Abstract
Biomechanical analysis of lower extremity activities while walking at different speeds and in challenging conditions may help to identify specific gait patterns associated with knee osteoarthritis (knee-OA). We hypothesized that individuals with asymptomatic knee-OA have lower ankle activity, while individuals with symptomatic knee-OA have similar or higher ankle activity compared to individuals without knee-OA, and that such differences are enhanced during challenging gait tasks. We tested this hypothesis by examining gait characteristics in multiple gait tasks using data from 153 Baltimore Longitudinal Study of Aging (BLSA) participants (112 without knee-OA, 41 with knee-OA; 53 – 87 years, 52 % women). All participants who could walk unassisted were evaluated in the BLSA gait lab while walking at self-selected speed (usual-walking), at maximum speed (fast-walking) and again at self-selected speed after 30-minutes of walking activities (usual-walking-after-30min). Knee range of motion was lower for knee-OA participants in the fast-walking and usual-walking-after-30min tasks (p < 0.030). Ankle range of motion for symptomatic knee-OA was greater compared to asymptomatic knee-OA for all walking tasks (p < 0.050). Symptomatic knee-OA had greater generative MWE of the ankle compared to asymptomatic knee-OA (p = 0.034), while keeping similar absorptive MWE of the knee when compared to no-OA controls (p = 0.151). Symptomatic knee-OA individuals seem to adapt an ankle kinematic gait pattern aimed at avoiding knee pain, by enhancing forward propulsion so to minimize knee joint load. Whether these conditions represent subsequent steps in the causal pathway from knee-OA to changes in gait is still not clear.
Keywords: Gait, Knee osteoarthritis, Challenging walking, Mechanical work expenditure
INTRODUCTION
Knee osteoarthritis (knee-OA) [1] is the most common age-related joint disease that causes mobility limitations [2]. Previous studies reported that knee-OA is associated with reduced muscle strength [3–5], slower gait speed [6], and impaired knee range of motion [7, 8]. However, the mechanism by which knee-OA is linked to reduced muscle strength and impaired mobility is still not completely clear. Despite overall lower muscle strength, individuals with knee-OA show greater hamstring muscle activation while executing activities of daily living [9] and greater knee adduction moment during customary walking [10]. A better understanding of these contradictory observations in knee-OA individuals is needed to clarify the mechanism of development and progression of knee-OA and to inform the design of new and effective preventive strategies. While the diagnosis of OA is based on characteristic structural knee joint changes, the differentiation between asymptomatic and symptomatic knee-OA depends on self-report of joint pains. Specific gait pattern differences between individuals with and without knee-OA have been described but it is unclear whether among individuals with knee-OA the presence of pain also has specific effects on gait.
Self-selected walking speed is a reliable and robust marker of overall gait performance. Previous studies have shown that during self-selected walking individuals with knee-OA have greater frontal-plane knee moment and increased activities on the lateral side than those without knee-OA. However, a full gait analysis that explore how knee-OA affects motor kinematics and kinetics at the hip, ankle as well as knee joints have not been performed [10, 11]. Considering the functional importance of ankle activity for generating forward momentum during walking and the fact that ankle performance significantly decline with older age [12], impairments in ankle activity in older adults can be one of the determinant factor for the knee-OA. Limited ankle movement could be implicated in the pathogenesis of knee-OA and, on the other hand, exaggerated ankle movement can be the compensatory effort by increasing forward momentum in patients with knee-OA. We hypothesized that changes in gait that are caused by knee-OA and the associated pain of knee-OA would be more evident during challenging motor tasks. In particular, in the present study we examined knee-OA associated gait characteristics during customary preferred speed walking, and also during various challenging gait tasks, which may mimic situations that are often encountered in daily life. In particular, we hypothesized that individuals with asymptomatic knee-OA would have lesser ankle activity than those without knee-OA, while individuals with symptomatic knee-OA would have similar or greater ankle activity compared to individuals without knee-OA during customary preferred speed gait and these patterns are more prominent for the challenging gait.
METHODS
Participants
The data reported here was collected from 153 adult (age 53 – 87 years) participants in the Baltimore Longitudinal Study of Aging (BLSA), a cohort study conducted by the investigators of the Intramural Research Program of the National Institute on Aging, National Institutes of Health. All participants received a detailed description of the study and consented to participate. The data presented here was collected in the BLSA Gait Laboratory between January and December of 2008 following a protocol approved by the Medstar Health Research Institutional Review Board. Knee pain and morning stiffness were ascertained by a highly trained nurse practitioners who used the following standard questions: “Have you ever had pain or aching on most days for at least one month in or around either knee?’ and “On most days, in the past 12 months, did you have morning stiffness in either of your knees?”. The nurse practitioners also performed a standardized physical exam to identify knee abnormalities such as crepitus, tenderness, and effusion. A posterior-anterior knee x-ray was performed in a standardized fixed flexion position (Siremobile Compact, Siemens, New York) to establish the presence of osteophytes. Combined information from the questionnaire, physical exam, and x-ray were used to adjudicate knee-OA diagnosis according to an algorithm modeled on the American College of Rheumatology (ACR) diagnostic classification criteria for knee-OA [13]. Briefly, participants with at least 3 of 6 following clinical findings (age > 50; stiffness; crepitus; tenderness; osteophytes; effusion) are classified as knee-OA, and based on experience of pain they were divided into asymptomatic and symptomatic knee-OA. The knee-OA group (N=41) was comprised of participants with knee pain that were either persistent or intermittent (“symptomatic” N =17), or without knee pain (“asymptomatic” N =24). The no-OA group (N =112) consisted of participants who did not fulfill the necessary criteria for a diagnosis of knee-OA. Participants with knee pain but who either did not have physical findings or imaging studies to confirm the presence of knee-OA were excluded from the analytic sample (N =28) to assure that each participants was properly categorized into a knee-OA or no-OA group. Participants were excluded if they had hip or knee prosthesis, severe joint pain, history of stroke or Parkinson’s disease, or could not follow instructions and safely complete all three walking tasks without the help of another person or a walking device. Participants with a Body Mass Index (BMI) > 40 were also excluded because of the technical difficulty in positioning pelvic markers during the gait analysis.
Gait measurement
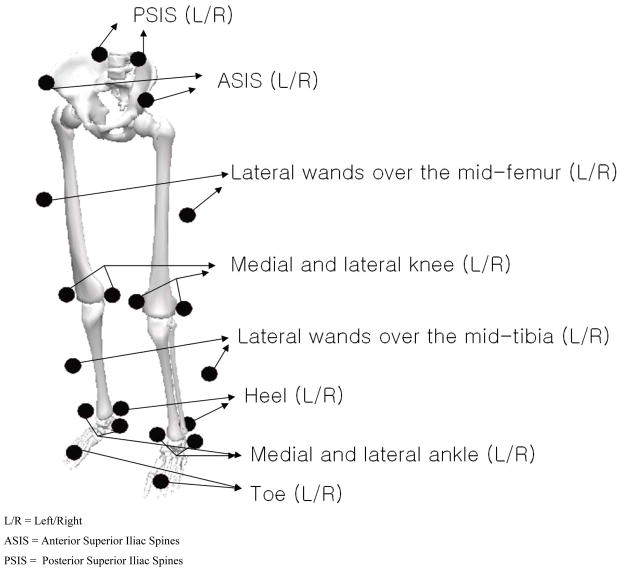
The procedure for the gait analysis performed in our laboratory has been previously reported [12, 14]. Briefly, participants were instrumented with 20 reflective markers on anatomical landmarks bilaterally (Figure 1): anterior and posterior superior iliac spines, medial and lateral knees, medial and lateral ankles, toe (second metatarsal head), heel, and lateral wands over the mid-femur and mid-tibia. Wands (8 cm length) were used for the femur and tibia markers to improve accuracy in the assessment of rotational angles. In an effort to avoid excessive errors in the calculation of the hip joint locations due to the adipose tissue of over-weight and obese participants, a tie band was used in the pelvic area and the distance between the left and right anterior superior iliac spines (ASIS) was measured manually. A Vicon 3D motion capture system with 10-digital cameras (Vicon 612 system, Oxford Metrics Ltd., Oxford, U.K.) measured the 3D locations of all markers on the landmarks of the lower extremity segments (60 Hz sampling frequency). During the gait test, ground reaction forces were measured with two staggered AMTI force platforms (Advanced Mechanical Technologies, Inc., Watertown, MA, USA; 1080 Hz sampling frequency).
Figure 1.
Marker set for gait analysis
After all markers were positioned on the skin and non-reflective firm fitting spandex shorts, participants were asked to walk across a 10 m long gait laboratory walkway at their self-selected and maximum speeds. The ‘usual-walking’ task was performed at the participant’s usual, self-selected walking speed, while the ‘fast-walking’ task required participants to walk as quickly as possible, without running. At the end of the testing session, which lasted approximately 30 minutes (including performing obstacle and narrow-base walking tasks, whose results are not included in the present study), a final task was performed at a self-selected walking speed; this task is referred to as ‘usual-walking-after-30min’. Participants were not informed about the presence or location of the force platforms on the walking path. Trials were performed until at least 3 complete gait cycles from the left and right sides, with the complete foot landing on the force platform, were obtained. The raw coordinate data of marker positions were digitally filtered with fourth-order zero-lag Butterworth filter with a cutoff at 6 Hz.
Data process and statistical analysis
The 3D kinematic measurements for the left and right lower extremities were calculated from all recorded positions of the markers over time based on the Euler angle theorem [15]. During walking, ranges of motions for the hip, knee, and ankle were measured using the angles between flexion and extension (dorsiflexion and planter flexion for the ankle) and the angles between abduction and adduction (inversion and eversion for the ankle) for the rotations in the sagittal and frontal planes, respectively. For the calculation of kinetics, only the gait cycles (defined as heel strike to subsequent heel strike of the ipsilateral foot) with a complete foot landing on the force platform were used in the analysis. Mechanical joint moments and mechanical joint powers from each lower extremity joint were calculated by Visual3D software (version 3.99; C-motion, Inc., Germantown, MD, USA) using kinematic measurements, ground reaction forces, biometric measurements (weight, height, the width between ASIS), and the paradigm of inverse dynamics starting and finishing with a heel strike. Mechanical work expenditures (MWEs) were calculated by numeric integration of mechanical joint powers for the durations of dominant gait periods for the hip, knee, and ankle in the stance phase. The differences in gait parameters within three different walking tasks across knee-OA categories were examined with generalized linear models (GLM). All the models were adjusted for gait speed (except gait speed itself), age, sex, height, and weight. Statistical significance was defined with p value less than 0.05. Statistical analysis was performed with SAS 9.1 Statistical Package (SAS Institute, Inc., Cary, NC, USA).
RESULTS
The descriptive characteristics of the 153 participants (80 women, 73 men) are summarized in Table 1. The groups were comparable for most variables except that participants with knee-OA were an average 3 years older than those without knee-OA.
Table 1.
Participant Characteristics
| Characteristics for participants | mean (SE) | p-values for the comparisons between | |||||
|---|---|---|---|---|---|---|---|
| no-OA (N =112) | knee-OA |
knee-OA vs. no-OA | asymptomatic vs. no-OA | symptomatic vs. no-OA | asymptomatic vs. symptomatic | ||
| asymptomatic (N =24) | symptomatic (N =17) | ||||||
| Age, years | 67.69 (0.80) | 72.33 (1.73) | 70.24 (2.06) | 0.016 | 0.042 | 0.482 | 0.715 |
| BMI, kg/m2 | 26.94 (0.41) | 27.20 (0.88) | 28.08 (1.05) | 0.425 | 0.959 | 0.569 | 0.800 |
| Height, m | 1.68 (0.01) | 1.68 (0.02) | 1.63 (0.02) | 0.338 | 0.965 | 0.128 | 0.179 |
| Weight, kg | 76.21 (1.44) | 77.28 (3.11) | 74.56 (3.69) | 0.983 | 0.948 | 0.909 | 0.839 |
| Sex, women | 57 | 10 | 13 | ||||
SE= Standard error
Bold indicates statistical difference (p < 0.05)
Gait parameters in spatiotemporal variables and kinematics and kinetics in the sagittal plane are summarized in Table 2 according to walking tasks, namely usual-walking, fast-walking, and usual-walking-after-30min. For the usual-walking and usual-walking-after30-min, gait speed was slower in knee-OA compared to no-OA controls. The stance period was shorter in knee-OA participants compared to no-OA controls for all walking tasks. Knee range of motion in the sagittal plane for the fast-walking and usual-walking-after-30min tasks was lower in knee-OA participants compared to no-OA controls. In the usual-walking and usual-walking-after-30min, ankle range of motion in the sagittal plane was significantly wider in the symptomatic knee-OA participants compared to both no-OA controls and participants with asymptomatic knee-OA. In the sagittal plane, knee-OA participants had lower generative MWE of the hip for usual-walking-after-30min, while they had greater absorptive MWE of the knee and lower generative MWE of the ankle for the usual-walking and fast-walking tasks compared to no-OA controls. For the fast-walking and usual-walking-after-30min, generative MWE of the ankle in the sagittal plane during ankle plantar-flexion was significantly lower in participants with asymptomatic knee-OA participants compared to no-OA controls and also compared to symptomatic knee-OA counterparts.
Table 2.
Gait parameters in spatiotemporal and in the kinematics and kinetics in the sagittal plane for three walking tasks in different knee-OA groups
| walking types, and gait parameters | adjusted mean † | p-values for the comparisons between | |||||
|---|---|---|---|---|---|---|---|
| no-OA(N =112) | knee-OA |
knee-OA vs. no-OA | asymptomatic vs. no-OA | symptomatic vs. no-OA | asymptomatic vs. symptomatic | ||
| asymptomatic (N =24) | symptomatic (N =17) | ||||||
| usual-walking | |||||||
| Gait speed, m/s | 1.17 | 1.09 | 1.09 | 0.008 | 0.076 | 0.153 | 0.999 |
| Stance, percentage gait cycle (PGC) | 64.14 | 63.15 | 63.65 | 0.011 | 0.023 | 0.490 | 0.591 |
| Range of motion in sagittal plane, degree | |||||||
| Hip | 40.24 | 40.81 | 41.47 | 0.251 | 0.799 | 0.457 | 0.852 |
| Knee | 55.46 | 53.82 | 54.02 | 0.050 | 0.207 | 0.403 | 0.987 |
| Ankle | 24.00 | 23.20 | 27.29 | 0.229 | 0.613 | 0.003 | 0.002 |
| MWE in sagittal plane, 1000*J/kg | |||||||
| Hip generative MWE during HF | 92.78 | 89.53 | 80.37 | 0.111 | 0.815 | 0.111 | 0.427 |
| Knee absorptive MWE during KF | 149.49 | 188.51 | 175.49 | 0.030 | 0.097 | 0.454 | 0.870 |
| Ankle Generative MWE during AF | 183.77 | 148.58 | 178.27 | 0.032 | 0.019 | 0.927 | 0.218 |
| fast-walking | |||||||
| Gait speed, m/s | 1.71 | 1.61 | 1.63 | 0.053 | 0.186 | 0.482 | 0.952 |
| Stance, percentage gait cycle (PGC) | 62.62 | 61.87 | 62.37 | 0.011 | 0.011 | 0.668 | 0.351 |
| Range of motion in sagittal plane, degree | |||||||
| Hip | 46.05 | 45.72 | 47.69 | 0.602 | 0.954 | 0.424 | 0.425 |
| Knee | 58.54 | 56.32 | 57.12 | 0.029 | 0.090 | 0.468 | 0.850 |
| Ankle | 24.99 | 23.66 | 26.96 | 0.963 | 0.362 | 0.188 | 0.042 |
| MWE in sagittal plane, 1000*J/kg | |||||||
| Hip generative MWE during HF | 179.05 | 160.57 | 168.17 | 0.059 | 0.152 | 0.606 | 0.845 |
| Knee absorptive MWE during KF | 206.77 | 271.36 | 213.69 | 0.028 | 0.012 | 0.961 | 0.151 |
| Ankle Generative MWE during AF | 258.91 | 196.55 | 260.73 | 0.021 | 0.003 | 0.996 | 0.034 |
| usual-walking-after30min | |||||||
| Gait speed, m/s | 1.29 | 1.22 | 1.22 | 0.029 | 0.176 | 0.269 | 0.999 |
| Stance, percentage gait cycle (PGC) | 63.45 | 62.69 | 63.36 | 0.040 | 0.021 | 0.961 | 0.202 |
| Range of motion in sagittal plane, degree | |||||||
| Hip | 42.44 | 42.72 | 43.33 | 0.464 | 0.945 | 0.663 | 0.876 |
| Knee | 56.40 | 54.46 | 54.67 | 0.021 | 0.118 | 0.278 | 0.987 |
| Ankle | 24.86 | 24.14 | 27.85 | 0.276 | 0.694 | 0.011 | 0.008 |
| MWE in sagittal plane, 1000*J/kg | |||||||
| Hip generative MWE during HF | 106.37 | 93.46 | 91.80 | 0.005 | 0.075 | 0.085 | 0.978 |
| Knee absorptive MWE during KF | 168.82 | 199.45 | 174.90 | 0.278 | 0.379 | 0.972 | 0.722 |
| Ankle Generative MWE during AF | 197.49 | 157.57 | 211.41 | 0.144 | 0.017 | 0.681 | 0.022 |
Speed adjusted by age, sex, height and weight; Others adjusted by speed, age, sex, height and weight
PGC = percentage gait cycle; MWE = mechanical work expenditure
HF = hip flexion period in stance phase; KF = knee flexion in late stance phase; AF = ankle plantar flexion period
Bold indicates statistical difference (p < 0.05)
No knee-OA associated differences in range of motion for the lower extremity in the frontal plane were observed (not reported in table). Kinetic gait parameters in the frontal plane in forms of peak joint moment and MWE are summarized in Table 3. In the frontal plane, peak moment from the knee joint of knee-OA participants was greater for the usual-walking and usual-walking-after-30min, but not for the fast-walking compared to no-OA controls. Total generative MWE of the hip in the frontal plane of knee-OA participants was greater for all walking tasks while total generative MWE of the knee in the frontal plane was greater only for the usual-walking-after-30min task compared to no-OA controls.
Table 3.
Kinetic gait parameters in the frontal plane for three walking tasks in different knee-OA groups
| walking types, and gait parameters | adjusted mean † | p-values for the comparisons between | |||||
|---|---|---|---|---|---|---|---|
| no-OA(N =112) | knee-OA |
knee-OA vs. no-OA | asymptomatic vs. no-OA | symptomatic vs. no-OA | asymptomatic vs. symptomatic | ||
| asymptomatic (N =24) | symptomatic (N =17) | ||||||
| usual-walking | |||||||
| Peak moment in frontal plane, Nm/kg | |||||||
| Hip | 0.87 | 0.91 | 0.88 | 0.172 | 0.217 | 0.951 | 0.601 |
| Knee | 0.43 | 0.48 | 0.51 | 0.003 | 0.109 | 0.018 | 0.684 |
| Ankle | 0.17 | 0.16 | 0.18 | 0.901 | 0.882 | 0.926 | 0.788 |
| Total MWE in frontal plane, 1000*J/kg | |||||||
| Generative hip | 74.52 | 87.95 | 90.14 | 0.014 | 0.140 | 0.136 | 0.972 |
| Generative Knee | 10.62 | 11.32 | 14.40 | 0.165 | 0.912 | 0.141 | 0.400 |
| Generative Ankle | 9.59 | 12.59 | 7.96 | 0.523 | 0.317 | 0.776 | 0.240 |
| Absorptive hip | 47.52 | 47.41 | 47.40 | 0.978 | 0.999 | 0.999 | 0.999 |
| Absorptive knee | 20.16 | 24.18 | 23.47 | 0.127 | 0.367 | 0.598 | 0.984 |
| Absorptive ankle | 17.38 | 19.81 | 16.91 | 0.582 | 0.646 | 0.988 | 0.721 |
| fast-walking | |||||||
| Peak moment in frontal plane, Nm/kg | |||||||
| Hip | 0.94 | 0.96 | 0.93 | 0.625 | 0.702 | 0.989 | 0.766 |
| Knee | 0.50 | 0.52 | 0.55 | 0.199 | 0.726 | 0.419 | 0.873 |
| Ankle | 0.19 | 0.16 | 0.20 | 0.297 | 0.134 | 0.842 | 0.156 |
| Total MWE in frontal plane, 1000*J/kg | |||||||
| Generative hip | 76.67 | 88.59 | 95.86 | 0.012 | 0.226 | 0.057 | 0.748 |
| Generative Knee | 15.89 | 14.72 | 19.49 | 0.702 | 0.893 | 0.450 | 0.382 |
| Generative Ankle | 12.92 | 10.48 | 12.55 | 0.556 | 0.739 | 0.995 | 0.893 |
| Absorptive hip | 74.05 | 78.96 | 80.45 | 0.388 | 0.806 | 0.759 | 0.990 |
| Absorptive knee | 23.51 | 26.72 | 25.79 | 0.268 | 0.561 | 0.801 | 0.975 |
| Absorptive ankle | 22.51 | 17.78 | 24.64 | 0.434 | 0.239 | 0.800 | 0.210 |
| usual-walking-after-30min | |||||||
| Peak moment in frontal plane, Nm/kg | |||||||
| Hip | 0.88 | 0.93 | 0.90 | 0.070 | 0.131 | 0.739 | 0.715 |
| Knee | 0.44 | 0.51 | 0.52 | 0.006 | 0.087 | 0.081 | 0.962 |
| Ankle | 0.18 | 0.17 | 0.20 | 0.624 | 0.783 | 0.219 | 0.150 |
| Total MWE in frontal plane, 1000*J/kg | |||||||
| Generative hip | 78.72 | 97.69 | 94.53 | 0.004 | 0.033 | 0.164 | 0.950 |
| Generative Knee | 11.82 | 14.96 | 17.43 | 0.008 | 0.220 | 0.029 | 0.610 |
| Generative Ankle | 10.61 | 11.56 | 10.56 | 0.742 | 0.883 | 0.999 | 0.932 |
| Absorptive hip | 52.21 | 52.56 | 56.34 | 0.647 | 0.997 | 0.764 | 0.855 |
| Absorptive knee | 21.36 | 24.96 | 23.93 | 0.246 | 0.528 | 0.783 | 0.973 |
| Absorptive ankle | 19.92 | 17.17 | 25.34 | 0.753 | 0.469 | 0.115 | 0.035 |
Speed adjusted by age, sex, height and weight; Others adjusted by speed, age, sex, height and weight
MWE = mechanical work expenditure
DISCUSSION
The present study explored gait patterns associated with symptomatic and asymptomatic knee-OA among older adults. We looked at multiple walking conditions to characterize kinematics and kinetics parameters at the hip, knee, and ankle. Partially supporting our “a priori” hypothesis, we found that asymptomatic knee-OA participants had lesser ankle activity compared to no-OA controls while symptomatic knee-OA participants had similar ankle activity with no-OA controls during customary walking.
Consistent with previous studies [11, 16], participants with knee-OA walked slower than no-OA controls in walking tasks of usual-walking and usual-walking-after-30min. Compared to no-OA controls, knee-OA participants walked with shorter stance for all three walking tasks. When looking at the subgroups of knee-OA, asymptomatic knee-OA appears to negatively affect stance time more than symptomatic knee-OA. These findings suggest that structural changes in the knee joint rather than joint-related symptoms (pain or rigidity) affect stance period or, alternatively, that changes in stance are compensated in the presence of symptoms. This hypothesis cannot be fully tested in our cross-sectional analysis and should be evaluated in longitudinal studies that track the transition between asymptomatic to symptomatic knee-OA.
Lower knee rotation in knee-OA individuals, previously reported for the self-selected speed walking [7, 8], was observed in the present study for the fast-walking and usual-walking-after-30min tasks, but not for the usual-walking task. This finding is somewhat unexpected and may be related to the substantial good health and paucity of overt symptoms in study participants. Interestingly, symptomatic knee-OA participants showed greater ankle range of motion in the sagittal plane compared to no-OA controls for usual-walking and usual-walking-after-30min. Given that asymptomatic knee-OA did not have influence on ankle rotation, this greater ankle range of motion in the symptomatic knee-OA participants may indicate a compensatory effort aimed at limiting the activity of the knee joint therefore avoiding knee-OA symptoms.
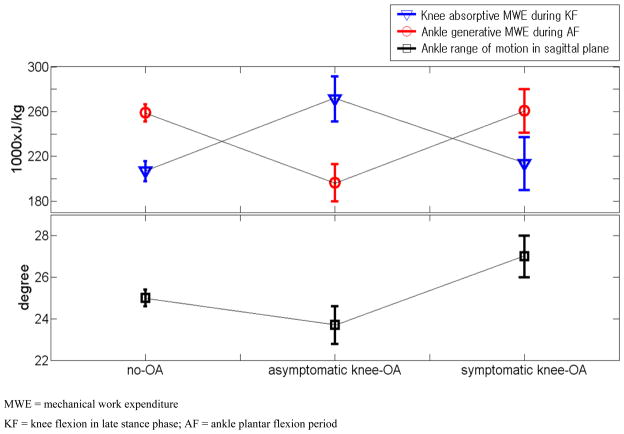
Different gait patterns in MWE differentiated knee-OA participants from no-OA controls in the different walking tasks. Interestingly, knee-OA participants showed lower generative MWE of the hip in the sagittal plane during the late stance compared to no-OA controls only for the usual-walking-after-30min task regardless of the presence of OA symptoms. This is consistent with previous findings and has been interpreted as reflecting weakness in the quadriceps [5, 17] and reduced biomechanical reserve in knee-OA patients. Greater absorptive MWE of the knee and lower generative MWE of the ankle in the overall knee-OA participants were evident in the asymptomatic knee-OA participants but not in the symptomatic knee-OA participants. Of note, these characteristics can challenge structural knee joint integrity and impair forward propulsion. All combined, our findings provide empirical support to the hypothesis suggested by previous studies that kinetic changes in gait patterns occurs in an early state of knee-OA development while kinematic changes emerge late in the process, when knee-OA is fully clinically detectable [8, 18]. This is particularly evident in fast speed walking where the symptomatic knee-OA individuals adopt an ankle kinematic gait pattern that by enhancing forward propulsion and minimizing knee joint load minimizes knee pain (Figure 2). Thus, while our findings offer some clue on the specific changes in gait characteristics that occur during knee-OA development they also point out the need for introducing challenging gait tasks, such as fast-walking and usual-walking-after-30min, in the study of gait to reveal characteristic that are not evident during unchallenged walking.
Figure 2.
Modified kinematic gait pattern of symptomatic knee-OA (ankle range of motion) which may be associated with kinetic gait patterns from the knee and ankle (knee absorptive MWE and ankle generative MWE, respectively), which are close to no-OA and different from asymptomatic knee-OA during fast-walking task.
Consistent with previous studies, greater peak joint moment of the knee in the frontal plane was observed for knee-OA in both usual speed walking tasks, but not for the fast-walking task [10, 19]. In the context of knee-OA, increased walking speed by enhancing forward momentum may mitigate medial-lateral loading. Of note, during stance period, total generative MWE of the hip in the frontal plane was also significantly greater in knee-OA participants for all walking tasks. There is evidence in the literature that frontal plane hip activity during walking declines with older age [12]. Thus, greater generative MWE of the hip in the frontal plane could be considered a “signature” of knee-OA that is not confounded by aging. Interestingly, the effect of knee-OA on generative MWE of the knee in the frontal plane was different when participants walked at the beginning and after the 30-minute testing session. This is consistent with the notion that medial-lateral knee activity is sensitive to physical conditions, such as being fatigued [20, 21].
This study has limitations. First, due to the cross-sectional nature of this study, we were unable to identify causality in the association between gait patterns and the prevalence of knee-OA and we cannot discriminate whether the observed associations are causes or effects of knee-OA. The BLSA is currently collecting longitudinal gait data which may allow observing transitions from no-OA to asymptomatic knee-OA and to symptomatic knee-OA states. This data may shed some more light on the relationship between knee-OA and changes in gait. Second, it is difficult to explain whether the differences seen in our study between the symptomatic and asymptomatic knee-OA groups are simply due to the lack of pain relief in the symptomatic knee-OA group or actually due to a change in gait patterns to compensate for their knee-OA symptom. It would be beneficial to look at gait patterns in the symptomatic knee-OA individuals once pain relief was achieved. Unfortunately, this approach would not be feasible in the context of a large epidemiological study of aging that includes multiple physical tests in addition to the gait laboratory analysis. Last, due to the fact that participants in this study were limited to those who could complete all three walking tasks unaided without severe joint pain, the small differences reported in the present study probably underestimate the effect of knee pain on gait characteristics.
In conclusion, ankle joint movement strategy was raised as a possible compensatory action for regaining gait patterns of normal individuals. If the modified kinematic gait pattern such as greater ankle range of motion in symptomatic knee-OA participants can be linked as the cause of kinetic gait patterns similar to normal individuals, this kinematic gait pattern adaptation can be applied to asymptomatic knee-OA individuals before knee-OA progresses to more severe knee-OA state. The present study emphasizes the importance of early detection of asymptomatic knee-OA because asymptomatic individuals may be most beneficial from the intervention of ankle strategy observed from gait patterns of symptomatic knee-OA individuals. Findings in the present study also emphasize the utility of challenging walking trials in demonstrating knee-OA associated gait patterns that were not demonstrable during usual walking.
Acknowledgments
This research was supported entirely by the Intramural Research Program of the NIH, National Institute on Aging. Data for these analyses were obtained from the Baltimore Longitudinal Study of Aging, a study performed by the National Institute on Aging.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the united states: Arthritis data from the third national health and nutrition examination survey 1991–94. J Rheumatol. 2006;33:2271–2279. [PubMed] [Google Scholar]
- 2.van Baar ME, Dekker J, Lemmens JA, Oostendorp RA, Bijlsma JW. Pain and disability in patients with osteoarthritis of hip or knee: The relationship with articular, kinesiological, and psychological characteristics. J Rheumatol. 1998;25:125–133. [PubMed] [Google Scholar]
- 3.Benedetti MG, Bonato P, Catani F, D’Alessio T, Knaflitz M, Marcacci M, Simoncini L. Myoelectric activation pattern during gait in total knee replacement: Relationship with kinematics, kinetics, and clinical outcome. IEEE Trans Rehabil Eng. 1999;7:140–149. doi: 10.1109/86.769404. [DOI] [PubMed] [Google Scholar]
- 4.Fisher NM, Pendergast DR. Reduced muscle function in patients with osteoarthritis. Scand J Rehabil Med. 1997;29:213–221. [PubMed] [Google Scholar]
- 5.Lewek MD, Rudolph KS, Snyder-Mackler L. Quadriceps femoris muscle weakness and activation failure in patients with symptomatic knee osteoarthritis. J Orthop Res. 2004;22:110–115. doi: 10.1016/S0736-0266(03)00154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mundermann A, Dyrby CO, Hurwitz DE, Sharma L, Andriacchi TP. Potential strategies to reduce medial compartment loading in patients with knee osteoarthritis of varying severity: Reduced walking speed. Arthritis Rheum. 2004;50:1172–1178. doi: 10.1002/art.20132. [DOI] [PubMed] [Google Scholar]
- 7.Al-Zahrani KS, Bakheit AM. A study of the gait characteristics of patients with chronic osteoarthritis of the knee. Disabil Rehabil. 2002;24:275–280. doi: 10.1080/09638280110087098. [DOI] [PubMed] [Google Scholar]
- 8.Deluzio KJ, Astephen JL. Biomechanical features of gait waveform data associated with knee osteoarthritis: An application of principal component analysis. Gait Posture. 2007;25:86–93. doi: 10.1016/j.gaitpost.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 9.Hortobagyi T, Westerkamp L, Beam S, Moody J, Garry J, Holbert D, DeVita P. Altered hamstring-quadriceps muscle balance in patients with knee osteoarthritis. Clin Biomech (Bristol, Avon) 2005;20:97–104. doi: 10.1016/j.clinbiomech.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 10.Hunt MA, Birmingham TB, Giffin JR, Jenkyn TR. Associations among knee adduction moment, frontal plane ground reaction force, and lever arm during walking in patients with knee osteoarthritis. J Biomech. 2006;39:2213–2220. doi: 10.1016/j.jbiomech.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 11.Hubley-Kozey CL, Deluzio KJ, Landry SC, McNutt JS, Stanish WD. Neuromuscular alterations during walking in persons with moderate knee osteoarthritis. J Electromyogr Kinesiol. 2006;16:365–378. doi: 10.1016/j.jelekin.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 12.Ko S, Ling SM, Winters J, Ferrucci L. Age-related mechanical work expenditure during normal walking: The baltimore longitudinal study of aging. J Biomech. 2009;42:1834–1839. doi: 10.1016/j.jbiomech.2009.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, Christy W, Cooke TD, Greenwald R, Hochberg M, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and therapeutic criteria committee of the american rheumatism association. Arthritis Rheum. 1986;29:1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 14.Teixeira-Salmela LF, Nadeau S, Milot MH, Gravel D, Requiao LF. Effects of cadence on energy generation and absorption at lower extremity joints during gait. Clin Biomech (Bristol, Avon) 2008;23:769–778. doi: 10.1016/j.clinbiomech.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 15.Ginsberg JH. Advanced engineering dynamics. 2. Cambridge, UK: Cambridge University Press; 1995. [Google Scholar]
- 16.Tseng SC, Liu W, Finley M, McQuade K. Muscle activation profiles about the knee during tai-chi stepping movement compared to the normal gait step. J Electromyogr Kinesiol. 2007;17:372–380. doi: 10.1016/j.jelekin.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 17.Hurley MV. Muscle dysfunction and effective rehabilitation of knee osteoarthritis: What we know and what we need to find out. Arthritis Rheum. 2003;49:444–452. doi: 10.1002/art.11053. [DOI] [PubMed] [Google Scholar]
- 18.Arokoski JP, Jurvelin JS, Vaatainen U, Helminen HJ. Normal and pathological adaptations of articular cartilage to joint loading. Scand J Med Sci Sports. 2000;10:186–198. doi: 10.1034/j.1600-0838.2000.010004186.x. [DOI] [PubMed] [Google Scholar]
- 19.Mundermann A, Dyrby CO, Andriacchi TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: Increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005;52:2835–2844. doi: 10.1002/art.21262. [DOI] [PubMed] [Google Scholar]
- 20.Gehring D, Melnyk M, Gollhofer A. Gender and fatigue have influence on knee joint control strategies during landing. Clin Biomech (Bristol, Avon) 2009;24:82–87. doi: 10.1016/j.clinbiomech.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 21.Rozzi SL, Lephart SM, Fu FH. Effects of muscular fatigue on knee joint laxity and neuromuscular characteristics of male and female athletes. J Athl Train. 1999;34:106–114. [PMC free article] [PubMed] [Google Scholar]