of language activities. None of these measures revealed a difference in auditory ecologies between the 14 subjects in this group who preferred two hearing aids and the 20 who preferred one. This is an additional indication that auditory lifestyle might not be predictive of a preference for two hearing aids.
Additional reasons for preferring one or two hearing aids
Using four of the variables that were selected a priori as potential predictors of a preference for two hearing aids, it was possible to correctly categorize two-thirds of the subjects regarding their preference. However, 18 subjects who were predicted to prefer two hearing aids actually chose one, and 14 subjects who were predicted to prefer one hearing aid actually chose two (Figure 9). To further explore their underlying motivations, all subjects were asked to provide in their own words up to three reasons for their choice of one or two hearing aids. Figure 13 summarizes these data and clearly demonstrates that subjects who preferred one hearing aid used very different decision criteria from those who preferred two. The three most frequently cited reasons for preferring one hearing aid were more comfort, better quality, and “it is enough to meet my needs”. These subjects seemed to indicate that help provided by one hearing aid was “good enough” and they found persuasive advantages (such as easy telephone use) in having one ear left open. Amplified sound in the second ear did not yield benefits sufficient to overcome disadvantages related to quality, comfort, and loudness (even though volume controls were provided). This impression is supported by the five reasons listed in Table 5 which can be summarized as: Two hearing aids did not help more than one and sometimes were worse.
The three most frequently cited reasons for preferring two hearing aids were: feeling balanced, clarity of sounds, and comfort. These kinds of reasons are familiar and anticipated by conventional wisdom. The reference to balance is consistent with clinical anecdotes about a need for sound in both ears to achieve a sense of stability in space as well as research that points to a need for bilateral input to execute auditory scene analysis (e.g., Noble & Gatehouse, 2006). Further, references to clarity of sounds are consistent with expectations about binaural processing with bilateral fitting: normal hearing listeners can achieve substantially improved effective signal-to-noise ratios with two-ear listening. It is interesting to note that greater comfort was among the three top reasons given for their preference by both groups of subjects. However, the components of comfort were subtly different in the two groups. Explication of comfort by subjects who preferred one hearing aid included feeling more normal and free, not closed in, plugged, or cut off. In contrast, subjects who preferred two hearing aids described comfort as feeling more capable, secure, relaxed and safe.
Other considerations
Hearing Aid Fittings
As described earlier, the process of hearing aid fitting was the same for all subjects. After target matching, the fittings were fine-tuned to ensure that they would be acceptable for each subject. It is reasonable to ask whether the patient-driven fine tuning process resulted in systematic differences in the final fittings for subjects who subsequently preferred two hearing aids versus those who preferred one. Three small differences did emerge. (1) The typical subject who preferred one hearing aid chose average gain for conversational speech equal to 97% of his/her target gain whereas the corresponding value for subjects who preferred two hearing aids was 98% of his/her target gain. This difference approached statistical significance (t(89) = 1.97, p = .052). (2) The average MPO was 13.6 dB below average target for subjects who preferred one hearing aid whereas it was 10.1 dB below target for subjects who preferred two. This 3.5 dB mean difference was statistically significant (t(84) = 3.45, p = .001). (3) Mid-frequency audibility of soft speech was 6.6 dB for the average subject who preferred one hearing aid whereas it was 10.7 dB for the average subject who preferred two. This 4.1 dB mean difference was statistically significant (t(77) = 2.12, p = .037). All of these subject-driven differences are consistent in suggesting that, compared to those who preferred two hearing aids, individuals who preferred one hearing aid had a lower tolerance for sound. Recall, however, that all hearing aids were provided with volume controls which could have been used to change gain levels during the field trial.
Open fittings
When this investigation was undertaken, open fittings were not widely used. The behind-the-ear hearing aids used in this study were coupled to the ear canal using ear molds with appropriate venting and feedback management. Given the success of open fittings in the past few years, it is natural to wonder whether the results of this study would have changed if open fittings had been used for some of the subjects, consistent with current clinical practice. It could be speculated that more openness in the ear canal coupling would have promoted greater acceptance of two hearing aids among subjects who preferred one in this study. Although we cannot resolve this matter with the current data, it is possible to consider any differences in the venting configuration between subjects who preferred one hearing aid or two. Specific information about the venting used for each person was available only for the HARL subjects. Their ear mold vents were measured using length, and diameter. For subjects who preferred two hearing aids, the mean length × diameter of the vents were 16.7 mm × 2.9 mm. For subjects who preferred one hearing aid, the mean length × diameter of the vents were 17.5 mm × 2.8 mm. Thus, the vents were similar for both groups, on average. Additional research will be necessary to determine the effect, if any, of open fittings on preference for one or two hearing aids.
Financial considerations
The cost of purchasing hearing aids is often noted as one of the reasons patients choose to wear one rather than two. It should be emphasized that these sorts of concerns did not play a part in this study. There was never a question of the subjects purchasing any of the hearing aids that they wore. The only time in which financial issues could have come into play was in the subjects' decisions about whether they would purchase one or two hearing aids. These decisions were undertaken after the study was completed and did not involve anyone associated with the research. As seen in Table 6, several subjects who had preferred two hearing aids ultimately decided to purchase one. This decision could have been impacted by financial considerations but it is not pertinent to the validity of our data.
Relevance for Clinical Practice
Evidence-based practice calls for a conscientious melding of current evidence, clinical judgment, and patient preferences. The results of this investigation reinforce and extend several decades of previous research on the preference for one or two hearing aids. The evidence in this and previous studies points to the conclusion that bilateral aiding is not necessarily the patient-centered treatment for all adults with mild to moderate bilaterally symmetrical hearing loss. It is reasonable to believe that regardless of practitioner inclination, at least 30-40% of these patients will ultimately decide that they prefer to wear one hearing aid.
Practitioners might be concerned about their ethical responsibilities towards patients who do not comply with a professional recommendation to wear two hearing aids. Since listeners who opt for two hearing aids tend to report better amplification outcomes on standardized questionnaires, practitioners might feel obligated to try to persuade listeners who opt for one hearing aid to change their minds and accept wearing two, in the hopes of achieving better outcomes in daily life. After all, at the very least, using two hearing aids will always give relief from head shadow effects. On the other hand, respect for patient decisions about their own treatment is a fundamental value in health care. In dealing with this kind of quandary, it is helpful to consider some theory about patient decision-making and compliance with treatment recommendations. Stewart and DeMarco (2006) presented a compelling theoretical approach to this topic that makes several important points: (1) Fully informed rational patients will attempt to maximize the net benefit of treatments. (2) Net benefit is the difference between treatment benefits (such as decrease in symptoms of hearing loss) and treatment burdens (such as money, aggravation, stigma, and discomfort of using hearing aids). The benefits and burdens of treatment differ across individuals and the treatment point at which net benefit is maximized likewise differs. (3) For many individuals, net benefit is maximized at a point that is well below the ideal treatment level recommended by professionals. Application of this theory to the present situation points to the conclusion that there will be patients for whom the decision to wear one hearing aid rather than the recommended two (noncompliance) is fully rational and, therefore, should be respected. The practitioner does have the ethical responsibility to make sure that the patient has accurate and clear information to bring to the decision-making process. This can be achieved using informational counseling as well as real life trials.
The goal of clinical practice should be to arrive at the most effective treatment that is compatible with patient preferences as expeditiously as possible and with maximum cost-effectiveness for patient, practitioner, and any third party payer. In current practice, it is typical to recommend two hearing aids for essentially all patients with mild to moderate symmetrical hearing loss. Then, over time, the patient determines whether he/she prefers to wear both of the purchased hearing aids or only one. If a substantial percentage of patients ultimately decide to wear only one device, this practice model is not expeditious for the patient or cost-effective for the payer.
How can clinical practice with respect to fitting one or two hearing aids be made more expeditious and cost effective? The ideal solution would be a short battery of clinical tests that could predict patient preference. The results of our study suggest that a battery of three clinical tests (unaided APHAB, binaural loudness summation, and free-recall dichotic digit test) could yield accurate prediction of aiding preference for two-thirds of patients with mild to moderate bilateral hearing loss, but this level of precision is not enough to justify a recommendation to use the battery in clinical settings. Perhaps further refinement of the predictive method can be achieved with additional research. In the meantime, however, there is no accurate way to predict in advance the aiding preference for a particular individual. At this time, the most effective approach open to practitioners would be to conduct a candid unbiased systematic field trial comparing unilateral and bilateral fittings with each patient, as has been recommended by several previous researchers (e.g., Schreurs and Olsen, 1985; Vaughan-Jones et al. 1993; Boymans et al. 2009). This would necessitate more fitting sessions and perhaps add to the practitioner's burden, but this downside should be weighed against the additional patient satisfaction that can be anticipated as a result of transparency in the fitting protocol, collaboration with the patient in the treatment decisions, and the knowledge of selecting the most cost-effective patient-centered solution. A satisfied patient is an important source of positive word of mouth advertising.
Although a patient's decision about his/her own best treatment must be respected, there are some caveats associated with the choice to wear one hearing aid rather than two. Patients who prefer and wear one hearing aid are potentially vulnerable to a deprivation effect in the unaided ear. In this condition, ability to recognize words declines in the unaided ear over time, even though audiogram thresholds remain symmetrical in the patient's two ears (Silman, Gelfand, & Silverman, 1984). As shown by Hurley (1999), about 25% of wearers of one hearing aid developed a deprivation effect after five years of hearing aid use, with the effect more likely in patients whose hearing loss is moderate or worse. Although the real world consequences of this laboratory effect have not been reported, there is clearly some change in the processing ability of the unaided ear in these individuals. Several researchers have observed that this effect often can be reversed at least partly if amplification is subsequently applied to the deprived ear (e.g. Silverman & Silman, 1990; Gelfand, 1995). Another relevant issue was brought to light by Gianopoulos and Stephens (2002) who found that patients who opted for one hearing aid rather than two were more likely to reject amplification over time. They suggested that patients who opt for one hearing aid might need more ongoing professional support to promote continued use of amplification. These considerations suggest that it would be important to follow patients who opt for one hearing aid even more closely than those who opt for two.
Conclusions
When adults with mild to moderate bilaterally symmetrical hearing loss were given an opportunity to experience unilateral and bilateral hearing aid fittings in their daily lives, a substantial percentage of them decided that they preferred to use the unilateral fitting. This result with modern technology hearing aids is consistent with many previous studies using older technology devices. Several widely accepted ideas about use of two hearing aids were at least partly supported in this study: subjects who reported more hearing problems in daily life, who experienced more binaural loudness summation, and whose ears were more equivalent in dichotic listening were more likely to prefer to use two hearing aids. In addition, subjects who preferred to use two hearing aids tended to report better real world outcomes and the mean effect size associated with this preference averaged across outcome measures was respectable at d=.40 (range .06 to 1.07). However, it is critical to note that this result was found when individuals who preferred to use two hearing aids were compared with individuals who preferred to use one hearing aid. Other widely believed ideas about use of two hearing aids were not supported in this study. Hearing loss measured by the audiogram was not predictive of preference for one or two hearing aids (although none of the subjects had severe or worse hearing loss). Auditory lifestyle also was not predictive of aiding preference. Finally, an analysis of reasons volunteered by subjects for their preference choice showed that the two groups of subjects tended to use different decision criteria.
It is self-evident, and consistent with previous research, that patients who develop a preference for one hearing aid will use only one hearing aid even when they have purchased (or otherwise obtained) two. The challenge for practitioners, therefore, is to recognize the existence of this tendency in many patients and to attempt to provide the most clinically effective and cost-effective hearing aid fitting that is consistent with the patient's preferences. Variables drawn from conventional wisdom and basic research were explored in this study in an attempt to develop an accurate method that could be applied pre-fitting to predict preference for one or two hearing aids in a given patient. Although results indicated that some of the variables provided some leverage, we were not able to devise a method with sufficient accuracy for clinical use. The prediction was wrong for one-third of the research subjects. Further research is needed to generate a more accurate predictive approach that could be clinically applicable. In the meantime, it is recommended that practitioners are candid and unbiased in exploring patient preference for one or two hearing aids before the fitting is finalized.
Acknowledgments
This research was supported by funding from NIH-NIDCD R01DC006222: “Optimizing Hearing aid fitting for Older Adults”. Jennifer Goshorn, Jeannie Lilly, and Christine Powers assisted with data collection. The contents do not represent the views of the Department of Veterans Affairs or the United States Government
Appendix A: Potential reasons for preferring to wear one hearing aid rather than two
|
References
- Akeroyd MA. The psychoacoustics of binaural hearing. Int J Audiol. 2006;45 1:S25–33. doi: 10.1080/14992020600782626. [DOI] [PubMed] [Google Scholar]
- Boymans M, Goverts ST, Kramer SE, Festen JM, Dreschler WA. Candidacy for bilateral hearing aids: a retrospective multicenter study. J Speech Lang Hear Res. 2009;52(1):130–140. doi: 10.1044/1092-4388(2008/07-0120). [DOI] [PubMed] [Google Scholar]
- Brooks DN, Bulmer D. Survey of binaural hearing aid users. Ear and Hearing. 1981;2(5):220–224. doi: 10.1097/00003446-198109000-00008. [DOI] [PubMed] [Google Scholar]
- Byrne D, Noble W, LePage B. Effects of long-term bilateral and unilateral fitting of different hearing aid types on the ability to locate sounds. Journal of the American Academy of Audiology. 1992;3(6):369–382. [PubMed] [Google Scholar]
- Carter AS, Noe CM, Wilson RH. Listeners who prefer monaural to binaural hearing aids. Journal of the American Academy of Audiology. 2001;12:261–272. [PubMed] [Google Scholar]
- Chmiel R, Jerger J. Hearing aid use, central auditory disorder, and hearing handicap in elderly persons. J Am Acad Audiol. 1996;7(3):190–202. [PubMed] [Google Scholar]
- Chmiel R, Jerger J, Murphy E, Pirozzolo F, Tooley-Young C. Unsuccessful use of binaural amplification by an elderly person. Journal of the American Academy of Audiology. 1997;8:1–10. [PubMed] [Google Scholar]
- Chung SM, Stephens SDG. Factors influencing binaural hearing aid use. British Journal of Audiology. 1986;20:129–140. doi: 10.3109/03005368609079006. [DOI] [PubMed] [Google Scholar]
- Cox RM, Alexander GC. The Abbreviated Profile of Hearing Aid Benefit. Ear and Hearing. 1995;16(2):176–186. doi: 10.1097/00003446-199504000-00005. [DOI] [PubMed] [Google Scholar]
- Cox RM, Alexander GC. The International Outcome Inventory for Hearing Aids (IOI-HA): Psychometric Properties of the English Version. International Journal of Audiology. 2002;41(1):30–35. doi: 10.3109/14992020209101309. [DOI] [PubMed] [Google Scholar]
- Cox RM, Alexander GC, Beyer CM. Norms for the International Outcome Inventory for Hearing Aids. Journal of the American Academy of Audiology. 2003;14(8):404–413. [PubMed] [Google Scholar]
- Cox RM, Alexander GC, Gilmore CA. Development of the Connected Speech Test (CST) Ear and Hearing. 1987;8(suppl):119S–126S. doi: 10.1097/00003446-198710001-00010. [DOI] [PubMed] [Google Scholar]
- Cox RM, Alexander GC, Taylor IM, Gray GA. The Contour test of loudness perception. Ear and Hearing. 1997;18:388–400. doi: 10.1097/00003446-199710000-00004. [DOI] [PubMed] [Google Scholar]
- Cox RM, Hyde M, Gatehouse S, Noble W, Dillon H, Bentler R, et al. Optimal Outcome Measures, Research Priorities, and International Cooperation. Ear and Hearing. 2000;21(4 (Supplement)):106S–115S. doi: 10.1097/00003446-200008001-00014. [DOI] [PubMed] [Google Scholar]
- Day GA, Browning GG, Gatehouse S. Benefit from binaural hearing aids in individuals with severe hearing impairment. British journal of Audiology. 1988;22(4):273–277. doi: 10.3109/03005368809076464. [DOI] [PubMed] [Google Scholar]
- Dermody P, Byrne D. Loudness summation with binaural hearing aids. Scandinavian Audiology. 1975;4:23–28. [Google Scholar]
- Dillon H, Birtles G, Lovegrove R. Measuring the outcomes of a national rehabilitation program: Normative data for the Client Oriented Scale of Improvement (COSI) and the Hearing Aid User's Questionnaire (HAUQ) Journal of the American Academy of Audiology. 1999;10(2):67–79. [Google Scholar]
- Dillon H, Storey L. The National Acoustic Laboratories procedure for selecting the saturated sound pressure level of hearing aids: theoretical derivation. Ear and Hearing. 1998;19(4):255–266. doi: 10.1097/00003446-199808000-00001. [DOI] [PubMed] [Google Scholar]
- Erdman SE, Sedge RK. Subjective Comparisons of Binaural versus Monaural Amplification. Ear and Hearing. 1981;2(5):225–229. doi: 10.1097/00003446-198109000-00009. [DOI] [PubMed] [Google Scholar]
- Freyaldenhoven MC, Plyler PN, Thelin JW, Burchfield SB. Acceptance of noise with monaural and binaural amplification. J Am Acad Audiol. 2006;17(9):659–666. doi: 10.3766/jaaa.17.9.5. [DOI] [PubMed] [Google Scholar]
- Gatehouse S, Elberling C, Naylor G. Aspects of auditory ecology and psychoacoustic function as determinants of benefits from and candidature for non-linear processing in hearing aids. In: Rasmussen A, Andersen P, Poulsen T, editors. Auditory Models and Non-linear Instruments. Holmens Trykkeri; Denmark: 1999. pp. 221–233. [Google Scholar]
- Gatehouse S, Naylor G, Elberling C. Linear and nonlinear hearing aid fittings--2. Patterns of candidature. Int J Audiol. 2006;45:153–171. doi: 10.1080/14992020500429484. [DOI] [PubMed] [Google Scholar]
- Gelfand SA. Long-term recovery and no recovery from the auditory deprivation effect with binaural amplification: six cases. J Am Acad Audiol. 1995;6(2):141–149. [PubMed] [Google Scholar]
- Gianopoulos I, Stephens D. Opting for two hearing aids: a predictor of long-term use among adult patients fitted after screening. Int J Audiol. 2002;41(8):518–526. doi: 10.3109/14992020209056072. [DOI] [PubMed] [Google Scholar]
- Grose JH, Poth EA, Peters RW. Masking level differences for tones and speech in elderly listeners with relatively normal audiograms. Journal of Speech and Hearing Research. 1994;37(2):422–428. doi: 10.1044/jshr.3702.422. [DOI] [PubMed] [Google Scholar]
- Hawkins DB, Yacullo WS. Signal-to-noise ratio advantage of binaural hearing aids and directional microphones under different levels of reverberation. Journal of Speech and Hearing Disorders. 1984 Aug;49(3):278–286. doi: 10.1044/jshd.4903.278. [DOI] [PubMed] [Google Scholar]
- Humes LE, Coughlin M, Talley L. Evaluation of the use of a new compact disc for auditory perceptual assessment in the elderly. Journal of the American Academy of Audiology. 1996;7(6):419–427. [PubMed] [Google Scholar]
- Hurley RM. Onset of auditory deprivation. J Am Acad Audiol. 1999;10(10):529–534. [PubMed] [Google Scholar]
- Jerger J, Alford B, Lew H, Rivera V, Chmiel R. Dichotic listening, event-related potentials, and interhemispheric transfer in the elderly. Ear and Hearing. 1995;16(5):482–498. doi: 10.1097/00003446-199510000-00005. [DOI] [PubMed] [Google Scholar]
- Jerger J, Brown D, Smith S. Effect of peripheral hearing loss on the masking level difference. Archives of Otolaryngology. 1984;110(5):290–296. doi: 10.1001/archotol.1984.00800310014003. [DOI] [PubMed] [Google Scholar]
- Jerger J, Silman S, Lew HL, Chmiel R. Case studies in binaural interference: converging evidence from behavioral and electrophysiologic measures. Journal of the American Academy of Audiology. 1993;4(2):122–131. [PubMed] [Google Scholar]
- Jerger J, Stach B, Johnson K, Loiselle L, Jerger S. Patterns of abnormality in dichotic listening in the elderly. In: Jensen JH, editor. Presbycusis and other age related aspects. Denmark: Danavox; 1990. pp. 143–150. [Google Scholar]
- Johansson MS, Arlinger SD. Binaural masking level difference for speech signals in noise. International Journal of Audiology. 2002;41(5):279–284. doi: 10.3109/14992020209077187. [DOI] [PubMed] [Google Scholar]
- Kiessling J, Muller M, Latzel M. Fitting strategies and candidature criteria for unilateral and bilateral hearing aid fittings. Int J Audiol. 2006;45 1:S53–62. doi: 10.1080/14992020600782808. [DOI] [PubMed] [Google Scholar]
- Kobler S, Rosenhall U, Hansson H. Bilateral hearing aids - effects and consequences from a user perspective. Scandinavian Audiology. 2001;30:223–235. doi: 10.1080/01050390152704742. [DOI] [PubMed] [Google Scholar]
- Kochkin S. MarkeTrak VIII: 25-year trends in the hearing health market. Hearing Review. 2009;16(11):12–31. [Google Scholar]
- Kochkin S, Kuk F. The binaural advantage: Evidence from subjective benefit and customer satisfaction data. The Hearing Review. 1997;4(4):29–34. [Google Scholar]
- Koenig W. Subjective effects in binaural hearing. Journ Acoust Soc Amer. 1950;22(1):61–62. [Google Scholar]
- Kramer SE, Goverts ST, Dreschler WA, Boymans M, Festen JM. International Outcome Inventory for Hearing Aids (IOI-HA): results from The Netherlands. Int J Audiol. 2002;41(1):36–41. doi: 10.3109/14992020209101310. [DOI] [PubMed] [Google Scholar]
- Krippendorf K. Content Analysis: An Introduction to Its Methodology. 2nd. Thousand Oaks: Sage; 2004. [Google Scholar]
- McCrae RR, Costa PT. Personality trait structure as a human universal. American Psychologist. 1997;52(5):509–516. doi: 10.1037//0003-066x.52.5.509. [DOI] [PubMed] [Google Scholar]
- Noble W. Bilateral hearing aids: a review of self-reports of benefit in comparison with unilateral fitting. Int J Audiol. 2006;45 1:S63–71. doi: 10.1080/14992020600782873. [DOI] [PubMed] [Google Scholar]
- Noble W, Gatehouse S. Effects of bilateral versus unilateral hearing aid fitting on abilities measured by the Speech, Spatial, and Qualities of Hearing Scale (SSQ) Int J Audiol. 2006;45(3):172–181. doi: 10.1080/14992020500376933. [DOI] [PubMed] [Google Scholar]
- Noffsinger D. Clinical applications of selected binaural effects. Scandinavian Audiology. 1982;15(Suppl):157–165. [PubMed] [Google Scholar]
- Schreurs KK, Olsen WO. Comparison of monaural and binaural hearing aid use on a trial period basis. Ear and Hearing. 1985;6(4):198–202. doi: 10.1097/00003446-198507000-00005. [DOI] [PubMed] [Google Scholar]
- Silman S, Gelfand SA, Silverman CA. Late-onset auditory deprivation: effects of monaural versus binaural hearing aids. J Acoust Soc Am. 1984;76(5):1357–1362. doi: 10.1121/1.391451. [DOI] [PubMed] [Google Scholar]
- Silverman CA, Silman S. Apparent auditory deprivation from monaural amplification and recovery with binaural amplification: two case studies. J Am Acad Audiol. 1990;1(4):175–180. [PubMed] [Google Scholar]
- Stephens SD, Callaghan DE, Hogan S, Meredith R, Rayment A, Davis A. Acceptability of binaural hearing aids: a cross-over study. Journal of the Royal Society of Medicine. 1991;84(5):267–269. doi: 10.1177/014107689108400508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steven Colburn H, Shinn-Cunningham B, Kidd G, Jr, Durlach N. The perceptual consequences of binaural hearing. Int J Audiol. 2006;45 1:S34–44. doi: 10.1080/14992020600782642. [DOI] [PubMed] [Google Scholar]
- Stewart DO, DeMarco JP. An economic theory of patient decision-making. Journal of Bioethical Inquiry. 2006;2:153–164. doi: 10.1007/BF02448596. [DOI] [PubMed] [Google Scholar]
- Swan IR. The acceptability of binaural hearing aids by first time hearing aid users. British Journal of Audiology. 1989;23:360. [Google Scholar]
- Vaughan-Jones RH, Padgham ND, Christmas HE, Irwin J, Doig MA. One aid or two? - more visits please! Journal of Laryngology and Otology. 1993;107(4):329–332. doi: 10.1017/s0022215100122947. [DOI] [PubMed] [Google Scholar]
- Vestergaard MD. Self-report outcome in new hearing-aid users: Longitudinal trends and relationships between subjective measures of benefit and satisfaction. Int J Audiol. 2006;45(7):382–392. doi: 10.1080/14992020600690977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LE, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wilson R, Zizz C, Sperry J. Masking-level difference for spondaic words in 2000-msec bursts of broadband noise. Journal of the American Academy of Audiology. 1994;5:236–242. [PubMed] [Google Scholar]
- Wilson RH, Shanks JE, Koebsell KA. Recognition masking-level differences for 10 CID W-1 spondaic words. J Speech Hear Res. 1982;25(4):624–628. doi: 10.1044/jshr.2504.624. [DOI] [PubMed] [Google Scholar]
Reference Notes
- 1.Kelly R, Cox R. Relationship between the NEO five-Factor Inventory (NEO-FFI) and the Positive and Negative Affect Schedule (PANAS) questionnaires. Hearing Aid Research Laboratory. University of Memphis; 2003. Unpublished Report. [Google Scholar]
- 2.Cox RM, Alexander GC, Xu J. Development of the Device Oriented Subjective Outcome Scale (DOSO). Annual Meeting of the American Auditory Society; 2009. Retrieved from http://www.memphis.edu/ausp/harl/publications.htm#posters. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shaughnessy K, Cox RM. Auditory Ecology and Preference for Unilateral or Bilateral Hearing Aids. Annual Meeting of the American Auditory Society; 2009. Retrieved from http://www.memphis.edu/ausp/harl/publications.htm#posters. [Google Scholar]


