Abstract
Purpose
The ferret cisplatin emesis model has been used for ~30 years and enabled identification of clinically used anti-emetics. We provide an objective assessment of this model including efficacy of 5-HT3 receptor antagonists to assess its translational validity.
Methods
A systematic review identified available evidence and was used to perform meta-analyses.
Results
Of 182 potentially relevant publications, 115 reported cisplatin-induced emesis in ferrets and 68 were included in the analysis. The majority (n = 53) used a 10 mg kg−1 dose to induce acute emesis, which peaked after 2 h. More recent studies (n = 11) also used 5 mg kg−1, which induced a biphasic response peaking at 12 h and 48 h. Overall, 5-HT3 receptor antagonists reduced cisplatin (5 mg kg−1) emesis by 68% (45–91%) during the acute phase (day 1) and by 67% (48–86%) and 53% (38–68%, all P < 0.001), during the delayed phase (days 2, 3). In an analysis focused on the acute phase, the efficacy of ondansetron was dependent on the dosage and observation period but not on the dose of cisplatin.
Conclusion
Our analysis enabled novel findings to be extracted from the literature including factors which may impact on the applicability of preclinical results to humans. It reveals that the efficacy of ondansetron is similar against low and high doses of cisplatin. Additionally, we showed that 5-HT3 receptor antagonists have a similar efficacy during acute and delayed emesis, which provides a novel insight into the pharmacology of delayed emesis in the ferret.
Keywords: Cisplatin, Emesis, Ferret, Meta-analysis, Systematic review, Ondansetron, 5-HT3 receptor antagonist, Granisetron, Tropisetron
Introduction
It is generally accepted that nausea and vomiting (emesis) are components of a protective mechanism by which the human body defends itself against ingested toxins. However, the emetic reflex can be triggered inappropriately, and nausea and vomiting are also relatively common side effects of drugs in current use (e.g. morphine, anti-cancer chemotherapy) as well as dose-limiting toxicities, which may limit the development of novel chemical entities intended for the treatment of a range of diseases (e.g. phosphodiesterase-IV inhibitors for the treatment of asthma [135]). The multi-system nature of the emetic reflex coordinated in the brainstem and the behavioural and sensory expression of nausea have meant that, to date, preclinical studies of the mechanisms involved and identification of novel anti-emetic agents have involved studies in whole animals (conscious, anaesthetised or decerebrate) [61]. Nausea and vomiting are particularly associated with the treatment of cancer by cytotoxic drugs (e.g. cisplatin), symptoms which patients find particularly distressing and impact upon compliance with treatment. In the absence of anti-emetic prophylaxis, cisplatin induces nausea and vomiting in virtually all patients [109]; the emetic response lasts up to 5 days on each cycle and is characterised by an intense acute phase lasting ~24 h and a less intense but more protracted delayed phase peaking during the period 48–72 h following the administration of cisplatin [72]. In the early 1980s, the ferret (Mustela putorius furo L.) was reported to develop an acute emetic response to high-dose cisplatin (8–10 mg kg−1) and was proposed as an alternative model to the dog, cat and monkey (commonly used at the time) to study cytotoxic drug-induced emesis and identify potential anti-emetic agents [40]. Subsequently, the acute cisplatin model was modified and the dose of cisplatin lowered to 5 mg kg−1 to investigate delayed emesis [114]. The ferret model of cisplatin-induced emesis was rapidly adopted for the investigation of new anti-emetic agents and was pivotal in establishing the anti-emetic efficacy of 5-hydroxytryptamine3 (5-HT3) [94] and tachykinin NK1 receptor antagonists [148], which are both currently in widespread use for the treatment of chemotherapy-induced nausea and vomiting [109].
The use and benefit of animal models in research is regularly questioned and anecdotal evidence or unsupported claims, as opposed to quantitative support, are too often used as justifications [88, 105]. There has recently been a growing interest in systematic reviews and meta-analyses to assess the validity of animal models (i.e. how preclinical research has informed clinical research) and their utility in drug discovery (i.e. evaluate data and inform the decision to carry out a clinical trial). The Nuffield Council for Bioethics [101] recommends that such reviews are undertaken to “evaluate more fully the predictability and transferability of animal models”. Such analyses also have implications for the application of the principles of the 3Rs (Replacement, Refinement, Reduction) to animal experimentation [61, 68] and should inform preclinical guidelines produced by regulators (e.g. [37]). Recently, systematic reviews and meta-analysis of animal models of stroke have been carried out. A retrospective study concluded that even though individual studies had reported beneficial effects of the calcium channel blocker nimodipine; overall, the preclinical data available were not conclusive [62], which is consistent with the fact that this type of drug was without effect in humans [63] and highlights the necessity of quantifying animal data adequately before starting clinical trials. Later studies assessed the preclinical evidence of the effect of potential treatments in experimental stroke and characterised their neuroprotective properties in order to identify research priorities [78–80].
The cisplatin-induced emesis ferret models provide a unique opportunity to assess the value of systematic reviews in specific areas, because the wealth of data available in this relatively circumscribed area allows assessment of two characteristics of a model: the response to cisplatin itself, and the anti-emetic potential of agents that are currently used in humans. The aim of this systematic review is twofold: firstly, this study intends to provide an objective measure of the characteristics of cisplatin-induced emesis in the ferret, in terms of the latency, magnitude (number of retches and vomits) and profile of the emetic response. Secondly, the effect of 5-HT3 receptor antagonists in the ferret model will be quantified; the present study will assess the efficacy of ondansetron against the acute phase of emesis; additionally, we will compare the overall effect of 5-HT3 receptors antagonists against the acute and delayed phases of emesis.
This paper is the first systematic review and meta-analysis covering a model of emesis and anti-emetics. It provides evidence, which supports the predictability of the model and identifies new features of the model not apparent from individual studies. Additionally, it shows the limitations of the model and identifies opportunities for enhanced animal welfare according to the principles of the “3Rs” formulated by Russell and Burch over 50 years ago [126].
Methods
Search strategy
Studies were identified from Pubmed (1974 to March 2007) and Embase (1980 to March 2007) using the combination of words: CISPLATIN and FERRET; hand searching of abstracts of scientific meetings and personal files. All references of newly identified publications were also screened until no further eligible references were found. Language was not restricted. Values for data expressed graphically were either requested from authors or measured from the graphs. Corresponding authors were also contacted to obtain data that was not reported clearly enough in their publications.
Inclusion criteria:
Report of cisplatin-induced emesis in the ferret
Emetic response documented, and quantified by at least one of the following: latency to onset of emesis (retching or vomiting), number of animals developing emesis, number of retches (R), vomits (V), retches and vomits (R+V) defined according to our definition and reported as mean only or mean ± SEM or SD, and number of ferrets per group.
Exclusion criteria:
Number of animals not stated
Emetic response investigated under anaesthesia
Emetic response not reported as the number of animals developing emesis, or mean latency, or mean number of retches and vomits compatible with the standard definition of emesis.
Emesis was defined as retching (i.e. rhythmic abdominal contractions against a closed glottis) and vomiting (i.e. rhythmic abdominal contractions associated with the oral expulsion of solid or liquid materials from the gastrointestinal tract) [14, 22, 89]. Reports stating this definition in their methods section were included in this study; if the definition was absent or unclear, evaluation of the results reported and their inclusion in this quantitative review were left to the judgement of the investigator and discussed with co-workers; reports were included:
If the same team had published other reports clearly stating this definition or a member of the team—most senior or corresponding author—was contacted to confirm the definition used to characterise emesis
If the report referred to publications clearly stating this definition
If the definition stated allowed the identification of the number of retches and/or vomits according to our definition.
The latency (time to onset of emesis) was a potential confounding factor as many publications reported the latency as a mean for all the animals in the groups, including those free of emesis, in which case the latency was taken as the total duration of the observation time. All latencies were recalculated as the mean latency to the first retch or vomit in animals that developed emesis only. The latency was either measured as the time to the first retch, the time to the first vomit or the time to the first emetic episode. All the latencies reported were included combined together, as it was considered that only a minimal period of time separates the first retch from the first vomit [144], a more rigid approach including only the studies with either one or the other measurement and excluding those reporting the latency to the first emesis or emetic episode would have induced a greater error.
Data extraction and analysis
Meta-analysis: the ferret model of cisplatin-induced emesis
The number of retches (R), vomits (V), retches + vomits (R+V) and/or latency data from control groups (i.e. animals that received no other drug than cisplatin or cisplatin and an inactive—i.e. non-emetogenic—vehicle) were extracted as mean, standard deviations (SD) and number of animals per group. Weighted mean and weighted mean of the SD were calculated and a one-way ANOVA was carried out to compare the onset of emesis following different doses of cisplatin. Unless stated, all results are reported as mean ± SD. In order to identify variables modulating the emetic response, subgroup analyses were carried out according to criteria such as the vehicle used, duration of the observation period, the mode of administration of cisplatin (i.v. or i.p.), the use of anaesthesia and the recovery time prior to the emetic challenge, the strain (fitch or albino), sex and origin of the ferrets. This analysis was only carried out on the most common doses of cisplatin used to induce acute (10 mg kg−1) and acute and delayed emesis in the ferret (5 mg kg−1); the two doses were treated separately. Weighted means and the weighted mean of the SDs were calculated and profiles of emesis were constructed with Graphpad Prism® version 5.0, Graphpad Software Inc., San Diego, USA. Differences were assessed by a one-way analysis of variance (ANOVA) or independent sample t tests as appropriate. Descriptive statistics and comparisons were carried out using SPSS® 14.00, SPSS Inc., Chicago, USA and CLINSTAT (M. Bland). Differences were considered statistically significant when P < 0.05.
Meta-analysis: the effect of anti-emetics
For the meta-analysis of the effects of anti-emetics, comparisons were only included if the effect of a prophylactic anti-emetic treatment was reported, the 3 outcomes measured were: the number of R+V, proportion of animals experiencing emesis and latency to the onset of emesis. To calculate the effect size and its 95% confidence interval for the continuous outcomes (i.e. R+V and latency), the mean outcome for the treatment group, and the SDs in treatment and control groups were expressed as a proportion of the outcome in the control group [80]. Actual data were used for dichotomous outcomes (i.e. the number of animals with emesis). When a control group was used to assess more than one treatment group, the number of animals in the control group was divided by the number of treatment groups and if needed, adjusted to the next integer. This methodology is consistent with what has been done in another meta-analysis of animal data in a model of stroke [80]. The effect of ondansetron was examined for each of the 3 outcomes; subgroup analyses were carried out depending on the dose of cisplatin and duration of the observation period, dose, timing and mode of administration of ondansetron, mode of administration of cisplatin, origin of the ferrets, and quality score of the study. Additional analyses examined the effects of 5-HT3 receptor antagonists on the latency to the onset of cisplatin (10 mg kg−1)-induced emesis and on the acute and delayed R+V induced by 5 mg kg−1 cisplatin (criteria for variation: individual compound). In the later analysis, comparisons on a given day were only included if the anti-emetic treatment started before or at the start of the 24-h period and was continued throughout the day.
Methodological quality of individual studies was assessed according to criteria chosen to evaluate the reliability of the data extracted. These criteria were: no duplicate publication identified—confirmed or suspected—, retch and vomit clearly defined or definition confirmed by authors, latency to the first retch or vomit given, SEM/SD given for the mean latency, number of retches and vomits or R+V given, SEM/SD given for the mean R+V, number of ferrets completely protected given (1 point per criterion fulfilled), origin, sex, strain and body weight of the ferrets given (1/2 point per criterion fulfilled). Each study was given a quality score out of a possible total of 9 points. The DerSimonian and Laird method was used to combine dichotomous (risk difference [RD]) and continuous data (weighted mean difference [WMD]). The random-effects model was chosen over the fixed effect assumption because it incorporates inter-study differences into the analysis of the overall treatment efficacy [28]. The data were analysed with Review Manager (RevMan. Version 5.0 for Macintosh. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2008). All effect estimates are reported as mean and 95% confidence intervals. Z tests were used to assess the overall effect of treatments and Chi-squared (χ2) tests were used to assess the heterogeneity along with I 2, which describes the percentage of the variability in effect estimates that is due to heterogeneity rather than chance (a value greater than 50% may be considered substantial heterogeneity). The differences between the treatment effects of sub-categories of a particular outcome were assessed by a Z test [1, 87], potential publication biases were assessed by Funnel plots [143].
Anti-emetic drugs examined
Ondansetron: 9-methyl-3-[(2-methylimidazol-1-yl)methyl]-2,3-dihydro-1H-carbazol-4-one. Granisetron: 1-methyl-N-(9-methyl-9-azabicyclo[3.3.1]nonan-7-yl)indazole-3-carboxamide. Indisetron: N-(3,9-dimethyl-3,9-diazabicyclo[3.3.1]nonan-7-yl)-1H-indazole-3-carboxamide. Zacopride: 4-amino-N-(1-azabicyclo[2.2.2]octan-8-yl)-5-chloro-2-methoxybenzamide. FK1052: (7S)-10-methyl-7-[(5-methyl-1H-imidazol-4-yl)methyl]-8,9-dihydro-7H-pyrido[1,2-a]indol-6-one hydrochloride. Dolasetron: (3R)-10-oxo-8-azatricyclo[5.3.1.03,8]undec-5-yl 1H-indole-3-carboxylate. L-683,877: 21-(1-Methyl-lH-indol-3-yl)-)spiro(1-azabicyclo[2.2.2]octane-3,51 (41H)-oxazole. Ramosetron: (1-methylindol-3-yl)-[(5R)-4,5,6,7-tetrahydro-3H-benzimidazol-5-yl]methanone. Azasetron: N-(1-azabicyclo[2.2.2]octan-8-yl)-6-chloro-4-methyl-3-oxo-1,4-benzoxazine-8-carboxamide. Renzapride: 4-amino-N-[(5S,6S)-1-azabicyclo[3.3.1]nonan-6-yl]-5-chloro-2-methoxybenzamide. Bemesetron: [(1S,5R)-8-methyl-8-azabicyclo[3.2.1]octan-3-yl] 3,5-dichlorobenzoate.
Results
Publications
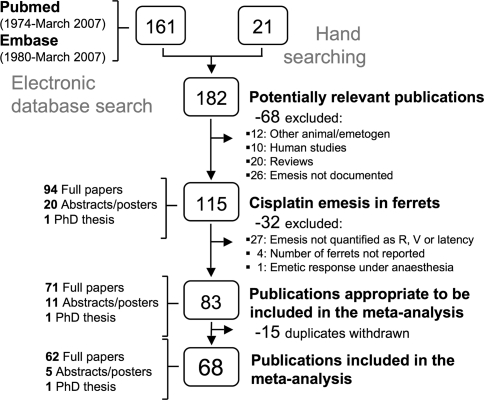
As of March 2007, 182 publications were retrieved, 115 publications describing cisplatin-induced emesis in the ferret were identified, 32 publications were excluded and 83 publication contained usable data (Fig. 1; Tables 1, 2). A further 15 publications were excluded on the grounds that data was already reported elsewhere. The remaining 68 publications were either fully or partly included as some papers presented original data and duplicate data together, in this case only the original data was extracted and the duplicate data was ignored.
Fig. 1.
Flow chart of identified studies. Reproduced and adapted from the QUOROM statement flow diagram [97]
Table 1.
List of 68 included publications
| Study | Quality score | Cisplatin dose | Obs. period | Study | Quality score | Cisplatin dose | Obs. period |
|---|---|---|---|---|---|---|---|
| Angel et al. (1993) [4] | 7 | 10 mg kg−1, i.v. | 3 h | Minami et al. (1998) [91] | 6 | 10 mg kg−1, i.p. | 6 h |
| Barnes et al. (1987) [6] | 6 | 10 mg kg−1, i.v. | 4 h | Miner et al. (1986a) [94] | 4 | 10 mg kg−1, i.v. | 4 h |
| Barnes et al. (1988) [5] | 9 | 10 mg kg−1, i.v. | 3 h | Miner et al. (1987) [96] | 4 | 10 mg kg−1, i.v. | 4 h |
| Barnes et al. (1991) [7] | 7 | 10 mg kg−1, i.v. | 4 h | Nakayama et al. (2005) [99] | 8.5 | 5, 10 mg kg−1, i.p. | 24, 4 h |
| Bermudez et al. (1988) [9] | 4.5 | 10 mg kg−1, i.v. | 4 h | Ozaki and Sakamoto (1999) [103] | 7 | 10 mg kg−1, i.v. | 4 h |
| Bingham et al. (1994) [11] | 4.5 | 12.5 mg kg−1, i.v. | 4 h | Reynolds et al. (1991) [108] | 6 | 10 mg kg−1, i.p. | 3 h |
| Blower (1990) [12] | 6 | 10 mg kg−1, i.v. | 4 h | Rudd et al. (1992) [111] | 5 | 10 mg kg−1, i.v | 4 h |
| Costall et al. (1986) [21] | 7 | 10 mg kg−1, i.v. | 2 h | Rudd et al. (1994a) [114] | 6.5 | 10 mg kg−1, i.p. | 40 h |
| Costall et al. (1987b) [19] | 6 | 10 mg kg−1, i.v. | 2 h | Rudd and Naylor (1994b) [117] | 5 | 5, 10 mg kg−1, i.p. | 24 h |
| Costall et al. (1987c) [22] | 6.5 | 10, 15 mg kg−1, i.v. | 2 h | Rudd and Naylor (1994c) [118] | 6 | 10 mg kg−1, i.v. | 4 h |
| Costall et al. (1990a) [20] | 7 | 10, 15 mg kg−1, i.v. | 4 h | Rudd et al. (1996b) [115] | 7.5 | 5, 10 mg kg−1, i.p. | 24, 40 h |
| Costall et al. (1990b) [23] | 7 | 10 mg kg−1, i.v. | 4 h | Rudd and Naylor (1996c) [119] | 7.5 | 5 mg kg−1, i.p. | 24 h |
| Davis (1988) [26] | 8 | 10, 12, 20 mg kg−1, i.v. | 2 h | Rudd et al. (1996a) [112] | 8 | 10 mg kg−1, i.v. | 4 h |
| Delagrange et al. (1996) [26, 27] | 3.5 | 10 mg kg−1, i.p. | 5 h | Rudd and Naylor (1997) [120] | 8.5 | 10 mg kg−1, i.p. | 24 h |
| Endo et al. (1990b) [33] | 6 | 7, 10 mg kg−1, i.p. | 6 h | Rudd et al. (1998b) [113] | 5.5 | 10 mg kg−1, i.p. | 24 h |
| Endo et al. (1994) [36] | 6.5 | 10 mg kg−1, i.p. | 6 h | Rudd et al. (2006a) [122] | 6 | 10 mg kg−1, i.p. | 6 h |
| Fink-Jensen (1992) [38] | 5 | 10 mg kg−1, i.v. | 4 h | Rycroft et al. (1996) [127] | 5 | 10 mg kg−1, i.v. | 4 h |
| Florczyk et al. (1982) [40] | 5 | 6, 8, 10 mg kg−1, i.v. | 4 h | Sam et al. (2001) [128] | 7.5 | 5 mg kg−1, i.p. | 24 h |
| Fukunaka et al. (1998) [42] | 8 | 5 mg kg−1, i.p. | 24 h | Sam et al. (2003) [129] | 7.5 | 5 mg kg−1, i.p. | 24 h |
| Gonsalves et al. (1996) [47] | 7.5 | 10 mg kg−1, i.p. | 2 h | Sam et al. (2007) [130] | 7.5 | 5 mg kg−1, i.p. | 24 h |
| Gylys et al. (1988) [49] | 5 | 12 mg kg−1, i.v. | 4 h | Schurig et al. (1982) [131] | 5.5 | 8 mg kg−1, i.p. | 4 h |
| Haga et al. (1993) [50] | 4.5 | 8 mg kg−1, i.v. | 5 h | Shiroshita et al. (1993) [132] | 6 | 10 mg kg−1, i.p. | 6 h |
| Hawthorn et al. (1988) [56] | 8.5 | 10 mg kg−1, i.p. | 4 h | Singh et al. (1997) [134] | 4.5 | 5 mg kg−1, i.p. | 24 h |
| Higgins et al. (1989) [59] | 5.5 | 9 mg kg−1, i.p. | 3 h | Taniguchi et al. (2004) [137] | 5 | 5 mg kg−1, i.p. | 24 h |
| Kamato et al. (1991) [67] | 6.5 | 10 mg kg−1, i.v., i.p. | 4 h | Tattersall et al. (1992) [139] | 7.5 | 10 mg kg−1, i.v. | 4 h |
| Kamato et al. (1993) [66] | 6.5 | 10 mg kg−1, i.v. | 6 h | Tattersall et al. (1993) [142] | 5.5 | 10 mg kg−1, i.v. | 4 h |
| King and Sanger (2005) [70] | 7.5 | 10 mg kg−1, i.p. | 6 h | Tattersall et al. (2000) [140] | 3.5 | 5, 10 mg kg−1, i.p., i.v. | 24, 4 h |
| Lau et al. (2005) [75] | 7.5 | 10 mg kg−1, i.p. | 2 h | Tsuchiya et al. (2002) [144] | 7.5 | 5 mg kg−1, i.p. | 24 h |
| Lehmann and Karrberg (1996) [76] | 7.5 | 10 mg kg−1, i.v. | 3 h | Watson et al. (1995) [148]{ | 7.5 | 10 mg kg−1, i.p. | 2 h |
| Marr et al. (1992) [81] | 6.5 | 10 mg kg−1, i.v. | 4 h | Yamakuni et al. (2002) [150] | 5 | 5, 10 mg kg−1, i.p. | 24, 4 h |
| Marr et al. (1994a) [82] | 7 | 10 mg kg−1, i.v. | 4 h | Yamakuni et al. (2006) [149] | 7.5 | 5, 10 mg kg−1, i.p., i.v. | 24, 4 h |
| Marr et al. (1994b) [83] | 3.5 | 12.5 mg kg−1, i.v. | 4 h | Yoshida et al. (1992a) [151] | 4 | 10 mg kg−1, i.v. | 3 h |
| Miller et al. (1993) [90] | 7 | 10 mg kg−1, i.v. | 4 h | Yoshida et al. (1993) [153] | 4.5 | 10 mg kg−1, i.v. | 3 h |
| Minami et al. (1997) [93] | 6 | 10 mg kg−1, i.p. | 6 h | Yoshikawa et al. (2001b) [157] | 3.5 | 10 mg kg−1, i.v. | 4 h |
For each included study, the quality score (out of 9), the dose and mode of administration of cisplatin and the duration of the acute phase observation period are indicated
Table 2.
List of 47 excluded publications
| Study | Reason for exclusion | Study | Reason for exclusion | Study | Reason for exclusion |
|---|---|---|---|---|---|
| Blum et al. (1992) [13] | Emesis | Gooch et al. (1998) [48] | Anaesthesia | Rudd et al. (2001) [116] | Group number |
| Bountra et al. (1993) [15] | Emesis | Haga et al. (2000) [51] | Emesis | Rudd et al. (2006b) [123] | Duplicate |
| Chevalier et al. (1998) [16] | Emesis | Hale et al. (1998) [53] | Duplicate | Rupniak et al. (1997) [125] | Emesis |
| Clark et al. (1993) [17] | Duplicate | Hale et al. (2000) [52] | Duplicate | Shiroshita et al. (1992) [133] | Emesis |
| Costall et al. (1987a) [18] | Duplicate | Hargreaves et al. (1994) [54] | Duplicate | Stables et al. (1987) [136] | Duplicate |
| Eglen et al. (1993) [31] | Emesis | Hollingworth et al. (2006) [60] | Group number | Tattersall et al. (1990) [138] | Duplicate |
| Eglen et al. (1994) [29] | Emesis | Ito et al. (1990) [64] | Emesis | Tattersall et al. (1996) [141] | Group number |
| Eglen et al. (1995) [30] | Emesis | Kim et al. (2005) [69] | Emesis | Twissell et al. (1993) [145] | Duplicate |
| Endo et al. (1990a) [32] | Duplicate | Lasheras et al. (1996) [74] | Emesis | Van Sickle et al. (2003) [146] | Emesis |
| Endo et al. (1992) [34] | Group number | Matsui et al. (1992) [86] | Emesis | Yoshida et al. (1991) [154] | Emesis |
| Endo et al. (1995) [35] | Emesis | Minami et al. (1991) [92] | Duplicate | Yoshida et al. (1992b) [152] | Emesis |
| Fitzpatrick et al. (1990) [39] | Emesis | Miner et al. (1986b) [95] | Duplicate | Yoshikawa et al. (1996) [155] | Emesis |
| Florczyk et al. (1981) [41] | Duplicate | Monkovic et al. (1988) [98] | Emesis | Yoshikawa et al. (2001a) [156] | Emesis |
| Gardner et al. (1994) [45] | Emesis | Ohta et al. (1996) [102] | Emesis | Youssefyeh et al. (1992a) [159] | Duplicate |
| Gardner et al. (1995) [46] | Emesis | Price et al. (1990) [107] | Emesis | Youssefyeh et al. (1992b) [158] | Duplicate |
| Gardner et al. (1996) [44] | Emesis | Rudd et al. (1998a) [121] | Emesis |
Reason for exclusion is indicated as: duplicate: data published elsewhere; group number: number of animals in the group missing; emesis: emesis not quantified as number of animals free of emesis, number of retches, number of vomits or latency, or emesis not defined; anaesthesia: emetic response investigated in anaesthetized animals
Out of the 68 publications from which at least one outcome was extracted, 44, 10 and 9 publications reported the effect of at least one 5-HT3, NK1 receptor antagonist and glucocorticoid, respectively. In terms of outcome, 63 studies reported the latency, which was either measured as the latency to the first retch (13% of the publications reporting the latency), the latency to the first vomit (16%) or the latency to the first emetic episode (75%). Fifty-one studies reported the number of retches and vomits (R+V) in a given observation time, 37 and 36 studies respectively reported the number of retches and vomits separately. The number of animals with emesis during the duration of the observation time was reported in 45 publications.
Meta-analysis: the ferret model of cisplatin induced emesis
Dose of cisplatin
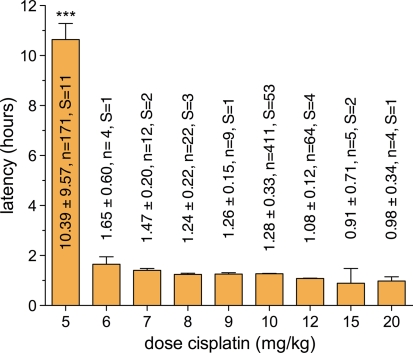
The latency to the onset of emesis was dose dependant; the time of onset was significantly delayed following a dose of cisplatin of 5 mg kg−1, compared with higher doses (6–20 mg kg−1, one-way ANOVA followed by Bonferroni post-tests, see Fig. 2). Additionally, differences between the doses of 6–20 mg kg−1 were detected (P < 0.001, one way ANOVA) and the latency shortened when the dose increased.
Fig. 2.
Latency to the onset of emesis (first retch, vomit or vomiting episode) induced by various doses of cisplatin. Data collected from 64 studies involving 702 animals and plotted on the graph as weighted mean ± SD. Differences between the doses were assessed by one-way ANOVA followed by Bonferroni post-tests, ***p < 0.0001 compared with all other doses in the post-tests. The exact latency values, the number of ferrets from which those values were calculated (n) and the number of studies from which this data was extracted (S) are given above each column
The 10 mg kg−1 cisplatin model
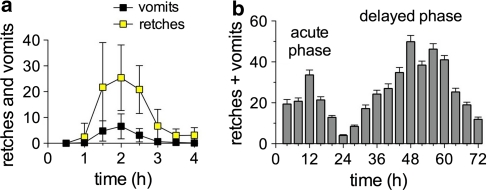
The duration of the observation period varied from 2 to 40 h (at which time the animals were killed). The most common observation period was 4 h, during which 107 ± 48 R+V (n = 199, 22 studies) were observed. In studies using 2, 3, 6, 24 and 40 h observation periods, 79 ± 35 R+V (n = 40, 6 studies), 101 ± 48 R+V (n = 29, 3 studies), 170 ± 56 R+V (n = 73, 8 studies), 204 ± 52 R+V (n = 16, 3 studies) and 188 R+V (n = 4, 1 study) were observed, respectively. The number of R+V significantly increased as the observation period increased up to 24 h (one-way ANOVA, P < 0.001). The intensity of emesis reached a maximum after 2 h and decreased to a very low level (less that 5 R+V per hour) from 3 h onward post cisplatin (Fig. 3a).
Fig. 3.
Profile of emesis induced by 10 mg kg−1 (a) and 5 mg kg−1 (b) cisplatin in the ferret. a Data plotted as mean vomits ± SD per 30 min periods, collected from 6 studies involving 34 animals and mean retches ± SD, collected from 4 of those studies involving 20 out of the 34 animals. b Data plotted as weighted mean R+V ± SD per 4-h periods collected from 9 studies involving 92 animals
The latency to the onset of emesis was shorter when cisplatin was administered intravenously (1.16 ± 0.35 h, n = 277) compared to intraperitoneally (1.51 ± 0.29 h, n = 134, P < 0.001, independent sample t test). However, the route of administration was directly related to the use of anaesthesia, and all the animals injected with cisplatin intravenously (i.v.) had prior anaesthesia during which an i.v. line was implanted or were anaesthetised at the time of cisplatin injection, and prior anaesthesia was not reported in any of the animals that received an intraperitoneal (i.p.) injection of cisplatin. The recovery period between anaesthesia and the administration of cisplatin did not make a difference as ferrets that received cisplatin under anaesthesia developed emesis with a latency of 1.21 ± 0.32 h (n = 93), and those allowed up to 3 and more than 3 days recovery developed emesis with a latency of 1.11 ± 0.31 h (n = 51) and 1.13 ± 0.46 h (n = 89), respectively (one-way ANOVA, P = 0.21). The use of an injectable anaesthetic (sodium pentobarbital 30–35 mg kg−1 i.p.) further shortened the latency (0.95 ± 0.14 h, n = 46) compared to volatile anaesthetics (1.21 ± 0.39 h, n = 176, P < 0.001, independent sample t test).
Intraperitoneal cisplatin induced a more severe emetic response and 156 ± 41 R+V (n = 19) and 172 (n = 65, SD not available) were quantified over 4 and 6 h, respectively, compared to 102 ± 52 R+V (n = 180, P < 0.001, independent sample t test) and 152 (n = 8, SD not available) following i.v. cisplatin injection (with prior anaesthesia). No differences were observed over an observation period of 2 h (i.p.: 72 ± 41, n = 22; i.v.: 88 ± 32, n = 18, P = 0.194, independent samples t test). There was not enough data available on the emetic response quantified for 3, 24 and 40 h to investigate the influence of the mode of administration of cisplatin and the use of anaesthesia.
In animals that did not receive any vehicle, the latency was 1.39 ± 0.20 h (n = 18) and ferrets had 92 ± 15 R+V (n = 5). Different vehicles such as saline/distilled water (1.30 ± 0.38 h, n = 296; 97 ± 31 R+V, n = 125), propylene glycol (1.23 ± 0.06 h, n = 4), PEG 300 (1.79 ± 0.18 h, n = 5), Tween 80 (1.22 ± 0.19 h, n = 8) and methyl cellulose (1.13 ± 0.25 h, n = 5) impacted on the latency (P < 0.0001, one-way ANOVA) but no significant differences were found compared to the group that received no vehicle (P > 0.05, Bonferroni post-tests). Glucose (1.33 ± 0.24 h, n = 7; 148 ± 100 R+V, n = 7) was also found to increase the number of R+V (P < 0.05, one-way ANOVA and Bonferroni post-tests).
No differences were detected in latency or number of R+V over 4 h in groups of male ferrets only compared to groups of males and females (P > 0.05, independent sample t tests). The latency was significantly reduced in albino ferrets (1.07 ± 0.14 h, n = 29) compared to fitch ferrets (1.34 ± 0.20 h, n = 70) and mixed groups of albino and fitch ferrets (1.25 ± 0.36 h, n = 108, P < 0.05, one-way ANOVA and Bonferroni post-tests) but not enough data were available to compare the number of R+V.
The latency to the onset of emesis was significantly longer in ferrets bred in New Zealand (1.73 ± 0.37 h, n = 11) compared to animals bred in the UK (1.25 ± 0.44 h, n = 170) and in the USA (1.31 ± 0.19 h, n = 176, P < 0.05, one-way ANOVA and Bonferroni post-tests). No differences were detected in the number of R+V over 4 h (P > 0.05), but the number of R+V over 2 h was reduced in New Zealand ferrets (40 ± 41 R+V, n = 6) compared to U.K. animals (88 ± 32 R+V, n = 18, P = 0.007, independent sample t tests). As all the ferrets originating from New Zealand were challenged with an intraperitoneal dose of cisplatin, a sub-analysis was carried out only in animals administered cisplatin i.p. and the delay in latency was still significant in ferrets bred New Zealand compared to animals bred in the UK (1.43 ± 0.46 h, n = 29, P < 0.05) but not to animals bred in the USA (1.51 ± 0.21 h, n = 84, P > 0.05, one-way ANOVA and Bonferroni post-tests).
The 5 mg kg−1 cisplatin model (acute and delayed emesis model)
Fourteen studies investigated cisplatin-induced acute and delayed emesis in the ferret; cisplatin was administered i.p. in all studies and no study reported prior use of anaesthesia. A biphasic profile of emesis was observed; the acute phase started 10.51 ± 0.58 h (n = 156) after cisplatin administration, peaked after 12 h and a nadir was reached after 24 h (Fig. 3b). The delayed phase was more intense than the acute phase and reached a peak 48 h post cisplatin before gradually decreasing in intensity during the next 24 h, until 72 h post cisplatin, at which time a small amount of emesis still persisted. 105 ± 83 R+V (n = 215) and 340 ± 171 (n = 153) were observed during the acute and delayed phase, respectively (161 ± 98 R+V during day 2 and 179 ± 94 R+V during day 3, n = 130). Overall, 448 ± 231 R+V (n = 153) were observed during the entire 72-h period.
In animals that did not receive any vehicle, the latency was 11.76 ± 9.86 h (n = 98) and animals that received i.p. injections of vehicles such as saline, distilled water and 10% NaHCO3 had a latency of 5.52 ± 3.32 h (n = 12), 8.74 ± 8.61 h (n = 41) and 5.71 ± 5.66 h (n = 5), respectively. Overall, the injection of a vehicle had an impact on the latency (P < 0.0001, one-way ANOVA) but no specific differences were detected compared to the group that did not receive any vehicle (P > 0.05, Bonferroni post-tests). None of the vehicles had a significant impact on the number of R+V during the acute or the delayed phase (P > 0.05, one-way ANOVA). Neither the strain nor the sex of the ferrets had an impact on the latency or the number of R+V (P > 0.05, one-way ANOVA).
Meta-analysis: the effect of anti-emetics
Effect of ondansetron on the acute phase of emesis
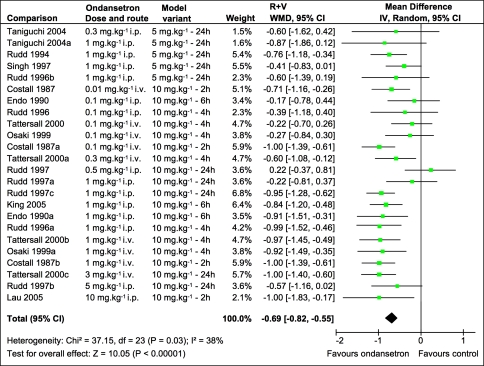
Outcome: number of retches and vomits (R+V)
Data for the number of R+V was extracted from 11 full papers, 23 comparisons involving 107 ferrets assessed the efficacy of ondansetron versus control during the acute phase of emesis induced by 5 and 10 mg kg−1 cisplatin. As shown in Fig. 4, the overall effect of ondansetron was a reduction of the R+V by about 70% (−0.69, −0.82 to −0.55) and this was highly significant (Z = 10.05, P < 0.0001). A small statistical heterogeneity was detected (χ2 = 37.15, df = 23, P = 0.03; I 2 = 38.1%).
Fig. 4.
Efficacy of ondansetron number of retches + vomits during the acute phase of emesis induced by cisplatin 5 or 10 mg kg−1. Point estimates and 95% confidence intervals for each of the ondansetron versus control comparisons ranked by dose. The effect estimate was computed as the weighted mean difference (WMD) and expressed as the proportion of retches and vomits in the control group. An effect estimate of −1 indicates that emesis was abolished in the treatment group, 0 indicates that the treatment had no effect on the R + V response and an effect estimate >0 indicates that the treatment increased the number of R + V. The size of each square represents the weight of the comparison in the WMD calculation
Five variants of the acute model of cisplatin-induced emesis were combined in this meta-analysis: emesis induced by 5 mg kg−1 cisplatin and R+V quantified for 24 h and emesis induced by 10 mg kg−1 and R+V quantified for 24, 6, 4 and 2 h. Ondansetron significantly reduced the R+V in all variants of the model but one; as shown Table 3, the reduction of R+V did not reach statistical significance when emesis was induced by 10 mg kg−1 cisplatin and quantified for 24 h. There was a trend for the effect of ondansetron to increase with shorter observation times (41, 68, 70 and 93% reduction for 24, 6, 4 and 2-h observation periods, respectively) but this did not reach statistical significance. The R+V reduction was dose-dependent, doses of 1–10 mg kg−1 afforded a more effective protection than lower doses of 0.1–0.5 mg kg−1 (40 and 83%, respectively, Z = 2.52, P = 0.010). The regimen of ondansetron administration did not change the outcome; the effect of ondansetron was similar with i.v., i.p., and s.c. injections (Z tests, P > 0.05) and ferrets treated 30 min prior to cisplatin administration received the same degree of protection as ferrets treated at the time of cisplatin injection (Z = 0.04, P = 0.965, see Table 3). With longer observation periods, ondansetron three times daily was as effective as twice-daily injections (Z = 0.05, P = 0.959). Ondansetron had the same efficacy on the R+V induced by an i.p. or an i.v. dose of cisplatin (Z = 1.07, P = 0.287) and the origin of the animals or the quality score of the studies (see Table 1) did not influence the outcome (Z tests, P > 0.05).
Table 3.
Sensitivity analyses of the effect of ondansetron on the number of retches + vomits (R+V) induced by cisplatin (5 or 10 mg kg−1)
| Effect estimate (proportion of R+V difference) | 95% CI | Number of comparisons | Overall effect (Z tests) | Heterogeneity (χ2) | |
|---|---|---|---|---|---|
| Cisplatin dose and duration of the observation period | |||||
| 5 mg/kg (24 h) | −0.61 | −0.87 to −0.35 | 5 | P < 0.001*** | P = 0.800 |
| 10 mg/kg (24 h) | −0.41 | −0.95 to 0.13 | 4 | P = 0.13 | P = 0.004** |
| 10 mg/kg (6 h) | −0.68 | −1.09 to −0.26 | 3 | P = 0.001** | P = 0.140 |
| 10 mg/kg (4 h) | −0.70 | −0.94 to −0.46 | 8 | P < 0.001*** | P = 0.100 |
| 10 mg/kg (2 h) | −0.93 | −1.15 to −0.70 | 4 | P < 0.001*** | P = 0.750 |
| Ondansetron dose | |||||
| 0.01 mg kg−1 | −0.71 | −1.16 to −0.26 | 1 | P = 0.002** | N/A |
| 0.1–0.5 mg kg−1 | −0.40 | −0.69 to −0.10 | 8 | P = 0.009** | P = 0.030* |
| 1–10 mg kg−1 | −0.83 | −0.95 to −0.70 | 15 | P < 0.001*** | P = 0.600 |
| Mode of delivery of ondansetron | |||||
| i.v. | −0.77 | −0.95 to −0.60 | 11 | P < 0.001*** | P = 0.130 |
| i.p. | −0.59 | −0.81 to −0.37 | 11 | P < 0.001*** | P = 0.030* |
| s.c. | −0.74 | −1.45 to −0.03 | 2 | P = 0.040* | P = 0.710 |
| Treatment time | |||||
| With cisplatin | −0.67 | −0.86 to −0.48 | 15 | P < 0.001*** | P = 0.010* |
| 30 min before | −0.68 | −1.09 to −0.26 | 3 | P = 0.001** | P = 0.140 |
| Twice daily | −0.74 | −1.45 to −0.03 | 4 | P = 0.04* | P = 0.710 |
| Three times daily | −0.72 | −0.98 to −0.48 | 2 | P < 0.001*** | P = 0.26 |
| Mode of administration of cisplatin | |||||
| i.v. | −0.77 | −0.97 to −0.57 | 9 | P < 0.001*** | P = 0.100 |
| i.p. | −0.62 | −0.81 to −0.44 | 15 | P < 0.001*** | P = 0.080 |
| Animal origin | |||||
| UK | −0.70 | −0.88 to −0.53 | 15 | P < 0.001*** | P = 0.020* |
| USA | −0.67 | −0.91 to −0.44 | 7 | P < 0.001*** | P = 0.330 |
| NZ | −1.00 | −0.83 to −0.17 | 1 | P = 0.020* | N/A |
| Quality score | |||||
| Less that 5/9 | −0.65 | −0.95 to −0.34 | 5 | P < 0.001*** | P = 0.060 |
| 5 to 7/9 | −0.76 | −0.97 to −0.56 | 9 | P < 0.001*** | P = 0.260 |
| 7.5 to 9/9 | −0.65 | −0.88 to −0.42 | 10 | P < 0.001*** | P = 0.050 |
The effect estimate was computed as the weighted mean difference (WMD) and expressed as the proportion of retches and vomits in the control group. An effect estimate of −1 indicates that emesis was abolished in the treatment group, 0 indicates that the treatment had no effect on the R+V response and an effect estimate >0 indicates that the treatment increased the number of R+V. The variables examined were the variant of the cisplatin model (5 or 10 mg kg−1 cisplatin and the duration of the observation period), the mode of administration of cisplatin, the dose of ondansetron, the regimen of ondansetron administration (mode of delivery and timing relative to cisplatin administration), the animal origin (country animals were bred) and the quality score assigned to the study where comparisons were extracted
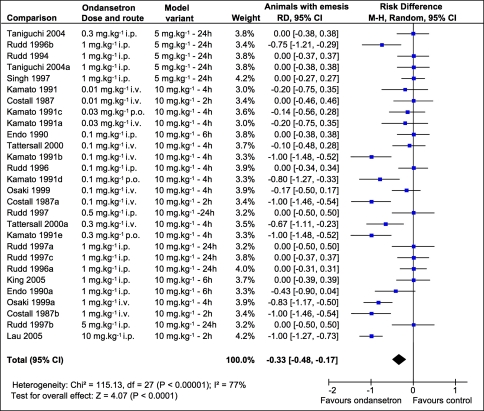
Outcome: number of animals with emesis
Data on the number of animals with emesis was extracted from 14 publications; 28 comparisons involving 256 ferrets were identified. The global estimate of the effect of ondansetron was −0.33 (−0.48 to 0.17) indicating that following the administration of cisplatin 5 or 10 mg kg−1, ondansetron abolished the emetic response during the observation time in one-third of the ferrets (see Fig. 5). Overall, this effect was significant (Z = 4.09, P < 0.001) but a substantial statistical heterogeneity (χ2 = 115.13, df = 27, P < 0.001, I 2 = 76.5%) was detected between comparisons. Subgroup analyses revealed differences in estimates of efficacy between variants of the model. Whereas ondansetron had a significant effect against emesis induced by 10 mg kg−1 cisplatin and quantified over short observation times (2–4 h) it did not show any significant effect against 10 mg kg−1 cisplatin-induced emesis quantified for 6 and 24 h and 5 mg kg−1 cisplatin-induced emesis quantified for 24 h (see Table 4). Efficacy increased as the dose increased, and only doses of ondansetron higher than 0.1 mg kg−1 had a significant effect but there was significant heterogeneity within those two subgroups (see Table 4). No statistical differences were detected between i.p., i.v. and oral (p.o.) administration of ondansetron (Z tests, P > 0.05) but χ2 and I 2 tests revealed a high degree of heterogeneity in all 3 subgroups. Administered s.c., ondansetron was ineffective but this could potentially be misleading as only 2 comparisons were included in that group and both reported the number of animals completely protected for 24 h in which setting none of the animals were completely protected (see Table 4, Fig. 5). The regimen used did not influence significantly the number of animals completely protected by ondansetron. There were no differences between the subgroup that received ondansetron at the time of cisplatin injection and the subgroups that received it 30 min and 1 h prior to cisplatin (Z tests, P > 0.05) but once again, these results should be taken with caution as the heterogeneity within each subgroup was high. With longer observation times (24 h), ondansetron was equally ineffective given 2 or 3 times a day. Ondansetron appeared slightly more effective when cisplatin was injected i.v. compared to i.p. but this did not reach statistical significance (Z = 1.757, P = 0.079) and could be biased by the fact that in all the comparisons where animals were observed for 24 h, cisplatin was injected i.p. Furthermore, heterogeneity was, once again, highly significant in both groups (see Table 4). The origin of the animals and the quality score of the studies did not influence the effect of ondansetron (Z tests, P > 0.05); however heterogeneity was high in all subgroups (see Table 4).
Fig. 5.
Efficacy of ondansetron on the number of animals developing an acute phase of emesis following cisplatin 5 or 10 mg kg−1. Point estimates and 95% confidence intervals for each of the ondansetron versus control comparisons ranked by dose. The effect estimate was computed as the risk difference (RD) and represents the proportion of animals with emesis during the duration of the observation period. An effect estimate of 0 indicates that the treatment had no effect on the number of animals with emesis, −1 indicates maximal effect. The size of each square represents the weight of the comparison in the total RD calculation
Table 4.
Sensitivity analyses of the effect of ondansetron on the number of animals with emesis following the administration of cisplatin (5 or 10 mg kg−1)
| Effect estimate (proportion of ferrets with emesis) | 95% CI | Number of comparisons | Overall effect (Z tests) | Heterogeneity (χ2) | |
|---|---|---|---|---|---|
| Cisplatin dose and duration of the observation period | |||||
| 5 mg/kg (24 h) | 0.00 | −0.15 to 0.15 | 5 | P = 1.000 | P = 1.000 |
| 10 mg/kg (24 h) | 0.00 | −0.23 to 0.23 | 4 | P = 1.000 | P = 1.000 |
| 10 mg/kg (6 h) | −0.11 | −0.38 to 0.15 | 3 | P = 0.400 | P = 0.280 |
| 10 mg/kg (4 h) | −0.48 | −0.70 to −0.26 | 12 | P < 0.001*** | P < 0.001*** |
| 10 mg/kg (2 h) | −0.76 | −1.21 to −0.31 | 4 | P = 0.001** | P = 0.002** |
| Ondansetron dose | |||||
| 0.01–0.03 mg kg−1 | −0.13 | −0.37 to 0.12 | 4 | P = 0.31 | P = 0.93 |
| 0.1–0.5 mg kg−1 | −0.39 | −0.68 to −0.11 | 10 | P = 0.006** | P < 0.001*** |
| 1–10 mg kg−1 | −0.33 | −0.57 to −0.10 | 14 | P = 0.006** | P < 0.001*** |
| Mode of delivery of ondansetron | |||||
| i.v. | −0.49 | 0.25 to 0.73 | 12 | P < 0.001*** | P < 0.001*** |
| i.p. | −0.14 | −0.10 to 0.38 | 11 | P = 0.25 | P < 0.001*** |
| s.c. | −0.00 | −0.27 to 0.27 | 2 | P = 1.000 | P = 1.000 |
| p.o. | −0.64 | −1.16 to −0.11 | 3 | P = 0.020* | P = 0.020* |
| Treatment time | |||||
| With cisplatin | −0.43 | −0.68 to −0.18 | 13 | P < 0.001*** | P < 0.001*** |
| 30 min before | −0.29 | −0.60 to 0.02 | 6 | P = 0.060 | P = 0.020* |
| 1 h before | −0.64 | −1.16 to −0.11 | 3 | P = 0.020* | P = 0.020* |
| Twice daily | 0.00 | −0.27 to 0.27 | 2 | P = 1.000 | P = 1.000 |
| Three times daily | 0.00 | −0.16 to 0.16 | 4 | P = 1.000 | P = 1.000 |
| Mode of administration of cisplatin | |||||
| i.v. | −0.49 | −0.73 to −0.25 | 12 | P < 0.001*** | P < 0.001*** |
| i.p. | −0.21 | −0.41 to −0.01 | 16 | P = 0.04* | P < 0.001*** |
| Animal origin | |||||
| UK | −0.24 | −0.43 to −0.04 | 14 | P = 0.020* | P < 0.001*** |
| USA | −0.36 | −0.57 to −0.14 | 13 | P = 0.001** | P < 0.001*** |
| NZ | 1.00 | −1.27 to −0.73 | 1 | P < 0.001*** | N/A |
| Quality score | |||||
| Less that 5/9 | −0.23 | −0.62 to 0.16 | 3 | P = 0.250 | P = 0.030* |
| 5 to 7/9 | −0.44 | −0.66 to −0.22 | 15 | P < 0.001*** | P < 0.001*** |
| 7.5 to 9/9 | −0.18 | −0.46 to 0.09 | 10 | P = 0.19 | P < 0.001*** |
The effect estimate was computed as the risk difference (RD) and represents the proportion of animals with emesis during the duration of the observation period. An effect estimate of 0 indicates that the treatment had no effect on the number of animals with emesis, −1 indicates maximal effect. The variables examined were the variant of the cisplatin model (5 or 10 mg kg−1 cisplatin and the duration of the observation period), the mode of administration of cisplatin, the dose of ondansetron, the regimen of ondansetron administration (mode of delivery and timing relative to cisplatin administration), the animal origin (country animals were bred) and the quality score assigned to the study where comparisons were extracted
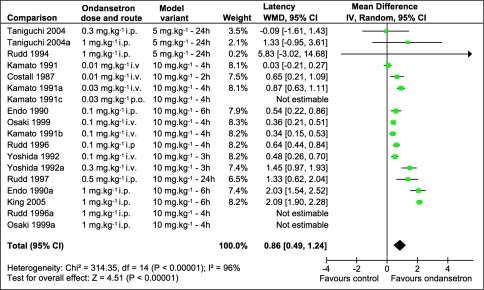
Outcome: latency
Latency data was extracted from 10 full papers. Fifteen comparisons involving 131 ferrets assessed the effect of ondansetron on emesis induced by 10 mg kg−1 cisplatin and 3 comparisons assessed the effect of ondansetron on the latency to the onset of emesis induced by 5 mg kg−1 cisplatin (see Fig. 6). The global estimate of the effect of ondansetron on the latency was 0.86 (0.49–1.24), which means that the latency was nearly twice as long in the groups treated with ondansetron compared to the control groups. This effect was significant (Z = 4.45, P < 0.001) but χ2 test revealed a high degree of heterogeneity (χ2 = 314.35, df = 14, P < 0.001), which was corroborated by the I 2 (96%). Subgroup analysis revealed that ondansetron statistically delayed the latency to the onset of emesis induced by 10 mg kg−1 cisplatin but not 5 mg kg−1 cisplatin (Table 5, Fig. 6). The effect of ondansetron was dose dependant and doses of 1 mg kg−1 conferred a significantly higher protection, increasing the latency by about 200% (Z tests, P < 0.05). Ondansetron was more effective when given i.p. than p.o. or i.v. (Z tests, P < 0.05); however, this result needs to be taken with caution as ondansetron was injected i.p. in all the comparisons where the highest dose was given (see Fig. 6). No significant differences were observed with different treatment times, there was no difference in outcome if cisplatin was injected i.p. or i.v. and the origin of the ferrets did not influence the outcome (Z tests, P > 0.05). The outcome was not influenced by the quality of the study (see Table 1) as no differences were detected between studies scoring less than 5 out of 9, between 5 and 7/9 and 7.5 or higher (Z tests, P > 0.05).
Fig. 6.
Efficacy of ondansetron on the latency to emesis induced by cisplatin (5 or 10 mg kg−1). Point estimates and 95% confidence intervals for each of the ondansetron versus control comparisons ranked by dose. The effect estimate is the impact of the treatment on the latency expressed as a proportion of the latency in the control group. An effect estimate <0 indicates that the latency was shorter in the control group than in the treatment group, 0 indicates that the treatment had no effect on the latency and an effect estimate of 1 indicates that the treatment increased the latency by 100%. The size of each square represents the weight of the comparison in the WMD calculation. Note that in 3 comparisons, the effect estimate was not estimable as only one animal developed emesis in the group treated with ondansetron
Table 5.
Sensitivity analyses of the effect of ondansetron on the latency to the onset of emesis induced by cisplatin (5 or 10 mg kg−1)
| Effect estimate (proportion of latency change) | 95% CI | Number of comparisons | Overall effect (Z tests) | Heterogeneity (χ2) | |
|---|---|---|---|---|---|
| Cisplatin dose | |||||
| 10 mg kg−1 | 0.88 | 0.49 to 1.27 | 15 | P < 0.001*** | P < 0.001*** |
| 5 mg kg−1 | 0.60 | −0.97 to 2.16 | 3 | P = 0.45 | P = 0.29 |
| Ondansetron dose | |||||
| 0.01–0.02 mg kg−1 | 0.36 | 0.00 to 0.72 | 3 | P = 0.050 | P = 0.008** |
| 0.03–0.06 mg kg−1 | 0.85 | 0.30 to 1.40 | 3 | P = 0.002** | P < 0.001*** |
| 0.1 mg kg−1 | 0.49 | 0.31 to 0.67 | 5 | P < 0.001*** | P = 0.140 |
| 1 mg kg−1 | 1.96 | 1.66 to 2.25 | 7 | P < 0.001*** | P = 0.27 |
| Mode of delivery of ondansetron | |||||
| i.v. | 0.60 | 0.35 to 0.85 | 9 | P < 0.001*** | P < 0.001*** |
| p.o. | 0.34 | 0.15 to 0.53 | 2 | P < 0.001*** | N/A |
| i.p. | 1.54 | 0.67 to 2.41 | 5 | P < 0.001*** | P < 0.001*** |
| s.c. | 0.36 | −0.94 to 1.65 | 2 | P = 0.59 | P = 0.31 |
| Treatment time | |||||
| With cisplatin | 0.62 | 0.34 to 0.68 | 6 | P < 0.001*** | P = 0.010* |
| 20–30 min before | 1.11 | 0.25 to 1.96 | 5 | P = 0.010** | P < 0.001*** |
| 1 h before | 0.34 | 0.15 to 0.53 | 2 | P = 0.010** | N/A |
| 30 min before and 45 min after | 0.94 | −0.01 to 1.89 | 2 | P = 0.050* | P < 0.001*** |
| Twice daily | 0.36 | −0.94 to 1.65 | 2 | P = 0.590 | P = 0.310 |
| Three times daily | 5.83 | −3.02 to 14.68 | 1 | P = 0.020* | N/A |
| Mode of administration of cisplatin | |||||
| i.v. | 0.60 | 0.35 to 0.85 | 9 | P < 0.001*** | P < 0.001*** |
| i.p. | 1.16 | 0.35 to 1.96 | 9 | P = 0.005 | P < 0.001*** |
| Animal origin | |||||
| UK | 0.76 | 0.44 to 1.07 | 5 | P < 0.001*** | P = 0.19 |
| USA | 0.86 | 0.39 to 1.33 | 13 | P < 0.001*** | P < 0.001*** |
| Quality score | |||||
| Less that 5/9 | 0.94 | −0.01 to 1.89 | 2 | P = 0.050 | P < 0.001*** |
| 5 to 7/9 | 0.63 | 0.32 to 0.94 | 11 | P < 0.001*** | P < 0.001*** |
| 7.5 to 9/9 | 1.42 | 0.31 to 2.53 | 5 | P = 0.01** | P < 0.001*** |
The effect estimate was computed as the weighted mean difference (WMD) and represents the impact of the treatment on the latency expressed as a proportion of the latency in the control group. An effect estimate <0 indicates that the latency was shorter in the control group than in the treatment group, 0 indicates that the treatment had no effect on the latency and an effect estimate of 1 indicates that the treatment increased the latency by 100%. The variables examined were the dose and mode of administration of cisplatin, the dose of ondansetron, the regimen of ondansetron administration (mode of delivery and timing relative to cisplatin administration), the animal origin (country animals were bred) and the quality score assigned to the study where comparisons were extracted
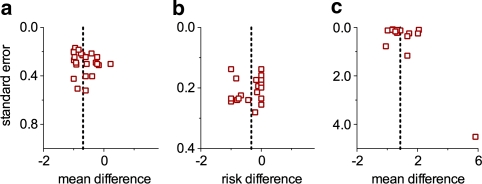
Funnel plots for the effect of ondansetron on the R+V and the number of animals with emesis were relatively symmetrical (see Fig. 7). The funnel plot for the latency was slightly asymmetrical, which reflects the high degree of heterogeneity detected for this outcome. Overall, no associations between treatment effect and sample size were detected, suggesting no evidence of publication bias.
Fig. 7.
Funnel plots for the effect of ondansetron on the number of retches + vomits (a), number of animals with emesis (b) and latency (c). For each comparison, the effect estimates are plotted on the x-axis and corresponding standard errors are plotted on the y-axis
Effect of 5-HT3 receptor antagonists on the latency to the onset of emesis induced by 10 mg kg−1 cisplatin
The effects of 5-HT3 receptor antagonists on the latency to the onset of 10 mg/kg cisplatin-induced emesis were investigated with 11 different anti-emetics (ondansetron, granisetron, tropisetron, indisetron, dolasetron, L-683,877, renzapride, zacopride, bemesetron, azasetron and ramosetron), this data was extracted from 22 studies; 76 comparisons were reported, involving 587 ferrets. However, for 14 comparisons, because only one animal developed emesis in the treatment group, the point estimate and confidence interval could not be computed and was therefore not included in the calculation of the effect estimate. Altogether, 5-HT3 receptor antagonists increased the latency by 72% (effect estimate: 0.72, 95% CI 0.56–0.87); this effect was highly significant (Z = 9.08, P < 0.0001) but a high degree of heterogeneity (χ2 = 1001.57, df = 61, P < 0.0001, I 2 = 93.9%) was detected. Dolasetron (0.02, −0.76 to 0.80) renzapride (1.11, −0.18 to 2.40), bemesetron (0.29, −0.17 to 120) and ramosetron (0.19, −0.02 to 0.39) did not delay the onset of emesis in a statistically significant manner (Z tests, P > 0.05), whereas ondansetron (0.88, 0.49–1.27), granisetron (0.67, 0.41–0.93), tropisetron (0.49, 0.17–0.81), indisetron (0.92, 0.28–1.57), L-683,877 (0.72, 0.11–1.33), zacopride (0.79, 0.37–1.20) and azasetron (0.52, 0.37–0.67) significantly increased the latency by 49–92% (Z tests, P < 0.05).
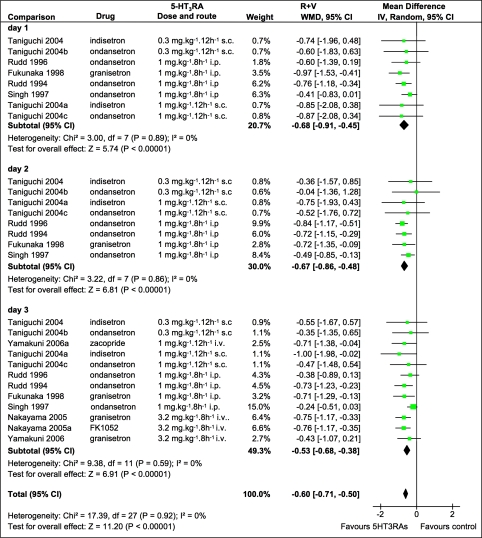
Effect of 5-HT3 receptor antagonists on the acute and delayed phases of emesis induced by 5 mg kg−1 cisplatin
Data for the effects of 5-HT3 receptor antagonists on the daily emetic response induced by 5 mg kg−1 i.p. cisplatin were extracted from 5 studies; 8 comparisons were identified, involving 72 animals. 5-HT3 receptor antagonists reduced the number of R+V by 68% (−0.68, −0.91 to −0.45) on day 1, 67% (−0.67, −0.86 to −0.48) on day 2 and 53% (−0.53, −0.85 to −0.38) on day 3; this was statistically significant on each of the 3 days (Z = 5.74, Z = 6.81 and Z = 4.44 for day 1, 2 and 3, respectively; P < 0.0001, see Fig. 8). There was no difference between the effect of 5-HT3 receptor antagonists on each of the 3 days (Z tests, P > 0.05); no statistical heterogeneity was detected (χ2 tests, P > 0.05 and I 2 = 0% on each of the 3 days). The effects of granisetron and ondansetron were significant for each of the 3 days, whereas indisetron did significantly reduce the R+V during day 1 and 3 but not day 2. No significant differences were detected between the effects of ondansetron, granisetron and indisetron for each of the 3 days (Z tests, P > 0.05).
Fig. 8.
Efficacy of 5-HT3 receptor antagonists on the daily number of retches + vomits (R + V) induced by 5 mg kg−1 i.p. cisplatin during the acute (day 1) and delayed (days 2, 3) phases of emesis. Point estimates and 95% confidence intervals for each of the 5-HT3 receptor antagonist versus control comparisons ranked by dose. The effect estimate was computed as the weighted mean difference (WMD) and expressed as the proportion of retches and vomits in the control group. An effect estimate of −1 indicates that emesis was abolished in the treatment group, 0 indicates that the treatment had no effect on the R + V response and an effect estimate >0 indicates that the treatment increased the number of R + V. The size of each square represents the weight of the comparison in the WMD calculation
Discussion and conclusions
Cisplatin-induced emesis in the ferret
We found that the latency to the onset of the cisplatin-induced emesis was dose dependent, which is consistent with findings in other species such as humans [71], dogs [10] and pigeons [106]. A step-change was observed between 5 and 6 mg kg−1, suggesting a difference in the mechanisms triggering emesis at low and high dose, possibly the activation of an additional mechanism (e.g. recruitment of less sensitive vagal afferent branches, area postrema). Prior anaesthesia and the route of administration of cisplatin were identified as confounding factors; the emetic response was also modulated by some of the vehicles used and factors inherent to the ferrets such as strain and origin. The difference between intravenous and intraperitoneal cisplatin may only reflect prior anaesthesia, as these two factors were dependent in the present study. Certainly, anaesthesia had an impact in its own right as differences were detected between injectable and volatile anaesthetics. The impact of the ferrets’ origin could reflect a genuine difference between populations of ferrets but it might also indicate differences between laboratories rather than a difference between animals; this cannot be determined from the present study.
These findings however stress the relevance of choosing appropriate controls (e.g. vehicle control, sham-operated) and homogeneous groups of animals when using the ferret cisplatin model of emesis.
The profile of emesis induced by 5 mg kg−1 i.p. cisplatin in the ferret was clearly biphasic, which is consistent with the profile of emesis observed in the clinic [84] but differences were observed in the timing and magnitude of the two phases. Whereas the acute phase is more severe than the delayed phase in humans [72, 84], with an onset 1–6 h following cisplatin infusion [55, 71, 84], the latency to the onset of the acute phase was greater in the ferret (>10 h) and its relative intensity compared to the delayed phase was lower. The incidence of emesis on each day could not be investigated in the ferret as all reports stated that 100% of the animals developed an emetic response but no distinction was made between the acute and delayed phases. A few studies have however suggested that the acute phase was not observed in all animals [115, 147], which is also consistent with our recent observations [104] and suggests that whereas the incidence of emesis during the delayed phase is close to 100%, the incidence of acute emesis at this dose is lower. In humans treated with placebo anti-emetics, however, the incidence of emesis during the acute phase (98%, [71]) is higher than during the delayed phase (44–89% [43, 72]).
Effect of 5-HT3 receptor antagonists
The efficacy of ondansetron in the acute model of cisplatin-induced emesis was assessed measuring 3 outcomes: the number of R+V, the number of animals with emesis and the latency to the onset of emesis. Overall, all 3 outcomes permitted the detection of significant anti-emetic protection, which is consistent with findings in humans [24], but different variants of the model resulted in different levels of anti-emetic protection. Whereas all variants of the acute model reflected a similar reduction of R+V, ondansetron only delayed significantly the onset of emesis following 10 but not 5 mg kg−1 cisplatin, and the number of animals with emesis was only reduced with observation periods no longer than 4 h. In the 10 mg kg−1 4 h variant of the model, half of the animals were completely protected from emesis, which was comparable to percentage of patients free of emesis during the acute phase of high-dose (>50 mg m−2) cisplatin-induced emesis in human patients [58, 65, 85, 124]. Overall, the acute phase of emesis induced by 5 mg kg−1 cisplatin represented poorly the clinical situation and the 4 h to 10 mg kg−1 model was more predictive of cisplatin-induced emesis in humans.
Overall, 5-HT3 receptor antagonists reduced the emetic response to the same extent during the acute and delayed phases, which contrasts with findings reported in the majority of clinical studies, describing limited or non-significant effect of 5-HT3 receptor antagonists during the delayed phase [57, 73]. This discrepancy may be explained by a difference in outcome usually measured in humans (daily incidence, percentage of patients developing emesis) and ferrets (severity, number of R+V). Even though daily incidence and severity (measured by visual analogue scale) of the delayed phase emesis appear to be positively correlated in the absence of anti-emetic therapy [72], they can be uncoupled following anti-emetic treatment and the number of emetic episodes may be reduced while the incidence remains unchanged [100]. Alternatively, it is conceivable that the delayed phase of emesis in the ferret is more sensitive to 5-HT3 receptor antagonists than it is in humans. The latter would be consistent with a longer acute phase in the ferret (see [110] for details), implying that the mechanism regulating the acute phase (i.e. 5-HT-mediated activation of the abdominal vagal afferents) remains activated longer. The ferret model thus correctly identified the anti-emetic potential of 5-HT3 receptor antagonists against both the acute and delayed phases of cisplatin-induced emesis, but the magnitude of the anti-emetic effect during the delayed phase appears greater in the ferret than it is in humans.
Methodology
In the present study, the methodology used in the meta-analysis of human clinical trials was modified and adapted to animal research, and several concessions had to be made. First of all, the criteria used to select studies for inclusion into the systematic review and meta-analysis, and assess quality, did not include randomization and blinding. Whereas these two parameters are considered essential for human clinical trials and it has been suggested that their absence favours positive findings in animal research [8], emesis is an objective measurement, which is not investigator-dependent and we have no reason to believe that the inclusion of such studies in our analysis biased our findings. Additionally, randomization and blinding in the identified studies were too rarely reported to be used as inclusion criteria. The exclusion criteria were chosen to ensure the collection of reliable, clearly defined data. The majority of excluded studies (see Table 2) were removed because emesis was not quantified as latency, retches, vomits and/or incidence. We chose not to include outcomes such as “emetic episodes” or “bouts of emesis” in the present analysis because of the disparity of definitions and possible interpretations. This may however restrict the conclusions of our study.
Secondly, whereas clinical trials usually report tens or hundreds of patients in each study arm, we found that in the cisplatin ferret model, typically 4 to 8 animals were allocated in each treatment group. This may limit the relevance of such an analysis, designed to compare much bigger samples. Additionally, because a majority of studies compared one control group to several treatment groups—typically different doses of a compound—in order to maintain the data from different doses as distinct comparisons, the number of animals in the control group was divided by the number of treatment groups it was compared to. The limitation of such an approach is that in the effect estimate calculation, the weight of such comparisons is reduced, which benefits comparisons extracted from studies that only compared one control group to one treatment group and is not justified by the quality of the studies.
Conclusions
We demonstrated the potential of a meta-analysis to address the 3R’s (Replacement, Refinement and Reduction), developed by Russel and Burch as criteria for a humane use of animals in research [126]. By maximising the utilisation of animal data, thus extracting novel scientific information without increasing the number of animals, such analysis addresses Reduction, as this reduces the future use of animals. Additionally, the effects of ondansetron on the 3 outcomes highlighted a logical Refinement of the model by reducing the observation period. The cisplatin 10 mg/kg to 4 h variant of the model stands out as the most appropriate to study the acute phase of cisplatin-induced emesis, whereas 5 mg/kg to 24–72 h remains the model of choice to study cisplatin-induced delayed emesis.
The present study is a proof of concept. In an attempt to focus the scope of the analysis, it was limited to an animal model with one emetic: cisplatin, one species: the ferret and one class of anti-emetic drugs: 5-HT3 receptor antagonists; the drugs investigated are already successfully used in humans against chemotherapy-induced emesis. Globally, the effects in the ferret were consistent with clinical findings, which were expected as they were originally developed in the ferret model; this demonstrates that a meta-analysis is an appropriate method to identify the anti-emetic potential of a drug and confirms that the ferret model of cisplatin-induced emesis is truly predictive and relevant to humans. This method can now be applied to investigate the effects of NK1 receptor antagonists, which were also developed using the ferret and which have recently been introduced into the clinic. However, recent studies suggest that there may be a discrepancy between the “broad spectrum” anti-emetic efficacy in the ferret and the efficacy in the clinic [3, 25]. This method can also be used in other “model” species (e.g. dog) to reassess “older” compounds such as dopamine receptor antagonists or opioids, whose effects on cisplatin-induced emesis are less well characterised. It can also be directly applied to other emetic models (different emetogen and/or different species) and adapted to assess the relevance of models arguably predictive of nausea and emesis such as pica in the rat and conditioned taste aversion [2, 77].
Acknowledgments
The authors would like to thank Carol Kilkenny (NC3Rs), Fiona Reid (SGUL) and Toby Lasserson (SGUL) for statistical advice, and Dr John Watson (Pfizer, USA), Dr Masahiko Hirafuji (University of Hokkaido, Japan) and Dr Hisashi Yamakuni (Astellas Pharma Inc., Japan), who provided original data. NPdS was supported by a PhD studentship from Merck Research Laboratories.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Abbreviations
- 5-HT3
5-Hydroxytryptamine3
- NK1
Neurokinin1
- i.v.
Intravenous
- i.p.
Intraperitoneal
- p.o.
Per os, oral
- s.c.
Sub-cutaneous
- R+V
Retches and vomits
- SD
Standard deviation
- CI
Confidence interval
References
- 1.Altman DG. Practical statistics for medical research. London: Chapman & Hall; 1991. [Google Scholar]
- 2.Andrews PLR, Horn CC. Signals for nausea and emesis: implications for models of upper gastrointestinal diseases. Auton Neurosci. 2006;125:100–115. doi: 10.1016/j.autneu.2006.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andrews PLR, Rudd JA. The role of tachykinins and the tachykinin NK1 receptor in nausea and emesis. In: Holzer P, editor. Handbook of experimental pharmacology. Berlin: Springer; 2004. [Google Scholar]
- 4.Angel I, Schoemaker H, Prouteau M, Garreau M, Langer SZ. Litoxetine: a selective 5-HT uptake inhibitor with concomitant 5-HT3 receptor antagonist and antiemetic properties. Eur J Pharmacol. 1993;232:139–145. doi: 10.1016/0014-2999(93)90767-c. [DOI] [PubMed] [Google Scholar]
- 5.Barnes JM, Barnes NM, Costall B, Naylor RJ, Tattersall FD. Reserpine, para-chlorophenylalanine and fenfluramine antagonise cisplatin-induced emesis in the ferret. Neuropharmacology. 1988;27:783–790. doi: 10.1016/0028-3908(88)90092-5. [DOI] [PubMed] [Google Scholar]
- 6.Barnes NM, Barry JM, Costall B, Naylor RJ, Tattersall FD. Antagonism by para-chlorophenylalanine of cisplatin-induced emesis. Br J Pharmacol. 1987;92:649P. [Google Scholar]
- 7.Barnes NM, Bunce KT, Naylor RJ, Rudd JA. The actions of fentanyl to inhibit drug-induced emesis. Neuropharmacology. 1991;30:1073–1083. doi: 10.1016/0028-3908(91)90136-y. [DOI] [PubMed] [Google Scholar]
- 8.Bebarta V, Luyten D, Heard K. Emergency medicine animal research: does use of randomization and blinding affect the results? Acad Emerg Med. 2003;10:684–687. doi: 10.1111/j.1553-2712.2003.tb00056.x. [DOI] [PubMed] [Google Scholar]
- 9.Bermudez J, Boyle EA, Miner WD, Sanger GJ. The anti-emetic potential of the 5-hydroxytryptamine3 receptor antagonist BRL 43694. Br J Cancer. 1988;58:644–650. doi: 10.1038/bjc.1988.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhandari P, Gupta YK, Seth SD, Chugh A. Emetic profile of cisplatin in dogs. Asia Pac J Pharmacol. 1988;3:131–133. [Google Scholar]
- 11.Bingham S, Blower PR, Davey PT, King PD, Sanger GJ, Wardle KA, Nishioka Y. Differences between the anti-emetic efficacies of the 5-HT3 receptor antagonists Granisetron and Azasetron in the conscious ferret. Pharmacometrics. 1994;47:21–28. [Google Scholar]
- 12.Blower PR. The role of specific 5-HT3 receptor antagonism in the control of cytostatic drug-induced emesis. Eur J Cancer. 1990;26(Suppl 1):S8–S11. [PubMed] [Google Scholar]
- 13.Blum E, Buchheit KH, Buecher HH, Gamse R, Kloeppner E, Meigel H, Papageorgiou C, Waelchli R, Revesz L. Design and synthesis of novel ligands for the 5-HT4 and the 5-HT4 receptor. Bioorg Med Chem Lett. 1992;2:461–466. [Google Scholar]
- 14.Borison HL, Wang SC. Physiology and pharmacology of vomiting. Pharmacol Rev. 1953;5:193–230. [PubMed] [Google Scholar]
- 15.Bountra C, Bunce K, Dale T, Gardner C, Jordan C, Twissell D, Ward P. Anti-emetic profile of a non-peptide neurokinin NK1 receptor antagonist, CP-99, 994, in ferrets. Eur J Pharmacol. 1993;249:R3–R4. doi: 10.1016/0014-2999(93)90673-6. [DOI] [PubMed] [Google Scholar]
- 16.Chevalier E, Singh L, Diop L. Anti-emetic effects of PD154075. Gastroenterology. 1998;114:A578. [Google Scholar]
- 17.Clark RD, Miller AB, Berger J, Repke DB, Weinhardt KK, Kowalczyk BA, Eglen RM, Bonhaus DW, Lee CH, Michel AD, et al. 2-(Quinuclidin-3-yl)pyrido[4, 3-b]indol-1-ones and isoquinolin-1-ones. Potent conformationally restricted 5-HT3 receptor antagonists. J Med Chem. 1993;36:2645–2657. doi: 10.1021/jm00070a008. [DOI] [PubMed] [Google Scholar]
- 18.Costall B, Domeney AM, Gunning SJ, Kelly ME, Naylor RJ, Nohria V, Owera-Atepo JB, Simpson KM, Tan CC, Tattersall D. The action of dazopride to enhance gastric emptying and block emesis. Neuropharmacology. 1987;26:669–677. doi: 10.1016/0028-3908(87)90227-9. [DOI] [PubMed] [Google Scholar]
- 19.Costall B, Domeney AM, Gunning SJ, Naylor RJ, Tattersall D, Tyers MB. GR38032F: a potent and novel inhibitor of cisplatin-induced emesis in the ferret. Br J Pharmacol. 1987;90:90P. [Google Scholar]
- 20.Costall B, Domeney AM, Naylor RJ, Owera-Atepo JB, Rudd JA, Tattersall FD. Fluphenazine, ICS 205–930 and dl-fenfluramine differentially antagonise drug-induced emesis in the ferret. Neuropharmacology. 1990;29:453–462. doi: 10.1016/0028-3908(90)90167-p. [DOI] [PubMed] [Google Scholar]
- 21.Costall B, Domeney AM, Naylor RJ, Tattersall FD. 5-Hydroxytryptamine M-receptor antagonism to prevent cisplatin-induced emesis. Neuropharmacology. 1986;25:959–961. doi: 10.1016/0028-3908(86)90030-4. [DOI] [PubMed] [Google Scholar]
- 22.Costall B, Domeney AM, Naylor RJ, Tattersall FD. Emesis induced by cisplatin in the ferret as a model for the detection of anti-emetic drugs. Neuropharmacology. 1987;26:1321–1326. doi: 10.1016/0028-3908(87)90094-3. [DOI] [PubMed] [Google Scholar]
- 23.Costall B, Naylor RJ, Tattersall FD. The actions of fenfluramine and interaction with 5-HT3 receptor-antagonists to inhibit emesis in the ferret. J Pharm Pharmacol. 1990;42:94–101. doi: 10.1111/j.2042-7158.1990.tb05361.x. [DOI] [PubMed] [Google Scholar]
- 24.Cubeddu LX, Hoffmann IS, Fuenmayor NT, Finn AL. Efficacy of ondansetron (GR 38032F) and the role of serotonin in cisplatin-induced nausea and vomiting. N Engl J Med. 1990;322:810–816. doi: 10.1056/NEJM199003223221204. [DOI] [PubMed] [Google Scholar]
- 25.Dando TM, Perry CM. Aprepitant: a review of its use in the prevention of chemotherapy-induced nausea and vomiting. Drugs. 2004;64:777–794. doi: 10.2165/00003495-200464070-00013. [DOI] [PubMed] [Google Scholar]
- 26.Davis CJ (1988) Neuropharmacological investigations into the mechanisms of emesis caused by cytotoxic drugs and radiation. Clinical pharmacology. Oxford University, PhD thesis
- 27.Delagrange P, Emerit MB, Merahi N, Abraham C, Morain P, Rault S, Renard P, Pfeiffer B, Guardiola-Lemaitre B, Hamon M. Interaction of S 21007 with 5-HT3 receptors. In vitro and in vivo characterization. Eur J Pharmacol. 1996;316:195–203. doi: 10.1016/s0014-2999(96)00680-2. [DOI] [PubMed] [Google Scholar]
- 28.DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28:105–114. doi: 10.1016/j.cct.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 29.Eglen RM, Bonhaus DW, Clark RD, Johnson LG, Lee CH, Leung E, Smith WL, Wong EH, Whiting RL. (R) and (S) RS 56532: mixed 5-HT3 and 5-HT4 receptor ligands with opposing enantiomeric selectivity. Neuropharmacology. 1994;33:515–526. doi: 10.1016/0028-3908(94)90083-3. [DOI] [PubMed] [Google Scholar]
- 30.Eglen RM, Lee CH, Smith WL, Johnson LG, Clark R, Whiting RL, Hegde SS. Pharmacological characterization of RS 25259–197, a novel and selective 5-HT3 receptor antagonist, in vivo. Br J Pharmacol. 1995;114:860–866. doi: 10.1111/j.1476-5381.1995.tb13283.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eglen RM, Lee CH, Smith WL, Johnson LG, Whiting RL, Hegde SS. RS 42358–197, a novel and potent 5-HT3 receptor antagonist, in vitro and in vivo. J Pharmacol Exp Ther. 1993;266:535–543. [PubMed] [Google Scholar]
- 32.Endo T, Minami M, Monma Y, Saito H, Takeuchi M. Emesis-related biochemical and histopathological changes induced by cisplatin in the ferret. J Toxicol Sci. 1990;15:235–244. doi: 10.2131/jts.15.235. [DOI] [PubMed] [Google Scholar]
- 33.Endo T, Minami M, Monma Y, Yoshioka M, Saito H, Kinami J, Toshimitsu Y, Parvez SH. Effect of GR38032F on cisplatin- and cyclophosphamide-induced emesis in the ferret. Biog Amines. 1990;7:525–533. [Google Scholar]
- 34.Endo T, Minami M, Monma Y, Yoshioka M, Saito H, Parvez SH. Vagotomy and ondansetron (5-HT3 antagonist) inhibited the increase of serotonin concentration induced by cytotoxic drugs in the area postreama of ferrets. Biog amines. 1992;9:163–175. [Google Scholar]
- 35.Endo T, Nemoto M, Minami M, Yoshioka M, Saito H, Parvez SH. Changes in the afferent abdominal vagal nerve activity induced by cisplatin and copper sulfate in the ferret. Biog Amines. 1995;11:399–407. [Google Scholar]
- 36.Endo T, Nemoto M, Monma Y, Hamaue N, Togashi M, Hirafuji M. Combined effect of domperidone and granisetron on cisplatin-induced emesis in the ferret. Pharmacometrics. 1994;47:435–442. [Google Scholar]
- 37.European Medicines Agency (2006) Guideline on non-clinical and clinical development of medicinal products for the treatment of nausea and vomiting associated with cancer chemotherapy. CPMP/EWP/4937/03. In: EMEA (ed) London, UK
- 38.Fink-Jensen A, Judge ME, Hansen JB, Jacobsen P, Turski L, Olney J, Honore T. Inhibition of cisplatin-induced emesis in ferrets by the non-NMDA receptor antagonists NBQX and CNQX. Neurosci Lett. 1992;137:173–177. doi: 10.1016/0304-3940(92)90397-p. [DOI] [PubMed] [Google Scholar]
- 39.Fitzpatrick LR, Lambert RM, Pendley CE, Martin GE, Bostwick JS, Gessner GW, Airey JE, Youssefyeh RD, Pendleton RG, Decktor DL. RG 12915: a potent 5-hydroxytryptamine-3 antagonist that is an orally effective inhibitor of cytotoxic drug-induced emesis in the ferret and dog. J Pharmacol Exp Ther. 1990;254:450–455. [PubMed] [Google Scholar]
- 40.Florczyk AP, Schurig JE, Bradner WT. Cisplatin-induced emesis in the Ferret: a new animal model. Cancer Treat Rep. 1982;66:187–189. [PubMed] [Google Scholar]
- 41.Florczyk AP, Schurig JE, Lenaz L, Bradner WT. the ferret: a new animal model of cis-platinum induced emesis. Proc Am Assoc Canc Res. 1981;22:228. [Google Scholar]
- 42.Fukunaka N, Sagae S, Kudo R, Endo T, Hirafuji M, Minami M. Effects of granisetron and its combination with dexamethasone on cisplatin-induced delayed emesis in the ferret. Gen Pharmacol. 1998;31:775–781. doi: 10.1016/s0306-3623(98)00102-5. [DOI] [PubMed] [Google Scholar]
- 43.Gandara, Harvey WH, Monaghan GG, Perez EA, Hesketh PJ. Delayed emesis following high-dose cisplatin: a double-blind randomised comparative trial of ondansetron (GR 38032F) versus placebo. Eur J Cancer. 1993;29A(Suppl 1):S35–S38. doi: 10.1016/s0959-8049(05)80259-x. [DOI] [PubMed] [Google Scholar]
- 44.Gardner CJ, Armour DR, Beattie DT, Gale JD, Hawcock AB, Kilpatrick GJ, Twissell DJ, Ward P. GR205171: a novel antagonist with high affinity for the tachykinin NK1 receptor, and potent broad-spectrum anti-emetic activity. Regul Pept. 1996;65:45–53. doi: 10.1016/0167-0115(96)00071-7. [DOI] [PubMed] [Google Scholar]
- 45.Gardner CJ, Bountra C, Bunce KT, Dale TJ, Jordan CC, Twissell DJ, Ward P. Anti-emetic activity of neurokinin NK1 receptor antagonists is mediated centrally. Br J Pharmacol. 1994;112:516P. [Google Scholar]
- 46.Gardner CJ, Twissell DJ, Dale TJ, Gale JD, Jordan CC, Kilpatrick GJ, Bountra C, Ward P. The broad-spectrum anti-emetic activity of the novel non-peptide tachykinin NK1 receptor antagonist GR203040. Br J Pharmacol. 1995;116:3158–3163. doi: 10.1111/j.1476-5381.1995.tb15118.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gonsalves S, Watson J, Ashton C. Broad spectrum antiemetic effects of CP-122, 721, a tachykinin NK1 receptor antagonist, in ferrets. Eur J Pharmacol. 1996;305:181–185. doi: 10.1016/0014-2999(96)00216-6. [DOI] [PubMed] [Google Scholar]
- 48.Gooch CL, Boissonade FM, Grundy D. Somatostatin analogue octreotide inhibits retching to cisplatin in anaesthetised ferret. Gastroenterology. 1998;114:A1147. [Google Scholar]
- 49.Gylys JA, Wright RN, Nicolosi WD, Buyniski JP, Crenshaw RR. BMY-25801, an antiemetic agent free of D2-dopamine receptor antagonist properties. J Pharmacol Exp Ther. 1988;244:830–837. [PubMed] [Google Scholar]
- 50.Haga K, Inaba K, Shoji H, Morimoto Y, Fukuda T, Setoguchi M. The effects of orally administered Y-25130, a selective serotonin3-receptor antagonist, on chemotherapeutic agent-induced emesis. Jpn J Pharmacol. 1993;63:377–383. doi: 10.1254/jjp.63.377. [DOI] [PubMed] [Google Scholar]
- 51.Haga K, Inaba K, Syoji H. The effect of azasetron hydrochloride (serotone (TM)) on delayed emesis induced by a chemotherapeutic agent, cisplatin. Jpn Pharmacol Ther. 2000;28:285–290. [Google Scholar]
- 52.Hale JJ, Mills SG, MacCoss M, Dorn CP, Finke PE, Budhu RJ, Reamer RA, Huskey SE, Luffer-Atlas D, Dean BJ, McGowan EM, Feeney WP, Chiu SH, Cascieri MA, Chicchi GG, Kurtz MM, Sadowski S, Ber E, Tattersall FD, Rupniak NM, Williams AR, Rycroft W, Hargreaves R, Metzger JM, MacIntyre DE. Phosphorylated morpholine acetal human neurokinin-1 receptor antagonists as water-soluble prodrugs. J Med Chem. 2000;43:1234–1241. doi: 10.1021/jm990617v. [DOI] [PubMed] [Google Scholar]
- 53.Hale JJ, Mills SG, MacCoss M, Finke PE, Cascieri MA, Sadowski S, Ber E, Chicchi GG, Kurtz M, Metzger J, Eiermann G, Tsou NN, Tattersall FD, Rupniak NM, Williams AR, Rycroft W, Hargreaves R, MacIntyre DE. Structural optimization affording 2-(R)-(1-(R)-3, 5-bis(trifluoromethyl)phenylethoxy)-3-(S)-(4-fluoro)phenyl-4-(3-oxo-1, 2, 4-triazol-5-yl)methylmorpholine, a potent, orally active, long-acting morpholine acetal human NK-1 receptor antagonist. J Med Chem. 1998;41:4607–4614. doi: 10.1021/jm980299k. [DOI] [PubMed] [Google Scholar]
- 54.Hargreaves R, Tattersall D, Rycroft W, Woodford K, Ladduwahetty T, Keown L, Merchant K, Swain C, MacLeod AM, Baker R, Francis B, Burns D, Cascieri M, Metzger J, MacIntyre DE, Williamson DJ, Iversen LL, Hill RG. Evidence that the anti-emetic effects of NK1 receptor antagonists are centrally mediated. Can J Physiol Pharmacol. 1994;72(suppl 2):45. [Google Scholar]
- 55.Harris AL, Cantwell BMJ. Mechanisms and treatment of cytotoxic-induced nausea and vomiting. In: Davis CJ, Lake-Bakaar GV, Grahame-Smith DG, editors. Nausea and vomiting: mechanisms and treatment. Berlin: Springer; 1986. pp. 78–93. [Google Scholar]
- 56.Hawthorn J, Ostler KJ, Andrews PLR. The role of the abdominal visceral innervation and 5-hydroxytryptamine M-receptors in vomiting induced by the cytotoxic drugs cyclophosphamide and cis-platin in the ferret. Q J Exp Physiol. 1988;73:7–21. doi: 10.1113/expphysiol.1988.sp003124. [DOI] [PubMed] [Google Scholar]
- 57.Hesketh PJ. Management of nausea and vomiting in cancer and cancer treatment. Sudbury: Jones and Barlett Publishers Inc.; 2005. [Google Scholar]
- 58.Hesketh PJ, Murphy WK, Lester EP, Gandara DR, Khojasteh A, Tapazoglou E, Sartiano GP, White DR, Werner K, Chubb JM. GR 38032F (GR-C507/75): a novel compound effective in the prevention of acute cisplatin-induced emesis. J Clin Oncol. 1989;7:700–705. doi: 10.1200/JCO.1989.7.6.700. [DOI] [PubMed] [Google Scholar]
- 59.Higgins GA, Kilpatrick GJ, Bunce KT, Jones BJ, Tyers MB. 5-HT3 receptor antagonists injected into the area postrema inhibit cisplatin-induced emesis in the ferret. Br J Pharmacol. 1989;97:247–255. doi: 10.1111/j.1476-5381.1989.tb11948.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hollingworth GJ, Carlson EJ, Castro JL, Chicchi GG, Clark N, Cooper LC, Dirat O, Salvo JD, Elliott JM, Kilburn R, Kurtz MM, Rycroft W, Tattersall FD, Tsao KL, Swain CJ. Novel lactam NK1 antagonists with anti-emetic activity. Bioorg Med Chem Lett. 2006;16:1197–1201. doi: 10.1016/j.bmcl.2005.11.111. [DOI] [PubMed] [Google Scholar]
- 61.Holmes AM, Rudd JA, Tattersall FD, Aziz Q, Andrews PLR. Opportunities for the replacement of animals in the study of nausea and vomiting. Br J Pharmacol. 2009;157:865–880. doi: 10.1111/j.1476-5381.2009.00176.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Horn J, de Haan RJ, Vermeulen M, Luiten PG, Limburg M. Nimodipine in animal model experiments of focal cerebral ischemia: a systematic review. Stroke. 2001;32:2433–2438. doi: 10.1161/hs1001.096009. [DOI] [PubMed] [Google Scholar]
- 63.Horn J, Limburg M. Calcium antagonists for ischemic stroke: a systematic review. Stroke. 2001;32:570–576. doi: 10.1161/01.str.32.2.570. [DOI] [PubMed] [Google Scholar]
- 64.Ito T, Yoshida N, Miura Y, Omoya H, Karasawa T. Antiemetic effects of AS-5370, a novel serotonin 5-HT3 receptor antagonist. Eur J Pharmacol. 1990;183:1214–1215. [Google Scholar]
- 65.Jantunen IT, Kataja VV, Muhonen TT. An overview of randomised studies comparing 5-HT3 receptor antagonists to conventional anti-emetics in the prophylaxis of acute chemotherapy-induced vomiting. Eur J Cancer. 1997;33:66–74. doi: 10.1016/s0959-8049(96)00276-6. [DOI] [PubMed] [Google Scholar]
- 66.Kamato T, Ito H, Nagakura Y, Nishida A, Yuki H, Yamano M, Miyata K. Mechanisms of cisplatin- and m-chlorophenylbiguanide-induced emesis in ferrets. Eur J Pharmacol. 1993;238:369–376. doi: 10.1016/0014-2999(93)90868-i. [DOI] [PubMed] [Google Scholar]
- 67.Kamato T, Miyata K, Ito H, Yuki H, Yamano M, Honda K. Antiemetic effects of YM060, a potent and selective serotonin (5HT)3-receptor antagonist, in ferrets and dogs. Jpn J Pharmacol. 1991;57:387–395. doi: 10.1254/jjp.57.387. [DOI] [PubMed] [Google Scholar]
- 68.Kilkenny C (2008) Systematic reviews of animal research. Available online at: http://www.nc3rs.org.uk/downloaddoc.asp?id=695
- 69.Kim JH, Yoon IS, Lee BH, Choi SH, Lee JH, Lee JH, Jeong SM, Kim SC, Park CK, Lee SM, Nah SY. Effects of Korean red ginseng extract on cisplatin-induced nausea and vomiting. Arch Pharm Res. 2005;28:680–684. doi: 10.1007/BF02969358. [DOI] [PubMed] [Google Scholar]
- 70.King AG, Sanger GJ. Effect of a selective and potent central nervous system penetrant, neurokinin-3 receptor antagonist (SB-222200), on cisplatin-induced emesis in the ferret. Neurosci Lett. 2005;376:5–8. doi: 10.1016/j.neulet.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 71.Kris MG, Cubeddu LX, Gralla RJ, Cupissol D, Tyson LB, Venkatraman E, Homesley HD. Are more antiemetic trials with a placebo necessary? Report of patient data from randomized trials of placebo antiemetics with cisplatin. Cancer. 1996;78:2193–2198. doi: 10.1002/(sici)1097-0142(19961115)78:10<2193::aid-cncr22>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 72.Kris MG, Gralla RJ, Clark RA, Tyson LB, O’Connell JP, Wertheim MS, Kelsen DP. Incidence, course, and severity of delayed nausea and vomiting following the administration of high-dose cisplatin. J Clin Oncol. 1985;3:1379–1384. doi: 10.1200/JCO.1985.3.10.1379. [DOI] [PubMed] [Google Scholar]
- 73.Kubota Y, Mihara K, Ishii F, Ohno K, Ogata H, Makimura M, Kikuchi N, Kitano T. Effectiveness of anti-emetics for the prophylaxis of cisplatin-induced delayed emesis: a systematic review. Yakugaku Zasshi. 2004;124:1–11. doi: 10.1248/yakushi.124.1. [DOI] [PubMed] [Google Scholar]
- 74.Lasheras B, Berjon A, Montanes R, Roca J, Romero G, Ramirez MJ, Del Rio J. Pharmacological properties of quinoxaline derivatives as a new class of 5-HT3 receptor antagonists. Arzneimittelforschung. 1996;46:401–406. [PubMed] [Google Scholar]
- 75.Lau AH, Kan KK, Lai HW, Ngan MP, Rudd JA, Wai MK, Yew DT. Action of ondansetron and CP-99, 994 to modify behavior and antagonize cisplatin-induced emesis in the ferret. Eur J Pharmacol. 2005;506:241–247. doi: 10.1016/j.ejphar.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 76.Lehmann A, Karrberg L. Effects of N-methyl-D-aspartate receptor antagonists on cisplatin-induced emesis in the ferret. Neuropharmacology. 1996;35:475–481. doi: 10.1016/0028-3908(96)00008-1. [DOI] [PubMed] [Google Scholar]
- 77.Liu YL, Malik NM, Sanger GJ, Andrews PL. Ghrelin alleviates cancer chemotherapy-associated dyspepsia in rodents. Cancer Chemother Pharmacol. 2006;58:326–333. doi: 10.1007/s00280-005-0179-0. [DOI] [PubMed] [Google Scholar]
- 78.Macleod MR, O’Collins T, Horky LL, Howells DW, Donnan GA. Systematic review and meta-analysis of the efficacy of melatonin in experimental stroke. J Pineal Res. 2005;38:35–41. doi: 10.1111/j.1600-079X.2004.00172.x. [DOI] [PubMed] [Google Scholar]
- 79.Macleod MR, O’Collins T, Horky LL, Howells DW, Donnan GA. Systematic review and metaanalysis of the efficacy of FK506 in experimental stroke. J Cereb Blood Flow Metab. 2005;25:713–721. doi: 10.1038/sj.jcbfm.9600064. [DOI] [PubMed] [Google Scholar]
- 80.Macleod MR, O’Collins T, Howells DW, Donnan GA. Pooling of animal experimental data reveals influence of study design and publication bias. Stroke. 2004;35:1203–1208. doi: 10.1161/01.STR.0000125719.25853.20. [DOI] [PubMed] [Google Scholar]
- 81.Marr HE, Davey PT, Blower PR. The effect of dexamethasone, alone or in combination with granisetron, on cisplatin-induced emesis in the ferret. Br J Pharmacol. 1992;104:371P. [Google Scholar]
- 82.Marr HE, Davey PT, Boyle EA, Blower PR. Further studies of the antiemetic activity of granisetron against whole body X-irradiation or cisplatin-induced emesis in the ferret. Pharmacology. 1994;48:283–292. doi: 10.1159/000139191. [DOI] [PubMed] [Google Scholar]
- 83.Marr HE, Davey PT, Boyle EA, Blower PR. The antiemetic activity of granisetron against cytostatic-treatment-induced emesis in 10- to 13-week-old ferrets. J Cancer Res Clin Oncol. 1994;120:204–207. doi: 10.1007/BF01372557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Martin M. The severity and pattern of emesis following different cytotoxic agents. Oncology. 1996;53(Suppl 1):26–31. doi: 10.1159/000227637. [DOI] [PubMed] [Google Scholar]
- 85.Marty M, Kleisbauer JP, Fournel P, Vergnenegre A, Carles P, Loria-Kanza Y, Simonetta C, de Bruijn KM. Is Navoban (tropisetron) as effective as Zofran (ondansetron) in cisplatin-induced emesis? The French Navoban Study Group. Anticancer Drugs. 1995;6(Suppl 1):15–21. [PubMed] [Google Scholar]
- 86.Matsui T, Sugiura T, Nakai H, Iguchi S, Shigeoka S, Takada H, Odagaki Y, Nagao Y, Ushio Y, Ohmoto K, et al. Novel 5-HT3 antagonists. Isoquinolinones and 3-aryl-2-pyridones. J Med Chem. 1992;35:3307–3319. doi: 10.1021/jm00096a001. [DOI] [PubMed] [Google Scholar]
- 87.Matthews JN, Altman DG. Interaction 3: How to examine heterogeneity. BMJ. 1996;313:862. doi: 10.1136/bmj.313.7061.862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Matthews RA. Medical progress depends on animal models—doesn’t it? J R Soc Med. 2008;101:95–98. doi: 10.1258/jrsm.2007.070164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.McCarthy LE, Borison HL. Respiratory mechanics of vomiting in decerebrate cats. Am J Physiol. 1974;226:738–743. doi: 10.1152/ajplegacy.1974.226.3.738. [DOI] [PubMed] [Google Scholar]
- 90.Miller RC, Galvan M, Gittos MW, Van Giersbergen PLM, Moser PC, Fozard JR. Pharmacological properties of dolasetron, a potent and selective antagonist at 5-HT3 receptors. Drug Dev Res. 1993;28:87–93. [Google Scholar]
- 91.Minami M, Endo T, Kikuchi K, Ihira E, Hirafuji M, Hamaue N, Monma Y, Sakurada T, Tan-no K, Kisara K. Antiemetic effects of sendide, a peptide tachykinin NK1 receptor antagonist, in the ferret. Eur J Pharmacol. 1998;363:49–55. doi: 10.1016/s0014-2999(98)00784-5. [DOI] [PubMed] [Google Scholar]
- 92.Minami M, Endo T, Monma Y, Shiroshita Y. Pharmacoogy of emesis induced by anti cancer drugs. J Toxicol Sci. 1991;16(suppl 2):35–39. [Google Scholar]
- 93.Minami M, Endo T, Tamakai H, Ogawa T, Hamaue N, Hirafuji M, Monma Y, Yoshioka M, Hagihara K. Antiemetic effects of N-3389, a newly synthesized 5-HT3 and 5-HT4 receptor antagonist, in ferrets. Eur J Pharmacol. 1997;321:333–342. doi: 10.1016/s0014-2999(96)00974-0. [DOI] [PubMed] [Google Scholar]
- 94.Miner WD, Sanger GJ. Inhibition of cisplatin-induced vomiting by selective 5-hydroxytryptamine M-receptor antagonism. Br J Pharmacol. 1986;88:497–499. doi: 10.1111/j.1476-5381.1986.tb10228.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Miner WD, Sanger GJ, Turner DH. Comparison of the effect of BRL 24924, metoclopramide and domperidone on cisplatin-induced emesis in the ferret. Br J Pharmacol. 1986;88:374P. [Google Scholar]
- 96.Miner WD, Sanger GJ, Turner DH. Evidence that 5-hydroxytryptamine3 receptors mediate cytotoxic drug and radiation-evoked emesis. Br J Cancer. 1987;56:159–162. doi: 10.1038/bjc.1987.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of reporting of meta-analyses. Lancet. 1999;354:1896–1900. doi: 10.1016/s0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- 98.Monkovic I, Willner D, Adam MA, Brown M, Crenshaw RR, Fuller CE, Juby PF, Luke GM, Matiskella JA, Montzka TA. Substituted benzamides. 1. Potential nondopaminergic antagonists of chemotherapy-induced nausea and emesis. J Med Chem. 1988;31:1548–1558. doi: 10.1021/jm00403a011. [DOI] [PubMed] [Google Scholar]
- 99.Nakayama H, Yamakuni H, Higaki M, Ishikawa H, Imazumi K, Matsuo M, Mutoh S. Antiemetic activity of FK1052, a 5-HT3- and 5-HT4-receptor antagonist, in Suncus murinus and ferrets. J Pharmacol Sci. 2005;98:396–403. doi: 10.1254/jphs.fpj05001x. [DOI] [PubMed] [Google Scholar]
- 100.Navari RM, Madajewicz S, Anderson N, Tchekmedyian NS, Whaley W, Garewal H, Beck TM, Chang AY, Greenberg B, Caldwell KC, et al. Oral ondansetron for the control of cisplatin-induced delayed emesis: a large, multicenter, double-blind, randomized comparative trial of ondansetron versus placebo. J Clin Oncol. 1995;13:2408–2416. doi: 10.1200/JCO.1995.13.9.2408. [DOI] [PubMed] [Google Scholar]
- 101.Nuffield Council on Bioethics (2005) The ethics of research involving animals. In: Bioethics NCo (ed) London
- 102.Ohta M, Suzuki T, Furuya T, Kurihara H, Tokunaga T, Miyata K, Yanagisawa I. Novel 5-hydroxytryptamine (5-HT3) receptor antagonists. III. Pharmacological evaluations and molecular modeling studies of optically active 4,5,6,7-tetrahydro-1H-benzimidazole derivatives. Chem Pharm Bull (Tokyo) 1996;44:1707–1716. doi: 10.1248/cpb.44.1707. [DOI] [PubMed] [Google Scholar]
- 103.Ozaki A, Sukamoto T. Improvement of cisplatin-induced emesis and delayed gastric emptying by KB-R6933, a novel 5-HT3 receptor antagonist. Gen Pharmacol. 1999;33:283–288. doi: 10.1016/s0306-3623(98)00286-9. [DOI] [PubMed] [Google Scholar]
- 104.Percie du Sert N, Rudd JA, Moss R, Andrews PL. The delayed phase of cisplatin-induced emesis is mediated by the area postrema and not the abdominal visceral innervation in the ferret. Neurosci Lett. 2009;465:16–20. doi: 10.1016/j.neulet.2009.08.075. [DOI] [PubMed] [Google Scholar]
- 105.Pound P, Ebrahim S, Sandercock P, Bracken MB, Roberts I. Where is the evidence that animal research benefits humans? BMJ. 2004;328:514–517. doi: 10.1136/bmj.328.7438.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Preziosi P, D’Amato M, Del Carmine R, Martire M, Pozzoli G, Navarra P. The effects of 5-HT3 receptor antagonists on cisplatin-induced emesis in the pigeon. Eur J Pharmacol. 1992;221:343–350. doi: 10.1016/0014-2999(92)90721-f. [DOI] [PubMed] [Google Scholar]
- 107.Price MT, Olney JE. Excitatory amino acid antagonists as anti-emetics. Soc Neurosci Abstr. 1990;16:377. [Google Scholar]
- 108.Reynolds DJ, Barber NA, Grahame-Smith DG, Leslie RA. Cisplatin-evoked induction of c-fos protein in the brainstem of the ferret: the effect of cervical vagotomy and the anti-emetic 5-HT3 receptor antagonist granisetron (BRL 43694) Brain Res. 1991;565:231–236. doi: 10.1016/0006-8993(91)91654-j. [DOI] [PubMed] [Google Scholar]
- 109.Roila F, Hesketh PJ, Herrstedt J. Prevention of chemotherapy- and radiotherapy-induced emesis: results of the 2004 Perugia International Antiemetic Consensus Conference. Ann Oncol. 2006;17:20–28. doi: 10.1093/annonc/mdj078. [DOI] [PubMed] [Google Scholar]
- 110.Rudd JA, Andrews PLR. Mechanisms of acute and delayed Nausea and vomiting induced by anticancer therapies. In: Hesketh P, editor. Management of Nausea and vomiting in cancer and cancer treatment. Sudbury: Jones and Barlett Publishers, Inc.; 2005. pp. 15–66. [Google Scholar]
- 111.Rudd JA, Bunce KT, Naylor RJ. The effect of 8-OH-DPAT on drug-induced emesis in the ferret. Br J Pharmacol. 1992;106:101P. [Google Scholar]
- 112.Rudd JA, Bunce KT, Naylor RJ. The interaction of dexamethasone with ondansetron on drug-induced emesis in the ferret. Neuropharmacology. 1996;35:91–97. doi: 10.1016/0028-3908(95)00137-9. [DOI] [PubMed] [Google Scholar]
- 113.Rudd JA, Cheng CH, Naylor RJ. Serotonin-independent model of cisplatin-induced emesis in the ferret. Jpn J Pharmacol. 1998;78:253–260. doi: 10.1254/jjp.78.253. [DOI] [PubMed] [Google Scholar]
- 114.Rudd JA, Jordan CC, Naylor RJ. Profiles of emetic action of cisplatin in the ferret: a potential model of acute and delayed emesis. Eur J Pharmacol. 1994;262:R1–R2. doi: 10.1016/0014-2999(94)90048-5. [DOI] [PubMed] [Google Scholar]
- 115.Rudd JA, Jordan CC, Naylor RJ. The action of the NK1 tachykinin receptor antagonist, CP 99, 994, in antagonizing the acute and delayed emesis induced by cisplatin in the ferret. Br J Pharmacol. 1996;119:931–936. doi: 10.1111/j.1476-5381.1996.tb15761.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rudd JA, Kan KW, Ngan MP, Okuno T, Sam TS (2001) Anti-emetic action of intranasally administered metoclopramide in the ferret. Presented at: 7th Hong Kong Pharmacology Society Scientific meeting in Association with the Zhjiang Pharmacological Society, Hong Kong, China, 16–18 October
- 117.Rudd JA, Naylor RJ. Effects of 5-HT3 receptor antagonists on models of acute and delayed emesis induced by cisplatin in the ferret. Neuropharmacology. 1994;33:1607–1608. doi: 10.1016/0028-3908(94)90136-8. [DOI] [PubMed] [Google Scholar]
- 118.Rudd JA, Naylor RJ. Modulation of emesis by 5HT1A receptors. Pathophysiology. 1994;1:267–268. [Google Scholar]
- 119.Rudd JA, Naylor RJ. An interaction of ondansetron and dexamethasone antagonizing cisplatin-induced acute and delayed emesis in the ferret. Br J Pharmacol. 1996;118:209–214. doi: 10.1111/j.1476-5381.1996.tb15388.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Rudd JA, Naylor RJ. The actions of ondansetron and dexamethasone to antagonise cisplatin-induced emesis in the ferret. Eur J Pharmacol. 1997;322:79–82. doi: 10.1016/s0014-2999(97)00073-3. [DOI] [PubMed] [Google Scholar]
- 121.Rudd JA, Ngan MP, Wai MK. 5-HT3 receptors are not involved in conditioned taste aversions induced by 5-hydroxytryptamine, ipecacuanha or cisplatin. Eur J Pharmacol. 1998;352:143–149. doi: 10.1016/s0014-2999(98)00359-8. [DOI] [PubMed] [Google Scholar]
- 122.Rudd JA, Ngan MP, Wai MK, King AG, Witherington J, Andrews PLR, Sanger GJ. Anti-emetic activity of ghrelin in ferrets exposed to the cytotoxic anti-cancer agent cisplatin. Neurosci Lett. 2006;392:79–83. doi: 10.1016/j.neulet.2005.08.062. [DOI] [PubMed] [Google Scholar]
- 123.Rudd JA, Sam TS, Ngan MP. A COX and LOX inhibitor regimen fails to mimic the action of dexamethasone on cisplatin-induced acute and delayed emesis in the Ferret. Beijing: IUPHAR-2006; 2006. [Google Scholar]
- 124.Ruff P, Paska W, Goedhals L, Pouillart P, Riviere A, Vorobiof D, Bloch B, Jones A, Martin C, Brunet R, et al. Ondansetron compared with granisetron in the prophylaxis of cisplatin-induced acute emesis: a multicentre double-blind, randomised, parallel-group study. The Ondansetron and Granisetron Emesis Study Group. Oncology. 1994;51:113–118. doi: 10.1159/000227321. [DOI] [PubMed] [Google Scholar]
- 125.Rupniak NM, Tattersall FD, Williams AR, Rycroft W, Carlson EJ, Cascieri MA, Sadowski S, Ber E, Hale JJ, Mills SG, MacCoss M, Seward E, Huscroft I, Owen S, Swain CJ, Hill RG, Hargreaves RJ. In vitro and in vivo predictors of the anti-emetic activity of tachykinin NK1 receptor antagonists. Eur J Pharmacol. 1997;326:201–209. doi: 10.1016/s0014-2999(97)85415-5. [DOI] [PubMed] [Google Scholar]
- 126.Russell WM, Burch RL (1959) The principles of humane experimental technique. Universities Federation For Animal Welfare (UFAW)
- 127.Rycroft W, Tattersall D, Ber E, Cascieri M, Hale JJ, Hill RG, MacCoss M, Mills SG, Sadowski S, Hargreaves R (1996) The anti-emetic actions of L-742,694, poster
- 128.Sam TS, Chan SW, Rudd JA, Yeung JH. Action of glucocorticoids to antagonise cisplatin-induced acute and delayed emesis in the ferret. Eur J Pharmacol. 2001;417:231–237. doi: 10.1016/s0014-2999(01)00915-3. [DOI] [PubMed] [Google Scholar]
- 129.Sam TS, Kan KK, Ngan MP, Rudd JA, Yeung JH. Action of metyrapone and tetracosactrin to modify cisplatin-induced acute and delayed emesis in the ferret. Eur J Pharmacol. 2003;466:163–168. doi: 10.1016/s0014-2999(03)01550-4. [DOI] [PubMed] [Google Scholar]
- 130.Sam TS, Ngan MP, Riendeau D, Robichaud A, Rudd JA. Action of cyclooxygenase inhibitors and a leukotriene biosynthesis inhibitor on cisplatin-induced acute and delayed emesis in the ferret. J Pharmacol Sci. 2007;103:189–200. doi: 10.1254/jphs.fp0061169. [DOI] [PubMed] [Google Scholar]
- 131.Schurig JE, Florczyk AP, Rose WC, Bradner WT. Antiemetic activity of butorphanol against cisplatin-induced emesis in ferrets and dogs. Cancer Treat Rep. 1982;66:1831–1835. [PubMed] [Google Scholar]
- 132.Shiroshita Y, Minami M, Endo T, Monma Y, Asaka M, Itoh H, Ikeda T, Matsumoto H, Satoh T. The protective effect of 4-hydroxy-2-methyl-N-[2-(tetrazol-5-yl)- phenyl]-2H–1, 2-benzothiazine-3-carboxamide-1, 1-dioxide monosodium salt (HX-1920) on cisplatin-induced toxicity in rats. J Toxicol Sci. 1993;18:31–41. doi: 10.2131/jts.18.31. [DOI] [PubMed] [Google Scholar]
- 133.Shiroshita Y, Minami M, Endo T, Takahashi M, Monma Y, Hiromishi I, Yokoyama R, Matsumoto K. Effects of HX-1920 on cisplatin-induced toxicity in mice, rat and ferrets. Jpn J Pharmacol. 1992;58:419P. [Google Scholar]
- 134.Singh L, Field MJ, Hughes J, Kuo BS, Suman-Chauhan N, Tuladhar BR, Wright DS, Naylor RJ. The tachykinin NK1 receptor antagonist PD 154075 blocks cisplatin-induced delayed emesis in the ferret. Eur J Pharmacol. 1997;321:209–216. doi: 10.1016/s0014-2999(96)00950-8. [DOI] [PubMed] [Google Scholar]
- 135.Spina D. The potential of PDE4 inhibitors in respiratory disease. Curr Drug Targets Inflamm Allergy. 2004;3:231–236. doi: 10.2174/1568010043343822. [DOI] [PubMed] [Google Scholar]
- 136.Stables R, Andrews PLR, Bailey HE, Costall B, Gunning SJ, Hawthorn J, Naylor RJ, Tyers MB. Antiemetic properties of the 5HT3-receptor antagonist, GR38032F. Cancer Treat Rev. 1987;14:333–336. doi: 10.1016/0305-7372(87)90026-0. [DOI] [PubMed] [Google Scholar]
- 137.Taniguchi S, Hagihara K, Hamada T, Minami M, Endo T, Tsuchiyama M. The inhibitory action of indisetron hydrochloride, a 5-HT3 receptor antagonist, against the anticancer drug-induced emesis in the dog, ferret and suncus. Jpn Pharmacol Ther. 2004;32:799–806. [Google Scholar]
- 138.Tattersall D, Dourish CT, Duchnowski M, Swain C, Iversen SD. The anti-emetic action of the novel 5-HT3 receptor antagonist L-683, 877 in the ferret. Eur J Pharmacol. 1990;183:1966–1967. [Google Scholar]
- 139.Tattersall D, Newberry N, Beer MS, Rigby M, Gilbert M, Maguire JJ, Mudukotuwa N, Duchnowski M, MacKnight AT, Swain C, Kneen C, Dourish CT. L-683, 877: Pharmacological Profile of a Novel 5-HT3 Receptor Antagonist. Drug Dev Res. 1992;25:17–28. [Google Scholar]
- 140.Tattersall FD, Rycroft W, Cumberbatch M, Mason G, Tye S, Williamson DJ, Hale JJ, Mills SG, Finke PE, MacCoss M, Sadowski S, Ber E, Cascieri M, Hill RG, MacIntyre DE, Hargreaves RJ. The novel NK1 receptor antagonist MK-0869 (L-754, 030) and its water soluble phosphoryl prodrug, L-758, 298, inhibit acute and delayed cisplatin-induced emesis in ferrets. Neuropharmacology. 2000;39:652–663. doi: 10.1016/s0028-3908(99)00172-0. [DOI] [PubMed] [Google Scholar]
- 141.Tattersall FD, Rycroft W, Francis B, Pearce D, Merchant K, MacLeod AM, Ladduwahetty T, Keown L, Swain C, Baker R, Cascieri M, Ber E, Metzger J, MacIntyre DE, Hill RG, Hargreaves RJ. Tachykinin NK1 receptor antagonists act centrally to inhibit emesis induced by the chemotherapeutic agent cisplatin in ferrets. Neuropharmacology. 1996;35:1121–1129. doi: 10.1016/s0028-3908(96)00020-2. [DOI] [PubMed] [Google Scholar]
- 142.Tattersall FD, Rycroft W, Hargreaves RJ, Hill RG. The tachykinin NK1 receptor antagonist CP-99, 994 attenuates cisplatin induced emesis in the ferret. Eur J Pharmacol. 1993;250:R5–R6. doi: 10.1016/0014-2999(93)90649-3. [DOI] [PubMed] [Google Scholar]
- 143.The Cochrane Collaboration® (2002) Open Learning Material
- 144.Tsuchiya M, Fujiwara Y, Kanai Y, Mizutani M, Shimada K, Suga O, Ueda S, Watson JW, Nagahisa A. Anti-emetic activity of the novel nonpeptide tachykinin NK1 receptor antagonist ezlopitant (CJ-11, 974) against acute and delayed cisplatin-induced emesis in the ferret. Pharmacology. 2002;66:144–152. doi: 10.1159/000063796. [DOI] [PubMed] [Google Scholar]
- 145.Twissell DJ, Bountra C, Bunce KT, Dale TJ, Gardner CJ, Jordan CC, Ward P (1993) Anti-emetic properties of a non-peptide neurokinin NK1 antagonist, CP-99,994, in ferrets [DOI] [PubMed]
- 146.Van Sickle MD, Oland LD, Mackie K, Davison JS, Sharkey KA. Delta9-tetrahydrocannabinol selectively acts on CB1 receptors in specific regions of dorsal vagal complex to inhibit emesis in ferrets. Am J Physiol Gastrointest Liver Physiol. 2003;285:G566–G576. doi: 10.1152/ajpgi.00113.2003. [DOI] [PubMed] [Google Scholar]
- 147.Watanabe Y, Okamoto M, Ishii T, Takatsuka S, Taniguchi H, Nagasaki M, Saito A. Long-lasting anti-emetic effect of T-2328, a novel NK(1) antagonist. J Pharmacol Sci. 2008;107:151–158. doi: 10.1254/jphs.08027fp. [DOI] [PubMed] [Google Scholar]
- 148.Watson JW, Gonsalves SF, Fossa AA, McLean S, Seeger T, Obach S, Andrews PLR. The anti-emetic effects of CP-99, 994 in the ferret and the dog: role of the NK1 receptor. Br J Pharmacol. 1995;115:84–94. doi: 10.1111/j.1476-5381.1995.tb16324.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Yamakuni H, Nakayama H, Matsui S, Imazumi K, Matsuo M, Mutoh S. Inhibitory effect of zacopride on Cisplatin-induced delayed emesis in ferrets. J Pharmacol Sci. 2006;101:99–102. doi: 10.1254/jphs.scj05007x. [DOI] [PubMed] [Google Scholar]
- 150.Yamakuni H, Sawai-Nakayama H, Imazumi K, Maeda Y, Matsuo M, Manda T, Mutoh S. Resiniferatoxin antagonizes cisplatin-induced emesis in dogs and ferrets. Eur J Pharmacol. 2002;442:273–278. doi: 10.1016/s0014-2999(02)01541-8. [DOI] [PubMed] [Google Scholar]
- 151.Yoshida N, Omoya H, Ito T. DAT-582, a novel serotonin3 receptor antagonist, is a potent and long-lasting antiemetic agent in the ferret and dog. J Pharmacol Exp Ther. 1992;260:1159–1165. [PubMed] [Google Scholar]
- 152.Yoshida N, Omoya H, Kato S, Ito T. 5-HT3 receptor antagonist effects of DAT-582, (R) enantiomer of AS-5370. Eur J Pharmacol. 1992;216:435–440. doi: 10.1016/0014-2999(92)90442-7. [DOI] [PubMed] [Google Scholar]
- 153.Yoshida N, Omoya H, Kato S, Ito T. Pharmacological effects of the new gastroprokinetic agent mosapride citrate and its metabolites in experimental animals. Arzneimittelforschung. 1993;43:1078–1083. [PubMed] [Google Scholar]
- 154.Yoshida N, Omoya H, Une T, Ito T, kato S. Pharmacological profile of the stereoisomers of AS-5370, a novel 5HT3 receptor antagonist. Jpn J Pharmacol. 1991;55(sup 1):385. [Google Scholar]
- 155.Yoshikawa T, Yoshida N, Hosoki K. Involvement of dopamine D3 receptors in the area postrema in R(+)-7-OH-DPAT-induced emesis in the ferret. Eur J Pharmacol. 1996;301:143–149. doi: 10.1016/0014-2999(96)00061-1. [DOI] [PubMed] [Google Scholar]
- 156.Yoshikawa T, Yoshida N, Oka M. Central antiemetic effects of AS-8112, a dopamine D2, D3, and 5-HT(3) receptor antagonist, in ferrets. Eur J Pharmacol. 2001;431:361–364. doi: 10.1016/s0014-2999(01)01459-5. [DOI] [PubMed] [Google Scholar]
- 157.Yoshikawa T, Yoshida N, Oka M. The broad-spectrum anti-emetic activity of AS-8112, a novel dopamine D2, D3 and 5-HT3 receptors antagonist. Br J Pharmacol. 2001;133:253–260. doi: 10.1038/sj.bjp.0704078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Youssefyeh RD, Campbell HF, Airey JE, Klein S, Schnapper M, Powers M, Woodward R, Rodriguez W, Golec S, Studt W, et al. Development of high-affinity 5-HT3 receptor antagonists. 2. Two novel tricyclic benzamides. J Med Chem. 1992;35:903–911. doi: 10.1021/jm00083a015. [DOI] [PubMed] [Google Scholar]
- 159.Youssefyeh RD, Campbell HF, Klein S, Airey JE, Darkes P, Powers M, Schnapper M, Neuenschwander K, Fitzpatrick LR, Pendley CE, et al. Development of high-affinity 5-HT3 receptor antagonists. 1. Initial structure-activity relationship of novel benzamides. J Med Chem. 1992;35:895–903. doi: 10.1021/jm00083a014. [DOI] [PubMed] [Google Scholar]