Summary
Background
Over 2.3 million (M) children died in India in 2005. All-cause mortality rates vary greatly across the regions of India and by gender. However, the major causes of child deaths have not yet been measured directly.
Methods
The Registrar General of India conducted a survey of all deaths occurring in 2001-03 in 1.1 M nationally representative homes. About 800 field staff interviewed households and completed standard questions and a half-page narrative about the events that preceded the death. Each field report was sent to two of 130 trained physicians, who independently assigned an ICD-10 code to each death. Discrepancies were resolved via anonymous reconciliation and, if necessary, adjudication. Cause-specific mortality rates for 2005 were calculated nationally and for the six regions by combining the observed proportions for each cause among 10 892 deaths in neonates and 12 260 deaths at ages 1-59 months with United Nations population and death totals.
Findings
Three causes accounted for 78% (0.79 M/1.01 M) of all neonatal deaths in India: prematurity & low birthweight (0.33 M; 99%CI 0.31-0.35 M), neonatal infections (0.27 M; 99%CI 0.25-0.29 M) and birth asphyxia & birth trauma (0.19 M; 99%CI 0.18-0.21 M). Two causes accounted for 50% (0.67 M/1.34 M) of all deaths at ages 1-59 months: pneumonia (0.37 M; 99%CI 0.35-0.39 M) and diarrhoeal diseases (0.30 M; 99%CI 0.28-0.32 M). At these ages, girls in Central India had a five times higher mortality rate (per 1000 live births) from pneumonia (20.9) compared to boys in South India (4.1) and had four times higher the diarrhoeal disease mortality rate (17.7) compared to boys in the West (4.1). Pneumonia and diarrhoea accounted for about two-thirds (0.1 M/0.15 M) of the excess girl deaths at ages 1-59 months.
Interpretation
Five major causes accounted for nearly 1.5 M child deaths in India in 2005, with remarkable regional and gender differences. Lower access for girls to effective prevention and treatment health services are likely responsible for the marked gender differences in mortality.
Introduction
Annual child mortality rates in India have decreased between 1.7% 1 and 2.3% 2 in the last two decades. Still, the United Nations (UN) estimates that about 2.35 million (M) children died in India in 2005. This corresponds to over 20% of the world's under-five deaths, more than any other country. 1, 3 Large differences in overall child survival between India's diverse regions have been previously documented. 4, 5 However, there is no direct and nationally-representative measurement of the major causes of death among neonates (first month of life) and at ages 1-59 months, 6, 7 and it remains unknown how these causes of death vary across India's regions. Social preference for boys is strong, as noted by widespread selective abortion of female fetuses before birth 7 and by lower immunization rates among girls. 8 The consequences of boy preference on child mortality remain undocumented. Understanding the causes of child death may, therefore, help to guide the use of widely practicable interventions for neonatal and child survival. 9, 10
Here we present the results of the first ever nationally representative survey of the causes of child deaths in India, separately for the neonatal period and at ages 1-59 months, for boys and girls and for each of six major regions of India (figure 1).
Figure 1. Annual number of livebirths and deaths at age 0–4 years in India, by region, 2005.

M=millions
*These poorer states are known as the ‘Empowered Action Group plus Assam’ (EAGA) states.
Methods
Most deaths in India, including of children, are not medically certified since the majority occurs at home, in rural areas, and without prior attention by a healthcare worker.11 Thus, other sources of information are needed to help determine the probable underlying causes of death. During the past decade the Registrar General of India (RGI) has introduced an enhanced form of verbal autopsy called RHIME or Routine, Reliable, Representative, Re-sampled Household Investigation of Mortality with Medical Evaluation, 12 into its nationally representative Sample Registration System (SRS), which covered about 6.3 M people and monitored all deaths in 1.1 M homes. 5 This mortality survey is part of the Million Death Study (MDS), which seeks to assign causes to all deaths in the SRS areas during the 13 years from 2001-13. Details of the MDS design, methods and preliminary results have been previously published. 5, 12-15
Study setting and field procedures
India was divided into about one million areas for the 1991 census, each with approximately 1000 inhabitants. The RGI chose 6671 such areas randomly for the SRS in 1993, each with all individuals and their household characteristics documented and with subsequent births and deaths (but not death causes) enumerated monthly by a part time enumerator resident in that area, and independently surveyed twice yearly by one of 800 full time RGI surveyors (trained non-medical graduates). Each of these RGI surveyors has visited, since 2002, each SRS area periodically to record from families (or other informants) a written narrative describing the events that preceded the death, in the local language, in addition to answers to standard questions on key symptoms. Separate forms for neonatal deaths and deaths at ages 1 month to 14 years were used, drawing on a WHO multi-country validation study of verbal autopsy for common causes of childhood deaths, 16 and were pre-tested in about 500 child deaths in India. 7 Random re-sampling and other fieldwork quality control methods were used. 7 Respondents for the 23 152 child deaths were the father (22.1%; 5117), mother (35.0%; 8103), siblings and other relatives (21.8%; 5047), grandparents (15.6%; 3612) or a neighbor or non-relative (5.5%; 1273).
Central medical coding of causes of death
Along with symptom data, each of the local language narratives were electronically scanned and sent randomly (based on the language of the narrative) to two of 130 collaborating physicians trained in disease coding who, working independently, assessed the probable underlying cause of death, and assigned an International Classification of Diseases, 10th revision (ICD-10) 3-character code using structured guidelines for each major disease group (published online 17). Disagreements on the ICD-10 codes assigned by the two physicians were resolved by anonymous reconciliation (i.e. asking each to reconsider) and for persisting differences, adjudication by a third physician. Separate classification systems were developed for the causes of neonatal deaths and at ages 1-59 months, based on input from the Child Health and Epidemiology Reference Group 9 (webappendix pp 5-7).
National and sub-national mortality rates
The age and sex-specific proportions of each cause of death were calculated (weighted according to the SRS sampling fractions in the rural and urban areas of each state 18). We applied the proportions of each cause of death to the independent UN Population Division estimates of livebirths (27.3 M) and deaths (2.35 M) in India in 2005 1 to calculate age- and sex-specific mortality rates (per 1000 livebirths) and absolute deaths by cause. The UN totals were used because the SRS slightly underestimates child mortality rates 19, 20 and because about 12% of the SRS-enumerated deaths were unavailable for interview in our survey. The UN totals for 2005 were used as these were most complete, could be compared to the available Indian Census projections for 2006 and were prior to the implementation of a new national health program to reduce child mortality. 10 Applying the 2001-03 proportions to the 2005 total deaths did not introduce major biases since there was little change in the yearly distribution of causes of deaths in our survey or between 2001 and 2004 in an independent survey of medically certified causes of death from selected urban hospitals. 7
To calculate sub-national mortality rates, we partitioned the UN total births and child deaths into 140 strata (35 states, rural and urban areas, and both genders) using the Census of India 2005 population, 21 relative SRS birth and death rates 5 or smaller demographic surveys 4 when SRS data were not available (details in webappendix pp 1-4). Sub-national results were produced for the six regions: North, South, West, Central, Northeast and East, 18 and for the poorer states with historically higher child mortality rates and poverty levels (Assam, Bihar, Chhattisgarh, Jharkhand, Madhya Pradesh, Orissa, Rajasthan, Uttarakhand, Uttar Pradesh) and the remaining states (figure 1). The 99% confidence intervals for each cause of death proportion or rate were calculated using Taylor linearization 22 based on the survey design and the observed sample deaths in the MDS. All statistical analyses were performed using Stata/SE version 10.1.
Role of the funding source
The study was funded by the US National Institutes of Health, International Development Research Centre, Canadian Institute of Health Research, the Li Ka Shing Knowledge Institute and the US Fund for UNICEF (via a grant from the Bill & Melinda Gates Foundation for CHERG). The funding sources had no role in study design or conduct, data collection, analysis, interpretation or in the decision to submit this manuscript for publication. The senior author had full access to all data and had final responsibility for the decision to submit for publication on behalf of all authors.
Results
Of the 24 841 child deaths surveyed, 93% (23 152) were double-coded by physicians and included in the study (table 1). Reasons for exclusion were missing age and/or gender (n=191), and non-legible forms, improper scanning of narrative or incorrect language code (n=1498). Most child deaths occurred in rural areas, and this varied little by cause. Only 17% (3877/23 152) died in a health facility with large variations between rural and urban areas, and between states (webtable 3). Physicians agreed on the cause of death initially for 62% (14 410/23 152) of all deaths (additional details already published 23).
Table 1. Causes of death in neonates and at age 1–59 months in the present study and estimated national totals.
| Study deaths, 2001-03 | All India, 2005 | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cause | Boys | / | Girls | / | Total | Rural area | Died in a health facility | Two coders immediately agreed | Mortality rate per 1000 livebirths | Total deaths (thousands) | ||||||||
| Boys | / | Girls | / | Total | Boys | / | Girls | / | Total (99%CI) | |||||||||
| Neonatal (<1 month) | ||||||||||||||||||
| Prematurity & low birthweight * | 2012 | / | 1619 | / | 3631 | 3265 | 988 | 2381 | 13.0 | / | 10.8 | / | 12.0 | 185 | / | 142 | / | 327 (309–345) |
| Infections† | 1544 | / | 1339 | / | 2883 | 2694 | 346 | 1804 | 10.3 | / | 9.4 | / | 9.9 | 145 | / | 123 | / | 268 (253–286) |
| Birth asphyxia & birth trauma | 1219 | / | 854 | / | 2073 | 1869 | 631 | 946 | 8.0 | / | 5.9 | / | 7.0 | 113 | / | 77 | / | 190 (176–206) |
| Other noncommunicable diseases | 316 | / | 243 | / | 559 | 502 | 118 | 251 | 2.0 | / | 1.6 | / | 1.8 | 28 | / | 21 | / | 49 (42–58) |
| Congenital anomalies | 213 | / | 146 | / | 359 | 304 | 139 | 202 | 1.4 | / | 1.0 | / | 1.2 | 20 | / | 13 | / | 33 (28–42) |
| Diarrhoeal diseases | 175 | / | 162 | / | 337 | 318 | 26 | 227 | 1.2 | / | 1.2 | / | 1.2 | 17 | / | 15 | / | 32 (26–40) |
| Tetanus | 149 | / | 115 | / | 264 | 255 | 14 | 180 | 1.3 | / | 1.0 | / | 1.2 | 18 | / | 14 | / | 32 (26–39) |
| Injuries | 27 | / | 20 | / | 47 | 43 | 8 | 15 | 0.2 | / | 0.1 | / | 0.2 | 3 | / | 2 | / | 5 (3–8) |
| Other causes | 414 | / | 325 | / | 739 | 665 | 147 | 329 | 2.7 | / | 2.5 | / | 2.4 | 39 | / | 33 | / | 72 (61–81) |
| All causes (%) | 6069 | / | 4823 | / | 10 892 | 9915 (91.0%) | 2417 (22.2%) | 6335 (58.2%) | 40.1 | / | 33.5 | / | 36.9 | 568 | / | 440 | / | 1008 – |
| 1 to 59 months | ||||||||||||||||||
| Pneumonia | 1542 | / | 1890 | / | 3432 | 3146 | 404 | 2546 | 11.2 | / | 16.0 | / | 13.5 | 159 | / | 210 | / | 369 (348–390) |
| Diarrhoeal diseases | 1184 | / | 1532 | / | 2716 | 2480 | 293 | 2146 | 8.9 | / | 13.4 | / | 11.1 | 126 | / | 176 | / | 302 (283–323) |
| Measles | 308 | / | 450 | / | 758 | 687 | 64 | 374 | 2.5 | / | 4.2 | / | 3.3 | 36 | / | 56 | / | 92 (79–104) |
| Other noncommunicable diseases | 418 | / | 433 | / | 851 | 772 | 142 | 490 | 3.0 | / | 3.5 | / | 3.2 | 42 | / | 46 | / | 88 (77–100) |
| Injuries | 400 | / | 357 | / | 757 | 689 | 91 | 673 | 2.9 | / | 2.9 | / | 2.9 | 42 | / | 38 | / | 80 (68–92) |
| Malaria | 262 | / | 325 | / | 587 | 562 | 43 | 354 | 1.7 | / | 2.4 | / | 2.0 | 24 | / | 32 | / | 56 (47–65) |
| Meningitis/encephalitis | 232 | / | 209 | / | 441 | 396 | 94 | 183 | 1.9 | / | 1.9 | / | 1.9 | 27 | / | 25 | / | 52 (43–62) |
| Nutritional diseases | 141 | / | 201 | / | 342 | 303 | 18 | 190 | 1.1 | / | 1.9 | / | 1.5 | 16 | / | 25 | / | 41 (34–51) |
| Acute bacterial sepsis & severe infections | 147 | / | 213 | / | 360 | 324 | 50 | 117 | 1.1 | / | 1.8 | / | 1.4 | 15 | / | 23 | / | 38 (31–47) |
| Other infectious diseases | 143 | / | 182 | / | 325 | 298 | 43 | 120 | 1.0 | / | 1.5 | / | 1.2 | 14 | / | 19 | / | 33 (27–41) |
| Other causes | 847 | / | 844 | / | 1691 | 1490 | 218 | 882 | 6.4 | / | 7.2 | / | 6.9 | 91 | / | 95 | / | 186 (170–203) |
| All causes (%) | 5624 | / | 6636 | / | 12 260 | 11 147 (90.9%) | 1460 (11.9%) | 8075 (65.9%) | 41.7 | / | 56.7 | / | 48.9 | 592 | / | 745 | / | 1337 – |
| 0 to 4 years | ||||||||||||||||||
| All causes (%) | 11 693 | / | 11 459 | / | 23 152 | 21 062 (91.0%)‡ | 3877 (16.7%)‡ | 14 410 (62.2%) | 81.8 | / | 90.2 | / | 85.8 | 1160 | / | 1185 | / | 2345 – |
Total livebirths (2005): 27.3 million; Boys/Girls: 14.2 million/13.1 million.
Estimates exclude stillbirths, cancelled reports (i.e. not coded), and children with missing information on gender or age. The percentage of deaths that could not be coded was 6.5% among boys, 5.6% among girls, 8.0% in urban areas and 5.8% in rural areas.
Prematurity MR (99%CI)/estimated total deaths for boys: 9.5 (8.9–10.1)/135 000; for girls: 7.4 (6.9–8.0)/97 000; for both: 8.5 (8.1–8.9)/232 000. Low birthweight MR (99%CI)/estimated total deaths for boys: 3.5 (3.1–3.9)/50 000; for girls: 3.4 (3.0–3.9)/45 000; for both: 3.5 (3.2–3.8)/95 000. These two conditions are combined given the difficulty in differentiating them in verbal autopsies.
Infections category includes pneumonia [MR (99%CI)/estimated total deaths for boys: 60 (5.5–6.5)/85 000; for girls: 5.8 (5.3–6.3)/76 000; for both: 5.9 (5.5–6.3)/161 000]; sepsis [MR (99%CI)/estimated total deaths for boys: 4.2 (3.8–4.7)/60 000; for girls: 3.6 (3.2–4.0)/47 000; for both: 3.9 (3.6–4.2)/107 000); and infections of the central nervous system (approximately 2000 deaths annually). These three conditions are combined given the difficulty in differentiating them in verbal autopsies.
Sample-weighted percentage of deaths: 87.1% occurred in a rural area, 16.6% occurred in a health facility.
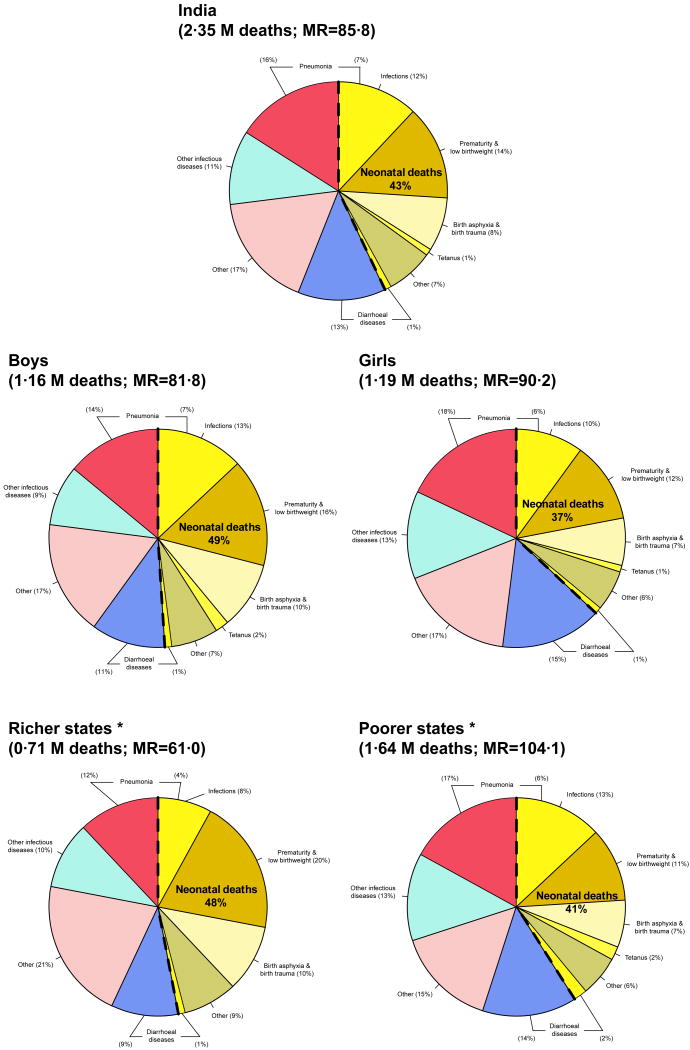
The under-five mortality rate per 1000 livebirths was 85.8 (81.8 for boys and 90.2 for girls). Five causes accounted for 62% (1.46 M/2.35 M) of all child deaths: pneumonia, prematurity & low birthweight, diarrhoeal diseases, neonatal infections and birth asphyxia & birth trauma. The gender and regional distribution of the five leading causes of child deaths varied among neonates and at ages 1-59 months (figures 2-5). Each age group is presented in turn. Estimates of deaths and mortality rates for the top causes of death for the major states of India are shown in the webappendix (webtable 4A-C; webfigures 2-6).
Figure 2. Causes of death at age 0–4 years in India, by gender and by richer/poorer states, 2001-03.
MR=under-five mortality rate
*Poorer states are the EAGA states (Assam, Bihar, Chhattisgarh, Jharkhand, Madhya Pradesh, Orissa, Rajasthan, Uttarakhand and Uttar Pradesh); richer states are the remaining 26 states/union territories.
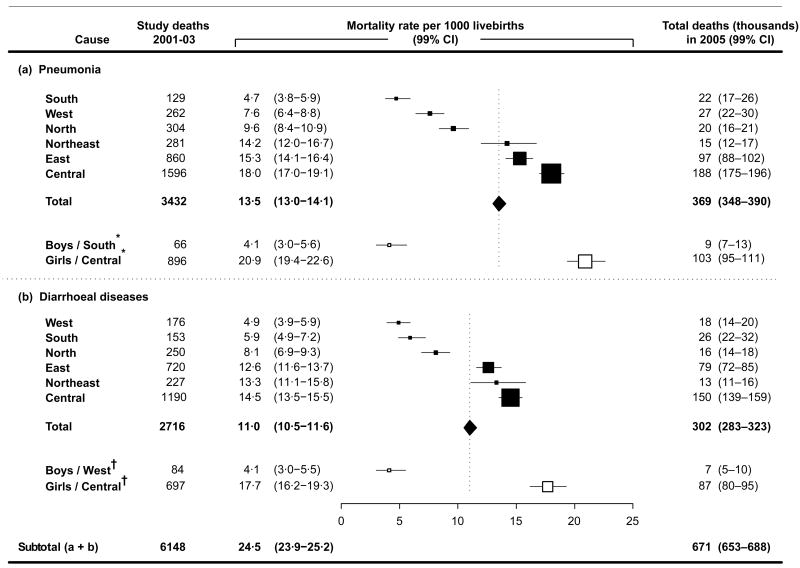
Figure 5. Mortality rates for the two leading causes of death at age 1–59 months in India, by region, 2005.
*Boys from the South region have the lowest mortality rate for pneumonia by gender and region (at age 1–59 months), and girls from the Central region have the highest.
† Boys from the West region have the lowest mortality rate for diarrhoeal diseases by gender and region (at age 1–59 months), and girls from the Central region have the highest.
Neonatal deaths (<1 month)
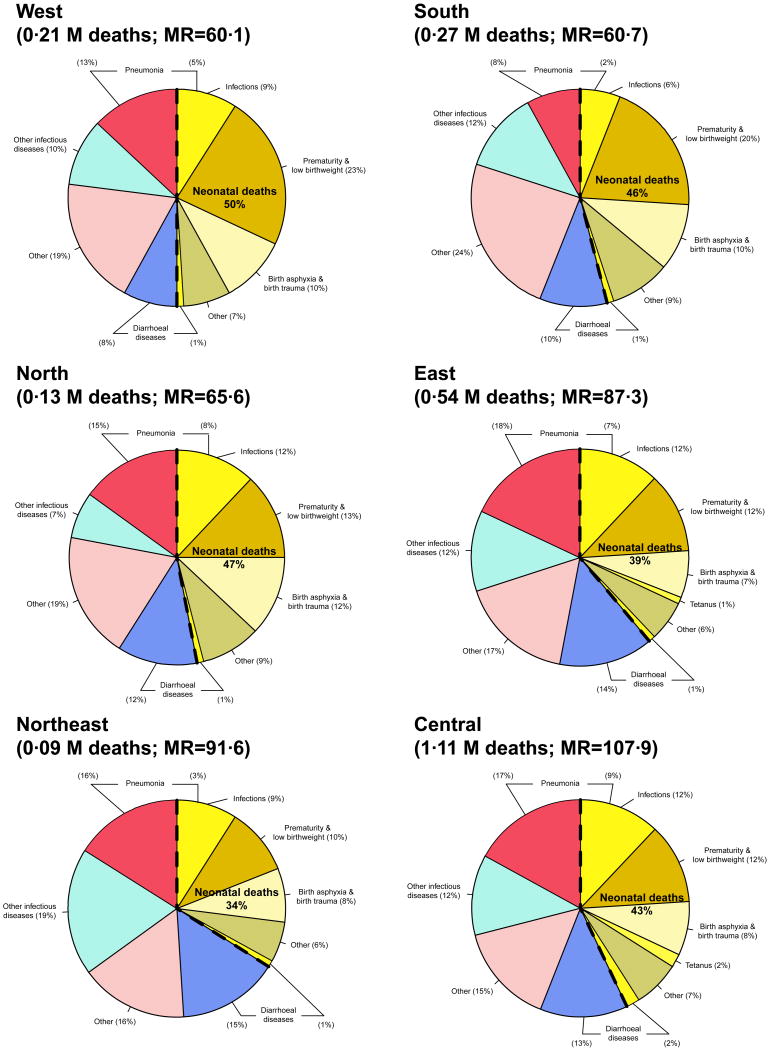
Three causes accounted for 78% (0.79 M/1.01 M) of all neonatal deaths in India: prematurity & low birthweight (0.33 M deaths, 99%CI 0.31-0.35 M; mortality rate per 1000 livebirths [MR] = 12.0); neonatal infections, comprising pneumonia, neonatal sepsis and infections of the central nervous system (0.27 M deaths, 99%CI 0.25-0.29 M; MR = 9.9); and birth asphyxia & birth trauma (0.19 M deaths, 99% CI 0.18-0.21 M; MR = 7.0). The proportion of under-five deaths that were neonatal was higher among boys than girls and in the richer states than in the poorer states (table 1; figure 2). The neonatal proportion generally rose as under-five mortality rates declined (figure 3). All-cause neonatal mortality rate was about 20% higher among boys (40.1) than girls (33.5), and mortality rates were higher for most causes among boys than girls, although mortality rates were comparable between boys and girls for diarrhoeal diseases. Mortality rates from neonatal infections were higher in the poorer states (31.0) than in the richer states (17.5), but were high in all regions. Prematurity & low birthweight formed a greater proportion of all child deaths in the West and South India compared to other regions. Tetanus was a notable cause of death in Central and East India.
Figure 3. Causes of death at age 0–4 years in India, by region, 2001-03.
MR=under-five mortality rate
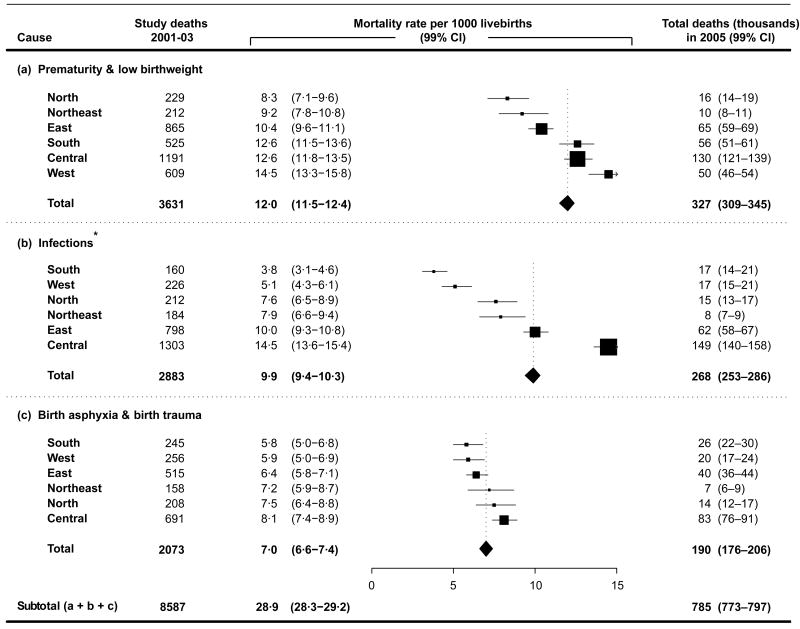
There was marked regional variation in the mortality rates for the three leading causes of death among neonates (figure 4). The mortality rate for prematurity & low birthweight was highest in the West (14.5) and lowest in the North (8.3). The mortality rate for neonatal infections in Central India (14.5) was nearly four times higher than in South India (3.8) and mortality rates for birth asphyxia and birth trauma was highest in Central India (8.1) and lowest in the South (5.8).
Figure 4. Mortality rates for the three leading causes of neonatal death in India, by region, 2005.
*Includes pneumonia, sepsis, and infections of the central nervous system.
Deaths at ages 1-59 months
Two causes accounted for 50% (0.67 M/1.34 M) of all deaths at ages 1-59 months: pneumonia (0.37 M deaths, 99%CI 0.35-0.39 M; MR = 13.5) and diarrhoeal diseases (0.30 M deaths, 99%CI 0.28-0.32 M; MR = 11.1). All-cause mortality rate at ages 1-59 months was about 36% higher among girls (56.7) than boys (41.7) and most of the leading causes of death were between 12% and 72% higher in girls than boys, with the exception of injuries and meningitis/encephalitis. Pneumonia and diarrhoeal diseases accounted for about two-thirds (0.10 M) of the 0.16 M excess deaths from all causes among girls at ages 1-59 months (table 1). Pneumonia and diarrhoeal diseases accounted for a greater proportion of deaths in the poorer states than in the richer states (figure 2), and their proportion of total child deaths declined as under-five mortality rates declined (figure 3).
There was marked regional variation in the mortality rates at ages 1-59 months for pneumonia and diarrhoeal diseases (figure 5). The mortality rate from pneumonia in Central India (18.0) was four times that in the South (4.7) and the mortality rate from diarrhoeal diseases in Central India (14.5) was three times that in the West (4.9). Differences were even more extreme when gender was taken into account. Girls in Central India had a five times higher mortality rate from pneumonia (20.9) compared to boys in South India (4.1) and had four times higher the diarrhoeal disease mortality rate (17.7) compared to boys in the West (4.1).
Discussion
Over three-fifths of all 2.3 M child deaths in India in 2005 were caused by five conditions: pneumonia, prematurity & low birthweight, diarrhoeal diseases, neonatal infections and birth asphyxia & birth trauma.
Each of the major causes of neonatal deaths can be prevented or treated with known, highly effective and widely practicable interventions such as improvements in prenatal care, intrapartum care (skilled attendance, emergency obstetric care and simple immediate newborn care), postnatal family-community care (preventive post-natal care, oral antibiotics management of pneumonia), 24 and tetanus toxoid immunization. 25 Concern has been raised that neonatal death rates in India are not falling at a fast pace. 10 However, our results suggest that almost half of India's neonatal deaths are caused by birth asphyxia & birth trauma, sepsis, pneumonia and tetanus – conditions that can be avoided by increases in delivery care and postnatal care. 26
The marked regional differences in cause-specific mortality, even among girls (webtable 4A-4C) must reflect the existence of some underlying social, behavioural or biological risk factors for child deaths which await further discovery. 11 However, at ages 1-59 months, girls in every region die more commonly than boys and inequities in access to care, not biologic or genetic factors, are a more plausible explanation of these observed gender differences. 7, 8 Household surveys 4, 27 reveal little gender differences in the incidence of respiratory symptoms and diarrhoeal disease, whereas our study and earlier analyses 28 showed marked gender differences in mortality. Integrated management of child illnesses increases care seeking for illnesses, 29 and reduces child deaths, 30 but in India boys use such programs more than girls. 10 Even though lower immunization rates have been observed among girls, 8 outreach vaccine programs can benefit girls more than boys as they rely less on parents taking children to clinics. Adding vaccines against pneumonia (Pneumococcal, Haemophilus influenzae type B) and diarrhoeal diseases to outreach home-based immunization programmes would reduce child deaths and also narrow the gender gap in child mortality India. 10, 31
Our study finds that boy preference likely affects girl child survival. The states with higher excess mortality rates among girls at ages 1-59 months were also those with higher rates of missing second girls as measured in a previous study by an index of selective abortion represented by female-to-male sex ratio for second births following a boy 12 (Pearson's correlation coefficient -0.47 p-value=0.0004 – data not shown). This suggests that lower use of health services by girls is seen in the same states where selective abortion of female fetuses is common. Moreover, a relative gap in mortality between girls and boys at ages 1-59 months is seen in urban areas, among more educated groups 12 and in states with lower mortality rates (webtable 4A-C). 4, 32 However, the excess of 0.15 M girl deaths at ages 1-59 months is largely offset by the excess of 0.13 M boy deaths among neonates. The most plausible explanation for the observed ‘missing’ total of 6 M girls in the 2001 Census 21 (which recorded 76 M girls and 82 M boys aged 0-6 years) likely remains selective abortion of female fetuses, 7 and less so the excess mortality in girls.
The main uncertainty in our estimates arises because verbal autopsy misclassifies some causes of death, 7, 16, 23 and our estimates relied mostly on family reports of deaths occurring in rural homes. Earlier studies comparing hospital based deaths to home-based verbal autopsy (which formed the basis for the field instrument used in the MDS) have found reasonable agreement for the symptoms used to assign the five major causes of death we report in the study. 16 Hospital deaths should not be considered a ‘gold standard’: there are likely important differences in the distribution of causes of child deaths, treatment patterns, and for infectious causes, in their underlying pathogens, 33 between hospital deaths (mostly in urban areas) and rural, unattended home deaths. Misclassification of causes can affect our estimates of the total number of deaths from each cause, 33 but misclassification is unlikely to be differential across gender, areas and regions, and would not likely influence our estimates of gender differences. The missing deaths or deaths which physicians were unable to code, while sizeable, are mostly random and unlikely to have affected the overall marked observed variation by gender and region. Similarly, there is also uncertainty in the UN total estimates of annual total child deaths (2.35 M deaths in 2005, ranging between 2.26 M to 2.46 M), 2 but such uncertainty would likely raise or lower the overall mortality rates, but would not materially affect the observed marked gender or regional variation in these mortality rates.
Results presented here correspond to deaths prior to the wide scale introduction of India's National Rural Health Mission in 2006. That programme reports increases in institutional deliveries 10 and in coverage of existing vaccines, and as such may have reduced child mortality in India. Our study further suggests that specific interventions might be priorities for different regions (for example, expanded case management and introduction of newer antigens into immunization would be particularly needed in Central India, especially for girls) The changes in the gender- and region-specific levels and causes of neonatal mortality and mortality at ages 1-59 months will continue to be monitored and reported by the RGI, 18 and should thus help evaluate the effectiveness of the National Rural Health Mission and other efforts to reduce child mortality in India.
Supplementary Material
Acknowledgments
The Registrar General of India established the SRS in 1971, has continued it ever since, and is collaborating with several of the authors on the ongoing MDS. External funding is from the Fogarty International Centre of the US National Institutes of Health (grant R01 TW05991–01), Canadian Institute of Health Research (CIHR; IEG-53506), International Development Research Centre (Grant 102172), Li Ka Shing Knowledge Institute and Keenan Research Centre at St Michael's Hospital, University of Toronto (CGHR support) and the US Fund for UNICEF (via a grant from the Bill & Melinda Gates Foundation for CHERG – Sub-grant 50140).
Prabhat Jha is supported by the Canada Research Chair programme. Shaun K. Morris is a Fellow of the Pediatric Scientist Development Program. The opinions expressed in this paper are those of the authors and do not necessarily represent those of the Government of India. We thank Joy Lawn for the inputs on the neonatal cause of death classification and categorization of ICD codes, and Colin Mathers, Mikkel Oestergaard and Prem Mony for comments on the neonatal and overall classification of causes of death and ICD codes. Alvin Zipursky for comments on the final manuscript, and Maya Kesler, Brendon Pezzack, Chinthanie Ramasundarahettige, Peter Rodriguez and Wilson Suraweera for data support.
Funding: US National Institutes of Health, International Development Research Centre, Canadian Institutes of Health Research, Li Ka Shing Knowledge Institute and the US Fund for UNICEF.
Footnotes
Million Death Study (MDS) collaborators
Writing committee: Diego G Bassani, Rajesh Kumar, Shally Awasthi, Shaun K Morris, Vinod K Paul, Anita Shet, Usha Ram, Michelle F Gaffey, Robert E Black (CHERG chair) and Prabhat Jha (Principal Investigator for the MDS).
India CHERG group: RK (chair), SA, DGB (facilitator), REB, PJ, Bhaskar Mishra, VKP, UR, Siddarth Ramji, AS and Mani Subramaniyam.
Contributors: RK, SA, DGB and PJ planned the child mortality study. The academic partners in India (MDS Collaborators; webappendix – p 13) planned the MDS in close collaboration with the Office of the Registrar General of India. DGB and PJ conducted the analyses. All authors were involved with data interpretation, critical revisions of the paper, and approved the final version; PJ is its guarantor.
Conflicts of interest: We declare that we have no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.UN Population Division. World Population Prospects (2008 revision) [June 14, 2010]; http://esa.un.org/peps/peps_interpolated-data.htm.
- 2.Rajaratnam JK, Marcus JR, Flaxman AD, Wang H, Levin-Rector A, Dwyer L, et al. Neonatal, postneonatal, childhood, and under-5 mortality for 187 countries, 1970-201: a systematic analysis of progress towards the Millenium Development Goal 4. Lancet. 2010;357:1988–2008. doi: 10.1016/S0140-6736(10)60703-9. [DOI] [PubMed] [Google Scholar]
- 3.UNICEF, WHO, Bank W UN Population Division. [September 13, 2010];Child Survival and Health - estimates developed by the Inter-agency Group for Child Mortality Estimation (IGME) http://www.childinfo.org/mortality.html.
- 4.International Institute for Population Sciences (IIPS) and Macro International. National Family Health Survey (NFHS-3), 2005-06: India. Mumbai: IIPS; 2008. [Google Scholar]
- 5.Registrar General of India. Sample Registration System. New Delhi, India: Office of the Registrar General of India; 2004. [Google Scholar]
- 6.Baqui AH, Darmstadt GL, Williams EK, Kumar V, Kiran TU, Panwar D, et al. Rates, timing and causes of neonatal deaths in rural India: implications for neonatal health programmes. Bull World Health Organ. 2006;84:706–13. doi: 10.2471/blt.05.026443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jha P, Gajalakshmi V, Gupta PC, Kumar R, Mony P, Dhingra N, et al. Prospective study of one million deaths in India: rationale, design, and validation results. PLoS Med. 2006;3:e18. doi: 10.1371/journal.pmed.0030018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Corsi DJ, Bassani DG, Kumar R, Awasthi S, Jotkar R, Kaur N, et al. Gender inequity and age-appropriate immunization coverage in India from 1992 to 2006. BMC Int Health Hum Rights. 2009;9(suppl 1):S3. doi: 10.1186/1472-698X-9-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–87. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 10.Jha P, Laxminarayan R. Choosing health: an entitlement for all Indians. [September 10, 2010]; http://cghrindia.org/images/choosing-health.pdf.
- 11.Jha P. Avoidable mortality in India: past progress and future prospects. Natl Med J India. 2002;15(suppl 1):32–6. [PubMed] [Google Scholar]
- 12.Jha P, Kumar R, Vasa P, Dhingra N, Thiruchelvam D, Moineddin R. Low female-to-male sex ratio of children born in India: national survey of 1.1 million households. Lancet. 2006;367:211–8. doi: 10.1016/S0140-6736(06)67930-0. [DOI] [PubMed] [Google Scholar]
- 13.Dhingra N, Jha P, Sharma VP, Cohen AA, Jotkar R, Rodrigues PS, et al. Adult and child malaria mortality in India: a retrospective observational study. Lancet. 2010;376 doi: 10.1016/S0140-6736(10)60831-8. forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jha P, Jacob B, Gajalakshmi V, Gupta PC, Dhingra N, Kumar R, et al. A nationally representative case-control study of smoking and death in India. N Engl J Med. 2008;358:1137–47. doi: 10.1056/NEJMsa0707719. [DOI] [PubMed] [Google Scholar]
- 15.Jha P, Kumar R, Khera A, Bhattacharya M, Arora P, Gajalakshmi V, et al. HIV mortality and infection in India: estimates from nationally representative mortality survey of 1.1 million homes. BMJ. 2010;340:c621. doi: 10.1136/bmj.c621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anker M, Black RE, Coldham C, Kalter HD, Quigley MA, Ross D, et al. A standard verbal autopsy method for investigating causes of death in infants and children. Geneva: World Health Organization; 1999. [Google Scholar]
- 17.Sinha D, Dikshit R, Kumar V, Gajalakshmi V, Dhingra N, Seth J. Technical document VII: Health care professional's manual for assigning causes of death based on RHIME household reports. Toronto, Canada: Centre for Global Health Research; University of Toronto; 2006. [Google Scholar]
- 18.Registrar General of India, Centre for Global Health Research. Causes of death in India, 2001-2003: Sample Registration System. New Delhi: Government of India; 2009. [Google Scholar]
- 19.Bhat MPN. Completeness of India's Sample Registration System: An assessment using the general growth balance method. Population Studies. 2002;56:119–134. doi: 10.1080/00324720215930. [DOI] [PubMed] [Google Scholar]
- 20.Saikia N, Jasilionis D, Ram F, Shkolnikov VM. Trends in geographical mortality differentials in India. [August 5, 2010]; doi: 10.1080/00324728.2010.534642. http://www.demogr.mpg.de/papers/working/wp-2009-013.pdf. [DOI] [PubMed]
- 21.Registrar General of India. Census of India 2001. New Delhi: Office of the Registrar General & Census Commissioner; 2001. [Google Scholar]
- 22.Wolter KM. Introduction to variance estimation. 2nd. New York: Springer; 2007. [Google Scholar]
- 23.Morris SK, Bassani DG, Kumar R, Awasthi S, Paul VK, Jha P. Factors associated with physician agreement on verbal autopsy of over 27000 childhood deaths in India. PLoS One. 2010;5:1–8. doi: 10.1371/journal.pone.0009583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, de Bernis L. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet. 2005;365:977–88. doi: 10.1016/S0140-6736(05)71088-6. [DOI] [PubMed] [Google Scholar]
- 25.Ronsmans C, Chowdhury ME, Alam N, Koblinsky M, El Arifeen S. Trends in stillbirths, early and late neonatal mortality in rural Bangladesh: the role of public health interventions. Paediatr Perinat Epidemiol. 2008;22:269–79. doi: 10.1111/j.1365-3016.2008.00939.x. [DOI] [PubMed] [Google Scholar]
- 26.Kumar V, Mohanty S, Kumar A, Misra RP, Santosham M, Awasthi S, et al. Effect of community-based behaviour change management on neonatal mortality in Shivgarh, Uttar Pradesh, India: a cluster-randomised controlled trial. Lancet. 2008;372:1151–62. doi: 10.1016/S0140-6736(08)61483-X. [DOI] [PubMed] [Google Scholar]
- 27.International Institute for Population Sciences (IIPS) District Level Household and Facility Survey (DLHS-3), 2007-08. Mumbai, India: IIPS; 2010. [Google Scholar]
- 28.Bassani DG, Jha P, Dhingra N, Kumar R. Child mortality from solid-fuel use in India: a nationally-representative case-control study. BMC Public Health. 2010;10:491–9. doi: 10.1186/1471-2458-10-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arifeen SE, Hoque DM, Akter T, Rahman M, Hoque ME, Begum K, et al. Effect of the Integrated Management of Childhood Illness strategy on childhood mortality and nutrition in a rural area in Bangladesh: a cluster randomised trial. Lancet. 2009;374:393–403. doi: 10.1016/S0140-6736(09)60828-X. [DOI] [PubMed] [Google Scholar]
- 30.Ali M, Asefaw T, Byass P, Beyene H, Pedersen FK. Helping northern Ethiopian communities reduce childhood mortality: population-based intervention trial. Bull World Health Organ. 2005;83:27–33. [PMC free article] [PubMed] [Google Scholar]
- 31.Zaman K, Dang DA, Victor JC, Shin S, Yunus M, Dallas MJ, et al. Efficacy of pentavalent rotavirus vaccine against severe rotavirus gastroenteritis in infants in developing countries in Asia: a randomised, double-blind, placebo-controlled trial. Lancet. 2010;376:615–23. doi: 10.1016/S0140-6736(10)60755-6. [DOI] [PubMed] [Google Scholar]
- 32.Registrar General of India. Special Fertility & Mortality Survey, 1988: A report of 1.1 million Indian households. New Delhi: Registrar General; 2005. Aug, [Google Scholar]
- 33.Maude GH, Ross DA. The effect of different sensitivity, specificity and cause-specific mortality fractions on the estimation of differences in cause-specific mortality rates in children from studies using verbal autopsies. Int J Epidemiol. 1997;26:1097–106. doi: 10.1093/ije/26.5.1097. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.