Abstract
Objective:
We describe herein a surgical technique, whereby we use a liposuction device for the laparoscopic treatment of hepatic hydatid cysts (HHC).
Methods:
Ten patients with 12 hepatic hydatid cysts were treated with this technique. All patients received pre- and postoperative antiscolecidal medications. The laparoscopic technique consisted of partial aspiration of the cyst fluid and replacement of the aspirated fluid with 10% Betadine. The Betadine solution was left in situ for 10 minutes. Evacuation of the cyst contents was carried out with the liposuction device. The residual cavity was unroofed by partial excision of the ectocyst. A drain was left alongside the cyst. No intra- or postoperative complications were encountered.
Results:
all patients were mobilized freely, were allowed to eat a regular meal 6 hours after recovery from anesthesia, and were discharged on the third postoperative day. All patients resumed their normal household and work activities by the tenth postoperative day. The patients were regularly followed up every 2 months for 2 years. At follow-up in the surgical clinic, no evidence of recurrence was noted either clinically, serologically, or by imaging techniques.
Conclusion:
We conclude that the laparoscopic treatment of HHC is feasible and advantageous. We believe that the use of a liposuction device facilitates rapid and efficient evacuation of the viscid organic contents of the cyst and helps in the obliteration of the residual cavity.
Keywords: Hepatic hydatid cyst, Laparoscopic treatment, Liposuction device
INTRODUCTION
Two thousand years ago, Hippocrates described hydatid disease of the liver as “the liver full of water.” Tyson in 1687 suggested the parasitic nature of the disease.1 The details of its clinical aspect, however, only became clear at the beginning of this century.
Hydatid disease is common in the sheep-rearing areas of the world, mainly Australia, Turkey, Wales, and South America. The prevalence of hydatid disease among humans was determined as 9.1% in a World Health Organization study in the Central Peruvian Andes.2 The disease is not uncommon in Saudi Arabia, especially in the South Western region of the Peninsula.3 In humans, most hydatid cysts occur in the liver and 75% of these are single cysts.4 Other commonly involved organs are the lungs, spleen, and kidneys.
Although percutaneous drainage with or without instillation of scolecidal agents has been increasingly used for the management of hepatic hydatid cysts in recent years, surgical intervention is still the treatment of choice.5–8 The aim of surgical treatment is elimination of scolices, previously killed by scolecidal drugs, together with removal of all viable parts of the cyst and obliteration of the residual cavity. This can be achieved by hepatic resection9, 10 or by drainage and obliteration of the cyst. The latter procedure can be done by open surgery or laparoscopy.8,11–13
PATIENTS AND METHODS
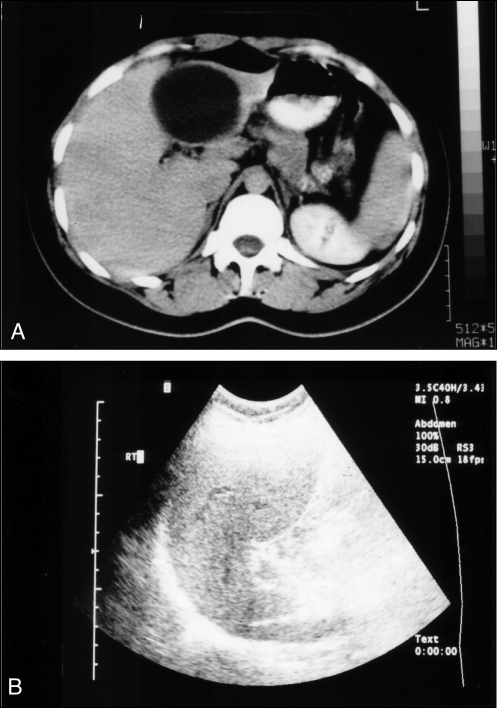
The present study included 10 patients with 12 hepatic hydatid cysts (HHC), who were admitted to the North West Armed Forces Hospital (NWAFH), Tabuk, Saudi Arabia, between June 1993 and December 1999. Ten patients (7 females and 3 males) had an average age of 43 years (16 to 63). On admission, the diagnosis of HHC was established by taking a relevant history and a thorough physical examination. The 3 males were soldiers from areas endemic for hydatid disease. All 10 patients had a positive history of contact with animals including sheep, camels, and dogs. Yet, none of them was a full-time shepherd. The diagnosis was confirmed by other relevant supportive blood investigations and imaging procedures. Each patient had routine blood tests, which included a complete blood count (CBC), liver function tests, kidney function tests, and an indirect hemagglutination test. Abdominal ultrasound scans showed a solitary anechoic lesion in 8 patients and bilateral anechoic lesions in 2 patients. A spiral CT scan was used whenever necessary to confirm ultrasonographic findings and to define the exact anatomical site and number of intrahepatic cysts. Figure 1 shows a preoperative ultrasound and computed tomographic (CT) scans of the liver demonstrating HHC. All patients received preoperative and postoperative antiscolecidal medications in the form of Albendazole or Mebendazole according to drug availability. All patients were followed up clinically, biochemically, and radiologically for 2 years.
Figure 1.
A. CT scan demonstrating the hepatic hydatid cyst preoperatively. B. Ultrasound demonstrating the hepatic hydatid cyst preoperatively.
After the diagnosis of HHC was confirmed, all patients underwent laparoscopic excision of the HHC under general anesthesia, 1 surgical technique being used for all patients.
Technique
With the patient in a supine position under general anesthesia with endotracheal intubation and muscle relaxation, pneumoperitoneum was created with a Veress needle to a pressure of 14 to 15 mm Hg. The primary 10-mm port was inserted through an incision in the umbilicus and a laparoscope was introduced. Diagnostic laparoscopy was performed and the site and size of the cyst(s) was decided. The remainder of the surgical ports was inserted under direct vision according to the site and number of cysts seen. A second 10-mm port was inserted to the right or to the left of the subcostal region according to where the cyst lay. A 5-mm port was inserted 5 cm below the xiphoid process for retraction purposes. Once the cyst was localized, a 12 French Silverman's needle was introduced percutaneously into the cyst and connected to a liposuction machine. Negative pressure from an ordinary suction machine was maintained beside the puncture hole to remove any fluid leakage or spillage. A 10% Betadine solution equal to the aspirated fluid was injected through the Silverman's needle and left in situ for 10 to 15 minutes. A second 10-mm surgical trocar was introduced directly inside the cyst through the Silverman's needle puncture site. The previously inserted suction cannula remained at the same site to take care of any leakage from the punctured site. The trocar was then removed keeping the port sheath inside the cyst's cavity. A size 24 French transparent chest tube was introduced inside the cyst through the port sheath. The chest tube was then connected to the liposuction device, which has a maximum vacuum power of 28 in of Hg and a maximum flow rate of 5.5 cubic feet per minute. Intermittent pressure was used until all content of the cyst including the laminated membrane and hydatid sand were completely evacuated.
The residual cavity was repeatedly irrigated with 10% povidone iodine (Betadine) until the solution was clear. The chest tube was removed and the ectocyst was partially excised with diathermy or an UltraCision device. The laparoscope was then introduced inside the cavity for further inspection and additional cleaning as needed.
Once the cavity and its surroundings were clean and dry, a tube was placed alongside the cyst cavity. The pneumoperitoneum was deflated and the port sites were meticulously closed.
RESULTS
Ten patients with 12 HHCs were treated by laparoscopic excision with the liposuction device. The presenting symptomatology of patients is shown in Table 1. Ultrasound and CT scans confirmed the diagnosis of HHC in all patients. Ten cysts (83.3%) were located in the right hepatic lobe, and 2 (16.6%) were found in the left hepatic lobe. Two patients (20%) had bilateral cysts. Cysts ranged in size from 5 to 20 cm (mean 10 cm). Laparoscopic findings were consistent with the ultrasound and CT scan diagnosis in all 10 patients (100%).
Table 1.
Symptomatology of Patients With HHC
| Symptom | No.of Patients | Percentage |
|---|---|---|
| Dull aching pain in right upper quadrant | 9 | 90% |
| Mass upper abdomen and dragging sensation | 6 | 60% |
| Dyspepsia | 1 | 10% |
| Jaundice | 1 | 10% |
Twelve cysts were treated laparoscopically with the liposuction device. None of the cases were converted to open laparotomy. No intra- or postoperative complications were encountered. The average operative time measured from the time of induction of anesthesia to the application of the skin dressing was 55 minutes. All patients were mobilized and allowed to eat a light meal as early as 6 hours after recovery from the anesthesia. They were all discharged on the third postoperative day. The 3 male soldiers resumed their army-related activities 10 days after discharge. However, the 7 housewives actually resumed their normal household activities as early as 7 days after discharge. Outpatient follow-up carried out every 2 months for 2 years showed no evidence of clinical or radiological recurrence. Complete obliteration and resolution of the HHC was demonstrated radiologically in all patients by the end of the 2-year follow-up period.
DISCUSSION
Laparoscopic surgery has already been established worldwide. It is known to offer many of the advantages of minimal access, including a smaller incision, low morbidity, short hospital stay, and early return to work.14, 15 Although hepatic hydatid cysts have been cured by puncture and instillation of scolecidal medication, surgery is still the mainstay of treatment. The surgical approach may involve liver resection or more conservative (open or laparoscopic) approaches.8, 11, 13 The disadvantages of a laparoscopic approach are the increased danger of contamination of the abdominal cavity with scolices and the difficulties in aspirating viscid organic cyst content. Furthermore, cysts located deep in the hepatic parenchyma carry the danger of hemorrhage if approached laparoscopically.8
In this report, a laparoscopic technique using a liposuction device for the treatment of hepatic hydatid disease is described and the results of the first 12 cysts are presented. The liposuction unit has been used to retrieve the spleen after laparoscopic splenectomy;16 however, we believe this is the first time that it has been used for the treatment of HHC. Classical surgical aspirators are usually blocked by daughter cysts and laminated membranes. To avoid this problem, Saglam17 invented a novel perforator-grinder-aspiration apparatus, specifically designed for grinding and evacuation of hydatid cysts together with vacuum obliteration of the cavity at minus 250 mbar. Other authors18 have reported the use of a large transparent cannula under vacuum to seal the cannula, and adhering it to the liver by cyanoacrylate or fibrin glue to prevent spillage.
What has been described in the literature as disadvantages of laparoscopic excision of hepatic hydatid cyst8 we believe have been overcome in this study. The liposuction unit with its high power negative pressure, the introduction of a transparent 24 French chest tube inside the cyst, and the use of a conventional sucker alongside the site of entry of the chest tube are measures that guard against any significant spillage of cyst content. The high negative pressure exerted by the liposuction device acts as a positive factor in obliterating the residual cavity.17 Although many systemic and local antiscolecidal agents have been tried with varying results,19–22 we believe use of the antiscolecidal medications mebendazole or albendazole (pre- and postoperative), plus intraoperative 10% povidone iodine intracystic irrigation have combined to prevent recurrence by killing all viable scolices.
CONCLUSION
We conclude that the laparoscopic treatment of hepatic hydatid cysts is feasible and safe. It combines the open surgical techniques of endocyst excision and partial pericystectomy with the advantages of minimally invasive surgery. Our patients benefited from immediate postoperative mobilization, early feeding, early discharge from the hospital and early return to work. Although 2 years is not long enough to say that no recurrences have taken place, we believe that the use of preoperative, intraoperative, and postoperative antiscolecidal agents helps prevent future recurrences.
References:
- 1. Kattan YB. Management of hydatid disease. Ann R Coll Surg Engl. 1997;59:108. [PMC free article] [PubMed] [Google Scholar]
- 2. Moro PL, McDonald J, Gilman RH, et al. Epidemiology of Echinococcus granulosus infection in the Central Peruvian Andes. Bull World Health Organ. 1997;75(6):553–561 [PMC free article] [PubMed] [Google Scholar]
- 3. Malaikas SS, Attayeb A, Sulaimani S, Reddi JJ. Human Echinococcus in Saudi Arabia. Saudi Med J. 1981;2(2):77–84 [Google Scholar]
- 4. Perek A, Numan F, Perek S, Durgun V, Kapan M, Aykuter G. Management of a patient with hepatic-thoracic-pelvic and omen-tal hydatid cysts and post-operative bilio-cutaneous fistula - A case report. Hepatogastroenterology. 1999;46(28): 2202–2207 [PubMed] [Google Scholar]
- 5. Khuroo MS, Zargar SA, Mahajan R. Echinococcus granulosus cysts in the liver: Management with percutaneous drainage. Radiology. 1991;81:141–145 [DOI] [PubMed] [Google Scholar]
- 6. Acuna B, Rozanus I, Celick L, et al. Purely cystic hydatid disease of the liver, treatment with percutaneous aspiration and injection of hypertonic saline. Radiology. 1992;182:541–543 [DOI] [PubMed] [Google Scholar]
- 7. Crippa FG, Bruno R, Brunetti E, Filice C. Echinococcal liver cysts: treatment with echo-guided percutaneous puncture PAIR for echinococcal liver cysts. Ital J Gastroenterol Hepatol. 1999;31(9):884–892 [PubMed] [Google Scholar]
- 8. Sayek I, Cakmakci M. Laparoscopic management of echinococcal cysts of the liver. Zentralbl Chir. 1999;124(12):1143–1146 [PubMed] [Google Scholar]
- 9. Saidi F. Hydatid cyst of the liver. In: Saidi F. ed. Surgery of Hydatid Disease. Suffolk, Va: W.B. Saunders; 1976:60–155 [Google Scholar]
- 10. Belli L, Aseni P, Rondinara GF, Berlini M. Improved results of pericystectomy in normothermic ischemia for hepatic hydatidosis. Surg Gynecol Obstet. 1986;163:127–132 [PubMed] [Google Scholar]
- 11. Strauss M, Schmidt J, Boedeker H, Zirngibl H, Jauch KW. Laparoscopic partial pericystectomy of echinococcus granulosus cysts in the liver. Hepatogastroenterology. 1999;46(28):2540–2544 [PubMed] [Google Scholar]
- 12. Berberoglu M, Taner S, Dilek ON, Demir A, Sari S. Gasless vs gaseous laparoscopy in the treatment of hepatic hydatid disease. Surg Endosc. 1999;13(12):1195–1198 [DOI] [PubMed] [Google Scholar]
- 13. Ertem M, Uras C, Karahasanoglu T, Erguncy S, Alemdaroglu K. Laparoscopic approach to hepatic disease. Dig Surg. 1998;15(4):333–336 [DOI] [PubMed] [Google Scholar]
- 14. Al-Shareef Z, Koneru SR, Al Tayeb A, Shahata Z, Aly T, Basyouni A. Laparoscopic ligation of varicocele: an anatomically superior operation. Ann R Coll Surg Engl. 1993;75(5):354–358 [PMC free article] [PubMed] [Google Scholar]
- 15. Al-Shareef Z, Ahmad I, Al-Shlash S, Al-Dhohayan A, Aly HEM. Laparoscopic herniorrhaphy: modified technique. J Irish Coll Physicians Surg. 1996;25(3):182–184 [Google Scholar]
- 16. Lai PBS, Leung KL, Ho WS, et al. The use of liposucker for spleen retrieval after laparoscopic splenectomy. Surg Laprosc Endosc Percutan Techn. 1999;(10):39–40 [PubMed] [Google Scholar]
- 17. Saglam A. Laparoscopic treatment of liver hydatid cysts. Surg Laparosc Endosc Percutan Techn. 1996;6(1):16–21 [PubMed] [Google Scholar]
- 18. Pickel A, Daud G, Urbach D, Lefler E, Barasch EF, Eitan A. Laparoscopic approach to hydatid liver cyst, is it logical? physical, experimental and practical aspects. Surg Endosc. 1998;12(8):1073–1077 [DOI] [PubMed] [Google Scholar]
- 19. Moller S, Kairies M, Krause BT. Echinococcosis - case report and review of literature. Zentralbl Gynakol. 1998;120(2):79–82 [PubMed] [Google Scholar]
- 20. Besim H, Karayalcin K, Hamamci O, Gungor C, Korkmaz A. Scolecoidal agents in hydatid cysts. Surgery. 1998;10(6):347–351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Deger E, Hokelek M, Deger BA, Tutar E, Asil M, Pakdemirli E. A new therapeutic approach for the treatment of cystic echinococcosis: percutaneous albendazole sulfoxide injection without re-aspiration. Am J Gastroenterol. 2000;95(1):248–254 [DOI] [PubMed] [Google Scholar]
- 22. Karayalcin K, Besim H, Sonisik M, Eruerdin N, Korkmaz A, Aras N. Effect of hypertonic saline and alcohol on viability of daughter cysts in hepatic hydatid disease. Eur J Surg. 1999;165(11):1043–1044 [DOI] [PubMed] [Google Scholar]