Abstract
Recent human clinical trials of the effects of (n-3) fatty acids on participants with type 2 diabetes (T2D) were reviewed, focusing on 11 clinical trials conducted within the past 4 y, and subsequent to a Cochrane Database meta-analysis of this topic. Doses of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) in these studies were mostly in the range of ∼2 g/d provided for 6 wk to 6 mo. Summarizing across these studies, there were no changes in fasting glucose or insulin compared with baseline or placebo. (n-3) Fatty acids generally decreased serum triglycerides but had varying effects on serum cholesterol, LDL cholesterol, and HDL cholesterol. A few studies indicated beneficial effects of (n-3) fatty acids on arterial blood flow. The effects of EPA and/or DHA have not yet been studied in clinical trials in participants at risk for T2D; the prevention or exacerbation of T2D by fish oil or EPA and DHA supplements of amounts >0.5 g/d deserves study. The prevention of adverse vascular effects of T2D by (n-3) fatty acids may be a promising direction for further study.
Introduction
Diabetes is a prevalent disease and a major risk factor for cardiovascular disease. There are 24 million children and adults in the United States, or 8% of the population, who have diabetes. Another 57 million people have prediabetic conditions (1). In 2007 the total economic cost of diabetes was estimated to be $174 billion, an increase of 32% since 2002 (1). Both physical activity and dietary intervention have been recommended to control and prevent diabetes. Epidemiologic evidence showed that populations with high intakes of fish had less risk of cardiovascular disease and diabetes, suggesting that (n-3) fatty acids may play a role in controlling and preventing diabetes. (n-3) Fatty acids are fundamental components of phospholipids in cell membranes. By altering the fatty acid composition of membrane phospholipids, (n-3) fatty acids modify membrane-mediated processes such as insulin transduction signals, activity of lipases, and synthesis of eicosanoids (2). (n-3) Fatty acids also control the expression of various metabolic genes (e.g. genes involved in lipid and glucose metabolism and adipogenesis) in part through the activation of PPAR (3). (n-3) Fatty acids include eicosapentaenoic acid (EPA) and docosahexaenoic (DHA) and their progenitor, α-linolenic acid (ALA)2. EPA and DHA are formed from linolenic acid by δ-6 desaturase/elongase and δ-5-desaturase and elongases. EPA and DHA are provided from marine sources and ALA is provided largely from plant sources such as canola and flaxseed. This review will summarize recent advances in clinical trials of (n-3) fatty acids in type 2 diabetes (T2D).
T2D is the disease most strongly associated with obesity (4) and arises from insulin resistance rather than the lack of insulin production that causes type 1 diabetes. Insulin resistance causes cells to take up glucose less efficiently, resulting in elevated blood glucose concentrations. Increased hepatic gluconeogenesis also results from insulin resistance, which further elevates blood glucose overnight. Increased chronic blood glucose causes glucose-protein adducts, which are instrumental in circulatory dysfunction, leading to retinopathy, kidney damage, and inability to fight infections that may result in gangrene in the limbs, requiring amputation. Hemoglobin A1c (HbA1c) is an indicator of the extent of glucose adducts and therefore of long-term elevated blood glucose. HbA1c and fasting glucose are the most common indicators of the ability of a treatment or regimen to lessen T2D.
Current state of knowledge
Recent reviews and meta-analyses
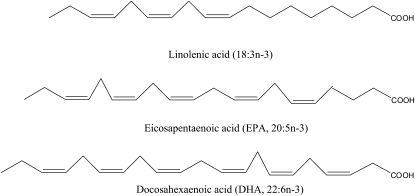
(n-3) Fatty acid (Fig. 1) effects on diabetes and insulin action and cardiovascular disease have been reviewed previously, most recently with a Cochrane database meta-analysis (5) that involved 23 randomized controlled trials (1075 participants) studying the effects of (n-3) PUFA supplementation on cardiovascular outcomes, cholesterol levels, and glycemic control in people with T2D. All randomized controlled trials in which (n-3) PUFA supplementation or dietary intake was randomly allocated and unconfounded in people with T2D were searched from 1966 to September 2006. The primary outcomes were fatal myocardial infarction or sudden cardiac death, proven nonfatal myocardial infarction, and coronary or peripheral revascularization procedures. The secondary outcomes were triglycerides, total cholesterol, HDL cholesterol, LDL cholesterol, VLDL cholesterol, HbA1c, fasting glucose, fasting insulin, body weight, and adverse effects. Twelve parallel group designs and 11 crossover trials with sample size ranging from 8 to 418 were selected to analyze. The majority of participants were male and the ages ranged between 21 and 85 y. The mean treatment duration was 8.9 wk. The mean dose of (n-3) PUFA used in the trials was 3.5 g/d. No trials with vascular events or mortality endpoints were identified. Among those taking (n-3) fatty acids, triglyceride levels were significantly lowered by 0.45 mmol/L and VLDL cholesterol lowered by 0.07 mmol/L. LDL cholesterol levels were raised by 0.11 mmol/L. No significant change in total cholesterol, HDL cholesterol, HbA1c, fasting plasma glucose, fasting insulin, or body weight was observed. No adverse effects of the intervention were reported. Hartweg et al. (5) also investigated the effect of the length of intervention, dose of (n-3) fatty acids, and the baseline triglyceride level on triglycerides and LDL and VLDL cholesterol levels. Triglycerides and VLDL cholesterol levels were reduced to a greater extent in longer trials by the difference of 0.22 and 0.56 mmol/L compared with shorter trials (<2 mo) for these 2 types of blood lipids, respectively. The mean difference of triglycerides was −0.35 mmol/L in high-dose trials (>2 g/d) and −0.57 mmol/L in low-dose trials. Triglycerides and VLDL cholesterol were also reduced to a greater extent in hypertriglyceridemic participants than in nonhypertriglyceridemic participants by 5-and 9-fold, respectively. Effects of (n-3) fatty acids on LDL cholesterol were nonsignificant in subgroup analyses.
Figure 1.
Structures of major (n-3) fatty acids in human diets.
Caterina et al. (6) reviewed clinical studies of the effect of (n-3) fatty acids on the treatment of people with both type 1 and 2 diabetes that had been performed up to November 2006. Twenty-eight people with T2D in 2 noncontrolled studies and 671 patients in 13 double-blinded studies were provided low-dose (≤3 g/d) (n-3) fatty acids for 2–24 wk. No effect was found on HbA1c and fasting plasma glucose in most cases. Triglycerides were decreased in most cases. Total cholesterol was decreased in 6 cases and increased in only 1 case. HDL cholesterol increased in 4 cases and decreased in 1 case. LDL cholesterol increased in 5 cases and decreased in 4 cases. A total of 112 type 2 people with diabetes patients participated in 7 high-dose (>3 g/d) studies (4 double-blinded, 1 single-blind, and 2 noncontrolled studies) for 3–24 wk. Fasting plasma glucose decreased in 3 studies and was not modified in 4 studies. HbA1c and total cholesterol were not modified by (n-3) fatty acid treatment. Plasma triglycerides decreased in 6 cases and LDL cholesterol increased in 6 cases. HDL cholesterol increased in 2 cases and decreased in 1 case.
An earlier meta-analysis (7) showed that in people with types 1 and 2 diabetes supplied with (n-3) fatty acids, triglycerides were decreased. LDL cholesterol increased in people with T2D. Fasting plasma glucose and HbA1c were not modified in people with both types of diabetes. In summary, current evidence with low numbers of participants studied for short periods of time showed that dietary (n-3) fatty acids are effective in reducing plasma triglycerides, one risk factor for adverse outcomes associated with obesity and metabolic syndrome. Clinical trials of (n-3) fatty acids in people with prediabetes and clinical trials examining the ability of (n-3) fatty acids to reduce blood pressure, leukocyte reactivity, and arrhythmias remain to be conducted. Further trials with hard end points, such as death, myocardial infarction, and stroke in people with T2D given (n-3) fatty acids also remain to be performed. Doses of (n-3) fatty acids for such trials also remain to be optimized.
Dietary fat quality and insulin resistance
Galgani et al. (8) reviewed the effect of dietary fat quality (types of dietary fats and dietary fatty acid composition) on insulin sensitivity. Randomized clinical trials in human participants published in PubMed until August 31, 2007 and their related articles available in Medline as well as bibliographies of primary references were used to identify relevant studies. Forty-one articles on controlled and intervention studies assessing the role of dietary fat quality on glucose metabolism were found. Dietary fatty acid quality was found to have no effect on insulin sensitivity in general. Further selection for high-quality studies was performed based on more strict criteria, such as insulin resistance being evaluated with euglycemic-hyperinsulinemic clamp, insulin suppression test, or frequently sampled intravascular glucose tolerance test; diets with similar energy and macronutrient content supplied according to a random, crossover/parallel design; and dietary compliance at least fairly well controlled. Fifteen studies (9 on healthy participants and 6 on participants with T2D) matched the proposed quality criteria. Among the 9 studies on healthy participants, only 3 of them studied the effect of (n-3) fatty acids on insulin sensitivity. (n-3) Fatty acid dose ranged from 2.4 to 3.4g/d. No changes in insulin sensitivity were observed. Of the 5 studies on people with T2D (n-3) fatty acid dose from 1.8 to 5g/d), 4 studies found no changes in insulin sensitivity and 1 (9) found (n-3) fatty acids (5 g/d EPA+DHA) lowered insulin sensitivity compared with corn oil.
Impaired insulin sensitivity is a hallmark of T2D; hence, strategies to prevent this impairment are crucial to reduce the population afflicted with T2D. Human studies have not demonstrated a consistent effect of dietary fat quality on insulin sensitivity, particularly the (n-3):(n-6) fatty acid ratio (8).
In human participants, the maximal fish oil dose studied did not exceed 20 g/d (∼7.5% of energy) and Western diets tend to contain large amounts of (n-6) fatty acids. Therefore, the potential protective effect of (n-3) fatty acids on insulin sensitivity in humans participants might require higher fish oil doses associated with lower (n-6) fatty acid dietary contents. In addition, the effect of (n-3) fatty acids on insulin sensitivity is difficult to test, because it is difficult to find a good marker for insulin sensitivity. Galgani et al. (8) suggested that surrogate measurements of insulin sensitivity (measuring fasting blood glucose and insulin) are not recommended, because they explain no more than 40% of the insulin sensitivity variance observed in a population and 13% of the insulin sensitivity variance in normal-weight participants. Reference methods such as the euglycemic-hyperinsulinemic clamp, insulin suppression test, and the frequently sampled i.v. glucose tolerance test are considered reliable approaches to determine the degree of insulin sensitivity and are much more challenging and expensive to perform, especially with the large numbers of participants required for meaningful dietary intervention studies. In addition, people with T2D need greater insulin doses to achieve fully suppressed hepatic glucose production. The time of intervention may also be important to the insulin response. Most of the human studies were <10 wk long, but the evidence from epidemiologic studies is based on a habitual fish diet consumed for years.
Another randomized crossover study on 11 men with T2D (age, 54.6 y; BMI, 33.2 kg/m2; fasting plasma glucose, <200 mg/dL; not receiving insulin therapy) was performed to evaluate the effect of fatty acids on postprandial insulin, glucose, and triglyceride responses (10). All participants received an isoenergetic diet (1000 kcal) of constant composition (15% of total energy as protein, 35% as fat, and 50% as carbohydrate). At intervals of 3–4 d, after an overnight fast, each participant consumed a mixed test meal rich in palmitic acid, oleic acid, linoleic acid, or EPA and DHA on 4 occasions in a randomized manner. The participants were also instructed to maintain a constant level of physical activity. The postprandial insulin response was lower to meals rich in oleic acid or EPA and DHA than to meals rich in palmitic acid or linoleic acid (P < 0.01). The triglyceride response did not reach significance but tended to be lower with EPA and DHA than with the other fatty acids. Similar trends were seen for area under the curve and incremental area under the curve for serum insulin and triglycerides. This study indicated that meals containing a high percentage of energy from oleic acid or EPA and DHA may be beneficial in lowering the postprandial insulin response compared with meals rich in palmitic acid or linoleic acid with a comparable postprandial glucose response. Meals containing a high percentage of energy from EPA and DHA also may be beneficial in lowering the postprandial triglyceride response.
Waite et al. (11) examined 5 healthy participants with BMI ≥ 25 kg/m2, waist circumference > 37 inches for men and > 31 inches for women who were not ingesting fish oil supplements and consumed <2 portions oily fish/wk to determine the effects of 60 d of fish oil supplementation (440 mg DHA and 660 mg EPA/d) on insulin sensitivity, plasma glucose, and insulin levels as assessed by an oral glucose tolerance test, total serum cholesterol levels, and serum triglyceride levels in a single-blind intervention study. There was a significant decrease in diastolic blood pressure following supplementation but no other significant changes in anthropometric measurements. However, the small sample size, screening method, original glucose tolerance, and insulin sensitivity of the participants and the lack of a control group reduced the strength of these findings.
Barre et al. (12) evaluated the effect of a high dose of flaxseed oil (containing ALA) on the serum glucose and insulin responses in T2D. Forty patients (age 60, BMI 30–32 kg/m2) entered the study and were randomly assigned to take flaxseed oil (60 mg/(kg BW−1 ⋅ d−1), 5.4 g/d) and safflower oil capsules for 3 mo. Eighteen patients given flaxseed oil and 14 patients given safflower oil finished the study. Administration of flaxseed oil and safflower oil did not change fasting serum glucose, insulin, or HbA1c levels, although these parameters tended to be higher in flaxseed oil-treated individuals but did not reach significance. Therefore, consumption of a high dosage of flaxseed oil did affect glycemic control in patients with T2D.
Recent studies of (n-3) fatty acids, plasma lipids, and other health indicators in participants with T2D
There have been several studies about the effects of (n-3) fatty acids on diabetes and obesity in the past 4 y (Table 1). Garg et al. (13) studied the effect of (n-3) fatty acid-enriched dip on the plasma lipid profiles of participants with T2D. Thirteen participants with T2D (mean BMI 28 kg/m2) were provided 100 g of the dip [1.2–1.3 g/d (n-3) fatty acids] daily for 6 wk. Body weight and BMI were kept constant and nutrient intakes remained unchanged during the 6 wk. After the 6-wk dietary intervention, compared with preintervention, triglycerides significantly decreased ∼0.25 mmol/L and LDL and HDL cholesterols significantly increased ∼0.26 and 0.06 mmol/L, respectively. All the long-chain (n-3) fatty acids [20:5(n-3), 22:5(n-3), and 22:6(n-3)] were significantly elevated in the plasma lipids. These results were consistent with the reviews above. A randomized controlled, double-blind, parallel study involving 26 women with T2D (mean age 55 y and BMI 30 kg/m2) without hypertriglyceridemia was performed to evaluate the effect of (n-3) fatty acids on adiposity, insulin sensitivity, adipose tissue function, and gene expression (14). Fourteen and 12 women, respectively, were provided either placebo (paraffin oil) or 3 g/d fish oil [1.8 g (n-3) fatty acids: 1.08 EPA and 0.72 DHA] for 2 mo. Each participant received individual counseling on diet and was asked to follow her usual diet recommendation more strictly with consumption of 55% of energy intake as carbohydrates, 15% as protein, and 30% as lipids. A 7-d food diary was used to assess food intake. After 2 mo, the concentrations of (n-3) fatty acids in plasma phospholipids significantly increased in the fish oil treatment, but the placebo group was not changed. Compared with the placebo group, the fish oil-treated women had less fat mass and a lower subcutaneous adipocyte diameter. However, the insulin sensitivity measured by euglycemic-hyperinsulinemic clamp did not significantly differ between the 2 groups. Plasma triglycerides, the ratio of total cholesterol:HDL cholesterol, and plasma plasminogen activator inhibitor-1 were lower in the fish oil group than in the placebo group. (n-3) Fatty acids also decreased the expression of some inflammation-related genes such as MMP9, CTSS, CD68, PLAUR (plasminogen activator/urokinase receptor), CD11b, and CD18 in adipose tissue. This indicated that (n-3) fatty acids could reduce adiposity and atherogenic markers without deterioration of insulin sensitivity in participants with T2D, which could benefit cardiovascular disease risk factors.
Table 1.
Recent human clinical trials of effects of (n-3) fatty acids in participants with T2D
| Type, dose, and source of (n-3) fatty acid | Timeframe | Participant characteristics | Endpoints, major findings | Reference |
| Fish oil, 5.9 g | 9 wk | 13 male, 14 female, 40–75 y, BMI (in kg/m2) 29–30 (14 participants took corn oil, 13 took fish oil) | Decreased insulin sensitivity and smaller VLDL particle size compared with controls | (9) |
| Salmon oil, 6 g (n-3) fatty acids | Single meal | 11 men | Decreased postprandial insulin response compared with palm or safflower oil | (10) |
| Fish oil, 440 mg DHA/660 mg EPA | 60 d | 5 participants, BMI ≥ 25 | No effect on insulin response, blood glucose | (11) |
| Flaxseed oil, 5 g ALA | 3 mo | 18 participants, mean age 60 y, BMI 30–32 | No effect on fasting glucose, insulin, or HbA1c compared with safflower oil (14 controls) | (12) |
| 540 mg EPA + 600 mg DHA in dip | 6 wk | 13 participants | Increased LDL and HDL cholesterol, decreased triglycerides, no effect on fasting glucose or HbA1c compared with baseline | (13) |
| 3 g fish oil | 2 mo | 26 women, mean age 55 y, BMI 30; 12 given fish oil and 14 given paraffin oil | Decreased triglycerides and total:HDL cholesterol ratio, no change in insulin sensitivity compared with controls | (14) |
| 930 mg EPA, 750 mg DHA | 12 wk | 30 participants, mean age 55 y, BMI 31 | Decreased triglycerides and C-reactive protein, increased HDL cholesterol, no change in fasting insulin or glucose | (15) |
| 920 mg EPA + 760 mg DHA | 4 mo | 732 participants, mean age 64 y, BMI 31, randomized to (n-3) fatty acids with or without atorvastatin | Decreased triglycerides and no effect on HbA1c or cardiovascular disease risk compared with placebo and regardless of atorvastatin treatment | (16) |
| 1800 mg EPA | 6 mo | 76 participants, mean age 66 y, BMI 27 | Decreased total and LDL cholesterol, triglycerides, angiopoeitin-2, and endothelial cell-derived microparticles with procoagulant activity, increased adiponectin | (17) |
| 2000 mg EPA + DHA (∼1:1) | 12 wk | Offspring of participants with T2D (mean age 31 y, BMI 26); 26 [(n-3) fatty acid treated] vs. 24 placebo controls | Decreased triglycerides, decreased tumor necrosis factor-α, increased flow-mediated dilation of brachial artery compared with controls | (18) |
| 920 mg EPA, 760 mg DHA | 6 wk | 34 participants, mean age 57 y, BMI 31, randomized to (n-3) fatty acids or placebo | Increased postprandial flow-mediated dilation of brachial artery compared with controls | (19) |
Mostad et al. (9) measured the effects of fish oil supplements on lipoprotein subclasses by NMR in participants with T2D and related them to insulin sensitivity. Twenty-seven normotriglyceridemic participants (13 male, 14 female participants, 40–75 y old, BMI 29–30 kg/m2) with T2D who did not receive insulin treatment were given either fish oil [5.9 g/d total (n-3) fatty acids; 1.8 g 20:5(n-3) and 3.0 g 22:6(n-3)] or corn oil [8.5 g/d 18:2(n-6) fatty acids] for 9 wk. Fourteen participants (6 men, 8 women) were randomly assigned to receive corn oil and 13 (7 men, 6 women) to receive fish oil. After 9 wk, compared with those receiving the corn oil, participants receiving the fish oil tended to have increased HDL size and LDL concentrations, but there was no effect on oxidized LDL. A high intake of (n-3) fatty acids exerted effects on several lipoprotein subclasses independent of decreased insulin sensitivity.
De Luis et al. (15) studied the responses of 30 people with T2D (mean age 55 y, BMI 31 kg/m2) to 930 mg EPA and 750 mg DHA given for 12 wk. Compared with baseline, participants had lower triglycerides and C-reactive protein and increased HDL cholesterol, with no changes in fasting insulin, glucose, or HbA1c.
Cardiovascular disease risk factors were assessed in 732 participants with T2D randomly assigned to atorvastatin with or without (n-3) fatty acids (2 g/d containing 920 mg EPA and 760 mg DHA) or placebo. The (n-3) fatty acid treatment decreased serum triglycerides regardless of whether participants also took atorvastatin or placebo [n = 371 taking (n-3) fatty acids vs. n = 361 not ingesting (n-3) fatty acids] and did not influence HbA1c or overall cardiovascular disease risk (16).
In 76 participants withT2D, 1800 mg EPA/d given for 6 mo decreased serum total and LDL cholesterol, triglycerides, angiopoeitin-2, and endothelial cell-derived microparticles with procoagulant activity and increased adiponectin compared with baseline (17).
In offspring of participants with T2D (n = 26, mean age 31 y, BMI 26 kg/m2) given 2 g EPA + DHA (∼1:1 ratio) for 12 wk, flow-mediated dilation of the brachial artery was improved in association with decreased tumor necrosis factor-α; triglycerides were also decreased compared with similar participants given olive oil placebo (18). In 34 participants with T2D (n = 34, mean age 57 y, BMI 31 kg/m2) randomized to 920 mg EPA + 760 mg DHA/d treatment for 6 wk, postprandial flow-mediated dilation of the brachial artery significantly improved compared with placebo-treated controls (19).
These data together indicate benefits of (n-3) fatty acids for blood triglycerides in people with T2D, varied results for other serum lipids, and no suggestion of benefits for blood glucose or HbA1c. Improved arterial blood flow and decreased blood coagulation responses in single studies suggest reason for further investigation regarding the abilities of (n-3) fatty acids to improve some adverse effects in people with T2D.
In summary, (n-3) fatty acids have been proven to improve plasma triglycerides in human clinical studies of people with T2D. (n-3) Fatty acids have not been shown to help restore insulin activity in humans. The (n-3) fatty acid dosage used in human clinical trials is generally relatively low [<3 g (n-3) fatty acids/d] and background diets have not been controlled or studied in such trials. Both of these factors may be considerable limitations in this field to date. The lack of and difficulty in performing high-quality studies on insulin sensitivity may be a barrier to progress in this field. ALA, a cheaper plant source of (n-3) fatty acids, is not well studied. Therefore, long-term, high-quality studies on (n-3) fatty acids, not only on marine sources but also on plant sources, need to be performed to answer the basic question of whether (n-3) fatty acids have beneficial effects on glycemic control in people with T2D. The prevention of T2D with intakes of (n-3) fatty acids of >0.5 g/d remains an unstudied aspect of this topic that deserves examination, but prevention studies will be quite expensive. It might be interesting and feasible to establish a database of volunteers who are currently consuming fish oil supplements to facilitate tracking their health status and serum chemistry over time.
Footnotes
Author disclosure: S. Hendrich, no conflicts of interest.
Abbreviations used: ALA, α-linolenic acid; DHA, docosahexaenoic acid; EPA, eicosapentaenoic acid; HbA1c, hemoglobin A1c; T2D, type 2 diabetes.
Literature Cited
- 1.CDC National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2007 [Internet]. Atlanta: U.S. Department of Health and Human Services, CDC; 2008. [cited 2010 Mar 12]. Available from: http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2007.pdf [Google Scholar]
- 2.Storlien LH, Hulbert AJ, Else PL. Polyunsaturated fatty acids, membrane function and metabolic diseases such as diabetes and obesity. Curr Opin Clin Nutr Metab Care. 1998;1:559–63 [DOI] [PubMed] [Google Scholar]
- 3.Jump DB, Botolin D, Wang Y, Xu J, Demeure O, Christian B. Docosahexaenoic acid (DHA) and hepatic gene transcription. Chem Phys Lipids. 2008;153:3–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Food and Nutrition Board Energy. In: Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids (macronutrients). Washington, DC: National Academies Press; 2005. p. 225–9 [Google Scholar]
- 5.Hartweg J, Perera R, Montori V, Dinneen S, Neil HA, Farmer A. Omega-3 polyunsaturated fatty acids (PUFA) for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2008:CD003205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Caterina R, Madonna R, Bertolotto A, Schmidt EB. N-3 fatty acids in the treatment of diabetic patients. Biological rationale and clinical data. Diabetes Care. 2007;30:1012–26 [DOI] [PubMed] [Google Scholar]
- 7.Friedberg CE, Janssen MJ, Heine RJ, Grobbee DE. Fish oil and glycemic control in diabetes: a meta-analysis. Diabetes Care. 1998;21:494–500 [DOI] [PubMed] [Google Scholar]
- 8.Galgani JE, Uauy RD, Aguirre CA. Dỉaz EO. Effect of the dietary fat quality on insulin sensitivity. Br J Nutr. 2008;100:471–9 [DOI] [PubMed] [Google Scholar]
- 9.Mostad IL, Bjerve KS, Lydersen S, Grill V. Effects of marine n-3 fatty acid supplementation on lipoprotein subclasses measured by nuclear magnetic resonance in subjects with type II diabetes. Eur J Clin Nutr. 2008;62:419–29 [DOI] [PubMed] [Google Scholar]
- 10.Shah M, Adams-Huet B, Brinkley L, Grundy SM, Garg A. Lipid, glycemic, and insulin responses to meals rich in saturated, cis-monounsaturated, and polyunsaturated (n-3 and n-6) fatty acids in subjects with type 2 diabetes. Diabetes Care. 2007;30:2993–8 [DOI] [PubMed] [Google Scholar]
- 11.Waite N, Lodge J, Hart K, Robertson D, Badley E, Burton S. The impact of fish-oil supplements on insulin sensitivity. J Hum Nutr Diet. 2008;21:402–3 [Google Scholar]
- 12.Barre DE, Mizier-Barre KA, Griscti O, Hafez K. High dose flaxseed oil supplementation may affect fasting blood serum glucose management in human type 2 diabetics. J Oleo Sci. 2008;57:269–73 [DOI] [PubMed] [Google Scholar]
- 13.Garg ML, Blake RJ, Clayton E, Munro IA, MacDonald-Wicks L, Singh H, Moughan PG. Consumption of an n-3 polyunsaturated fatty acid-enriched dip modulates plasma lipid profile in subjects with diabetes type II. Eur J Clin Nutr. 2007;61:1312–7 [DOI] [PubMed] [Google Scholar]
- 14.Kabir M, Skurnik G, Naour N, Pechtner V, Meugnier E, Rome S, Quignard-Boulangé A, Vidal H, Slama G, et al. Treatment for 2 mo with n-3 polyunsaturated fatty acids reduces adiposity and some atherogenic factors but does not improve insulin sensitivity in women with type 2 diabetes: a randomized controlled study. Am J Clin Nutr. 2007;86:1670–9 [DOI] [PubMed] [Google Scholar]
- 15.De Luis DA, Conde R, Aller R, Izaola O, González Sagrado M, Perez Castrillón JL, Dueñas A, Romero E. Effect of omega-3 fatty acids on cardiovascular risk factors in patients with type 2 diabetes mellitus and hypertriglyceridemia: an open study. Eur Rev Med Pharmacol Sci. 2009;13:51–5 [PubMed] [Google Scholar]
- 16.Holman RR, Paul S, Farmer A, Tucker L, Stratton IM, Neil HA. Atorvastatin in Factorial with Omega-3 EE90 Risk Reduction in Diabetes Study Group. Atorvastatin in Factorial with Omega-3 EE90 Risk Reduction in Diabetes (AFORRD): a randomised controlled trial. Diabetologia. 2009;52:50–9 [DOI] [PubMed] [Google Scholar]
- 17.Nomura S, Shouzu A, Omoto S, Inami N, Ueba T, Urase F, Maeda Y. Effects of eicosapentaenoic acid on endothelial cell-derived microparticles, angiopoietins and adiponectin in patients with type 2 diabetes. J Atheroscler Thromb. 2009;16:83–90 [DOI] [PubMed] [Google Scholar]
- 18.Rizza S, Tesauro M, Cardillo C, Galli A, Iantorno M, Gigli F, Sbraccia P, Federici M, Quon MJ, et al. Fish oil supplementation improves endothelial function in normoglycemic offspring of patients with type 2 diabetes. Atherosclerosis. 2009;206:569–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stirban A, Nandrean S, Götting C, Tamler R, Pop A, Negrean M, Gawlowski T, Stratmann B, Tschoepe D. Effects of n-3 fatty acids on macro- and microvascular function in subjects with type 2 diabetes mellitus. Am J Clin Nutr. 2010;91:808–13 [DOI] [PubMed] [Google Scholar]