Abstract
Objective
Comprehensive behavior change frameworks are needed to provide guidance for the design, implementation, and evaluation of diabetes self-care programs in diverse populations. We applied the Information-Motivation-Behavioral Skills (IMB) model, a well-validated, comprehensive health behavior change framework, to diabetes self-care.
Methods
Patients with diabetes were recruited from an outpatient clinic. Information gathered pertained to demographics, diabetes knowledge (information); diabetes fatalism (personal motivation); social support (social motivation); and diabetes self-care (behavior). Hemoglobin A1C values were extracted from the patient medical record. Structural equation models tested the IMB framework.
Results
More diabetes knowledge (r=0.22 p<0.05), less fatalistic attitudes (r=−0.20, p<0.05), and more social support (r=0.27, p < 0.01) were independent, direct predictors of diabetes self-care behavior; and through behavior, were related to glycemic control (r=−0.20, p<0.05).
Conclusions
Consistent with the IMB model, having more information (more diabetes knowledge), personal motivation (less fatalistic attitudes), and social motivation (more social support) was associated with behavior; and behavior was the sole predictor of glycemic control.
Practice implications
The IMB model is an appropriate, comprehensive health behavior change framework for diabetes self-care. The findings indicate that in addition to knowledge, diabetes education programs should target personal and social motivation to effect behavior change.
1. Introduction
Diabetes affects approximately 7.8% of the United States population or 23.6 million people [1]. Diabetes is the leading cause of cardiovascular disease, stroke, blindness, and non-traumatic lower limb amputations and was the seventh leading cause of death listed on U.S. death certificates in 2006. Diabetes is also associated with significant health care costs [1].
Multiple studies have established that poor glycemic control is a strong predictor of adverse outcomes in patients with diabetes [2-4]. Diabetes self-management training is an important aspect of diabetes care [5]. A systematic review of 72 randomized controlled trials in patients with type 2 diabetes (T2DM) showed that self-management training improved diabetes knowledge, frequency and accuracy of self-monitoring of blood glucose, self-reported dietary habits, and glycemic control [5]. There is also strong evidence that patient self-management practices account for 90-98% of the variance in glycemic control [6, 7].
However, recent studies using nationally representative samples have shown that few patients engage in multiple self-care behaviors at recommended levels [8, 9], suggesting that improvements are needed. The current trend in diabetes self-management is to use theory-based health behavior change models to inform educational efforts [10]. The Information—Motivation—Behavioral Skills (IMB) model of health behavior is a theoretical model developed in 1992 to predict HIV-preventive behavior; however, its concepts can be broadly applied to predict positive health behavior change in a range of contexts [11].
The IMB model of health behavior change posits that performing a health promotion behavior is a function of the extent to which someone is well informed about the behavior, motivated to perform the behavior (e.g., has positive personal beliefs and attitudes towards the behavior or outcome, and social support for the behavior), and has the requisite skills to execute the behavior and confidence in their ability to do so across various situations [12, 13]. Essentially, one who is well informed and motivated is thought to develop and enact the skills necessary to enact the behavior at focus, and is likely to ultimately reap greater health benefits [12, 13]. The model’s constructs and relationships among them have been well-supported across populations and health promotion behaviors [12, 13]; however, very minimal work has been done in diabetes.
We sought to evaluate the information and motivation components of the IMB model; information (diabetes knowledge) and motivation (personal: fatalistic attitudes; and social: social support) with respect to diabetes self-care behavior via a series of structural equation model tests. We hypothesized, based on the theoretical underpinnings of the IMB model, that information (diabetes knowledge) and motivation (personal: fatalistic attitudes; and social: social support) would be significantly associated with the performance of diabetes self-care behaviors and that such performance would be significantly associated with glycemic control.
2. Methods
2.1 Sample
We recruited consecutive patients with diagnosed T2DM and scheduled appointments at the Medical University of South Carolina (MUSC) Internal Medicine Clinic, Charleston, South Carolina. The institutional review board at MUSC approved all procedures prior to study enrollment. Eligible participants were clinic patients, age 18 years or older with a diagnosis of T2DM in the medical record, and a clinic appointment between June-August 2008. Patients were ineligible if they did not speak English, or if the research assistants determined (by interaction or chart documentation) they were too ill or cognitively impaired to participate.
2.2 Data and procedure
Research assistants reviewed the electronic clinic roster daily to identify eligible patients. Eligible patients were approached in the clinic waiting room, and provided a description of the study. Those interested and eligible were consented and taken to a private area in the clinic to complete the study instruments. Participants completed the assessment before or after their scheduled clinic appointments, depending on clinic flow. One hundred and thirty-six subjects were consented and completed the study.
We collected data on self-reported age, sex, race/ethnicity, education, household income, and marital status. Additional measures included validated surveys of diabetes knowledge, diabetes fatalism, social support, and diabetes self-care behavior. Hemoglobin A1C values were extracted from the electronic medical records.
2.2.1 Diabetes knowledge
Diabetes knowledge served as the measure of information, and was assessed with the Diabetes Knowledge Questionnaire (DKQ) [14]. The DKQ elicits information about respondent’s understanding of the cause of diabetes, types of diabetes, self-management skills, and complications of diabetes. Responses are graded as “yes”, “no”, or “don’t know”. The final score was based on the percentage of correct scores, with a maximal possible score of 100.
2.2.2 Fatalistic attitudes
Diabetes fatalism served as the measure of personal motivation [15], and was assessed with the 18-item Diabetes Fatalism Scale (DFS-18). Diabetes fatalism is operationally defined as “a complex psychological cycle characterized by perceptions of despair, hopelessness, and powerlessness.” Items are scored on a 6-point Likert scale with scores ranging from to 1 = strongly disagree to 6 = strongly agree. Higher scores represent more fatalistic attitudes (i.e. less individual motivation). A summary score consisting of the sum of individual items is created, such that higher summary scores represent greater diabetes fatalism. The DFS-18 has good internal consistency (Cronbach’s alpha 0.73) and response variability (range 30-90; mean 58.2.; SD 6.8).
2.2.3 Social support
Social support served as the measure of social motivation, and was assessed with the 19-item Medical Outcomes Study (MOS) Social Support Survey [16]. The MOS measures perceived general functional support in four domains, including emotional/informational, tangible, positive social interaction, affection; and yields an overall support index, which was used in our analyses.
2.2.4 Diabetes self-care behavior
Self-care behavior was assessed with the 11-item Summary of Diabetes Self-Care Activities (SDSCA) scale [17]. The SDSCA measures frequency of self-care activity in the last 7 days for five aspects of the diabetes regimen: general diet (followed healthful diet), specific diet (ate fruits/low fat diet), foot care, blood-glucose testing, exercise, and cigarette smoking.
2.2.5 Glycemic control
Patients’ most recent hemoglobin A1C value was extracted from the medical record, and served as the measure of glycemic control.
2.3 Statistical analyses
Descriptive statistics were performed using SPSS 17.0. A confirmatory factor analytic model (CFA) was estimated using AMOS 17.0, a structural equation modeling program. The CFA tested the measurement model (i.e., the latent variable diabetes self-care behavior was predicted to load onto six measured variables: general diet, specific diet, foot care, blood-glucose testing, exercise, and cigarette smoking). The CFA model was tested for data fit. Variables with non-significant factor loadings were omitted from the measurement model nested in the subsequent structural equation model (SEM).
The hypothesized SEM was estimated using AMOS 17.0. The Information—Motivation—Behavioral Skills (IMB) model of health behavior change [18-20] was used to conceptualize the hypothesis that information (diabetes knowledge), personal motivation (diabetes fatalism), and social motivation (social support) are independent predictors of behavior (diabetes self-care), and behavior, in turn, is an independent predictor of glycemic control (A1C). The sample size of 130 cases was sufficient to estimate fourteen paths, with eleven hypothesized causal effects and three covariances [21, 22].
Hypotheses regarding the specific structural relations of the constructs in the model were evaluated through inspection of the direction and magnitude of the path coefficients. Consistent with IMB model of diabetes self-care assumptions, diabetes knowledge (as a measure of information), fatalistic attitudes (as a measure of personal motivation), and social support (as a measure of social motivation) were hypothesized to predict diabetes self-care behavior, not glycemic control (A1C). Only behavior was predicted to relate to A1C. Pathways between variables hypothesized to be not significant were included for verification of no association.
The likelihood ratio chi-square tests are reported, but model fit was primarily evaluated with the comparative fit index (CFI), and root mean square error of approximation (RMSEA) [23, 24]. A non-significant likelihood ratio chi-square test suggests the data fit the hypothesized structure. A CFI value can range from 0 to 1, where 1 indicates perfect data fit, 0.9 indicates adequate fit, and 0.8 is considered marginal fit [25]. An RMSEA value can range from 0 to ∞, with smaller values indicating closer fit; specifically, values at 0.05 or lower indicate close fit, values at 0.08 or lower indicate reasonable fit, and values greater than or equal to 0.10 indicate poor fit [26].
3. Results
3.1 Sample characteristics
A total of 130 men and women with type 2 diabetes completed all measures noted above. Participants were, on average, 63 years old. The majority were female (72.5%), African American (70.9%), not working (78.3%), and insured (96.4%) (see Table 1). Descriptive information (Mean +/− SD, or %) on each measure is presented in Table 2.
Table 1.
Sample Demographics
| Demographics | Means ± SD, or % |
|---|---|
| Mean Age (Years) | 62.7 ± 11.8 |
| Age Categories | |
| 18-49 years | 14.5 |
| 50-64 years | 36.2 |
| 65+ years | 49.3 |
| Females | 72.5 |
| Race/Ethnicity | |
| Non-Hispanic White | 28.6 |
| Non-Hispanic Black | 71.4 |
| Mean Education (Years) | 12.4 ± 5.2 |
| Education Categories | |
| <High school graduate | 34.1 |
| High school graduate | 34.1 |
| >High school graduate | 31.8 |
| Married | 41.2 |
| Employed | 21.7 |
| Income Categories | |
| <$10,000 | 19.6 |
| <$15,000 | 26.1 |
| $15,000+ | 54.3 |
| Insured | 96.4 |
| Health Status | |
| Better than last year | 19.6 |
| Worse than last year | 26.1 |
| Same as last year | 54.3 |
Table 2.
Diabetes Knowledge, Fatalism, Social Support, Self-care, and Glycemic Control
| Measures | Means ± SD, or % |
|---|---|
| Diabetes Knowledge | |
| Diabetes Knowledge Test (Mean number correct) |
14.7 ± 4.7 |
| Diabetes Knowledge Test (Mean % correct) |
63.8 ± 20.5 |
| Diabetes Fatalism | 57.2 ± 8.0 |
| Social Support | 84.2 ± 20.1 |
| Diabetes Self-Care | |
| General diet | 4.6 ± 2.1 |
| Specific diet | 4.5 ± 1.6 |
| Exercise | 2.7 ± 2.4 |
| Blood sugar testing | 4.7 ± 2.4 |
| Foot care | 5.2 ± 2.3 |
| Smoking | 1.1 ± 2.2 |
| Glycemic Control | |
| Hemoglobin A1c | 7.6 ± 1.9 |
3.2. Diabetes self-care behavior
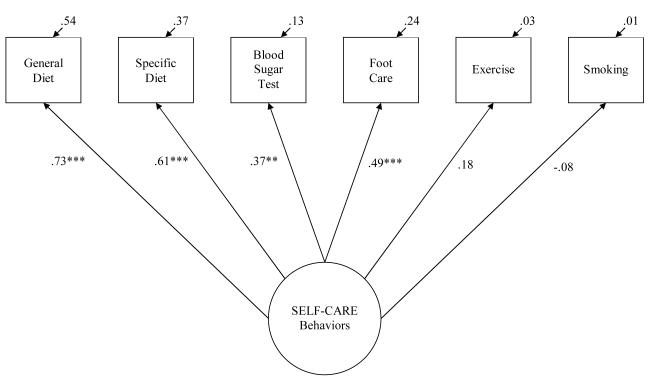
The estimated confirmatory factor analytic model (CFA) with parameters and tests of significance of factor loadings appears in Figure 1. This measurement model demonstrated good data fit, χ2(9, N = 130) = 15.60, p = 0.08, CFI = 0.90, RMSEA = 0.07 (90% CI: 0.00 - 0.14). No multivariate outliers or large residuals based on the items and replicated covariance matrices were observed. The correlation table was examined for multicollinearity and no relationships were above 0.90. Diabetes self-care behavior (SDSCA) loaded significantly onto the measured variables: specific diet (0.61, p<0.001), general diet (0.73, p<0.05), foot care (0.49, p<0.001), and blood sugar testing (0.36, p<0.01). Factor loadings onto exercise and cigarette smoking were not significant; therefore they were omitted from the measurement model nested in the subsequent structural equation model (SEM).
Figure 1.
Confirmatory Factor Analysis of Diabetes Self-Care Behaviors (Measurement Model).
Note: Overall model fit, χ2(9, N = 130) = 15.60, p = 0.08, CFI = 0.90, RMSEA = 0.07 (90% CI: 0.00 - 0.14). For tests of significance of individual factor loadings, *p < 0.05, **p < 0.01 and ***p < 0.001.
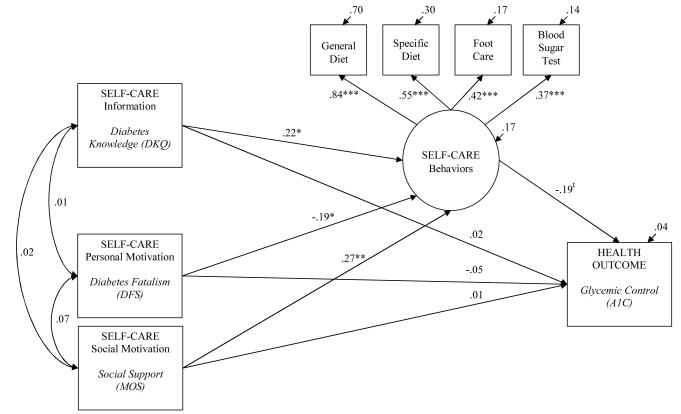
3.3. Validation of the IMB-DSC model
The estimated SEM with parameters and tests of significance of individual paths appears in Figure 2. The estimated model demonstrated good data fit, χ2(14, N = 130) = 17.92, p = 0.21, CFI = 0.95, RMSEA = 0.05 (90% CI: 0.00 - 0.10). As indicated in Figure 2, there were significant direct paths from diabetes knowledge (r=0.22, p<0.05), diabetes fatalism (r=−0.19, p<0.05), and social support (r=0.27 p<0.01) to diabetes self-care behaviors. Diabetes knowledge, diabetes fatalism, and social support were also unrelated, as indicated by non-significant co-variances in the model [27]. Thus, more diabetes knowledge, less diabetes fatalism, and more social support were independently associated with diabetes self-care behavior, explaining 17% of the variability in the diabetes self-care behavior score.
Figure 2.
Estimated Information—Motivation—Behavioral Skills model of Diabetes Self-care (Full).
Note: Coefficients are standardized path coefficients. Overall model fit, χ2(14, N = 130) = 17.92, p = 0.21, CFI = 0.95, RMSEA = 0.05 (90% CI: 0.00 - 0.10). For tests of significance of individual paths, tp = 0.09, *p < 0.05, **p < 0.01 and ***p < 0.001.
To corroborate the hypothesis that diabetes knowledge, diabetes fatalism, and social support would be solely related to behavior, and not A1C, we included paths to A1C that were hypothesized to be non-significant. Consistent with predictions, diabetes knowledge, diabetes fatalism, and social support were not significantly related to A1C. Instead, these variables appeared indirectly related to A1C through relations with diabetes self-care behavior. While diabetes self-care behavior was not significantly related to A1C, the path coefficient was in the predicted direction (r=−0.19, p = 0.09), suggestive of an association between diabetes self-care behavior and lower A1C values (i.e., glycemic control).
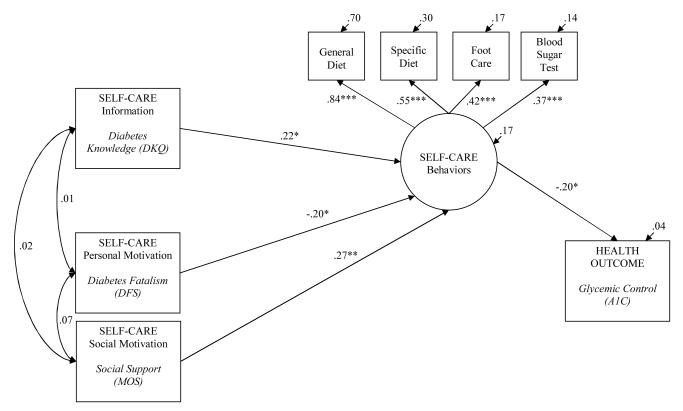
In an effort to generate a more parsimonious model, a trimmed version of the above model was estimated. The trimmed model included all significant paths from the initial model, omitting all non-significant paths. The trimmed model with structural parameters and tests of significance of individual paths appears in Figure 3. The estimated model demonstrated good data fit, χ2(17, N = 130) = 18.27, p = 0.37, CFI = 0.98, RMSEA = 0.02 (90% CI: 0.00 - 0.08). Furthermore, the path from diabetes self-care behavior to glycemic control reached statistical significance, such that performing diabetes self-care behaviors was associated with lower A1C values (r=−0.20, p<0.05),. The chi-square difference test between the trimmed and full models, χ2(3, N = 130) = 0.35, was non-significant, permitting the retention of the trimmed version as the final model.
Figure 3.
Estimated Information—Motivation—Behavioral Skills model of Diabetes Self-care (Trimmed).
Note: Coefficients are standardized path coefficients. Overall model fit, χ2(17, N = 130) = 18.27, p = 0.37, CFI = 0.98, RMSEA = 0.02 (90% CI: 0.00 - 0.08). For tests of significance of individual paths, *p < 0.05, **p < 0.01 and ***p < 0.001.
4. Discussion and Conclusion
4.1 Discussion
The Information—Motivation—Behavioral Skills (IMB) model of health behavior change [18, 20, 28] was used to conceptualize the determinants of diabetes self-care behavior and glycemic control in a sample of patients with T2DM. Consistent with the IMB model, having more information (greater diabetes knowledge), having more personal motivation (less diabetes fatalism), and having more social motivation (more social support) was associated with performing diabetes self-care behavior; and behavior was the sole predictor of glycemic control. A basic tenet of the IMB model is that behavioral performance is a function of the extent to which someone is well informed, and/or motivated to perform a behavior (e.g., has positive attitudes towards the behavior or outcome, and social support for the behavior). In this way, information and motivation are assumed to work through behavior to impact health, but are not direct predictors of health, per se.
While these findings highlight the importance of information, personal motivation, and social motivation for promoting diabetes self-care behavior, additional research is needed to explore the role of behavioral skills -- a fundamental prerequisite to behavioral performance. In other chronic disease contexts, behavioral skills have mediated the relationship between information and behavior, and motivation behavior [18, 27]. Thus, the inclusion of behavioral skills in future analyses will allow for understanding the totality of the IMB model in diabetes.
At this time, our results suggest that the IMB model’s information and motivation determinants of behavior are well positioned to explain the sample data. Diabetes self-care information and motivation were associated with behavior, and behavior was linked to lower A1C levels. These findings build support for the utility of the IMB model in organizing core determinants of diabetes self-care behavior, and suggest directions for IMB-model based interventions, where information and motivation are formally targeted through behavioral intervention strategies.
There are limitations to this study that should be acknowledged. First, we were unable to explore the role of moderators (e.g., literacy level, race) in the evaluated models due to a restricted sample size. Our results speak most clearly to the population under study, and should be replicated in different patient groups. Secondly, although the IMB model proposes causal relationships between information, motivation, and diabetes self-care behavior, the current study measured these constructs cross-sectionally, and thus can most appropriately speak to associations between constructs observed at a single point in time, not causality. Future research should be conducted to investigate the longitudinal effects of information and motivation on changes in diabetes self-care behaviors. In addition, future work should be guided by data that includes all the relevant constructs of the IMB model. This will provide a more comprehensive understanding of the elements that should be incorporated in future diabetes self-care interventions.
4.2 Conclusion
An accumulation of evidence is needed to allow for the identification of critical targets for diabetes self-care interventions for different populations. The present results suggest that theory-based interventions might benefit by targeting improvements in information, and personal and social motivation for diabetes self-care behaviors linked to clinical outcomes in other research. Future qualitative and quantitative research to determine the kinds of information and motivation that may be most influential to health behavior adoption is needed.
In conclusion, this study shows that consistent with the IMB model, information, personal motivation, and social motivation are important critical prerequisites to performing self-care behaviors in diabetes. Specifically, having more diabetes knowledge (information), having less diabetes fatalism (personal motivation), and having social support (social motivation) was associated with performing diabetes self-care behaviors; and these behaviors were directly linked to glycemic control.
4.3 Practice implications
In keeping with the current trend toward theory-based diabetes education, this study provides empirical support for the Information-Motivation-Behavioral Skills (IMB) model of health behavior change as an appropriate, comprehensive health behavior change framework for diabetes self-care. The findings characterize the key elements of diabetes self-management and indicate that in addition to knowledge, diabetes education programs should to target personal and social motivation effect behavior change.
Our results also lend support to the growing body of literature and recommendations of tailoring health promotion interventions to the knowledge and motivation needs of patients [29]. Based on the findings of this study and consistent with the IMB model, providers and educators need to first be aware of patients’ levels of knowledge and motivation and then tailor educational programs accordingly. Such interventions are likely to be more effective at producing behavior change than ad-hoc, knowledge-based programs alone.
Acknowledgements
Dr. Osborn is supported by a Diversity Supplement Award (NIDDK P60DK020593-S302).
References
- 1.U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: 2008. National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2007. [Google Scholar]
- 2.The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. The New England journal of medicine. 1993;329(14):977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 3.Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):854–865. [PubMed] [Google Scholar]
- 4.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):837–853. [PubMed] [Google Scholar]
- 5.Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes care. 2001;24(3):561–587. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 6.O’Connor PJ, Rush WA, Davidson G, Louis TA, Solberg LI, Crain L, Johnson PE, Whitebird RR. Variation in quality of diabetes care at the levels of patient, physician, and clinic. Preventing chronic disease. 2008;5(1):A15. [PMC free article] [PubMed] [Google Scholar]
- 7.Tuerk PW, Mueller M, Egede LE. Estimating physician effects on glycemic control in the treatment of diabetes: methods, effects sizes, and implications for treatment policy. Diabetes care. 2008;31(5):869–873. doi: 10.2337/dc07-1662. [DOI] [PubMed] [Google Scholar]
- 8.Nwasuruba C, Khan M, Egede LE. Racial/ethnic differences in multiple self-care behaviors in adults with diabetes. Journal of general internal medicine. 2007;22(1):115–120. doi: 10.1007/s11606-007-0120-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nwasuruba C, Osuagwu C, Bae S, Singh KP, Egede LE. Racial differences in diabetes self-management and quality of care in Texas. Journal of diabetes and its complications. 2009;23(2):112–118. doi: 10.1016/j.jdiacomp.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, Maryniuk M, Peyrot M, Piette JD, Reader D, et al. National standards for diabetes self-management education. Diabetes care. 2009;32(Suppl 1):S87–94. doi: 10.2337/dc08-S087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fisher JD, Fisher WA. The information-motivation behavioral skills model. In: RJ D, RA C, MC K, editors. Emerging theories in health promotion practice and research: strategies for improving public health. Jossey-Bass, Inc; Indianapolis, IN: 2002. [Google Scholar]
- 12.Fisher JD, Fisher WA. Theoretical approaches to individual-level change. In: Peterson JL, DiClemente RJ, editors. Handbook of HIV prevention. Kluwer Academic/Plenum Press; New York: 2000. pp. 3–55. [Google Scholar]
- 13.Fisher WA, Fisher JD, Harman J. The Information-Motivation-Behavioral Skills Model: A general social psychological approach to understanding and promoting health behavior. In: Suls J, Wallston KA, editors. Social psychological foundations of health and illness. Blackwell; Malden, MA: 2003. pp. 82–106. [Google Scholar]
- 14.Garcia AA, Villagomez ET, Brown SA, Kouzekanani K, Hanis CL. The Starr County Diabetes Education Study: development of the Spanish-language diabetes knowledge questionnaire. Diabetes care. 2001;24(1):16–21. doi: 10.2337/diacare.24.1.16. [DOI] [PubMed] [Google Scholar]
- 15.Egede LE, Ellis C. Health-related quality of life and glycemic control in adults with type 2 diabetes. Diabetes. 2008;57(Suppl 1: A244) [Google Scholar]
- 16.Sherbourne CD, Stewart AL. The MOS social support survey. Social science & medicine (1982) 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 17.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes care. 2000;23(7):943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 18.Fisher JD, Fisher WA, Amico KR, Harman JJ. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychol. 2006;25(4):462–473. doi: 10.1037/0278-6133.25.4.462. [DOI] [PubMed] [Google Scholar]
- 19.Suls Jerry, Wallston Kenneth A. Fisher WA, Fisher JD, Harman J, editors. The information-motivation-behavioraI skills model: A general social psychological approach to understanding and promoting health behavior. 2003.
- 20.Fisher WA, Schachner H. Self-monitoring of blood glucose in diabetic children and adolescents--barriers, behaviors, and the search for solutions. US Endocrinology. in press. [Google Scholar]
- 21.Kline R. Principles and Practice of Structural Equation Modeling. 2nd edn Guilford; New York: 2004. [Google Scholar]
- 22.Loehlin JC. Latent Variable Models: An Introduction to Factor, Path, and Structural Analysis. Lawrence Erlbaum Associates; Hillsdale, NJ: 1992. [Google Scholar]
- 23.Browne MW, Cudeck RI. Alternative ways of assessing model fit. In: Bollen K, Long K, editors. Testing Structural Equation Models. Sage; Newbury Park, CA: 1993. pp. 136–162. [Google Scholar]
- 24.Steiger JH. Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research. 1990;25(2):173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- 25.Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 26.MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1:130–149. [Google Scholar]
- 27.Amico KR, Barta W, Konkle-Parker DJ, Fisher JD, Cornman DH, Shuper PA, Fisher WA. The information-motivation-behavioral skills model of ART adherence in a Deep South HIV+ clinic sample. AIDS and Behavior. 2009;13(1):66–75. doi: 10.1007/s10461-007-9311-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111(3):455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- 29.Osborn CY, Fisher JD. Diabetes education: Integrating theory, cultural considerations, and individually tailored content. Clinical Diabetes. 2008;26(4):148–150. [Google Scholar]