Abstract
This paper describes the disparities in the U.S. childhood obesity epidemic, mainly based on recent nationally representative data. The prevalence of overweight and obesity has increased since the late 1970s; the over time shifts (changes) in distributions of various body fatness measures indicate that U.S. children have become fatter and the obese groups gained more body fat, especially more central obesity, as indicated by waist circumference. However, considerable between-group and regional disparities exist in the prevalence, fatness measures, and over time trends. The disparities and trends are complex, which reflects the complexity and dynamics in obesity etiology. Clearly, some population groups are affected more seriously than others. Native American children have the highest prevalence of obesity, whereas Asians have the lowest rate among all ethnic groups. Preschool age children have a lower obesity prevalence than older children. Young people in some states and cities are twice more likely to be overweight or obese than those living in other regions. Low-socioeconomic status is associated with obesity only among some population groups, e.g. white children and adolescents. Vigorous, effective interventions are needed to promote healthy lifestyles among U.S. young people and to reduce disparities in obesity.
Introduction
Obesity is a good indicator of unhealthy lifestyles, characterized by overeating and lack of physical activity. Obesity has become a serious public health problem in the United States and many parts of the world (1–3). There are large disparities in obesity between sociodemographic groups (1, 4). The Healthy People 2010 Program in the U.S. sets the goals of reducing obesity prevalence to 5% in children (5), which is unlikely to be met. Obesity in childhood often follows into adulthood (6), which further supports the importance of preventing childhood obesity. Some research also suggests that some minority groups (e.g. African Americans) are more likely to remain obese over time (7). Some recent data indicate a possible leveling off in the obesity prevalence increase (8, 9), but one may suspect that this is inconclusive before more data become available (1, 9, 10). The U.S. obesity epidemic can have many serious health and financial consequences if it cannot be controlled, and likely minority and low-income groups are hit harder (11).
This paper was built on recent research, including our work, on related topics of the childhood obesity epidemic in the U.S. We focused on the between-group disparities and related trends in obesity, including prevalence and over time changes (or called shifts), in the distribution of various body fatness measures. We summarized the age, sex, ethnic, socioeconomic status (SES),3 and geographic disparities. A good understanding of the disparities in childhood obesity in the U.S. can have many important implications, including gaining a better understanding of the etiology and better guiding future intervention efforts.
We focused on findings from 2 nationally representative surveys conducted by the CDC, the NHANES, and the Youth Risk Behavior Surveillance System (YRBSS), but we also included some key findings from other nationwide studies (1). NHANES comprises a series of cross-sectional examination surveys conducted since the 1970s, including NHANES I (1971–74), II (1976–1980), and III (1988–94), which became continuous since 1999. Rich data on Americans’ health and related lifestyle behaviors such as diet and physical activity have been collected. Weight, height, waist circumference (WC), and triceps skinfold thickness (TST) were measured by direct physical examination (12, 13). The 2007–08 data were made available most recently. Often, these recent data collected since 1999 were pooled in analyses to give adequate sample sizes and more reliable estimates. (2) YRBSS, initiated in 1991, monitors priority health risk behaviors among U.S. high school students (~15–18 y old), including self-reported weight and height, which may suffer from reporting errors and bias and underestimate obesity prevalence (10). Different from NHANES, YRBSS data allow for analysis at state and city levels, e.g. to show regional differences.
In most cases, we presented overweight as BMI ≥ 85th percentile, and obesity as BMI ≥ 95th percentile, based on the 2000 CDC Growth Chart (14). To reduce paper length, our results were often reported only for adolescents (12–19 y), while in many cases, those for younger children (<12) are similar. We termed non-Hispanic (NH) whites ‘whites’ and NH blacks ‘blacks.’
Current status of knowledge
Overview
Studies conducted by the CDC and, in particular, some of our recent in-depth analysis have provided good evidence on the sociodemographic disparities in obesity prevalence, adiposity distribution shifts, and trends, including SES-obesity associations across population groups and changes in those associations across time in the U.S. (1, 4, 13, 15–21). The sex, age, ethnic, and SES disparities in obesity and overweight prevalence are complicated and have changed over time. It is more complicated than the widely held perception that low-SES and minority groups had a high prevalence of obesity. Some of the disparities (e.g. by sex) have become greater, whereas some (e.g. by SES) seemed become smaller over the past decade.
The over time shifts in various adiposity measures such as BMI, WC, and TST reveal many more important insights on the patterns than solely examining the prevalence based on BMI percentiles. For instance, U.S. children and adolescents have become more centrally obese (e.g. gained more WC than BMI), in particular, the heavy groups. Adjusted adiposity shifts over time varied significantly across sex-age-ethnicity groups. Adolescents and some minority groups had greater increases in fatness than their counterparts. Some of those patterns observed among U.S. children and adolescents differed from those in U.S. adults (1, 4, 15, 16, 20).
Age and sex disparities in prevalence in recent years
Table 1 shows the age, sex, and ethnic disparities in recent prevalence of obesity and overweight among U.S. children and adolescents based on NHANES 2003–06 and 2007–08 data. In general, sex differences in the rates were small, which were very different from those in U.S. adults (1). In young people, there were considerable age differences; preschool age (2–5 y old) children had a lower prevalence than their older counterparts by ~10 percentage points (Fig. 1). The prevalence among school age children (6–11 y old) and adolescents (12–19 y old) was similar.
Table 1.
Age, sex, and ethnic disparities in recent prevalence of obesity and overweight among U.S. children and adolescents: NHANES 2003–06 to 2007–2008
| Prevalence (2003–06) |
Prevalence (2007–08) |
Change 2003–06 to 2007–08,1percentage point | |||||
| Sex | Ethnicity | % | SE | % | SE | ||
| Children, 6–11 y | |||||||
| Obesity (BMI ≥ 95th percentile)† | Boys and girls | All | 17.0 | 1.3 | 19.6 | 1.3 | 2.6 |
| Boys | All | 18.0 | 1.7 | 21.2 | 1.7 | 3.2 | |
| Girls | All | 15.8 | 1.4 | 18.0 | 2.2 | 2.2 | |
| Boys | NH white | 15.5 | 2.8 | 20.5 | 2.8 | 5.0 | |
| NH black | 18.6 | 2.6 | 17.7 | 3.8 | −0.9 | ||
| Mexican-American | 27.5 | 2.1 | 27.1 | 4.2 | −0.4 | ||
| Girls | NH white | 14.4 | 2.1 | 17.4 | 3.6 | 3.0 | |
| NH black | 24.0 | 2.0 | 21.1 | 5.1 | −2.9 | ||
| Mexican-American | 19.7 | 2.6 | 22.3 | 3.6 | 2.6 | ||
| Boys and girls | All | 33.3 | 2.0 | 35.5 | 1.6 | 2.2 | |
| Overweight (BMI ≥ 85th percentile)† | Boys | All | 33.9 | 2.2 | 35.9 | 2.9 | 2.0 |
| Girls | All | 32.6 | 2.4 | 35.2 | 2.9 | 2.6 | |
| Boys | NH white | 31.7 | 3.6 | 34.6 | 4.4 | 2.9 | |
| NH black | 33.8 | 3.6 | 36.4 | 3.9 | 2.6 | ||
| Mexican-American | 47.1 | 2.5 | 44.0 | 4.4 | −3.1 | ||
| Girls | NH white | 31.5 | 3.6 | 34.3 | 4.9 | 2.8 | |
| NH black | 40.1 | 2.3 | 38.9 | 4.8 | −1.2 | ||
| Mexican-American | 38.1 | 3.3 | 39.3 | 5.2 | 1.2 | ||
| Adolescents, 12–19 y | Boys and girls | All | 17.6 | 1.2 | 18.1 | 1.8 | 0.5 |
| Obesity (BMI ≥ 95th percentile)† | Boys | All | 18.2 | 1.5 | 19.3 | 2.4 | 1.1 |
| Girls | All | 16.8 | 1.5 | 16.8 | 2.1 | 0.0 | |
| Boys | NH white | 17.3 | 2.0 | 16.7 | 3.1 | −0.6 | |
| NH black | 18.5 | 1.3 | 19.8 | 3.0 | 1.3 | ||
| Mexican-American | 22.1 | 2.2 | 26.8 | 3.7 | 4.7 | ||
| Girls | NH white | 14.5 | 2.0 | 14.5 | 3.4 | 0.0 | |
| NH black | 27.7 | 1.9 | 29.2 | 3.1 | 1.5 | ||
| Mexican-American | 19.9 | 1.4 | 17.4 | 4.6 | −2.5 | ||
| Overweight (BMI ≥ 85th percentile)† | Boys and girls | All | 34.1 | 1.5 | 34.2 | 1.9 | 0.1 |
| Boys | All | 34.9 | 1.9 | 35.0 | 2.5 | 0.1 | |
| Girls | All | 33.3 | 1.8 | 33.3 | 2.6 | 0.0 | |
| Boys | NH white | 34.5 | 2.6 | 32.6 | 3.7 | −1.9 | |
| NH black | 32.1 | 1.8 | 33.0 | 5.0 | 0.9 | ||
| Mexican-American | 40.5 | 2.6 | 46.1 | 7.4 | 5.6 | ||
| Girls | NH white | 31.7 | 2.4 | 29.9 | 4.3 | −1.8 | |
| NH black | 44.5 | 1.5 | 46.3 | 4.1 | 1.8 | ||
| Mexican-American | 37.1 | 1.9 | 42.1 | 4.3 | 5.0 | ||
Change = prevalence in 2007–08 − prevalence in 2003–06.
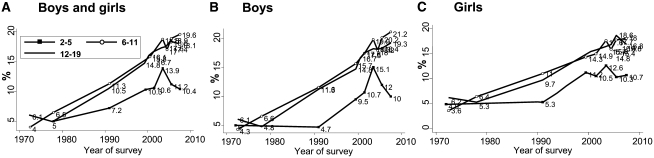
Figure 1.
Age and sex disparities: trend in the prevalence (percent) of obesity (BMI ≥ 95th percentile) in U.S. children and adolescents. NHANES 1971–74 to 2007–08. Values are prevalence [data sources: (8, 9)].
Age and sex disparities in the trends in prevalence between 1971–72 and 2007–08
Figure 1 shows that in all age groups, the prevalence of obesity has increased since the 1970s (1, 8, 18, 19) and the increases seem to be occurring at a faster rate since NHANES III (1988–94). Between 1988–94 and 2007–08, our estimated average annual increase was ~0.6 percentage points. Among children, boys had a faster increase in obesity than girls (0.7 vs. 0.5 percentage points), although the increases were similar in adolescents (~0.5%). Overall, between 2003–06 and 2007–08, the prevalence continued to increase, although it decreased in some groups (preschool children and some minority groups).
Some recent NHANES data indicate the increase in obesity prevalence might have leveled off (8), but we suspect that this is inconclusive, in part due to the limitations of the NHANES data such as relatively small yearly sample sizes and for subgroups. For example, the decrease or no changes in the prevalence observed might be because of sampling problems, which has been shown in YRBSS. Recent YRBSS data showed no increase in obesity prevalence among U.S. adolescents between 1999 (10.7%) and 2001 (10.5%), but it increased to 13.1% in 2005–07 (10).
Ethnic disparities in the prevalence and time trends
NHANES and other national survey data, which included other minority groups not covered in NHANES, reveal large ethnic disparities. Overall, these data indicate that whites and Asians had the lowest prevalence and American Indians had the highest prevalence. Blacks and Mexican Americans had rates higher than those in whites.
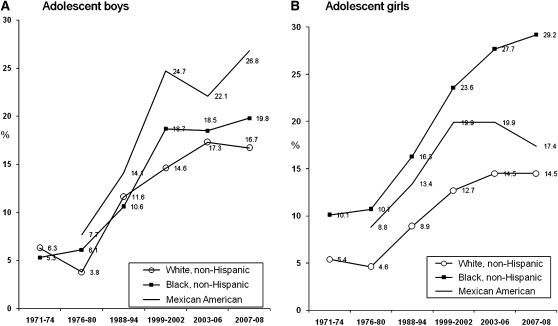
show the ethnic disparities in the prevalence of obesity in U.S. children and adolescents based on 3 different national surveys. Figure 2 show the patterns and time trends in adolescents based on NHANES data. There were considerable ethnic disparities in the prevalence. The ethnic disparities were greater in girls than in boys and they became greater between 1976–80 and 2003–06. Note that we suspected that the patterns indicated by the 2007–08 data may not be reliable regarding ethnic disparities. White children and adolescents had the lowest prevalence compared with their black and Mexican-American counterparts. In 2003–06, the combined prevalence was 30.7, 34.9, and 38.0% among the 2- to 19-y olds in the 2 groups, respectively. Among boys, Mexican-Americans had the highest combined prevalence (40.5% vs. 34.5% in whites and 32.1% in blacks). In girls, blacks had the highest prevalence (44.5% vs. 31.7% in whites and 142 37.1% in Mexican-Americans) (8).
Figure 2.
Ethnic disparities: trends in the prevalence (percent) of obesity (BMI ≥ 95th percentile) in U.S. adolescent boys and girls: NHANES 1971–72 to 2007–08. Values are prevalence [data sources: 1, 8, 9, 11)].
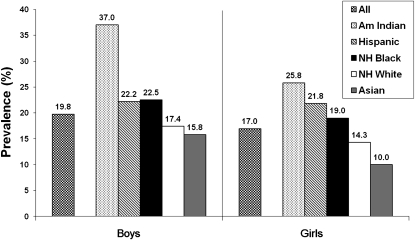
Other research shows that large ethnic disparities emerge at very young ages and exist even in homogeneous SES groups in the U.S. For example, data from the Early Childhood Longitudinal Study (ECLS), nationally representative data collected from 8550 preschool children in 2005, show that large ethnic differences in obesity prevalence emerged in this age group (Fig. 3). Among preschool U.S. boys, the prevalence was 37.0% in American Indians (highest), 15.8% in Asians (lowest), and 17.4% in whites (21). A study of 21,911 preschool children enrolled in the Hawaiian WIC program (low income participants in federal nutrition programs) in 1997–98 found large ethnic differences in obesity rates (22). Among the 8 ethnic groups (white, black, Asian, Filipino, Hawaiian, Hispanic, Samoan, and other), Samoan children had the highest prevalence (17.5% in 1-y olds and 27.0% in 2- to 4-y olds), whereas Asian 1-y olds (2.3%) and black 2- to 4-y olds (7.3%) had the lowest rates.
Figure 3.
Ethnic disparities: prevalence (percent) of obesity (BMI ≥ 95th percentile) in U.S. preschool children: ECLS 2005 data. Based on nationally representative data collected from 8550 preschool children in the ECLS in 2005. Values are prevalence [data source: (21)].
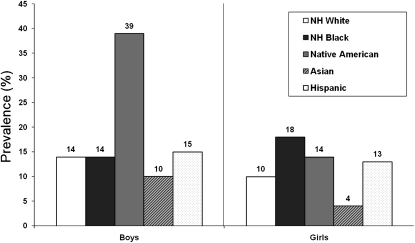
Previously, the PATHWAY study of 1704 schoolchildren (in grades 2–3) from 41 schools from 7 American Indian communities reported a much higher prevalence than the national average. At baseline at the end of the 1990s, about one-half of the study participants were overweight or obese (51.5% in girls vs. 46.5% in boys) and 30.5% of girls and 26.8% of boys were obese, except for large variations across the study sites (23). The Add Health Study 1996 data show that Asian adolescents had the lowest obesity prevalence among main ethnic groups (Fig. 4). It was 10 and 4% in Asian adolescent boys and girls compared with 14 and 10% in whites, respectively (24).
Figure 4.
Ethnic disparities: prevalence (percent) of obesity among U.S. adolescents: Add Health Study Wave II (1996) data. Measured weight and height were collected (in Wave II, 1996) from >10,000 adolescents aged 13–20 y. Obesity was defined based on the IOTF BMI cutpoints corresponding to BMI = 30 at age 18 y. Values are prevalence [data source: (30)].
Sex and ethnic disparities in the over time increases in the distribution of different adiposity measures
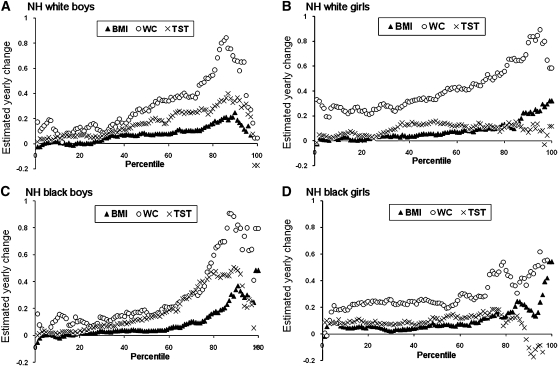
Recently, we examined the shifts in BMI, WC, and TST (only in children) in children and adolescents (16) between NHANES 1988–94 and 1999–04. First, based on each adiposity measure, we divided the U.S. population in each NHANES wave into 100 groups, from the thinnest to the heaviest groups (called percentiles). Then, we estimated the mean BMI within each percentile group. Next, we calculated the between wave changes in these means and similarly for other fatness measures. To calculate the yearly changes, the changes were divided by 10.5 y, the average inter-wave period. Based on these measures we created distribution curves using kernel densities, a nonparametric smoothing technique to help examine distributions and visually assess their change in shape and shifts over time (16). These provide much more informative and important insights than solely examining overweight and obesity prevalence. In adolescents, during this period, mean BMI increased by 0.64 in boys and 0.60 in girls; mean BMI percentiles increased by 3.15 and 3.01; average WC increased substantially, by 2.42 and 2.85 cm; and TST increased by 1.18 and 0.81 mm, respectively.
Figure 5 shows the over time changes in BMI, WC, and TST in U.S. adolescents during 1988–2004. Though apparently different, their shift patterns had several common features: the population gained more adiposity over time. Heavier (obese) U.S. adolescents had gained more body fat over time, especially more visceral fat (as indicated by WC), than of overall body fat as indicated by BMI. In that study, we also fit models estimating the over time adjusted adiposity changes by sex, age, and ethnicity and within the lowest (thin group) against those in the uppermost quintile (obese group) (16). The average annual changes were significantly greater in the obese groups. Further, the increase in WC was greater than those in BMI and TST. This indicates greater health risks, because WC is a better predictor of adverse health consequences.
Figure 5.
Sex and ethnic disparities in over time adiposity increases during 1988–94 to 1999–2004: yearly average over time increases in BMI (kg/m2), WC (cm), and TST (mm) by their distribution in U.S. adolescents. Values are means of estimated average yearly shift within percentile groups. Ordinary least square estimate of average yearly shift within percentile groups based on data collected NHANES III (1988–94) and during 1999 and 2004 [adapted with permission from (16)].
There were sociodemographic disparities in these shifts. In fact, mean BMI disparity increased over time, particularly when comparing black to white girls. Among girls (2–19 y), but not boys, blacks had significantly larger adjusted mean shifts in all adiposity measures than whites; their mean BMI adjusted shifts were 1.34 vs. 0.42.
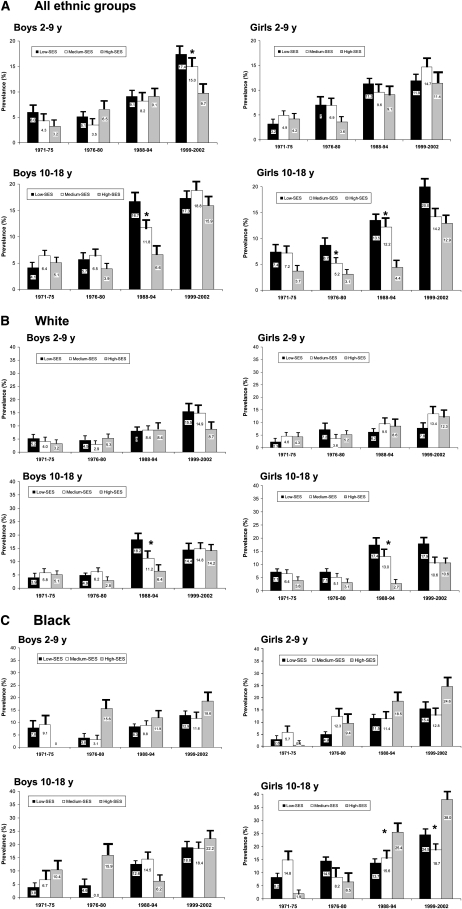
SES disparities in the prevalence
The patterns observed in U.S. youth share some similarities with those in adults but with some unique features. In one study based on NHANES data collected between 1971 and 2002, we used family per capita income tertiles to define low-, medium-, and high-SES groups and assessed the association between SES and obesity and the related sex, age, and ethnic differences and the over time changes in the association in U.S. children and adolescents (4). SES was inversely related to obesity in whites but not among blacks or Mexican-Americans (Fig. 6). High-SES young boys had the lowest prevalence compared with their counterparts, whereas the SES difference in the prevalence was small in young girls. Adolescents saw no consistent SES-obesity association in boys, but low-SES adolescent girls had a much higher prevalence than their medium- and high-SES counterparts (20.0 vs. 14.2 and 12.9%). This is mainly due to the strong inverse association between SES and obesity in white adolescent girls. High-SES black adolescent girls had a higher prevalence than their lower SES counterparts (38.0 vs. 18.7 and 24.5%). Further, our analysis also indicates that only a very small proportion (e.g. <5%) of the variations in BMI could be explained by family income.
Figure 6.
SES disparities of obesity in U.S. children and adolescents by sex, age, and ethnicity: the prevalence (percent) in low-, medium-, and high-SES groups in NHANES 1971–74 to 1999–2002. Values are prevalence and standard errors. *Significant between group difference, P < 0.05 [adapted with permission from (4)].
Geographic and urban-rural disparities
YRBSS data have shown considerable disparities in obesity rates across the covered states and cities in the U.S. (Table 2) (10). We ranked the states (or cities) based on their prevalence and calculated the ratio between the lowest and highest rates, respectively. In 2007, across the 39 included states, obesity prevalence ranged from 8.7 to 17.9% and was 20.4 to 35.8% for the combined prevalence. Utah (8.7%) had the lowest and Mississippi (17.9%) had the highest obesity prevalence. The disparities were greater across cities, ranging between 21.0 (San Francisco, CA) and 39.7 (Detroit, MI) for combined prevalence.
Table 2.
Regional differences in the prevalence (percent) of obesity and overweight in U.S. adolescents (high school students), the 2007 YRBSS data: ranks of states being covered1
| Obesity (BMI ≥ 95th percentile) |
Combined (BMI ≥ 85th percentile) |
|||||||
| Site | Female | Male | Total | Rank2 | Female | Male | Total | Rank2 |
| State surveys | ||||||||
| Alaska | 9.7 | 12.5 | 11.1 | 26 | 24.4 | 30.1 | 27.3 | 18 |
| Arizona | 8.5 | 14.7 | 11.7 | 22 | 20.7 | 30.7 | 25.9 | 25 |
| Arkansas | 9.1 | 18.4 | 13.9 | 9 | 25.9 | 33.2 | 29.7 | 12 |
| Connecticut | 8.2 | 16.2 | 12.3 | 19 | 19.7 | 31.1 | 25.6 | 28 |
| Delaware | 10.9 | 15.6 | 13.3 | 12 | 30.1 | 31.6 | 30.8 | 8 |
| Florida | 6.8 | 15.4 | 11.2 | 25 | 21.9 | 30.7 | 26.4 | 21 |
| Georgia | 11.1 | 16.6 | 13.8 | 10 | 30.0 | 34.1 | 32.0 | 3 |
| Hawaii | 11.3 | 19.4 | 15.6 | 4 | 26.8 | 32.7 | 29.9 | 9 |
| Idaho | 6.4 | 15.5 | 11.1 | 26 | 19.6 | 25.9 | 22.8 | 37 |
| Illinois | 9.9 | 15.9 | 12.9 | 14 | 25.7 | 31.4 | 28.6 | 15 |
| Indiana | 9.9 | 17.8 | 13.8 | 10 | 24.7 | 33.7 | 29.1 | 13 |
| Iowa | 8.8 | 13.7 | 11.3 | 24 | 19.4 | 29.9 | 24.8 | 32 |
| Kansas | 6.8 | 15.2 | 11.1 | 26 | 20.9 | 29.8 | 25.5 | 29 |
| Kentucky | 11.0 | 19.7 | 15.6 | 4 | 26.5 | 37.0 | 32.0 | 3 |
| Maine | 7.6 | 17.5 | 12.8 | 15 | 19.9 | 31.3 | 25.9 | 25 |
| Maryland | 9.2 | 16.7 | 13.1 | 13 | 24.6 | 31.8 | 28.3 | 16 |
| Massachusetts | 7.1 | 14.8 | 11.1 | 26 | 22.3 | 28.9 | 25.7 | 27 |
| Michigan | 9.8 | 15.0 | 12.4 | 17 | 25.4 | 32.3 | 28.9 | 14 |
| Mississippi | 14.7 | 21.2 | 17.9 | 1 | 33.5 | 38.1 | 35.8 | 1 |
| Missouri | 8.6 | 15.3 | 12.0 | 20 | 22.2 | 30.2 | 26.3 | 22 |
| Montana | 6.3 | 13.7 | 10.1 | 35 | 19.2 | 27.5 | 23.4 | 36 |
| Nevada | 7.6 | 14.2 | 11.0 | 31 | 21.5 | 29.3 | 25.5 | 29 |
| New Hampshire | 7.2 | 15.9 | 11.7 | 22 | 20.3 | 31.6 | 26.1 | 24 |
| New Mexico | 6.0 | 15.5 | 10.9 | 32 | 19.8 | 28.7 | 24.4 | 33 |
| New York | 7.6 | 14.1 | 10.9 | 32 | 23.9 | 30.4 | 27.2 | 19 |
| North Carolina | 9.5 | 15.9 | 12.8 | 15 | 26.7 | 32.9 | 29.9 | 9 |
| North Dakota | 8.0 | 11.8 | 10.0 | 36 | 19.2 | 27.8 | 23.7 | 34 |
| Ohio | 8.5 | 16.0 | 12.4 | 17 | 23.1 | 31.4 | 27.4 | 17 |
| Oklahoma | 9.8 | 19.2 | 14.7 | 6 | 26.6 | 32.9 | 29.9 | 9 |
| Rhode Island | 7.5 | 13.8 | 10.7 | 34 | 23.7 | 30.1 | 26.9 | 20 |
| South Carolina | 12.2 | 16.6 | 14.4 | 8 | 31.1 | 31.9 | 31.5 | 6 |
| South Dakota | 7.6 | 10.6 | 9.1 | 38 | 20.0 | 27.1 | 23.6 | 35 |
| Tennessee | 12.0 | 21.6 | 16.9 | 2 | 31.9 | 38.0 | 35.0 | 2 |
| Texas | 11.6 | 19.9 | 15.9 | 3 | 27.4 | 35.4 | 31.5 | 6 |
| Utah | 5.1 | 12.1 | 8.7 | 39 | 15.0 | 25.5 | 20.4 | 39 |
| Vermont | 8.0 | 15.1 | 11.8 | 21 | 21.8 | 30.1 | 26.3 | 22 |
| West Virginia | 11.7 | 17.6 | 14.7 | 6 | 30.7 | 32.6 | 31.7 | 5 |
| Wisconsin | 7.2 | 14.7 | 11.1 | 26 | 19.8 | 30.0 | 25.1 | 31 |
| Wyoming | 6.6 | 11.8 | 9.3 | 37 | 16.6 | 24.5 | 20.7 | 38 |
| Median | 8.5 | 15.5 | 12.0 | 23.3 | 30.8 | 27.0 | ||
| Range | 5.1–14.7 | 10.6–21.6 | 8.7–17.9 | 19.4–33.5 | 25.5–38.1 | 20.4–35.8 | ||
| Ratio3 | 2.9 | 2.0 | 2.1 | 1.7 | 1.5 | 1.8 | ||
| Local survey | ||||||||
| Baltimore, MD | 19.0 | 17.9 | 18.5 | 2 | 40.0 | 36.5 | 38.4 | 3 |
| Boston, MA | 11.7 | 17.2 | 14.5 | 12 | 33.7 | 32.4 | 33.0 | 12 |
| Broward County, FL | 6.5 | 10.2 | 8.4 | 22 | 23.7 | 23.9 | 23.8 | 20 |
| Charlotte-Mecklenburg, NC | 8.9 | 10.7 | 9.8 | 19 | 23.7 | 28.9 | 26.3 | 18 |
| Chicago, IL | 13.6 | 18.0 | 15.8 | 9 | 34.3 | 34.6 | 34.5 | 8 |
| Dallas, TX | 15.7 | 22.9 | 19.3 | 1 | 36.9 | 39.6 | 38.3 | 4 |
| DeKalb County, GA | 13.4 | 12.8 | 13.1 | 13 | 30.3 | 28.6 | 29.4 | 13 |
| Detroit, MI | 17.1 | 19.9 | 18.4 | 3 | 41.7 | 37.7 | 39.7 | 1 |
| District of Columbia | 15.8 | 19.6 | 17.7 | 4 | 35.7 | 35.4 | 35.5 | 7 |
| Hillsborough County, FL | 8.4 | 14.6 | 11.5 | 17 | 21.4 | 28.7 | 25.1 | 19 |
| Houston, TX | 11.5 | 21.7 | 16.7 | 6 | 31.2 | 37.6 | 34.4 | 9 |
| Los Angeles, CA | 11.7 | 20.9 | 16.5 | 7 | 35.8 | 41.3 | 38.7 | 2 |
| Memphis, TN | 13.7 | 19.0 | 16.2 | 8 | 37.0 | 34.7 | 35.9 | 6 |
| Miami-Dade County, FL | 8.9 | 16.8 | 13.0 | 14 | 23.4 | 32.3 | 28.0 | 14 |
| Milwaukee, WI | 15.4 | 20.0 | 17.7 | 4 | 39.6 | 33.8 | 36.7 | 5 |
| New York City, NY | 9.4 | 13.6 | 11.5 | 17 | 27.1 | 28.5 | 27.8 | 15 |
| Orange County, FL | 8.6 | 16.5 | 12.6 | 15 | 23.3 | 30.6 | 27.0 | 17 |
| Palm Beach County, FL | 6.1 | 10.9 | 8.5 | 20 | 17.1 | 24.9 | 21.0 | 21 |
| Philadelphia, PA | 14.1 | 16.6 | 15.2 | 10 | 32.9 | 34.6 | 33.6 | 10 |
| San Bernardino, CA | 12.6 | 17.3 | 15.0 | 11 | 32.4 | 34.1 | 33.3 | 11 |
| San Diego, CA | 6.7 | 17.5 | 12.3 | 16 | 22.9 | 31.6 | 27.4 | 16 |
| San Francisco, CA | 3.7 | 13.0 | 8.5 | 20 | 15.8 | 25.9 | 21 | 21 |
| Median | 11.7 | 17.2 | 14.8 | 30.9 | 32.9 | 32.5 | ||
| Range | 3.7–19.0 | 10.2–22.9 | 8.4–19.3 | 17.1–41.7 | 24.9–41.3 | 21.0–39.7 | ||
| Ratio3 | 5.1 | 2.2 | 2.3 | 2.4 | 1.7 | 1.9 | ||
Our analysis was conducted based on results reported in (10).
Ranked the states based on the prevalence for both boys and girls, from highest to lowest. Data were available for only 39 states. These were based on self-reported weight and height.
Ratio = highest prevalence/lowest prevalence.
Our previous research based on NHANES III data shows that rural-urban differences were small and varied across age groups (25). In children aged 6–9 y, the combined prevalence was higher in urban areas (26.1 vs. 22.8%), but in adolescents, it was slightly higher in rural areas (27.2 vs. 24.4%). In both age groups, obesity prevalence was similar. No such studies have been reported based on recent NHANES data on the rural-urban differences. We suspect it is unlikely there would be main changes in the patterns.
Conclusions
Childhood obesity is becoming a national public health crisis, because one-third of U.S. young people are overweight or obese. However, the disparity patterns and related trends in the U.S. childhood obesity epidemic are complex. This reflects the complexity and dynamics in its etiology. Clearly, some population groups are affected more seriously than others. For example, Native American children have the highest prevalence of obesity, whereas Asians have the lowest rate among all ethnic groups. Preschool age children have a lower obesity prevalence than older children. Young people in some states and cities are twice more likely to be overweight or obese than those living in other regions. Low-SES is associated with obesity only among some population groups. Thus, both tailored and comprehensive intervention approaches are needed to fight the epidemic considering the scope of the obesity disparities and available recourses.
The disparities in the prevalence of obesity in U.S. young people suggest that obegenic environmental changes may affect some groups more than others, which is also because different groups may have responded differently to the environmental factors. Lifestyles such as higher consumption of energy dense foods and sedentary behaviors may in part explain the gender, age, and ethnic disparities. For example, adolescents had greater autonomy in deciding their health behavior and choices than young children who are under more parental influence. Some minority groups often are more likely to live in low-SES communities with less access to healthy choices and tend to underestimate the risks of obesity than other groups.
Eliminating ethnic and socioeconomic disparities in health status, including obesity, is a national priority in the U.S. (5). However, the determinants of ethnic disparities in obesity remain poorly understood. Although obesity disparities may be a result of interactions between genetic and environmental factors, with different groups responding differently to similar environmental conditions, environmental factors play a key role fueling the obesity epidemic and related disparities. A growing body of research suggests that complex factors operating interactively at multiple levels including individual, community/school, society, and international levels have contributed to the obesity crisis in the U.S. and many other countries (26). More research and monitoring programs are needed to help understand the underlying causes of the disparities. In addition, future research on the health and economic consequences of childhood obesity is needed, both in the whole population and minority groups. Such consequences could vary across groups and change over time.
Several health organizations, including The Institute of Medicine and the WHO, have published recommendations to help fight childhood obesity (27, 28). Overall, these recommendations call on comprehensive, population-based interventions with the involvement of multiple parties in society. Several recent reviews suggest the majority of previous childhood obesity intervention trials, most of which focused on individuals’ behaviors and school settings, are not successful (29–32). It is clear that the U.S. national objectives specified in the Healthy People 2010 Program related to obesity cannot be met. The objectives need to be reframed and be more realistic when developing the Healthy People 2020 objectives. More vigorous government support and programs are needed to fight the epidemic, reduce the disparities, and prepare the nation to face the related future consequences. Effective intervention programs to promote healthy lifestyles among young people will not only reduce obesity but will also help prevent other chronic diseases and reduce related costs.
Acknowledgments
I thank Dr. May Beydoun from The National Institute on Aging for her great assistance in helping develop an earlier draft of this paper, Hsin-jen Chen for his assistance in analyzing the YRBSS data, and Dr. Xiaoli Chen and Dr. Hyunjung Lim for their assistance in reviewing the final paper draft. The sole author had responsibility for all parts of the manuscript.
Footnotes
Supported in part by the NIH/The National Institute of Diabetes and Digestive and Kidney Diseases (R01DK81335-01A1) and The National Institute of Child Health and Human Development (1R01HD064685-01A1, 1R03HD058077-01A1, R03HD058077-01A1S1).
Author disclosure: Y. Wang, no conflicts of interest.
Abbreviations used: ECLS, Early Childhood Longitudinal Study; NH, non-Hispanic; SES, socioeconomic status; TST, triceps skinfold thickness; WC, waist circumference; YRBSS, Youth Risk Behavior Surveillance System.
Literature Cited
- 1.Wang Y, Beydoun MA. The obesity epidemic in the United States: gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28 [DOI] [PubMed] [Google Scholar]
- 2.WHO Obesity: preventing and managing the global epidemic: report of a WHO consultation. Technical report series 894. Geneva: WHO; 2000 [PubMed] [Google Scholar]
- 3.Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1:11–25 [DOI] [PubMed] [Google Scholar]
- 4.Wang Y, Zhang Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. Am J Clin Nutr. 2006;84:707–16 [DOI] [PubMed] [Google Scholar]
- 5.U.S. Department of Health and Human Services. Healthy People 2010; 2006 [cited 2010 Nov 30]. Available from: http://www.healthypeople.gov/
- 6.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–73 [DOI] [PubMed] [Google Scholar]
- 7.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. Racial differences in the tracking of childhood BMI to adulthood. Obes Res. 2005;13:928–35 [DOI] [PubMed] [Google Scholar]
- 8.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299:2401–5 [DOI] [PubMed] [Google Scholar]
- 9.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303:242–9 [DOI] [PubMed] [Google Scholar]
- 10.Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Harris WA, Lowry R, McManus T, et al. Youth risk behavior surveillance: United States, 2007. MMWR Surveill Summ. 2008;57:1–131 [PubMed] [Google Scholar]
- 11.Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, Hayflick L, Butler RN, Allison DB, Ludwig DS. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352:1138–45 [DOI] [PubMed] [Google Scholar]
- 12.CDC. National Health and Nutrition Examination Survey [cited 2006 Sep 25]. Available from: http://www.cdc.gov/nchs/nhanes.htm.
- 13.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–55 [DOI] [PubMed] [Google Scholar]
- 14.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, Johnson CL. CDC growth charts: United States. Adv Data. 2000;314:1–27 [PubMed] [Google Scholar]
- 15.Beydoun MA, Wang Y. Gender-ethnic disparity in BMI and waist circumference distribution shifts in US adults. Obesity (Silver Spring). 2009;17:169–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beydoun MA, Wang Y. Socio-demographic disparities in distribution shifts of adiposity measures among American children and adolescents. Int J Pediatr Obes. Epub 2010 Aug 19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang Q, Wang Y. Using concentration index to study changes in socio-economic inequality of overweight among US adolescents between 1971 and 2002. Int J Epidemiol. 2007;36:916–25 [DOI] [PubMed] [Google Scholar]
- 18.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291:2847–50 [DOI] [PubMed] [Google Scholar]
- 19.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002;288:1728–32 [DOI] [PubMed] [Google Scholar]
- 20.Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity (Silver Spring). 2008;16:2323–30 [DOI] [PubMed] [Google Scholar]
- 21.Anderson SE, Whitaker RC. Prevalence of obesity among US preschool children in different racial and ethnic groups. Arch Pediatr Adolesc Med. 2009;163:344–8 [DOI] [PubMed] [Google Scholar]
- 22.Baruffi G, Hardy CJ, Waslien CI, Uyehara SJ, Krupitsky D. Ethnic differences in the prevalence of overweight among young children in Hawaii. J Am Diet Assoc. 2004;104:1701–7 [DOI] [PubMed] [Google Scholar]
- 23.Caballero B, Himes JH, Lohman T, Davis SM, Stevens J, Evans M, Going S, Pablo J; Pathways Study Research Group Body composition and overweight prevalence in 1704 schoolchildren from 7 American Indian communities. Am J Clin Nutr. 2003;78:308–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harris KM, Gordon-Larsen P, Chantala K, Udry JR. Longitudinal trends in race/ethnic disparities in leading health indicators from adolescence to young adulthood. Arch Pediatr Adolesc Med. 2006;160:74–81 [DOI] [PubMed] [Google Scholar]
- 25.Wang Y. Cross-national comparison of childhood obesity: the epidemic and the relationship between obesity and socioeconomic status. Int J Epidemiol. 2001;30:1129–36 [DOI] [PubMed] [Google Scholar]
- 26.Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. Obes Rev. 2004;5 Suppl 1:4–104 [DOI] [PubMed] [Google Scholar]
- 27.Institute of Medicine Preventing childhood obesity: health in the balance. Washington, DC; 2005 [Google Scholar]
- 28.WHO. What can be done to fight the childhood obesity epidemic? [cited 2009 Jun 30]. Available from: http://www.who.int/dietphysicalactivity/childhood_what_can_be_done/en/index.html.
- 29.Birch LL, Ventura AK. Preventing childhood obesity: what works? Int J Obes (Lond). 2009;33 Suppl 1:S74–81 [DOI] [PubMed] [Google Scholar]
- 30.Summerbell CD, Waters E, Edmunds LD, Kelly S, Brown T, Campbell KJ. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2005;(3):CD001871. [DOI] [PubMed] [Google Scholar]
- 31.Gonzalez-Suarez C, Worley A, Grimmer-Somers K, Dones V. School-based interventions on childhood obesity: a meta-analysis. Am J Prev Med. 2009;37:418–27 [DOI] [PubMed] [Google Scholar]
- 32.Zenzen W, Kridli S. Integrative review of school-based childhood obesity prevention programs. J Pediatr Health Care. 2009;23:242–58 [DOI] [PubMed] [Google Scholar]