Abstract
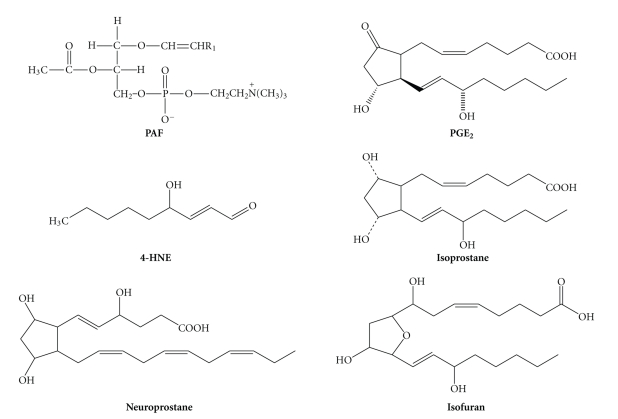
Parkinson's disease (PD) is a neurodegenerative movement disorder of unknown etiology. PD is characterized by the progressive loss of dopaminergic neurons in the substantia nigra, depletion of dopamine in the striatum, abnormal mitochondrial and proteasomal functions, and accumulation of α-synuclein that may be closely associated with pathological and clinical abnormalities. Increasing evidence indicates that both oxidative stress and inflammation may play a fundamental role in the pathogenesis of PD. Oxidative stress is characterized by increase in reactive oxygen species (ROS) and depletion of glutathione. Lipid mediators for oxidative stress include 4-hydroxynonenal, isoprostanes, isofurans, isoketals, neuroprostanes, and neurofurans. Neuroinflammation is characterized by activated microglial cells that generate proinflammatory cytokines, such as TNF-α and IL-1β. Proinflammatory lipid mediators include prostaglandins and platelet activating factor, together with cytokines may play a prominent role in mediating the progressive neurodegeneration in PD.
1. Introduction
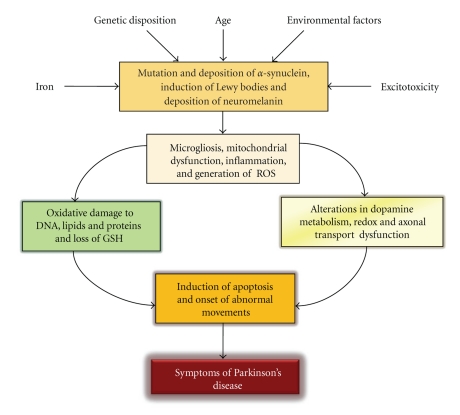
Parkinson's disease (PD) is a neurodegenerative disorder of unknown etiology. PD is characterized by the progressive loss of dopaminergic neurons in the substantia nigra pars compacta, which project to the striatum, the output of which governs locomotor behavior [1, 2]. While 90–95% of PD cases have no known genetic basis, approximately 5–10% arise from inherited mutations [3]. Roughly half of early-onset PD is caused by loss-of-function mutations in the parkin gene [4], which encodes an E3 ubiquitin ligase. Although the molecular mechanism of vulnerability of dopaminergic neurons in the substantia nigra pars compacta is not known, it is suggested that monoamine oxidase-mediated abnormal dopamine metabolism, hydrogen peroxide generation, abnormal mitochondrial and proteasomal dysfunctions along with microglial cell activation may be closely associated with neurodegenerative process [5]. Monoamine oxidase catalyzes the oxidative deamination of dietary amines and monoamine neurotransmitters, such as serotonin, norepinephrine, dopamine, β-phenylethylamine, and other trace amines. The rapid degradation of these molecules ensures the proper functioning of synaptic neurotransmission and is critically important not only for the regulation of emotional behaviors, but also for other neural functions. PD is accompanied by abnormalities in synaptic neurotransmission in the basal ganglia. The loss of dopaminergic neurons in the substantia nigra pars compacta may be related to resting tremor, rigidity, bradykinesia, postural instability, and gait disturbance in PD patients. The neuropathological hallmarks of PD include the presence of Lewy bodies mostly composed of α-synuclein, a presynaptic protein that not only plays an important role in neuropathology of PD, but is also known to bind Cu2+, a divalent metal ion, which accelerates the aggregation of α-synuclein to form various toxic aggregates in vitro [5, 6]. Neurochemically, PD is characterized by the mitochondrial dysfunction, reactive oxygen species (ROS) generation, nitric oxide (NO) production, excitotoxicity, inflammation, accumulation of aberrant or misfolded proteins, and ubiquitin-proteasome system dysfunction (Figure 1) [1, 2].
Figure 1.
Potential factors and events associated with the pathogenesis of PD.
2. Oxidative Stress and Its Consequences in Brain
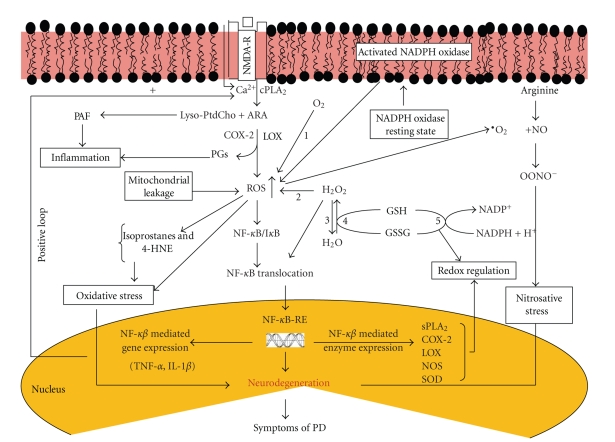
Oxidative stress is a cytotoxic condition that occurs in the tissue when antioxidant mechanisms are overwhelmed by ROS [7]. Thus, oxidative stress is a threshold phenomenon characterized by a major increase in the amount of oxidized cellular components. ROS include superoxide anions, hydroxyl, alkoxyl, and peroxyl radicals, and hydrogen peroxide. The major sources of ROS are the mitochondrial respiratory chain, an uncontrolled arachidonic acid (ARA) cascade, and NADPH oxidase (Figure 2) [8]. These processes utilize molecular oxygen and produce ROS, which include superoxide anion (O2‒) and H2O2. Superoxide is rapidly converted to H2O2 by superoxide dismutase (SOD), and in turn H2O2 is converted to H2O by catalase [9]. In the presence of metal ions, such as Fe2+ and Cu2+, H2O2 can be further converted to hydroxyl radical (•OH) through the Fenton reaction. Hydroxyl radicals can attack polyunsaturated fatty acids in membrane phospholipids forming the peroxyl radical (ROO•) and then propagate the chain reaction of lipid peroxidation [5].
Figure 2.
Generation of ROS, activation of NF-κB, redox status, and gene expression in Parkinson's disease. (1) NADPH oxidase; (2) superoxide dismutase; (3) catalase; (4) glutathione peroxidase; (5) glutathione reductase; cytosolic phospholipase A2 (cPLA2); secretory phospholipase A2 (sPLA2); cyclooxygenase-2 (COX), lipoxygenase (LOX); SOD; nitric oxide synthase (NOS); cytokines, TNF-α and IL-1β; reduced glutathione (GSH); oxidized glutathione (GSSG) and hydrogen peroxide (H2O2). Increase in oxidative stress-mediated expression of NF-κB induces transcription of sPLA2. COX-2, NOS, and SOD in the nucleus as well as proinflammatory cytokines (TNF-α and IL-1β) that further upregulate activities of cPLA2, sPLA2, NOS through a positive loop mechanism in cytoplasm and neural membranes.
Low levels of ROS are needed for normal cellular functions including, but not restricted to, the regulation of neuronal excitability via redox-sensitive ion channels, synaptic plasticity, gene transcription, and for the activity of enzymes controlling protein phosphorylation [10]. At higher concentrations, ROS cause neural membrane damage. The biological targets of ROS include membrane proteins, unsaturated lipids, and DNA [11]. Although neurodegeneration in neurological disorders is a multifactorial process [5, 12], it is becoming increasingly evident that the major underlying factor in the neurological disorders is the increased oxidative stress substantiated by the findings that the protein side-chains are modified either directly or indirectly by ROS. The reaction between ROS and proteins or unsaturated lipids in the plasma membrane also results in the chemical cross-linking of membrane proteins and lipids and a reduction in membrane unsaturation. The depletion of unsaturation in membrane lipids is associated with decreased membrane fluidity and decreased activity of membrane-bound enzymes, ion-channels, and receptors [13].
ROS also attack DNA bases causing damage through hydroxylation, ring opening, and fragmentation [14]. This attack generates 8-hydroxy-2′-deoxyguanosine (8-OHdG) and 2, 6-diamino-4-hydroxy-5-formamidopyrimidine (FapyGua) [15]. ROS may also attack the sugar phosphate backbone of DNA [7]. An indication of this DNA damage comes from the presence of free bases in urine. Abstraction of hydrogen by ROS at the C-4 position of the sugar moiety also produces single-strand breaks in DNA. This is accompanied by a second sugar oxidation on the complementary strand, causing a double strand break in DNA. These reactions may be responsible for the mutagenic effects of ROS in brain tissue [14].
Activation of nitric oxide synthase (NOS) generates nitric oxide (NO), which reacts with superoxide to form peroxynitrite. This molecule oxidatively modifies nucleic acid, lipid, sugar, and protein, leading to nuclear damage, mitochondrial damage, proteasome inhibition, and endoplasmic reticulum (ER) stress [16]. NO and peroxynitrite not only decrease glutathione but also S-nitrosylate many proteins. Excessive nitrosative stress contributes to the hyperactivation of the N-methyl-D-aspartate (NMDA)-type glutamate receptor, mitochondrial dysfunction, and cellular aging. Excessive generation of free radicals and related molecules (ROS) and NO species have been reported to trigger pathological production of misfolded proteins, abnormal mitochondrial dynamics (comprised of mitochondrial fission and fusion events), and apoptotic pathways in neuronal cells [17, 18]. Emerging evidence suggests that excessive NO production can contribute to these pathological processes, specifically by S-nitrosylation of specific target proteins, such as protein disulfide isomerase (PDI), ubiquitin protein ligase, parkin (forming SNO-parkin), and mitochondrial fragmentation through β-amyloid-related S-nitrosylation of dynamin-related protein-1 [18]. Among these proteins, PDI is responsible for normal protein folding in the endoplasmic reticulum (ER). S-nitrosylation of PDI compromises its function and induces misfolding not only in cell cultures systems, but also in animal models of neurodegenerative diseases [17, 18]. In addition, NO-mediated effects on dopaminergic neurons may also include the inhibition of cytochrome oxidase, ribonucleotide reductase, mitochondrial complexes I, II, and IV in the respiratory chain, superoxide dismutase, glyceraldehyde-3-phosphate dehydrogenase, activation or initiation of DNA strand breakage, poly (ADP-ribose) synthase, lipid peroxidation, protein oxidation, release of iron, and increased generation of toxic radicals such as hydroxyl radicals and peroxynitrite [19]. Accumulating evidence suggests that excessive ROS/RNS formation by above-mentioned processes may induce UPS-impairment and/or misfolding of molecular chaperons, thus resulting in protein aggregation and neuronal damage [18]. This suggestion supports the possible occurrence of cross-talk between mitochondria and UPS controlling organelles (proteasomes). Thus, the production of excessive ROS by mitochondria may adversely affect UPS activity leading to neurodegeneration in neurological disorders [12, 20].
Among neural cells, neurons are particularly vulnerable to oxidative damage not only because of mitochondrial dysfunction [21], but also due to inactivation of glutamine synthetase, which reduces the uptake of glutamate by glial cells and increases glutamate availability at the synapse producing excitotoxicity [9]. In addition, neuronal membrane peroxidative injury may lead to the depletion of unsaturated fatty acids in neural membranes, which not only causes changes in membrane fluidity but also affects activities of membrane-bound enzymes, ion channels, and receptors [10].
Glial cell's response to oxidative stress-mediated neurodegenerative process is extremely complex. On one side, astrocytes protect neurons from excitotoxicity through glutamate uptake system, and on the other side astrocytes contribute to the extracellular glutamate via reversed glutamate transporter [22]. In addition, astrocytes may undergo astrocytosis after dopaminergic cell loss and contribute to the inflammatory response [7]. Microglial cells respond to oxidative stress-mediated neurodegenerative process by transforming themselves into activated microglia. They not only change their shape into “ameboid" morphology, but also release matrix metalloproteinases, ROS, RNS, prostaglandin E2, and proinflammatory cytokines such as TNF-α and IL-β1 [10].
3. Oxidative Stress, Nitrosative Stress and Their Consequences in PD
Involvement of oxidative stress in the pathogenesis of PD is supported by both postmortem studies and by studies showing the increased level of oxidative stress in the substantia nigra pars compacta. A plausible source of oxidative stress in nigral dopaminergic neurons is the redox reactions that specifically involve dopamine and producing various toxic quinone species (DAQ), such as dopamine-o-quinone (DQ), aminochrome (AC), and indole-quinone (IQ). Oxidation products of dopamine have been shown to alter mitochondrial function, including mitochondrial swelling and decrease in electron transport chain activity [23, 24]. Studies on toxic effects of dopamine-derived DAQ on mitochondria, specifically on NADH and GSH pools, indicate that the generation of DAQ in isolated respiring mitochondria induces the opening of the permeability transition pore most probably by inducing oxidation of NADH, while GSH levels are not affected. It is proposed that studies on diverse reactivity for the different DAQ may provide information on the complex molecular mechanisms underlying oxidative stress and mitochondria dysfunction in PD. Markers of lipid peroxidation include 4-hydroxy-trans-2-nonenal (4-HNE), 4-oxo-trans-2-nonenal (4-ONE), acrolein, isoprostanes, and isofurans are significantly increased in PD (Table 1 and Figure 3). These markers are derived from arachidonic acid (ARA), which is released from neural membrane glycerophospholipids through the activation of cytosolic phospholipases A2 (cPLA2). This enzyme is coupled with NMDA receptors through G protein independent mechanism [10]. This suggestion is supported by studies on cPLA2 deficient mice. These mice are resistant to a specific dopaminergic neurotoxicity induced by the toxin 1-methyl,4-phenyl-1,2,3,6 tetrahydropyridine (MPTP) [25]. In the brain, MPTP is converted to its toxic metabolite, 1-methyl-4-phenylpyridinium ion (MPP+), in the presence of monoamine oxidase B. MPP+ is actively taken up into nigrostriatal neurons where it inhibits mitochondrial oxidative phosphorylation leading to neuronal cell death [26]. In MPTP-induced model of Parkinsonism, PLA2 inhibitors (quinacrine and arachidonyltrifluoromethyl ketone) protect dopaminergic neurons from neurodegeneration [27, 28]. In addition, the inhibition of COX-2, the enzyme responsible for the production of proinflammatory prostaglandin (PGE2), not only decreases the lesions caused by MPTP but also protects dopaminergic neurons in the substantia nigra. However, the molecular mechanism associated with COX-2-mediated neurodegeneration in animal model of PD remains unknown. However, COX-2 inhibition may prevent the formation of the oxidant species of reactive quinones. These metabolites are involved in the pathogenesis of PD [29–31].
Table 1.
Levels of mediators, proteins, and factors, which facilitate and maintain oxidative stress and inflammatory responses in PD.
(a)
| (A) Lipid mediator | Effect | Reference |
|---|---|---|
| Prostaglandins | Increased | [10] |
| Lipid peroxidation | Increased | [10] |
| 4-Hydroxynonenal | Increased | [10] |
| Hydroxycholesterol | Increased | [32] |
| 8-OHdGua | Increased | [32] |
| PINK | Increased | [33] |
| Aggregated α-synuclein | Increased | [34] |
| NF-κB activity | Increased | [35] |
| Oxidative stress | Increased | [12] |
| Neuroinflammation | Increased | [12] |
| Neurodegeneration | Increased | [12] |
(b)
Figure 3.
Chemical structures of biomarkers for oxidative stress.
Nitric oxide (NO) plays multiple roles in the brain and spinal cord tissues. In addition to regulating proliferation, survival and differentiation of neurons, it is involved in synaptic activity, neural plasticity, and memory function [39]. The evidence for the involvement of NO in neurotoxic processes associated with PD comes from studies using experimental models of this disease. NOS inhibitors can prevent MPTP-mediated dopaminergic neurotoxicity. Furthermore, NO not only fosters dopamine depletion, but NO-mediated neurotoxicity is averted by 7-nitroindazole, a nNOS inhibitor, in the substantia nigra pars compacta [19]. Moreover, mutant mice lacking the nNOS gene are more resistant to MPTP neurotoxicity when compared with wild-type littermates. Selegiline, an irreversible inhibitor of monoamine oxidase B, produces beneficial effects in PD by enhancing dopaminergic function. Selegiline and its metabolite (desmethylselegiline) also act by reducing apoptotic cell death by modulating the expression of number of genes, including superoxide dismutase, Bcl-2, Bcl-xl, NOS, c-Jun, and nicotinamide adenine nucleotide dehydrogenase. It is likely that selegiline-mediated antiapoptotic activity may also be involved in the prevention of a progressive reduction of mitochondrial membrane potential in preapoptotic neurons [19]. The neuroprotective effects of selegiline may also involve neurotrophic factors (nerve growth factor, brain-derive neurotrophic factor, neurotrophin 3) and ligands of glial cell line-derived neurotrophic factor [5, 12], which contribute to neurogenesis in the damaged brains. Excessive generation of NO may also facilitate the pathological production of misfolded proteins, abnormal mitochondrial dynamics (comprised of mitochondrial fission and fusion events), and apoptotic pathways in neuronal cells [40]. Thus, in animal models of PD, S-nitrosylation targets include parkin, a ubiquitin E3 ligase and neuroprotective molecule, and protein-disulfide isomerase (PDI), a chaperone enzyme associated with nascent protein folding. S-nitrosylation of parkin and PDI compromises its ubiquitin E3 ligase and PDI activities and their protective function suggesting that nitrosative stress is an important factor in regulating neuronal survival during the pathogenesis of PD [41, 42]. Significant S-nitrosylation of above proteins may contribute to abnormal mitochondrial fragmentation, resulting in synaptic damage that is found not only in PD but also in other neurodegenerative diseases, such as AD and ALS [40].
4. Inflammatory Responses in Brain
Inflammation is a protective process that not only isolates the injured brain tissue from uninjured area but also destroys affected cells, and repairs the extracellular matrix [31, 43]. Without a strong inflammatory response, brain would be prone to neurotraumatic and neurodegenerative diseases. The main mediators of neuroinflammation are microglial cells. They participate in repair and resolution processes after injury to restore normal tissue homeostasis. Microglial cells also play an important role as resident immunocompetent after neural cell injury and disease. As stated above, during neurodegenerative process, the resting microglial cells are transformed into activated microglia, which are characterized by amoeboid morphology [44]. Activated microglial cells not only migrate rapidly to the site where neurodegenerative process is taking place, but also engulf dead cells, and clear cellular debris [45, 46]. The chronic activation of microglia in PD may cause neuronal damage through the release of potentially cytotoxic molecules such as proinflammatory cytokines, ROS, proteinases and complement proteins [5, 11, 44]. Although very little is known about signaling mechanisms associated with modulation of microglial activation in PD, it is proposed that low levels of cytokines and chemokines released by microglial cells and to lesser extent astrocytes not only facilitate modulation of neurogenesis through the release of trophic factors that protect against ROS, and glutamate, but also promote the removal of dead and damaged neuron [11, 44–46]. In contrast, high levels of glial cell-secreted cytokines and chemokines promote neurodegeneration through the activation of phospholipases A2 and COX-2 [44]. Emerging evidence suggests that microglia have a specialized immune surveillance role and mediate innate immune responses to neurodegenerative process by secreting a myriad of factors that include cytokines, chemokines, prostaglandins, ROS, RNS, and growth factors. Some of these factors have neuroprotective and trophic activities and aid in brain repair processes, while others enhance oxidative stress and trigger neurodegeneration [47].
Two types of inflammatory responses (acute and chronic) occur in brain tissue. Acute inflammation response develops rapidly and may be accompanied by pain, whereas chronic inflammation develops slowly and remains below the threshold of pain perception. As a result, the immune system continues to attack the brain tissue and chronic inflammation lingers for years, ultimately reaching the threshold of detection [31]. Inflammatory response also involves recruitment and migration of polymorphonuclear leukocytes (PMN) and lymphocytes from the blood stream into brain tissue. This is followed by a process called resolution, a turning off mechanism by neural cells to limit tissue injury. Acute inflammation normally resolves spontaneously, but the mechanism associated with this process remains elusive [48].
The chronic activation of microglia may not only cause neuronal damage through the release of proinflammatory cytokines and chemokines, but also ROS, proteinases and complement proteins. Very little is known about molecular mechanisms and internal and external factors that control and modulate the dynamics of acute and chronic neuroinflammation. Collective evidence suggests that inflammatory response involves the interplay not only among microglia, astrocytes, neurons, PMN, and endothelial cells, but also among various lipid mediators that originate from enzymatic and nonenzymatic degradation of neural membrane glycerophospholipids sphingolipids and cholesterol [44, 49]. In addition, transcription factors such as peroxisome proliferator-activated receptor (PPAR) and NF-κB also play an important role in modulation of inflammatory responses.
During inflammatory response expression and activities of a number of enzymes including secretory phospholipase A2 (sPLA2), cytosolic phospholipase A2 (cPLA2), cyclooxygenase-2 (COX-2), and lipoxygenases (LOX), that release ARA and convert it to proinflammatory prostaglandin (PGE2) and leukotriene B4, are markedly increased [44]. Lysophospholipids, the other product of PLA2 catalyzed reaction is converted to proinflammatory lipid mediator, the platelet-activating factor (PAF). Generation of prostaglandins and PAF increases the intensity of inflammatory response [12]. During inflammatory response, upregulation of inducible NOS (iNOS) generates high levels of nitric oxide and peroxynitrite (ONOO−), which not only nitrates proteins but breaks down into hydroxyl radicals promoting further intensification of inflammatory response. In addition, at the site of neurodegenerative process, neural and nonneural cells express and secrete cytokines, chemokine, and complement proteins, which also play important roles in induction, propagation, and maintenance of inflammatory response [12, 44].
Cytokines are major effectors of the inflammatory response. Cytokines produce their effects by interacting with specific membrane-associated receptors. Cytokines play an-important role in neural cell response to neurodegenerative processes [50]. Although physiological levels of cytokines are needed for normal neural cell function and survival, but increased secretion of cytokines during neurodegenerative process can be detrimental to neurons [51]. Tumor necrosis factor-α (TNF-α) and interleukin-1β (IL-1β) are major cytokines that are upregulated in the brain tissue during inflammatory response (Table 1). In addition, interleukin-1α (IL-1α), interleukin-3, interleukin-6 (IL-6), and tumor and growth factors (TGF-α and β) are also secreted by both microglia and astrocytes during inflammatory response. Accumulating evidence suggests that secretion and interactions of various cytokines during inflammatory response may result in their synergistic or antagonistic activities through a complex network that not only involves their feedback loops, but also modulates levels of various lipid mediators by regulating activities of isoforms of PLA2, COX-2, NOS [51, 52]. The consequences of excessive inflammatory response include secretion of high levels of proinflammatory cytokines and chemokines and production of more free radical causing more oxidative stress, which can not only damage neurons through the downregulation of neurotrophins and their receptors but also by blocking neurogenesis. In addition, the interactions of cytokines with their receptors result in activation of cascades of protein kinases, which may lead to the activation of transcription factor, nuclear factor kappa B (NF-κB). Activated NF-κB migrates to the nucleus where it mediates the transcription of many genes implicated in inflammatory and immune responses [44]. These genes include COX-2, intracellular adhesion molecule-1 (ICAM-1), vascular adhesion molecule-1 (VCAM-1), E-selectin, TNF-α, IL-1β, IL-6, sPLA2, inducible nitric oxide synthase (iNOS), and matrix metalloproteinases (MMPs). It is not known whether inflammatory response in neurodegenerative diseases is the consequence or the cause of neurodegeneration [12].
5. Inflammation in PD Brain
Aging, genetic disposition, increase in iron levels, and environmental factors may trigger the abnormality in proteasomal function leading to the initiation and deposition of mutated α-synuclein and induction of Lewy body formation in the brain (Figure 1). Neuromelanin (NM), an iron binding complex polymer pigment, interacts with α-synuclein and contributes to its aggregation. Neuromelanin (NM) occurs in catecholaminergic neurons of the substantia nigra and locus coeruleus in human brains and in brains of different animal species [53]. In brain, the conversion of dopamine to NM through the generation of aminochrome and polymerization is facilitated by iron, and this process is blocked by iron chelator, desferrioxamine [53, 54]. The interactions between iron and NM not only promote NM synthesis but also play an important role in intraneuronal iron homeostasis [53]. In PD, where nigral iron levels are increased, saturation of high-affinity iron-binding sites on NM may saturate the protective capacity of this molecule, leading instead to an increase in redox-active iron, and subsequent cellular damage both in vitro and in vivo [53, 55]. The increase in the release of iron from NM modulates the ubiquitin-proteasome system in mitochondria, leading to the failure to clear proteins such as α-synuclein and to the development of abnormal α-synuclein-immunopositive Lewy bodies that may facilitate the degeneration of dopaminergic neurons in PD [55]. During neurodegenerative process, microgliosis may also play a crucial role. It is proposed that NM acts as a stimulus and triggers microgliosis in animal and cell culture models of PD [56, 57]. This proposal is supported by studies on injections of NM in rat brain cerebral cortex and substantia nigra to monitor microglial cell activation (Iba-1 and/or GFAP antibody) and neurodegeneration (tyrosine hydroxylase) [57]. In this study, LPS injections are used as positive controls and PBS injections are used as negative controls. The injections of LPS induce a strong inflammatory response in the cortex as well in the substantia nigra. Similar results have been obtained in NM injected brains, and PBS injections induce only moderate or no glial activation. However, the inflammatory response declines during the time course when LPS and NM were different. In the NM injected group strong microglia activation is accompanied by a significant dopaminergic cell loss after 1 week of survival time whereas in LPS-injected, brains inflammatory response declines during the time course. These results clearly indicate that extracellular NM may be one of the key molecules leading to microglial activation and neuronal cell death in the substantia nigra [57]. It is proposed that extraneuronal melanin may trigger microgliosis, microglial chemotaxis and microglial activation in PD with subsequent release of neurotoxic mediators. The addition of human NM to microglial cell cultures not only produces positive chemotactic effects, but activates the proinflammatory transcription factor nuclear factor-κB (NF-κB) via phosphorylation and degradation of the inhibitor protein κB (I-κB), and induces an upregulation of TNF-α, IL-6 and NO [56]. In addition, microglial cells secrete a myriad of factors, such as cytokines, chemokines, prostaglandins, ROS and RNS, and growth factors [58]. Some of these factors produce neuroprotective and trophic effects and promote in brain repair processes, while others increase oxidative stress and induce and mediate apoptotic cascades in neurons. Therefore, pro- and anti-inflammatory responses must be in balance to prevent the potential detrimental effects of prolonged or unregulated inflammation-induced oxidative stress on vulnerable neuronal populations. Accumulating evidence suggests that in PD degeneration of dopaminergic neurons in substantia nigra is accompanied not only by the progressive loss of NM but also by the induction of microgliosis [59]. Although NM particles are phagocytized and degraded by microglial cells within minutes, but extracellular NM particle-mediated microglial activation results in the generation of superoxide, nitric oxide, hydrogen peroxide, and other proinflammatory factors including cytokines and chemokines, which support oxidative stress and inflammation in the brain [36, 37, 59].
6. Conclusions
PD is a common neurodegenerative movement disorder, which affects increasing number of elderly population. The disorder is caused by a selective degeneration of dopaminergic neurons in the substantia nigra pars compacta. Although the molecular mechanism associated with neurodegeneration in PD is not known, it is becoming increasingly evident that neurodegeneration in PD is a multifactorial process that may involve monoamine oxidase-mediated abnormal dopamine metabolism, increase in iron levels, hydrogen peroxide generation, abnormal mitochondrial and proteasomal function along with microgliosis may be closely associated with the pathogenesis of PD. Microglial cells play a critical role in forming a self-propelling cycle leading to sustained chronic neuroinflammation and driving the progressive neurodegeneration in PD. The above-mentioned processes have been shown to contribute to the oxidative stress, accumulation of α-synuclein, and neuroinflammation not only in cell culture and animal models of PD, but also in brains of PD patients.
Acknowledgments
The authors would like to thank Prof. Carlos Barcia at SAGE-Hindawi for carefully reviewing and editing this manuscript.
References
- 1.Beal MF. Mitochondrial dysfunction in neurodegenerative diseases. Biochimica et Biophysica Acta. 1998;1366(1-2):211–223. doi: 10.1016/s0005-2728(98)00114-5. [DOI] [PubMed] [Google Scholar]
- 2.Jenner P, Olanow CW. The pathogenesis of cell death in Parkinson’s disease. Neurology. 2006;66(10, supplement 4):S24–S36. doi: 10.1212/wnl.66.10_suppl_4.s24. [DOI] [PubMed] [Google Scholar]
- 3.Farrer MJ, Haugarvoll K, Ross OA, et al. Genomewide association, Parkinson disease, and PARK10. American Journal of Human Genetics. 2006;78(6):1084–1088. doi: 10.1086/504728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lücking CB, Dürr A, Bonifati V, et al. Association between early-onset Parkinson's disease and mutations in the parkin gene. New England Journal of Medicine. 2000;342(21):1560–1567. doi: 10.1056/NEJM200005253422103. [DOI] [PubMed] [Google Scholar]
- 5.Farooqui AA. Neurochemical Aspects of Neuroinflammation in Brain in Molecular Aspects of Neurodegeneration and Neuroprotection. Oak Park, Ill, USA: Bentham Science; 2010. A. A. Farooqui and T. Farooqui, Eds. [Google Scholar]
- 6.Wang C, Liu L, Zhang L, Peng Y, Zhou F. Redox reactions of the α-synuclein-Cu2+ complex and their effects on neuronal cell viability. Biochemistry. 2010;49(37):8134–8142. doi: 10.1021/bi1010909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halliwell B. Oxidative stress and neurodegeneration: where are we now? Journal of Neurochemistry. 2006;97(6):1634–1658. doi: 10.1111/j.1471-4159.2006.03907.x. [DOI] [PubMed] [Google Scholar]
- 8.Sun GY, Horrocks LA, Farooqui AA. The roles of NADPH oxidase and phospholipases A2 in oxidative and inflammatory responses in neurodegenerative diseases. Journal of Neurochemistry. 2007;103(1):1–16. doi: 10.1111/j.1471-4159.2007.04670.x. [DOI] [PubMed] [Google Scholar]
- 9.Farooqui AA, Ong WY, Horrocks LA. Neurochemical Aspects of Excitotoxicity. New York, NY, USA: Springer; 2008. [Google Scholar]
- 10.Farooqui AA, Horrocks LA. Glycerophospholipids in Brain. New York, NY, USA: Springer; 2007. [Google Scholar]
- 11.Valko M, Morris H, Cronin MTD. Metals, toxicity and oxidative stress. Current Medicinal Chemistry. 2005;12(10):1161–1208. doi: 10.2174/0929867053764635. [DOI] [PubMed] [Google Scholar]
- 12.Farooqui AA. Neurochemical Aspects of Neurotraumatic and Neurodegenerative Disease. New York, NY, USA: Springer; 2010. [Google Scholar]
- 13.Fernstrom JD. Effects of dietary polyunsaturated fatty acids on neuronal function. Lipids. 1999;34(2):161–169. doi: 10.1007/s11745-999-0350-3. [DOI] [PubMed] [Google Scholar]
- 14.Buisson A, Lakhmeche N, Verrecchia C, Plotkine M, Boulu RG. Nitric oxide: an endogenous anticonvulsant substance. NeuroReport. 1993;4(4):444–446. [PubMed] [Google Scholar]
- 15.Jenkinson AM, Collins AR, Duthie SJ, Wahle KWJ, Duthie GG. The effect of increased intakes of polyunsaturated fatty acids and vitamin E on DNA damage in human lymphocytes. FASEB Journal. 1999;13(15):2138–2142. doi: 10.1096/fasebj.13.15.2138. [DOI] [PubMed] [Google Scholar]
- 16.Shibata N, Kobayashi M. The role for oxidative stress in neurodegenerative diseases. Brain and Nerve. 2008;60(2):157–170. [PubMed] [Google Scholar]
- 17.Lipton SA, Gu Z, Nakamura T. Inflammatory mediators leading to protein misfolding and uncompetitive/fast off-rate drug therapy for neurodegenerative disorders. International Review of Neurobiology. 2007;82:1–27. doi: 10.1016/S0074-7742(07)82001-0. [DOI] [PubMed] [Google Scholar]
- 18.Nakamura T, Lipton SA. Emerging roles of S-nitrosylation in protein misfolding and neurodegenerative diseases. Antioxidants and Redox Signaling. 2008;10(1):87–101. doi: 10.1089/ars.2007.1858. [DOI] [PubMed] [Google Scholar]
- 19.Ebadi M, Sharma SK. Peroxynitrite and mitochondrial dysfunction in the pathogenesis of Parkinson’s disease. Antioxidants and Redox Signaling. 2003;5(3):319–335. doi: 10.1089/152308603322110896. [DOI] [PubMed] [Google Scholar]
- 20.Branco DM, Arduino DM, Esteves AR, Silva DF, Cardoso SM, Oliveira CR. Cross-talk between mitochondria and proteasome in Parkinson’s disease pathogenesis. Frontiers in Aging Neuroscience. 2010;2, article 17 doi: 10.3389/fnagi.2010.00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Atlante A, Calissano P, Bobba A, Azzariti A, Marra E, Passarella S. Cytochrome c is released from mitochondria in a reactive oxygen species (ROS)-dependent fashion and can operate as a ROS scavenger and as a respiratory substrate in cerebellar neurons undergoing excitotoxic death. Journal of Biological Chemistry. 2000;275(47):37159–37166. doi: 10.1074/jbc.M002361200. [DOI] [PubMed] [Google Scholar]
- 22.Dronne MA, Grenier E, Dumont T, Hommel M, Boissel JP. Role of astrocytes in grey matter during stroke: a modelling approach. Brain Research. 2007;1138(1):231–242. doi: 10.1016/j.brainres.2006.12.062. [DOI] [PubMed] [Google Scholar]
- 23.Khan FH, Sen T, Maiti AK, Jana S, Chatterjee U, Chakrabarti S. Inhibition of rat brain mitochondrial electron transport chain activity by dopamine oxidation products during extended in vitro incubation: implications for Parkinson’s disease. Biochimica et Biophysica Acta. 2005;1741(1-2):65–74. doi: 10.1016/j.bbadis.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 24.Bisaglia M, Soriano ME, Arduini I, Mammi S, Bubacco L. Molecular characterization of dopamine-derived quinones reactivity toward NADH and glutathione: implications for mitochondrial dysfunction in Parkinson disease. Biochimica et Biophysica Acta. 2010;1802(9):699–706. doi: 10.1016/j.bbadis.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 25.Klivenyi P, Beal MF, Ferrante RJ, et al. Mice deficient in group IV cytosolic phospholipase A2 are resistant to MPTP neurotoxicity. Journal of Neurochemistry. 1998;71(6):2634–2637. doi: 10.1046/j.1471-4159.1998.71062634.x. [DOI] [PubMed] [Google Scholar]
- 26.Singer TP, Castagnoli N, Jr., Ramsay RR, Trevor AJ. Biochemical events in the development of parkinsonism induced by 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine. Journal of Neurochemistry. 1987;49(1):1–8. doi: 10.1111/j.1471-4159.1987.tb03384.x. [DOI] [PubMed] [Google Scholar]
- 27.Tariq M, Khan HA, Moutaery KA, Deeb SA. Protective effect of quinacrine on striatal dopamine levels in 6-OHDA and MPTP models of Parkinsonism in rodents. Brain Research Bulletin. 2001;54(1):77–82. doi: 10.1016/s0361-9230(00)00427-5. [DOI] [PubMed] [Google Scholar]
- 28.Yoshinaga N, Yasuda Y, Murayama T, Nomura Y. Possible involvement of cytosolic phospholipase A2 in cell death induced by 1-methyl-4-phenylpyridinium ion, a dopaminergic neurotoxin, in GH3 cells. Brain Research. 2000;855(2):244–251. doi: 10.1016/s0006-8993(99)02340-9. [DOI] [PubMed] [Google Scholar]
- 29.Feng Z, Li D, Fung PCW, Pei Z, Ramsden DB, Ho SL. COX-2-deficient mice are less prone to MPTP-neurotoxicity than wild-type mice. NeuroReport. 2003;14(15):1927–1929. doi: 10.1097/00001756-200310270-00009. [DOI] [PubMed] [Google Scholar]
- 30.Teismann P, Vila M, Choi DK, et al. COX-2 and neurodegeneration in Parkinson’s disease. Annals of the New York Academy of Sciences. 2003;991:272–277. doi: 10.1111/j.1749-6632.2003.tb07482.x. [DOI] [PubMed] [Google Scholar]
- 31.Wood PL. Neuroinflammation: Mechanisms and Managements. Totowa, NJ, USA: Humana Press; 1998. [Google Scholar]
- 32.Seet RCS, Lee CYJ, Lim ECH, et al. Oxidative damage in Parkinson disease: measurement using accurate biomarkers. Free Radical Biology and Medicine. 2010;48(4):560–566. doi: 10.1016/j.freeradbiomed.2009.11.026. [DOI] [PubMed] [Google Scholar]
- 33.Büeler H. Impaired mitochondrial dynamics and function in the pathogenesis of Parkinson’s disease. Experimental Neurology. 2009;218(2):235–246. doi: 10.1016/j.expneurol.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 34.Beyer K. Mechanistic aspects of Parkinson’s disease: α-synuclein and the biomembrane. Cell Biochemistry and Biophysics. 2007;47(2):285–299. doi: 10.1007/s12013-007-0014-9. [DOI] [PubMed] [Google Scholar]
- 35.Ghosh A, Roy A, Liu X, et al. Selective inhibition of NF-κB activation prevents dopaminergic neuronal loss in a mouse model of Parkinson’s disease. Proceedings of the National Academy of Sciences of the United States of America. 2007;104(47):18754–18759. doi: 10.1073/pnas.0704908104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sawada M, Imamura K, Nagatsu T. Role of cytokines in inflammatory process in Parkinson’s disease. Journal of Neural Transmission, Supplement. 2006;(70):373–381. doi: 10.1007/978-3-211-45295-0_57. [DOI] [PubMed] [Google Scholar]
- 37.Nagatsu T, Sawada M. Inflammatory process in Parkinson’s disease: role for cytokines. Current Pharmaceutical Design. 2005;11(8):999–1016. doi: 10.2174/1381612053381620. [DOI] [PubMed] [Google Scholar]
- 38.Nagatsu T, Mogi M, Ichinose H, Togari A. Changes in cytokines and neurotrophins in Parkinson’s disease. Journal of Neural Transmission, Supplement. 2000;(60):277–290. doi: 10.1007/978-3-7091-6301-6_19. [DOI] [PubMed] [Google Scholar]
- 39.Calabrese V, Cornelius C, Rizzarelli E, Owen JB, Dinkova-Kostova AT, Butterfield DA. Nitric oxide in cell survival: a janus molecule. Antioxidants & Redox Signaling. 2009;11(11):2717–2739. doi: 10.1089/ars.2009.2721. [DOI] [PubMed] [Google Scholar]
- 40.Nakamura T, Lipton SA. S-nitrosylation of critical protein thiols mediates protein misfolding and mitochondrial dysfunction in neurodegenerative diseases. doi: 10.1089/ars.2010.3570. Antioxidants and Redox Signaling. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tsang AHK, Chung KKK. Oxidative and nitrosative stress in Parkinson’s disease. Biochimica et Biophysica Acta. 2009;1792(7):643–650. doi: 10.1016/j.bbadis.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 42.Chung KKK, Thomas B, Li X, et al. S-nitrosylation of parkin regulates ubiquitination and compromises Parkin’s protective function. Science. 2004;304(5675):1328–1331. doi: 10.1126/science.1093891. [DOI] [PubMed] [Google Scholar]
- 43.Correale J, Villa A. The neuroprotective role of inflammation in nervous system Injuries. Journal of Neurology. 2004;251(11):1304–1316. doi: 10.1007/s00415-004-0649-z. [DOI] [PubMed] [Google Scholar]
- 44.Farooqui AA, Horrocks LA, Farooqui T. Modulation of inflammation in brain: a matter of fat. Journal of Neurochemistry. 2007;101(3):577–599. doi: 10.1111/j.1471-4159.2006.04371.x. [DOI] [PubMed] [Google Scholar]
- 45.Hirsch EC, Hunot S. Neuroinflammation in Parkinson’s disease: a target for neuroprotection? The Lancet Neurology. 2009;8(4):382–397. doi: 10.1016/S1474-4422(09)70062-6. [DOI] [PubMed] [Google Scholar]
- 46.Long-Smith CM, Sullivan AM, Nolan YM. The influence of microglia on the pathogenesis of Parkinson’s disease. Progress in Neurobiology. 2009;89(3):277–287. doi: 10.1016/j.pneurobio.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 47.Tansey MG, Goldberg MS. Neuroinflammation in Parkinson’s disease: its role in neuronal death and implications for therapeutic intervention. Neurobiology of Disease. 2010;37(3):510–518. doi: 10.1016/j.nbd.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Serhan CN, Savill J. Resolution of inflammation: the beginning programs the end. Nature Immunology. 2005;6(12):1191–1197. doi: 10.1038/ni1276. [DOI] [PubMed] [Google Scholar]
- 49.Farooqui AA, Horrocks LA, Farooqui T. Interactions between neural membrane glycerophospholipid and sphingolipid mediators: a recipe for neural cell survival or suicide. Journal of Neuroscience Research. 2007;85(9):1834–1850. doi: 10.1002/jnr.21268. [DOI] [PubMed] [Google Scholar]
- 50.Amor S, Puentes F, Baker D, van der Valk P. Inflammation in neurodegenerative diseases. Immunology. 2010;129(2):154–169. doi: 10.1111/j.1365-2567.2009.03225.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wilson CJ, Finch CE, Cohen HJ. Cytokines and cognition—the case for a head-to-toe inflammatory paradigm. Journal of the American Geriatrics Society. 2002;50(12):2041–2056. doi: 10.1046/j.1532-5415.2002.50619.x. [DOI] [PubMed] [Google Scholar]
- 52.Xing Z, Gauldie J, Cox G, et al. IL-6 is an antiinflammatory cytokine required for controlling local or systemic acute inflammatory responses. Journal of Clinical Investigation. 1998;101(2):311–320. doi: 10.1172/JCI1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sulzer D, Bogulavsky J, Larsen KE, et al. Neuromelanin biosynthesis is driven by excess cytosolic catecholamines not accumulated by synaptic vesicles. Proceedings of the National Academy of Sciences of the United States of America. 2000;97(22):11869–11874. doi: 10.1073/pnas.97.22.11869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Paris I, Lozano J, Perez-Pastene C, Muñoz P, Segura-Aguilar J. Molecular and neurochemical mechanisms in PD pathogenesis. Neurotoxicity Research. 2009;16(3):271–279. doi: 10.1007/s12640-009-9059-4. [DOI] [PubMed] [Google Scholar]
- 55.Gerlach M, Riederer P, Double KL. Neuromelanin-bound ferric iron as an experimental model of dopaminergic neurodegeneration in Parkinson’s disease. Parkinsonism and Related Disorders. 2008;14(supplement 2):S185–S188. doi: 10.1016/j.parkreldis.2008.04.028. [DOI] [PubMed] [Google Scholar]
- 56.Wilms H, Zecca L, Rosenstiel P, Sievers J, Deuschl G, Lucius R. Inflammation in Parkinson’s diseases and other neurodegenerative diseases: cause and therapeutic implications. Current Pharmaceutical Design. 2007;13(18):1925–1928. doi: 10.2174/138161207780858429. [DOI] [PubMed] [Google Scholar]
- 57.Zecca L, Wilms H, Geick S, et al. Human neuromelanin induces neuroinflammation and neurodegeneration in the rat substantia nigra: implications for Parkinson’s disease. Acta Neuropathologica. 2008;116(1):47–55. doi: 10.1007/s00401-008-0361-7. [DOI] [PubMed] [Google Scholar]
- 58.Tansey MG, Goldberg MS. Neuroinflammation in Parkinson’s disease: its role in neuronal death and implications for therapeutic intervention. Neurobiology of Disease. 2010;37(3):510–518. doi: 10.1016/j.nbd.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang W, Phillips K, Wielgus AR, et al. Neuromelanin activates microglia and induces degeneration of dopaminergic neurons: implications for progression of Parkinson's disease. Neurotoxicity Research. 2011;19(1):63–72. doi: 10.1007/s12640-009-9140-z. [DOI] [PMC free article] [PubMed] [Google Scholar]