Abstract
Background
Blood pressure (BP) control remains elusive for many Americans. Although home health nurses are uniquely positioned to help vulnerable individuals achieve BP control, hypertension (HTN) management has not been a high priority in post-acute care.
Objective
To examine the effects of two home-based interventions designed to improve BP outcomes among high-risk African-American patients.
Design
Cluster randomized controlled trial.
Participants
A total of 845 newly admitted patients with uncontrolled HTN (JNC7 stages 1 or 2).
Interventions
The “basic” intervention delivered key HTN information to clinicians and patients, and a home BP monitor to patients, while the patients received usual post-acute care. The “augmented” intervention provided more intensive and extensive HTN information, monitoring and feedback for 3 months beyond the index home care admission.
Measures
Primary: BP control. Secondary: reductions in mmHG SBP and DBP, improvements in proportions improving JNC7 stage or achieving clinically meaningful reductions in SBP and DBP.
Methods
Multivariate regression models.
Key Results
The basic intervention produced no significant BP improvements; the augmented intervention significantly improved stage 2 patients’ outcomes. Among stage 2 patients, the augmented intervention increased BP control by 8.7 percentage points relative to usual care (8.9% vs. 17.6%; p = 0.01), yielded an 8.3 mmHG relative reduction in SBP (p = 0.01), and increased the proportion achieving at least a 20 mmHG reduction in SBP by 16.4 percentage points (p = 0.01).
Conclusion
Among stage 2 patients, a nurse-led intervention providing additional HTN medication review and patient self-management support during the 3-month post-acute care period yielded significant improvements in 3-month BP control, plus improvements in secondary BP outcomes.
Key words: hypertension, blood pressure, home health care, African American
INTRODUCTION
Conclusive evidence demonstrates that tightly controlled medication regimens in conjunction with appropriate dietary and lifestyle counseling can dramatically improve blood pressure (BP) control1. However, BP control remains elusive for many Americans2, and racial disparities persist3. Blacks have disproportionately high rates of uncontrolled hypertension (HTN)4,5, HTN-related heart disease and hypertensive nephropathy, as well as stroke, heart failure, and end-stage renal disease6. Moreover, the death rate from uncontrolled HTN is nearly three times as high among blacks as whites7.
This paper reports on results of a three-arm community-located randomized controlled trial (RCT), which builds on earlier studies showing that multifaceted interventions with reminder systems and team-based care hold promise for improving BP control8. While most studies have been conducted in physician offices, clinics, or pharmacies9, our focus is on high-risk patients receiving home-based post-acute care. We report the 3-month effectiveness and costs, relative to usual home care, of a “basic” and an “augmented” intervention aimed at lowering BP and improving BP control in a low-income, chronically ill population of black patients who entered home health care with uncontrolled HTN. The “basic” intervention delivered two e-mails with HTN-specific detailed recommendations to the patient’s home care nurse, plus a BP monitor and HTN guide to the patient. The “augmented” intervention incorporated all basic intervention components and, additionally, employed a study nurse and health educator to provide more extensive information and feedback to patients and clinicians.
A fundamental goal of home health care is to improve the management and outcomes of at-risk patients with multiple comorbidities and complex care requirements. Nationally, HTN is one of the top five diagnoses of home care patients10; however, BP control has not been a high priority in the home care setting. The major aim of this study was to answer the question: Can BP control in a high-risk black home care population be improved through organizationally feasible interventions designed to effect changes in routine post-acute care delivery?
METHODS
The study was approved by the Institutional Review Boards at the Visiting Nurse Service of NY and the Medical College of Wisconsin. The trial was registered in http://clinicaltrials.gov/ (NCT00139490) and monitored by a Data Safety and Monitoring Board11.
Setting
The study was conducted in an urban, non-profit, Medicare-certified home health organization that employed over 2,000 nurses and served over 100,000 patients in 2009. HTN was the patients’ most frequent primary or secondary admission diagnosis.
Nurse and Patient Participants
All field nurses in the agency’s main metropolitan area regions were eligible for the study. The patient population consisted of black, English-speaking patients aged 21 to 80, who had uncontrolled HTN determined by a primary, secondary, or tertiary admission diagnosis of HTN (ICD9-CM401, 402, 403, or 404) in the electronic health record (EHR) and a BP at the time of the study recruitment interview of ≥140 mmHg systolic (SBP) and/or ≥90 mmHg diastolic (DBP); (≥130 mmHg SBP and/or ≥80 mmHg DBP for patients with diabetes or kidney disease). An in-home recruitment interview was conducted by trained interviewers using a Microlife Model 3AA1-2, an automated device validated using criteria from the British Hypertension Society. The average of three readings determined study eligibility. Excluded were: patients with a kidney transplant, end-stage renal disease, severe heart failure, dementia, organic brain disorder, or other cognitive impairment; those on dialysis; and patients whose baseline BP reading could not be obtained due to arm size.
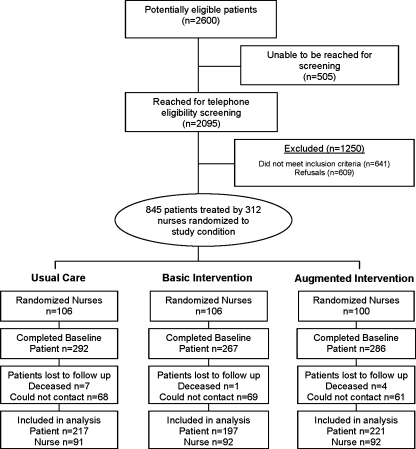
Randomization
After the home care nurse completed the patient’s usual care admission assessment, a computerized algorithm developed by project staff identified nurses whose patients met the study screening criteria and followed a random table algorithm to assign nurses to one of the study groups. A nurse’s initial random assignment to a group determined the status for all of her new patients (Fig. 1). While nurses were randomly assigned to study groups, random assignment of patients to nurses was not feasible because the study organization routinely assigns patients to a specific nurse based on factors designed to promote operational efficiency and care continuity (patient residence and a nurse’s overall caseload). Operations staff, blinded to the study, thus assigned patients to nurses according to these observable, exogenous criteria, which were controlled for in the study’s analyses.
Figure 1.
Consort diagram.
Usual Care
All patients received usual post-acute home care, consisting of a uniform clinical and functional assessment; medication review and reconciliation; a plan of care (signed by the patient’s physician); patient/family education, monitoring, and tailored hands-on care. Usual care nurses also received, as did all eligible nurses prior to randomization, a brief e-mail with a link to the JNC7 report.
Interventions
Basic Intervention Home care nurses in the basic intervention group received an automated e-mail targeted to the specific HTN patient shortly after the patient had been interviewed and enrolled in the study. The message relayed information on nursing-specific practices required to support JNC7 recommendations and a weblink to the guidelines. A second e-mail, sent 7 days later, provided information on the “5 A” model for promoting patient self-management12. Patients in the basic intervention group received the JNC7 patient guide “Lowering your Blood Pressure,” a home BP monitor, a BP log, and recommendations to record BP regularly and share the results with their home care nurse and PCP.
Augmented Intervention The augmented intervention incorporated all home care nurse and patient components of the basic intervention. Additionally, it deployed a study-trained “HTN support” nurse and health educator who used explicit protocols to help patients strengthen their self-management skills, adhere to recommended medication and behavioral regimens, and communicate more effectively with their PCP. After enrollment, the HTN support nurse conducted a comprehensive, in-home HTN-focused assessment and medication review, formulated collaborative self-management goals with the patient, and introduced an interactive workbook with HTN information and tools to be used throughout the intervention period. During subsequent biweekly phone counseling sessions over a 12-week period, the support team regularly reviewed the patient’s BP log and communicated, as needed, with the patient’s home care nurse and/or PCP to consider medication adjustments.
Outcome Measures
BP control, determined according to JNC7 guidelines by BP readings taken at the baseline and 3-month in-home interviews conducted by trained, blinded interviewers, was the primary outcome. Three secondary patient-level outcomes were examined: (1) systolic or diastolic BP at 3 months; (2) HTN stage at 3 months, a binary variable indicating whether the patient’s HTN stage was improved relative to baseline (improved = stage 2 to 1 or to BP control; or 1 to BP control); and (3) achievement of a clinically meaningful reduction in SBP or DBP, two binary variables indicating whether the patient’s BP at 3 months was reduced by at least 20 mmHg SBP or 10 mmHg DBP relative to baseline levels. Change in HTN stage was selected as an outcome because JNC7 treatment recommendations vary by BP stage. Achievement of a clinically meaningful reduction in SBP or DBP was selected because each increment of 20 mmHg in SBP or 10 mmHg in DBP has been estimated to double the risk of CVD across a wide BP range13,14.
Two measures of cost also were examined: (1) intervention, home care, and outpatient costs, and (2) overall health care-related costs, which included, in addition to intervention and outpatient costs directly affected by the intervention, resource costs associated with patient’s self-reported use of hospital and emergency department (ED) services during the study period. Medical services were valued using published data based on CMS’s average Medicare payment (or provider charges) for each service type.
Statistical Analyses
Sample size determination was based on the formulae presented in Cohen15. A complete follow-up sample size of 525 patients, divided roughly equally across groups, was estimated to be required to yield the desired level of precision (>80% power, alpha = 0.05) for detecting moderate-to-large (>25%) improvements in BP control among treatment group subjects relative to usual care patients. Sample size requirements were determined based on treatment-control differences obtained via regression equations, assuming a total variance explained of 0.35 and clustering/design effect of 0.10. Based on conservative estimates of longitudinal attrition, a total of 845 patients were recruited.
A probit specification was used to model treatment effects on binary dependent variables such as achieving BP control (primary outcome). Ordinary least squares was used to analyze continuous dependent variables (e.g., mmHg systolic and diastolic BP). Analyses were conducted for the overall sample as well as stratified by the subgroup of patients with stage 2 HTN at baseline. In all models, robust standard errors were computed to account for design clustering. Given that randomization occurred at the nurse rather than at the patient-level, in addition to group membership, all multivariate analyses controlled for characteristics that might influence patient assignment to a specific nurse or confound the relationship between interventions and patient-level outcomes. These included: patient age >65 years old and poverty status, as proxied by Medicaid enrollment; baseline measures of patient’s comorbidity, diagnosis of diabetes, systolic and diastolic BP; as well as an indicator of hospitalization in the 2 weeks preceding home health admission, borough of residence, and the nurse’s caseload. Given the inherent difficulty in interpreting nonlinear coefficients, the magnitude of the intervention effects was estimated by comparing regression adjusted outcomes (or probabilities) for the three intervention groups. All analyses were conducted using SAS 11 and Stata 10.0 statistical software.
RESULTS
Sample Characteristics
Figure 1 shows the flow of participants in the study. Of the 2,095 potentially eligible patients who were reached for screening, 641 (30.6%) did not meet inclusion criteria, and 609 (29%) declined to participate, yielding a sample of 845 enrolled patients corresponding to 312 randomized nurses. Our analysis focuses on the group of 635 patients with complete baseline and 3-month interview data.1 These patients were treated by 275 home health nurses who treated an average of 4 study patients each (mean = 3.8, SD = 2.6; range: 1–12). Correlation among patients assigned to the same nurse was 0.08.
Table 1 presents selected socio-demographic and health characteristics of our sample. There were no significant differences between enrolled and 3-month study participants with respect to socio-demographic, health or BP characteristics. The mean age of subjects was approximately 65 (range: 29–80 years); about two-thirds were women. Nearly half (45%) were poor enough to qualify for Medicaid benefits. Mean systolic BP at baseline was 155.4 mmHg (SD = 20.6); mean diastolic BP was 87.2 mmHg (SD = 14.1). Although there were no marked differences in comorbidity score or mean baseline systolic and diastolic BP among the three groups, group members differed by the proportion of persons aged 65 or older, gender, Medicaid enrollment, diabetes, and proportion of persons with severe uncontrolled HTN (JNC7 stage 2).
Table 1.
Key Sociodemographic and Health Characteristics of Study Patients, Overall and by Randomization Status
| Enrolled (N = 845) | Analysis sample (N = 635) | Usual care (N = 217) | Basic intervention (N = 197) | Augmented intervention (N = 221) | |
|---|---|---|---|---|---|
| N (%) or mean ± standard deviation | |||||
| Socio-demographic characteristics | |||||
| Age | |||||
| Age | 64.3 ± 10.9 | 64.7 ± 10.6 | 64.3 ± 10.5 | 65.7 ± 10.1 | 64.2 ± 11.1 |
| 65+ | 456 (54) | 343 (54) | 113 (52) | 120 (61)* | 113 (51)† |
| Female | 556 (66) | 420 (66) | 137 (63) | 126 (64) | 155 (70)* |
| Medicaid | 372 (44) | 286 (45) | 106 (49) | 85 (43)* | 97 (44 ) |
| Baseline health status | |||||
| Comorbidity score, mean | 3.78 ± 2.80 | 3.73 ± 2.78 | 3.61 ± 2.76 | 3.67 ± 2.64 | 3.90 ± 2.9 |
| Diabetes | 499 (59) | 375 (59) | 115 (53) | 124 (63)* | 133 (60) |
| Blood pressure status at baseline | |||||
| Overall | |||||
| Systolic BP, mean mmHg | 155.49 ± 20.4 | 155.4 ± 20.6 | 156.1 ± 20.2 | 155.9 ± 21.7 | 154.3 ± 20.1 |
| Diastolic BP, mean mmHg | 87.3 ± 13.0 | 87.2 ± 14.1 | 88.1 ± 16.0 | 86.7 ± 13.9 | 86.8 ± 12.2 |
| JNC7 stage 2 | 456 (54) | 336 (53) | 117 (54) | 109 (55) | 108 (49)*, † |
| Systolic BP among stage 2, mean mmHg | 168.4 ± 18.5 | 168.8 ± 18.7 | 168.7 ± 18.5 | 169.1 ± 19.8 | 168.6 ± 18.2 |
| Diastolic BP among stage 2, mean mmHg | 92.5 ± 13.2 | 92.9 ± 15.0 | 93.4 ± 18.2 | 92.3 ± 14.1 | 92.8 ± 11.9 |
*Significantly different from usual care group at the p < 0.05 level (two-sided test)
†Significantly different from basic intervention group at the p < 0.05 level (two-sided test)
Impact of Interventions on BP Outcomes
Table 2 presents unadjusted measures of BP control and systolic/diastolic BP at 3 months. Just above 1/5 of patients in each arm achieved BP control at 3 months, with no significant differences across groups. Although mean SBP was 3.3 points lower among augmented patients relative to usual care subjects, differences across the two groups were not significant at conventional levels. The augmented intervention, however, did result in significant relative improvements among patients with stage 2 HTN at baseline. These patients were significantly more likely to achieve BP control than usual care patients (16% vs 10%, p < 0.05). In addition, their mean SBP was significantly lower at 3 months relative to usual care stage 2 patients (-8 mmHg, p < 0.05).
Table 2.
Unadjusted Key Blood Pressure Outcomes at 3-Month Follow-up
| Usual care | Basic intervention | Augmented intervention | |
|---|---|---|---|
| n (%) or mean ± standard deviation | |||
| Proportion achieving BP control | |||
| Overall | 48 (22) | 41 (21) | 55 (25) |
| JNC7 stage 2 at baseline | 22 (10) | 26 (13) | 35 (16)* |
| Systolic BP, mean mmHg | |||
| Overall | 151.7 ± 24.0 | 151.3 ± 24.8 | 148.4 ± 24.5 |
| JNC7 stage 2 at baseline | 160.5 ± 25.3‡ | 158.7 ± 25.4‡ | 152.5 ± 26.2*,†,‡ |
| Diastolic BP, mean mmHg | |||
| Overall | 85.3 ± 14.0 | 84.2 ± 15.0 | 84.0 ± 13.9 |
| JNC7 stage 2 at baseline | 87.3 ± 14.9‡ | 88.0 ± 14.9‡ | 85.5 ± 14.2‡ |
*Significantly different from usual care group at the p < 0.05 level (two-sided test)
†Significantly different from basic intervention group at the p < 0.05 level (two-sided test)
‡Significantly lower than baseline measure at the p < 0.05 level (one-sided test)
Table 3 reports the regression-adjusted effects of the interventions on patients’ primary outcome (HTN control) and all secondary outcomes (SBP and DBP, improving HTN stage, and experiencing a clinically meaningful reduction in SBP or DBP). Relative to usual care, the basic intervention demonstrated no significant improvements in patient outcomes overall or by HTN severity, nor did the augmented intervention result in statistically significant improvements for the entire sample relative to usual care, despite marginally significant relative improvements for several outcomes.
Table 3.
Adjusted Treatment Effects on HTN Outcomes, Overall and for Patients with Severely Uncontrolled HTN at Baseline
| Usual care | Basic intervention | Augmented intervention | |||
|---|---|---|---|---|---|
| Primary outcome | |||||
| Achieved BP control, % | |||||
| Overall | 20.7 | 23.2 | 2.5 [0.53] | 25.2 | 4.5 [0.23] |
| JNC7 stage 2 at baseline | 8.9 | 13.4 | 4.5 [0.22] | 17.6 | 8.7 [0.04] |
| Secondary outcomes | |||||
| Systolic BP, mmHg | |||||
| Overall | 151.6 | 149.8 | -1.8 [0.48] | 147.8 | -3.8 [0.12] |
| JNC7 stage 2 at baseline | 160.8 | 158.5 | -2.3 [0.49] | 152.5 | -8.3 [0.01] |
| Diastolic BP, mmHg | |||||
| Overall | 84.6 | 84.0 | -0.6 [0.71] | 83.3 | -1.3 [0.37] |
| JNC7 stage 2 at baseline | 86.9 | 88.4 | 1.5 [0.43] | 85.5 | -1.4 [0.45] |
| Experienced clinically meaningful reduction in BP, % | |||||
| Systolic | |||||
| Overall | 22.6 | 26.6 | 4.0 [0.31] | 28.7 | 6.1 [0.11] |
| JNC7 stage 2 at baseline | 30.1 | 37.0 | 6.9 [0.24] | 46.5 | 16.4 [0.01] |
| Diastolic | |||||
| Overall | 28.0 | 33.5 | 5.5 [0.21] | 35.2 | 7.2 [0.08] |
| JNC7 stage 2 at baseline | 33.4 | 34.5 | 1.1 [0.85] | 43.0 | 9.6 [0.10] |
| Improved HTN stage, % | |||||
| Overall | 35.7 | 36.4 | 0.7 [0.87] | 39.6 | 3.9 [0.38] |
| JNC7 stage 2 at baseline | 36.3 | 38.9 | 2.6 [0.67] | 46.8 | 10.5 [0.09] |
Notes: P-values are in brackets. Adjusted probabilities are calculated based on underlying coefficients from multivariate models that control for socio-demographic characteristics of the patient (age, Medicaid enrollment); baseline measures of patients’ BP and health status (presence of diabetes, number of other co-morbidities); and the provider nurse’s caseload and patient borough of residence at the time of the visit. Standard errors have been adjusted to account for clustering effects (i.e., multiple observations on patients for a given nurse)
In contrast, among JNC7 stage 2 patients, the augmented intervention resulted in superior outcomes for all but one outcome measure (mmHG DBP). Stage 2 patients in the augmented group were 8.7 percentage points more likely than those in usual care to achieve BP control (adjusted probability = 17.6% versus 8.9%, respectively, p = 0.04). They also experienced a reduction of 8.3 mmHg in their systolic BP relative to usual care subjects (p = 0.01) and were significantly more likely to achieve a clinically meaningful reduction in systolic BP of 20 or more mmHg relative to their baseline levels (+16.4 percentage points, p = 0.01). Although less precisely estimated, the proportion of stage 2 patients experiencing clinically meaningful reductions in diastolic BP was 9.6 percentage points (or 29%) greater in the augmented group relative to usual care group subjects (p = 0.10). Finally, stage 2 patients in the augmented group also were more likely than those in the usual care group to experience reductions in BP consistent with improved HTN stage (10.5 percentage points, p = 0.09). This improvement represented a 28% gain over usual care patients during the 3-month period.
Of the control variables included in the analyses, only baseline BP, a diagnosis of diabetes and age were consistently significant across outcomes. Regardless of intervention group, the higher the person’s baseline BP was, the greater the likelihood of experiencing a clinically meaningful reduction in SBP or DBP, but the lower the likelihood of actually achieving BP control. Having a diagnosis of diabetes and being elderly made it less likely that a patient experienced improvements in BP outcomes.
Cost Analysis
Outpatient (including intervention) costs among treatment subjects were about 19% (p = 0.04) and 24% higher (p = 0.01) among basic and augmented group patients than comparable costs associated with usual care of $3,654. The same pattern held true for patients with stage 2 BP at baseline. However, once inpatient and ED use costs were taken into account, differences between groups were small and not statistically significant, suggesting lower use of more costly, hospital-based services among treatment groups when compared to usual care subjects. Differences in mean overall health care costs ranged from $1,079 (p = 0.11; augmented versus usual care, overall sample) to $295 (p = 0.35; basic versus usual care, stage 2 patients).
DISCUSSION
We examined the effects of two interventions—a basic information-based intervention and an augmented, nurse-led intervention—designed to improve patients’ BP outcomes through changes in the delivery of home-based post-acute care. The study demonstrated that the nurse-led intervention, providing additional medication review and patient self-management support during the 3-month post-acute care period, significantly improved BP control in a high-risk, low income black population admitted to care with JNC7 stage 2 HTN. Relative to usual care, the augmented intervention dramatically increased the probability of 3-month BP control (17.6 vs 8.9% adjusted control) among stage 2 patients. The augmented intervention also yielded an 8.3-mmHg relative reduction in SBP and a 29% relative increase in the proportion of stage 2 patients achieving at least a 20 mmHg reduction in SBP.
The findings are particularly important given the HTN-related risk profile of the study population, all uncontrolled at baseline. National data show that BP control is especially problematic for blacks, women, persons aged 70 and over, individuals with diabetes, and those who have less than a high school education1,3,16. In this black study population, approximately a fifth were 75 or older17, 42% had less than a high school education, 45% had an annual income of $10,000 or less, 53% were JNC7 stage 2 at baseline, and 59% had diabetes. Our study thus focused on a much higher risk population than previous HTN interventions.
The finding of significant intervention effects solely among patients with severe uncontrolled HTN, although disappointing, is not surprising. The majority of community-based HTN intervention trials enroll provider and/or patient volunteers18, who may be more focused on or motivated to achieve BP control than participants in our study. Second, evidence suggests considerable provider inertia in adjusting BP medications among patients with lower disease severity19. Third, patients themselves may be less adherent to medications and more reluctant to seek adjustment or adopt therapeutic lifestyle changes when BP values are perceived as within an “acceptable range”20. Our approach of examining the interventions’ effectiveness by HTN severity, although initially unplanned, highlights the importance of targeting specific types of intervention to specific patient severity groups.
The study has several limitations. First, it is based on black patients served by a single, albeit large, home health organization providing care to an urban patient population that is poorer, less well educated, and more culturally diverse than the population typically served by post-acute home care organizations17. Generalizability of findings to other groups is thus unclear. Second, randomization occurred at the nurse rather than the patient level. Third, the study was powered to discern significant effects for all uncontrolled patients, while significant outcomes were limited to the patient subgroup with stage 2 HTN. Although ideally subgroup effects would have been incorporated in the study’s initial design, the baseline distribution of patients by stage was unavailable a priori and therefore could provide no guidelines for power analysis. Nevertheless, the sub-group effects were sufficiently robust to achieve statistical significance despite the smaller sample size. Lastly, the BP improvements reported here were measured at 3 months, and it is possible that the intervention’s effects may have dissipated over a longer time period21.
Home health patients are an especially high-risk group characterized by multiple comorbid conditions and medications22. Keeping abreast of evidence-based practices, supporting patients’ adherence to physician-prescribed medication regimens and appropriate lifestyle changes, and linking patients to other medical and community resources are central to the nurse’s role. However, the potential for improving HTN management for this chronically ill and costly population has not been exploited. The results reported here, however, demonstrate that augmenting home health care can significantly improve BP outcomes among black patients with severe uncontrolled HTN. The study’s cost findings suggest that in the short-term, such a home-based post-acute care intervention would be cost-neutral with respect to overall (inpatient + outpatient) costs, thus providing policy-relevant information for designing and targeting future transitional care demonstrations. These findings represent the first RCT-derived evidence estimating the effects of a transitional care intervention for post-acute home care patients otherwise at risk of “slipping through” the system with suboptimal BP management.
Acknowledgements
This work was supported by grant R01 HL078585 from the National Heart, Lung and Blood Institute (NHLBI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, And Blood Institute or the National Institutes of Health. The authors wish to acknowledge the significant contributions of the intervention staff involved in this project: Paula Wilson, Nicole Fraser and Sharon Browne-Isles and the programming support provided by Sridevi Sridharan.
Conflict of Interest None disclosed.
Disclosures The authors do not have any financial interests in the manuscript.
Footnotes
A standard concern in experiments with longitudinal follow-up is the potentially biasing effects of sample attrition. Multivariate results comparing patients lost to follow-up with those for whom complete data were obtained using baseline characteristics revealed no evidence of attrition bias in this sample.
NIH trial registry: NCT00139490
References
- 1.Cushman WC, Ford CE, Cutler JA, et al. Success and predictors of blood pressure control in diverse North American settings: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT) J Clin Hypertens (Greenwich). 2002;4(6):393–404. doi: 10.1111/j.1524-6175.2002.02045.x. [DOI] [PubMed] [Google Scholar]
- 2.Lloyd-Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA. 2005;294(4):466–472. doi: 10.1001/jama.294.4.466. [DOI] [PubMed] [Google Scholar]
- 3.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165(18):2098–2104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 4.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988-1994 and 1999-2004. Hypertension. 2008;52(5):818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- 5.Ostchega Y, Yoon SS, Hughes J, Louis T. Hypertension awareness, treatment, and control—continued disparities in adults: United States, 2005-2006. NCHS Data Brief No. 3. Hyattsville, Maryland: National Center for Health Statistics. 2008. [PubMed]
- 6.Douglas JG, Bakris GL, Epstein M, et al. Management of high blood pressure in African Americans: consensus statement of the Hypertension in African Americans Working Group of the International Society on Hypertension in Blacks. Arch Intern Med. 2003;163(5):525–541. doi: 10.1001/archinte.163.5.525. [DOI] [PubMed] [Google Scholar]
- 7.Lloyd-Jones D, Adams R, Carnethon M, et al. American Heart Association Statistics Committee and Stroke Statistics Committee. Heart disease and stroke statistics–2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119(3):e21–181. doi: 10.1161/CIRCULATIONAHA.108.191261. [DOI] [PubMed] [Google Scholar]
- 8.Carter BL, Ardery G, Dawson JD, et al. Physician and pharmacist collaboration to improve blood pressure control. Arch Intern Med. 2009;169(21):1996–2002. doi: 10.1001/archinternmed.2009.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dennison CR, Post WS, Kim MT, et al. Underserved urban African American men: hypertension trial outcomes and mortality during 5 years. Am J Hypertens. 2007;20(2):164–171. doi: 10.1016/j.amjhyper.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 10.NCHS. National Center for Health Statistics. National Home Health and Hospice Care Survey. Home Health Discharges February 2004. Downloaded from the web August 12, 2010: http://www.cdc.gov/nchs/data/nhhcsd/homecaredischarges00.pdf
- 11.Feldman PH, McDonald MV, Mongoven JM, Peng TR, Gerber LM, Pezzin LE. Home-based blood pressure interventions for blacks. Circ Cardiovasc Qual Outcomes. 2009;2(3):241–248. doi: 10.1161/CIRCOUTCOMES.109.849943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fiore MC, Bailey WC, Cohen SJ. Treating tobacco use and dependence: a clinical practice guideline. Rockville: US Department of Health and Human Services. A Public Health Service report; 2000. [Google Scholar]
- 13.Chobanian AV, Bakris GL, Black HR, et al. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 14.Lewington S, Clarke R, Qizilbash N, Peto R. Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/S0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 15.Cohen J. Statistical power analysis for the behavioral sciences. 2. New Jersey: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 16.Ostchega Y, Dillon CF, Hughes JP, Carroll M, Yoon S. Trends in hypertension prevalence, awareness, treatment, and control in older U.S. adults: data from the National Health and Nutrition Examination Survey 1988 to 2004. J Am Geriatr Soc. 2007;55(7):1056–1065. doi: 10.1111/j.1532-5415.2007.01215.x. [DOI] [PubMed] [Google Scholar]
- 17.McDonald MV, Pezzin LE, Peng TR, Feldman PH. Understanding the complexity of hypertensive African American home care patients: Challenges to intervention. Ethn Dis. 2009;19(2):148–153. [PMC free article] [PubMed] [Google Scholar]
- 18.Fahey T, Schroeder K, Ebrahim S. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2006(4):CD005182. [DOI] [PubMed]
- 19.Pavlik VN, Greisinger AJ, Pool J, Haidet P, Hyman DJ. Does reducing physician uncertainty improve hypertension control? Rationale and methods. Circ Cardiovasc Qual Outcomes. 2009;2(3):257–263. doi: 10.1161/CIRCOUTCOMES.109.849984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scisney-Matlock M, Bosworth HB, Giger JN, et al. Strategies for implementing and sustaining therapeutic lifestyle changes as part of hypertension management in African Americans. Postgrad Med. 2009;121(3):147–159. doi: 10.3810/pgm.2009.05.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bosworth HB, Olsen MK, Grubber JM, et al. Two self-management interventions to improve hypertension control: a randomized trial. Ann Intern Med. 2009;151(10):687–695. doi: 10.1059/0003-4819-151-10-200911170-00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murtaugh C, Peng T, Totten A, Costello B, Moore S, Aykan H. Complexity in geriatric home healthcare. J Healthc Qual. 2009;31(2):34–43. doi: 10.1111/j.1945-1474.2009.00017.x. [DOI] [PubMed] [Google Scholar]