Abstract
Background Literature on the socio-economic ‘gradient’ in health often asserts that income is associated with better health not only for the very poor, but also across the entire income distribution. In addition, changes in the shape of the association between incomes during a period of increasing economic inequality have not been previously studied. The goal of the current study was to estimate and compare the shape of the relationship between income and mortality in the USA for the 1970s, the 1980s and the 1990s.
Methods Using income and mortality data from the Panel Study of Income Dynamics for respondents aged 35–64 years, we used a Bayesian Cox Model with regression splines to model the risk of mortality over three 10-year follow-up periods. To identify whether income was more strongly associated with mortality at different parts of the income distribution, we treated income as a linear spline with an unknown knot location.
Results The shape of the association between income and mortality was quite non-linear, with a much stronger association at lower levels of income. The relationship between income and mortality in the USA was also not invariant across time, with the increased risk of death associated with lower income applying to an increasing proportion of the US population over time (9th percentile of income in 1970–79, 20th percentile in 1980–89 and 32nd percentile in 1990–99).
Conclusions Our analyses do not support the claim that income is associated with mortality throughout the income distribution, nor is the association between income and mortality the same across periods. Based on our analyses, a focus on the bottom 30% of the income distribution would seem to return the greatest benefits in reducing socio-economic inequalities in health.
Keywords: Income, mortality
Introduction
The association between lower income and increased risk of mortality is well established in many countries, including the USA.1–6 A frequent assertion of the literature on the socio-economic ‘gradient’ in health is that increased income is associated with better health not only for the very poor, but also across the entire income distribution.2,7,8 If true, such a uniform relationship would suggest that population health could be improved by targeting the mechanisms linking income and mortality for all individuals, regardless of their income level. In the USA, however, increasing evidence suggests that the relationship between income and mortality may be non-linear, with additional income more strongly associated with mortality only at the lower end of the income distribution. An accurate understanding of the shape of the relationship between income and mortality is critical to informing policies aimed at reducing health inequalities related to socio-economic position.
Despite the large amount of research on socio-economic gradients in health, studies on the shape of the income–mortality relationship are quite scarce, whereas allusions to the impact of income on health across the income distribution are common. Although several studies have examined the income–mortality relationship in European countries,1 only four studies have explicitly examined the shape of the income–mortality relationship in the USA.9–12 All four studies found evidence of a non-linear relationship between income and mortality, with income more strongly associated with mortality at the lower end of the income distribution. However, three of these studies were limited by a lack of continuous income data and top-coding of income data above $50 000, and none examined the changing nature of the income–mortality relationship over time. With the exception of recent work by Rehkopf et al.,11 these papers did not utilize methods to estimate the location of non-linearities in the income–mortality relationship in the USA. The goal of the current study was to estimate and compare the shape of the relationship between income and mortality in the USA for the 1970s, the 1980s and the 1990s, a period in which there were significant changes in income distribution in the USA, using data from the Panel Study for Income Dynamics (PSID).
Methods
Study population
The data are obtained from the PSID. The PSID began in 1968 as a longitudinal study of a representative sample of US individuals and the family units in which they reside. Starting with a national sample of 18 230 people living in 4800 families in 1968, the PSID has re-interviewed individuals from those families every year (biennially starting in 1997) since that time, whether or not they continue to live in the same dwelling or with the same people. In addition, all people born to or adopted by PSID sample members become sample numbers themselves and are followed in subsequent waves. This design feature replenishes the sample with new birth cohorts. Annual response rates have been 96–98% for the core PSID families in almost every wave, and 50–65% of individuals who were non-responsive at some point came back to the study in a subsequent wave. Bias due to selective attrition has been shown to be quite small in magnitude for many important socio-economic variables, despite cumulative attrition over such a long time period, and the cross-sectional representativeness of the PSID has remained roughly constant over time.13 The central focus of the data is economic and demographic, with substantial detail collected on income sources and amounts, employment, demographic events, family composition changes and residential location. Studies have shown that the PSID income data matches closely with the US income distribution as measured by the Current Population Surveys throughout its four-decade history.14 The PSID, thus, contains among the most comprehensive individual-level income information available in the USA.
In order to examine the income–mortality relationship in the USA over time, we created three cross-sectional samples of PSID respondents for the survey years 1970, 1980 and 1990. The PSID distinguishes between ‘sample members’ who were members of a PSID family at the start of the study and subsequently followed, and ‘non-sample members’ consisting of other family members that were not followed if they broke off from a PSID family unit. Both sample and non-sample members are included in these analyses. The analyses were restricted to working-age adults between ages 35 and 65 years at the time of reported income, as income may be a less useful measure of economic status after retirement. The overall sample consisted of 12 137 respondents and 1057 deaths. There were 4159 working-age respondents in 1970, with 424 observed deaths. In 1980, there were 3820 working-age respondents with 374 observed deaths, and in 1990 there were 4158 working-age respondents with 259 deaths.
Measures
Income
Total family income was calculated as income from all jobs (including tips and overtime pay), farm labour, income from home businesses and professional trades, market gardens, roomers and boarders, rent, dividends, alimony, welfare, social security insurance (SSI), social security, pensions, retirement, unemployment, workers compensation, child support and help from relatives. Each income component was separately self-reported by the head or spouse for the year prior to the interview. Income was adjusted for inflation (US$2000) using the Consumer Price Index data, and reported in thousands of dollars.
Mortality
The PSID collects data on the date and cause of death of study participants and family members. For this analysis, mortality data were available through a restricted-use contract for over 5000 PSID family members. PSID has obtained the decedent status of many who have left the study by contacting family members who remain. For the remaining cases, PSID staff searched the freely available Social Security Death Index (SSDI) for additional mortality information. Although social security numbers were not collected in the course of regular interviews for the PSID, other respondent characteristics available from the survey interview were used to verify decedent status with great accuracy. Seventy-five percent of decedents were confirmed through relatives, whereas the remaining cases were located through SSDI searches. Months and years of death were used in the mortality analysis. In cases where only the year of death was observed, July was imputed as the month of death. Respondents and family members who dropped out of the study and for whom no mortality information was available were treated as censored beginning in July of the year following the last observation. Individuals who remained in the study and survived were treated as censored 10 years following the time at which income was measured.
Additional covariates
Age and sex were included as additional covariates due to their associations with both income and mortality. Age was coded as a continuous variable. Sex was coded as female = 1 and male = 0. As the goal of this analysis was to describe the overall income–mortality association in the USA, we have not included additional covariates such as education level or race/ethnicity that may be relevant in understanding a portion of the income–mortality association.
Statistical analysis
First, we conducted traditional Cox proportional hazard models to test whether linear or log-transformed income fit our data better for each decade. Linear and log-transformed models were comparable for 1970, whereas the log-transformed models provided far superior model fit for 1980 and 1990 (results available upon request). Having confirmed a non-linear relationship in our data, we next moved on to our primary goal of identifying the location of the non-linearity over time. We estimated mortality risk over a 10-year follow-up for the three pooled PSID samples where income was measured in 1970, 1980 and 1990, respectively, using a Bayesian Cox model with regression splines. In order to identify whether income was more strongly associated with mortality at different parts of the income distribution, we estimated the location of the non-linearity in the income–mortality relationship, treating income as a linear spline with an unknown knot location. We specified a model that included a separate slope parameter for the income terms in 1970, 1980 and 1990. The knot for the 1970 income spline was set as a free parameter, and we included dummy variables for 1980 and 1990 to represent possible shifts in the position of the knot over the 1970 baseline. Estimation of this model was formulated using a Bayesian framework and was carried out using Markov Chain Monte Carlo simulation. (Specifically, we ran two chains of a Gibbs sampler for 10 000 iterations after a 5000 iteration burn-in period. We specified diffuse priors centered on zero for each parameter except for k0, which was given a non-informative gamma prior.) Analyses were carried out using the BRugs package in R and utilized PSID sampling weights. Identical models were also run using the widely used Organisation for Economic Co-operation and Development equivalence scale for income, which assigns a value of 1 for the first adult, 0.7 for each additional adult and 0.5 for each child. The pattern and magnitude of changes over time was very similar to our findings (available upon request).
Results
Table 1 shows descriptive statistics for our sample.
Table 1.
PSID sample characteristics, ages 35–64 years
| 1970 | 1980 | 1990 | |
|---|---|---|---|
| Age | 47.65 | 48.74 | 47.06 |
| Male (%) | 56 | 57 | 56 |
| Income percentile (year 2000 dollars) | |||
| 10th | 11 730 | 12 520 | 12 380 |
| 25th | 21 670 | 24 650 | 25 810 |
| 50th | 38 680 | 43 840 | 47 430 |
| 75th | 60 440 | 66 810 | 75 960 |
| Respondents | 4149 | 3820 | 4158 |
| Deaths over follow-up | 424 | 374 | 259 |
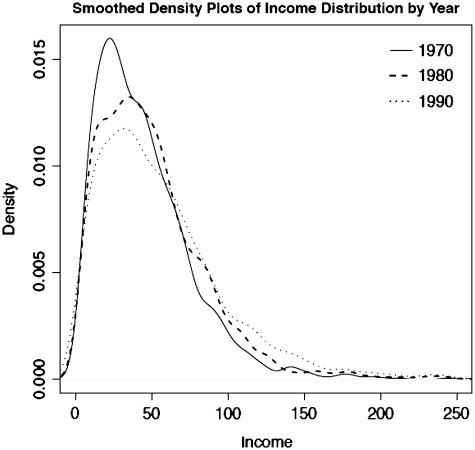
Median income for those 35–64 years of age increased by 22.6% in constant year 2000 dollars across the three samples; in 1970 sample it was $38 680, rising to $43 840 in 1980 and $47 430 in 1990. Each sample is roughly 56% male with an average age of 48 years. Figure 1 illustrates the income distribution for the three samples in constant dollars. While there has been some movement of the entire income distribution to the right over the three periods, there has also been a movement to greater density in the right tail of the distribution, reflecting an increase in income inequality over this time period.15
Figure 1.
Income distribution across decades, year 2000 dollars
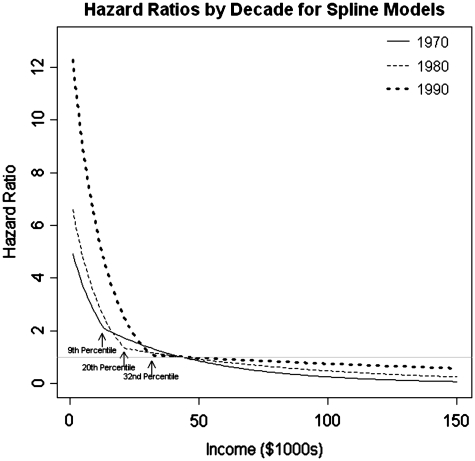
Results from the spline models are shown in Table 2 and illustrated in Figure 2.
Table 2.
HRs for mortality over 10 years associated with income (per $10 000)
| 1970 |
1980 |
1990 |
||||||
|---|---|---|---|---|---|---|---|---|
| Knot (income %) | HR < Knot | HR > Knot | Knot (income %) | HR < Knot | HR > Knot | Knot (income %) | HR < Knot | HR > Knot |
| 9 | 0.496 | 0.785 | 20 | 0.454 | 0.903 | 32 | 0.453 | 0.947 |
| (4–22) | (0.439–0.674) | (0.586–0.956) | (9–30) | (0.381–0.579) | (0.666–1.134) | (24–45) | (0.385–0.532) | (0.811–1.124) |
Model adjusted for age and sex. 95% confidence intervals are given in parentheses. ‘Knot’ refers to the location of the non-linearity in the income–mortality association; the hazard of death associated with income is different above or below the knot. (1 − HR) × 100 is the percentage reduction in the hazard of death associated with a $10 000 increase in income.
Figure 2.
Graphs of income HRs (in reference to median income)
The knot for the 1970s was estimated to fall at $14 180, or the ninth income percentile for the 1970 sample. The hazard ratio (HR) for income below the knot in 1970 indicates that a $10 000-increase in income was associated with a 50.4% lower risk of death over the 10-year follow-up. Above the ninth income percentile, the association of increased income was much reduced, corresponding to a 21.5% reduced risk of mortality for each additional $10 000 of income. In 1980, the knot location was estimated to fall higher in the income distribution, at $22 360 (20th percentile). Below this threshold in 1980, an additional $10 000 of income was associated with roughly the same mortality reduction as the pre-knot estimate for 1970, 54.6%, but importantly, this steeper association applied to a greater percentage of the population. For income above the knot threshold, the income–mortality association was much weaker, corresponding to a 9.7% reduction in mortality risk for each additional $10 000 of income. The 1990 estimate found the location of the knot moving out even further to $33 080 (32nd percentile). Below this threshold, each additional $10 000 of income was still associated with a 54.7% reduction in mortality risk as in previous decades, with an even flatter relationship above the threshold—a 5.3% reduction in risk for each additional thousand dollars of income. Thus, over these three decades, the increased risk of death associated with having less income applied to an increasing proportion of the US population.
The estimated patterns by decade are further illustrated in Figure 2, which shows the predicted HRs during all three decades, with median income at the beginning of each decade as the reference. With each decade, the portion of the income distribution subject to a strong association between income and mortality gets larger, whereas the relationship between income and mortality for those beyond the estimated threshold gets weaker over time. The relative risk for the poorest individuals also increased across decades, such that those in the bottom 5% of the income distribution in 1970 had roughly 2.6 times the risk of mortality compared with individuals at median income, whereas in 1980 had 3.5 times the risk, and in 1990 this risk had increased to >7.6-fold.
Discussion
The notion of the socio-economic ‘gradient’ in mortality is often discussed as if it were linear or near-linear, with much being made out of the fact that the increased risk associated with lower income holds, regardless of where one is on the income distribution. Our analyses do not support this claim. The shape of the association between income and mortality is strongly non-linear, with a much stronger association at low levels of income. Our results also indicate that the relationship between income and mortality in the USA is not invariant across time. While consistently concentrated in the bottom half of the income distribution, the increased risk of death associated with having less income applied to an increasing proportion of the US population over time, and the risk for the poorest in the country relative to those in the middle of the income distribution increased sharply over this time period.
Our results are consistent with previous findings of a non-linear association between income and mortality in the USA.6–8 Our analyses expand upon these findings by estimating the location of non-linearities in this relationship and examining changes in the association across three decades. We also utilize continuous detailed income data from the high-quality PSID, which is not limited by income top-coding as in previous studies.
There are two striking findings of these analyses and both can be used to reflect on the potential mechanisms that link income and risk of death, and policies that can reduce income-associated deaths. First, the results underscore the non-linearity of the association between income and mortality. Additional income makes very little difference in risk of death beyond a certain level of income, but makes a great deal of difference below that level. As a result, deaths are not distributed evenly across the income spectrum and cluster below the knots that we have discovered. In 1970–79, 25.0% of the deaths occurred below the knot at the ninth percentile. In 1980–89, the knot increased to the 20th percentile and 38.8% of deaths fell below the knot, and in 1990–99, 52.5% of deaths fell below the knot at the 32nd percentile in the income distribution.
Secondly, concurrent with this increase in the breadth of the effect of income on mortality and the proportion of deaths that occurred in the range of income most sensitive to income effects, there was also an increase in the relative risk of death for those who were poorest. In 1970, those at the fifth percentile of the income distribution had 2.6 times the risk of death over the next 10 years compared with those with incomes at the median, and in 1990 this increased risk was over seven times that of those at the median income level. Our analysis sample size of 12 167 individuals and 1057 deaths contributed to wide confidence intervals (CIs) in estimating the location of non-linearities in the income–mortality association, but we could still say with statistical confidence that the location of the non-linearity moved significantly outwards between 1970 and 1990.
Our results indicate that the effect of income on risk of death became both broader and deeper during these three decades. During this period there was also an increase in income inequality, with Gini, mean logarithmic deviation and Atkinson measures of inequality of household income also rising during this period.16 Our data are not adequate to explore the reasons why increased income inequality might be associated with widening and deepening of the association between income and mortality. However, the results are consistent with a picture of a middle class that is progressively losing ground economically, the poor and near-poor finding it increasingly hard to meet their needs, and health suffering as a consequence.
These analyses are relevant but are not determinative with regard to arguments about the causal impact of income on health. They establish more firmly the nature of the association between income and mortality and changes in the shape of this association over time. Any convincing argument for a causal or non-causal interpretation of the income–mortality association must be able to match the observed non-linearity and changes in knot locations over time. These results also call for future analyses of the patterns of risks and resources available to households at various locations in the income distribution, and how those have changed over time. Our analyses do not specifically address, for instance, the possibility that poor health adversely impacts earnings, so-called ‘reverse causality’. We chose not to exclude deaths that occurred in the first years of follow-up in order to provide the clearest description of the shape of the income–mortality association, regardless of the direction of causality. Whatever the direction of effect, competing explanations will need to explain the shape of the association and its changes over time. As mentioned above, if reverse causality were to be an important mechanism in the overall association, it would need to have become increasingly salient over time in order to explain the change in the location of non-linearities over time, which seems unlikely. Our results were also robust to using 5-year averages of income instead of 1 baseline year as an income measure.
The current results are also relevant to discussion of how we can reduce socio-economic inequalities in health. Focus on the gradient as if it is near-linear obscures the concentration of considerable risk for certain groups. While there may be arguments for policy approaches to reducing health inequalities that appeal to the broadest spectrum of the population, it is not accurate to base such an argument on increased income-related risk of death. On the other hand, the current results indicate that an increasing proportion of the population is feeling the impact of income-associated risk (32% in 1990–99), whereas at the same time the very poor are falling increasingly behind health-wise. Based on our analyses, a focus on the bottom 30% of the population, with additional emphasis on the poor and working poor, would seem to return the greatest benefits in reducing socio-economic inequalities in health, and there are numerous policy instruments that can be brought to bear to potentially improve their health.17
Funding
This work was supported by an award from the National Institute on Aging at the National Institutes of Health (1R21AG031358-01A1) to G.A.K.
Conflicts of interest: None declared.
KEY MESSAGES.
The association between income and mortality in the USA is much stronger at lower levels of income, with a highly curvilinear association.
The increased risk of deaths associated with lower income has applied to an increasing proportion of the US population over time (1970–2000).
At the same time, the risk of death for those with the lowest incomes has increased.
A focus on the bottom 30% of the income distribution may provide the greatest benefits in reducing socio-economic inequalities in health.
References
- 1.Martikainen P, Makela P, Kosknen S, Valkonen T. Income differences in mortality: a register-based follow-up study of three million men and women. Int J Epidemiol. 2001;30:1397–405. doi: 10.1093/ije/30.6.1397. [DOI] [PubMed] [Google Scholar]
- 2.Kaplan GA, Haan MN, Syme SL, Minkler M, Winkleby M. Socioeconomic status and health. Am J Prev Med. 1987;3:125–29. [Google Scholar]
- 3.Syme SL, Berkman LF. Social class, susceptibility and sickness. Am J Epidemiol. 1976;104:1–8. doi: 10.1093/oxfordjournals.aje.a112268. [DOI] [PubMed] [Google Scholar]
- 4.Marmot M. The influence of income on health: views of an epidemiologist. Health Affairs. 2002;21:31–46. doi: 10.1377/hlthaff.21.2.31. [DOI] [PubMed] [Google Scholar]
- 5.Adler NE, Boyce WT, Chesney MA, Folkman S, Syme SL. Socioeconomic inequalities in health: no easy solution. J Am Med Assoc. 1993;269:3140–45. [PubMed] [Google Scholar]
- 6.Kitagawa E, Hauser P. Differential Mortality in the United States: A Study in Socioeconomic Epidemiology. Cambridge, MA: Harvard University Press; 1973. [Google Scholar]
- 7.Adler NE, Boyce T, Chesney MA, et al. Socioeconomic status and health: the challenge of the gradient. Am Psychologist. 1994;49:15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- 8.Wilkinson R. Unhealthy Societies: The Afflictions of Inequality. New York: Routledge; 1996. [Google Scholar]
- 9.Backlund E, Sorlie PD, Johnson NJ. The shape of the relationship between income and mortality in the United States evidence from the national longitudinal mortality study. Ann Epidemiol. 1996;6:12–20. doi: 10.1016/1047-2797(95)00090-9. [DOI] [PubMed] [Google Scholar]
- 10.Elo IT, Martikainen P, Smith KP. Socioeconomic differentials in mortality in Finland and the United States: the role of education and income. Eur J Population. 2006;22:179–203. [Google Scholar]
- 11.Rehkopf D, Berkman L, Coull B, Krieger N. The non-linear risk of mortality by income level in a healthy population: US National Health and Nutrition Examination Survey mortality follow-up cohort, 1988-2001. BMC Public Health. 2008;8:383. doi: 10.1186/1471-2458-8-383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wolfson M, Kaplan G, Lynch J, et al. Relation between income inequality and mortality: empirical demonstration Diminishing returns to aggregate level studies; Two pathways, but how much do they diverge? BMJ. 1999;319:953–57. doi: 10.1136/bmj.319.7215.953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fitzgerald J, Gottschalk P, Moffitt R. An analysis of sample attrition in panel data: the Michigan Panel study of income dynamics. J Hum Resources. 1998;33:251–99. [Google Scholar]
- 14.Gouskova E, Schoeni R. Panel Study of Income Dynamics Technical Paper Series. Michigan: Ann Arbor; 2007. Comparing Estimates of Family Income in the PSID and the March Current Population Survey, 1968–2005. [Google Scholar]
- 15.Burkhauser R, Feng S, Jenkins SJ, Larrimore J. Estimating trends in US income inequality using the current population survey: the importance of controlling for censoring. NBER Working Paper. 2008 No. 14247. [Google Scholar]
- 16.Jones AF, Weinberg DH. Current Population Reports. Washington, DC: U.S. Census Bureau; 2000. The Changing Shape of the Nation's Income Distribution: 1947-1998; pp. 60–204. [Google Scholar]
- 17.Kaplan G. The Poor Pay More: Poverty's High Cost to Health. Princeton, New Jersey: Robert Wood Johnson Foundation; 2009. [Google Scholar]