Abstract
Inhibition of phosphodiesterase 4 (PDE4) to increase endothelial cAMP and stabilize the endothelial barrier attenuates acute inflammatory increases in vascular permeability. We extended this approach to attenuate physiological increases in vascular permeability in response to atrial natriuretic peptide (ANP), which acts with the kidney to regulate plasma volume. We measured blood-to-tissue albumin clearance and changes in plasma volume in isoflurane-anaesthetized mice (C57BL/6J) pre-treated with rolipram (8 mg kg−1i.p., 30 min). Rolipram significantly reduced albumin permeability, measured using a dual-label fluorescence method, in skin and skeletal muscle compared with ANP alone (500 ng kg−1 min−1). Skin and muscle tissue accounted for 70% of the reduction in whole body albumin clearance taking into account albumin clearance in gastrointestinal (GI) tissue, heart and kidney. The action of ANP and rolipram to modify albumin clearances in duodenum and jejunum could be accounted for by local increases in vascular perfusion to increase surface area for exchange. ANP increased haematocrit from 40.6% to 46.8%, corresponding to an average loss of 22% plasma fluid volume (227 μl), and this was almost completely reversed with rolipram. Renal water excretion accounted for less than 30% of plasma fluid loss indicating that reduced albumin permeability and reduced filtration into vasodilated GI tissue were the predominant actions of PDE4 inhibition. Similar fluid retention was measured in mice with endothelial-restricted deletion of the guanylyl cyclase-A receptor for ANP. Stabilizing the endothelial barrier to offset ANP-induced increases in vascular permeability may be part of a strategy to maintain plasma volume.
Non-technical summary
Natriuretic peptides (such as atrial natriuretic peptide, ANP) are normally present at very low levels in the blood and are part of physiological systems that control blood volume. During diseases such as heart failure and sepsis, circulating levels of ANP increase, leading to an increase in blood vessel permeability and loss of blood fluid volume to the tissues. Other studies show that some inflammatory responses are strongly blocked by increased intracellular cAMP. Here we tested whether rolipram, an inhibitor of the degradation of cAMP, could counteract the movement of protein and fluid out of the blood that is induced by ANP. We found that rolipram almost completely blocked the ANP-induced loss of blood volume. Stabilizing the endothelial barrier by controlling cAMP levels to offset ANP-induced increases in vascular permeability may be part of a strategy to maintain plasma volume in disease states with elevated natriuretic peptides.
Introduction
At physiological concentrations, atrial natriuretic peptide (ANP) is recognized to have multiple actions including those on kidney to increase water excretion, on vascular smooth muscle to cause vasodilatation, and on endothelium to increase vascular permeability. The actions of ANP on kidney, vascular smooth muscle and vascular endothelium are part of the physiological mechanisms to regulate plasma volume and arterial pressure. Of these actions, the least well studied and understood is the role of ANP in the endothelium-dependent control of vascular permeability to albumin. The ANP control over albumin permeability distinguishes it from other diuretics that result in fluid loss from both plasma and interstitial spaces. One key mechanism whereby ANP effects preferential loss of fluid from the plasma volume appears to be that ANP-dependent increase in vascular permeability to plasma proteins, occurring at the same time that water is excreted by the kidney, reduces the tendency for albumin to concentrate in the plasma due to renal water loss from the plasma. Since albumin is by far the largest contributor to the plasma colloid osmotic pressure, the expected shift of water from the interstitial space into plasma, predicted from the Starling balance of capillary exchange when plasma proteins are concentrated, does not occur in the presence of the increased permeability. There have been relatively few attempts to modulate ANP-dependent changes in microvascular permeability in multiple organs of the body and evaluate the effects of such changes on plasma volume.
In a recent study we used genetically modified mice having endothelium-restricted deletion of the ANP guanylyl cyclase A receptor GC-A (EC GC-A KO mice) as well as control littermates to study the tissue-specific role of ANP in endothelial control of albumin permeability (Curry et al. 2010). These experiments demonstrated that a failure of endothelium to respond to ANP at the plasma concentrations measured during plasma volume expansion could explain, at least in part, the loss of the plasma volume regulatory mechanisms in these mice and the development of mice with a hypertensive phenotype with expanded vascular volumes. The aim of the present experiments was to extend the investigation of atrial natriuretic peptide-induced increases in blood-to-tissue clearance of albumin to further evaluate the contribution of ANP-dependent changes in vascular permeability to plasma volume regulation in normovolumic wild-type mice. We argued that if increased vascular permeability to albumin was a major determinant of fluid loss from the plasma space, then stabilizing the endothelial barrier and attenuating ANP-induced increases in vascular permeability should attenuate ANP-induced loss of plasma fluid.
To stabilize vascular permeability we used an inhibitor (rolipram) of the most highly expressed cAMP hydrolyzing phosphodiesterase in normal endothelium (PDE4) to increase endothelial cell cAMP (Netherton & Maurice, 2005; Lugnier, 2006). The approach extended detailed investigations from many laboratories, including our own, showing that increased intracellular cAMP, acting via both PKA-dependent and PKA-independent pathways, significantly attenuates increased vascular permeability induced by a wide range of inflammatory mediators including platelet activating factor, bradykinin (BK) and bacterial toxins in intact microvessels, as well as thrombin, histamine and others in cultured endothelium (Stelzner et al. 1989; Moy et al. 1998; van Nieuw Amerongen & van Hinsbergh, 2002; Qiao et al. 2003; Waschke et al. 2004; Bos, 2005; Cullere et al. 2005; Fukuhara et al. 2005; Kooistra et al. 2005). We also note that an advantage of using rolipram to increase intracellular cAMP in tissue cells is that any action of rolipram on microvascular haemodynamics (as opposed to permeability) is expected to increase rather than decrease blood-to-tissue exchange because rolipram-induced increased cAMP levels in vascular smooth muscle is expected to be similar to a β-2 adrenergic vasodilatation which would favour increased clearance due to increased exchange area. Thus, decreased clearance in the presence of rolipram is an indicator of decreased vascular permeability; the extent of permeability decrease may actually be underestimated if exchange area also increases.
ANP is present in the normal circulation at low levels (0.1–0.3 ng ml−1, i.e. < 0.1 nm). When vascular volume is expanded, ANP is released from specialized cells in the heart at concentrations that approach 1 ng ml−1 (approx 0.3 nm (Pedram et al. 2002; Schreier et al. 2008)). Infusion of ANP at rates to achieve close to this level in the plasma produce an increase in albumin clearance in a range of organs, particularly skin, muscle and the GI tract of both rats and mice (Tucker et al. 1992; Renkin & Tucker, 1998; Sabrane et al. 2005). We designed our experiments to directly compare ANP-induced increase in vascular permeability in C57BL/6J mice (with and without rolipram pre-treatment) with our recently published results which measured the action of ANP to increase albumin clearance in EC GC-A KO mice and their control littermates. Thus, if rolipram significantly attenuated ANP-induced increases in vascular permeability in wild-type mice we expected no acute effect of ANP on vascular permeability and plasma volume, similar to results in the EC GC-A KO mice. If this is the case, our results would support the idea that pharmacological modulation of the vascular actions of ANP using phosphodiesterase inhibitors to modify endothelial cAMP levels might be a tool for manipulation of plasma volume.
Methods
Ethical approval
The investigation conforms to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85-23, revised 1996). Animal protocol 13052 was approved by the Institutional Animal Care and Use Committee of the University of California, Davis.
Animal preparation and tissue collection
Male mice (C57BL/6J, 25–35 g, The Jackson Laboratory) were anaesthetized with isoflurane (1.5–2.0%) and both the jugular vein and carotid artery were cannulated with heparinized cannulae (very low dead volume, 10 μl). The jugular vein cannula was connected to an infusion pump for delivery of fluorescently labelled albumin (bovine serum albumin (BSA) dye) tracers and infusion of either test solution (ANP, 500 ng (kg body wt)−1 min−1 in phosphate-buffered saline, PBS) or control solution (PBS). The carotid cannula was clamped and left untouched until blood collection at the end of the experiment. All animals were stabilized with a 30 min baseline infusion of PBS at 1 μl min−1 (starting at t = −30 min). At t = 0 min, 40 μl of Alexa Fluor 647-labelled bovine serum albumin (BSA-647) at concentrations of 60–100 mg ml−1 was injected via the jugular cannula and the cannula was quickly flushed with 10 μl of PBS followed by continued infusion of control or test solution at 1 μl min−1. At t = 30 min, 40 μl of Alexa Fluor 555-labelled albumin (BSA-555) at the same concentration as the BSA-647 was injected. The cannula was flushed with 10 μl of PBS, and the 1 μl min−1 infusion was continued during the following 5 min to allow the BSA-555 (as a marker of local intravascular volume) to mix completely in the blood. At t = 35 min, blood samples were quickly drawn from the carotid cannula and the animal was killed with saturated KCl injected into the jugular cannula. Total volume of fluid injection was carefully controlled to enable distinction between haematocrit changes due to fluid infusion and due to fluid redistribution. This two-tracer fluorescence method for determining macromolecule permeability, here adapted for mice, is based on earlier studies, using isotope-labelled albumins, which were extensively characterized and tested in rat (Tucker et al. 1992). The development of two-tracer methods and comparison with lymph collection techniques has been reviewed (Renkin & Tucker, 1998).
For rolipram (8 mg (kg body wt)−1) treatment, the rolipram (stock 50 mm in EtOH) in 100 μl total volume (prepared in PBS) was injected i.p. after the cannulations were completed and just prior to the first 30 min stabilization period (t = −30 min). In this way, the rolipram was allowed to absorb for 30 min before tracer albumin was injected and either control or test infusions were started. The rolipram dose used here has been shown to block a range of inflammatory responses (Teixeira et al. 1994; Elwood et al. 1995; Alvarez et al. 2001). For non-rolipram control experiments, 100 μl of PBS with vehicle was injected before the stabilization period.
Analysis of blood and tissue samples for fluorescence
Plasma samples were separated from blood after centrifugation and measurement of haematocrit. The exact amount of plasma was determined by weighing. Tissues were dissected, placed into pre-weighed vials, minced with scissors, and then reweighed. The labelled albumin was extracted from the tissue samples by adding 1 ml of 1 mg ml−1 unlabelled albumin in PBS to each vial, vortexing and storing them overnight at 4°C. After this, the extract was separated from the tissue by centrifugation and the fluorescence from each tracer (BSA-647 and BSA-555) in both plasma samples and tissue extracts was determined by fluorometry. The tissues were then oven dried to constant weight.
To remove particulate matter which could interfere with the fluorescence measurements, the tissue extracts were filtered through a 5 μm syringe filter, and then through a 1.2 μm syringe filter, before fluorometric analysis. Standard curves were also prepared in the same way with solutions having comparable tissue extracts; both BSA-dyes were added at equal concentrations to non-fluorescent tissue extract and the extracts were filtered before fluorescence intensity measurement. Control experiments, using a known amount of labelled albumin added to non-fluorescent tissue and extracted using the same process, showed that BSA-dye recovery by extraction was better than 95%.
Tracer preparation
Bovine serum albumin (Sigma A0281) was labelled with either Alexa Fluor 647 (emission max at 671 nm) or Alexa Fluor 555 (emission max at 570 nm) according to the instructions from the manufacturer (Invitrogen/Molecular Probes) to produce BSA-647 and BSA-555, respectively. Briefly, 40 mg of albumin was labelled using 5 mg of dye in 11 ml of bicarbonate-buffered PBS for 2.5 h. The reaction was terminated with hydroxylamine and the albumin purified by running through a size-exclusion column (Bio-Gel P-30, Bio-Rad). This process yielded a labelling efficiency of 3–5 moles of dye per mole of albumin.
Elimination of free dye
As non-covalently bound dye (free dye) dissociating from the albumin would compromise measurements of tissue albumin uptake, great care was taken to ensure that the amount of free dye in the injectate was less than 0.3%. After labelling and column purification, the BSA-dye was stored for 3 weeks at 4°C in 2 mm sodium azide PBS to allow free dye to dissociate from the albumin. To increase the rate of dye dissociation, the free dye was removed each week by concentrating the labelled albumin using 30 kDa molecular weight cut-off centrifuge filters (Amicon Ultracel-4, 30K, Millipore) and re-diluting to the original volume with fresh PBS–azide. After 3 weeks the solution was concentrated again and then purified by cold ethanol precipitation. The precipitated albumin was re-dissolved in PBS alone to a concentration of about 60–100 mg ml−1, the concentration used in the experiments. Free dye was checked by centrifuging a 2 mg ml−1 solution of BSA-dye through a 30 kDa molecular weight cut-off centrifuge filter (Centrifree YM30, Millipore) and checking the fluorescence of the ultrafiltrate in a fluorometer, comparing it to standards prepared from free dyes alone. Free dye concentration was always reduced to less than 0.3% before the labelled albumin was used for an experiment.
ANP infusion
ANP (1-28, rat/mouse, synthetic, from Bachem) was dissolved in PBS and infused via the jugular vein at a dose of 500 ng (kg BW)−1 min−1 using an infusion pump (SP120P, World Precision Instruments). This dose was previously used in mice (Sabrane et al. 2005) and was close to the dose used in comparable experiments in rats (400 ng (kg BW)−1 min−1) (Tucker et al. 1992).
Calculation of clearances
A 30 min albumin clearance was estimated as an extravascular plasma equivalent volume. This was calculated as the difference between the plasma equivalent distribution volume of BSA-647 at t = 35 min and the plasma equivalent volume of BSA-555 over the final 5 min (t = 30 to t = 35 min). The plasma equivalent distribution volume (μl (g dry weight)−1) for each tracer was calculated from the fluorescence intensity measurements as [total BSA-dye content (μg (g dry weight)−1)]/[plasma BSA-dye concentration (μg μl−1)]. Assuming most of the BSA-555 was still in the plasma after 5 min, the BSA-555 equivalent volumes give a measure of local vascular volumes in each tissue. All calculations were referenced to tissue blood-free dry weight as previously published (Nedrebo et al. 2003; Curry et al. 2010).
Statistical analysis
SigmaStat Version 3.1 (Systat Software Inc.) was used for statistical analysis. The four experimental groups were compared using a one-way ANOVA and post hoc Bonferroni and Holm–Sidak tests to correct for multiple testing, unless otherwise specified. A difference was considered statistically significant when P < 0.05.
Results
The most important new observations were that the 30 min clearance of albumin caused by ANP was significantly attenuated in skin and muscle (P < 0.05; ANOVA) when the animals were pre-treated with rolipram. There was no tendency for rolipram to change local vascular volume suggesting the primary effect of rolipram in skin and muscle was on vascular permeability. By contrast in kidney, heart and GI tissues, the actions of ANP and rolipram were associated with significant increases in local vascular volumes, and these changes had to be taken into account to evaluate the mechanisms of action of ANP to increase clearance and rolipram pre-treatment to attenuate clearance of albumin when increased with ANP. We therefore describe results from skin and muscle separate from GI and other tissue. Also, mean arterial pressure was stable at 90 ± 5 mmHg in control experiments (30 min of pre-treatment with vehicle alone and tracer injection without ANP). There was a tendency for mean arterial pressure to fall by 10 mmHg by the end of the ANP infusion, and this was not significantly modified by rolipram.
The 30 min albumin clearances for vehicle control, ANP, vehicle plus rolipram, and ANP plus rolipram are in Table 1. Together, skin and muscle account for 60–65% of total body weight and similar percentages of the total extracellular fluid volume. A 30 g mouse has approximately 12 g muscle (40% body weight) and 6 g skin (20% body weight). Control values of 30 min albumin clearance measured using fluorescently labelled albumins were similar to values measured in C57BL/6J mice in previous experiments using isotope-labelled albumin (Curry et al. 2010; see Discussion). ANOVA analysis of the changes in these clearances demonstrated the most significant differences were between measured clearances for ANP vs. ANP plus rolipram, followed by ANP vs. rolipram, and ANP vs. vehicle control (Fig. 1A). Further details are given below.
Table 1.
Local vascular volumes (μl (g dry wt)−1); 30 min albumin clearances (μl (g dry wt)−1); normalized albumin clearances and water content (ml (g dry wt)−1) in skin and muscle
| Vehicle | ANP | Rolipram | Rolipram + ANP | |
|---|---|---|---|---|
| Vascular volume | ||||
| Back skin | 9.0 ± 0.8 | 8.9 ± 0.8 | 9.4 ± 1.4 | 10.5 ± 1.1 |
| Hamstring muscle | 22.9 ± 1.1 | 20.1 ± 0.8 | 23.0 ± 0.9 | 24.0 ± 1.5 |
| Quadriceps muscle | 16.1 ± 0.9 | 14.0 ± 0.8 | 19.9 ± 0.92 | 17.3 ± 1.4 |
| Clearance | ||||
| Back skin | 15.8 ± 1.8 | 36.1 ± 5.81 | 9.5 ± 1.32 | 13.3 ± 1.42 |
| Hamstring muscle | 11.3 ± 1.0 | 14.1 ± 1.1 | 8.5 ± 0.82 | 8.6 ± 0.62 |
| Quadriceps muscle | 9.2 ± 0.6 | 11.9 ± 1.01 | 6.4 ± 1.62 | 6.9 ± 0.52 |
| Normalized clearance | ||||
| Back skin | 1.91 ± 0.24 | 4.02 ± 0.531 | 1.06 ± 0.102 | 1.39 ± 0.152 |
| Hamstring muscle | 0.52 ± 0.05 | 0.72 ± 0.061 | 0.38 ± 0.042 | 0.37 ± 0.032 |
| Quadriceps muscle | 0.64 ± 0.06 | 0.91 ± 0.091 | 0.34 ± 0.032 | 0.46 ± 0.052 |
| Water content | ||||
| Back skin | 1.79 ± 0.12 | 1.86 ± 0.13 | 1.83 ± 0.14 | 1.88 ± 0.12 |
| Hamstring muscle | 4.01 ± 0.08 | 3.93 ± 0.05 | 3.92 ± 0.11 | 3.88 ± 0.07 |
| Quadriceps muscle | 4.07 ± 0.04 | 4.16 ± 0.05 | 4.14 ± 0.16 | 4.14 ± 0.13 |
P < 0.05:
when compared to Control;
when compared to ANP; Means ± SEM.
Figure 1. Thirty minute albumin clearances in skin and muscle.
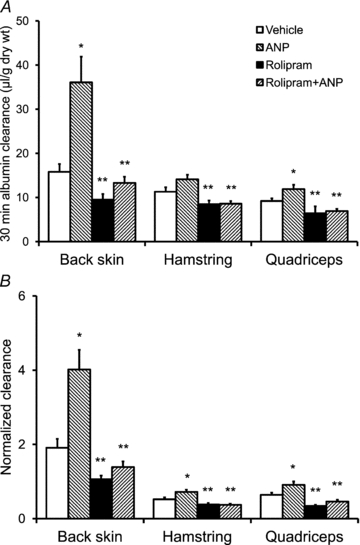
A, the 30 min albumin clearances are shown for skin (back) and two muscles (hamstring and quadriceps) under 4 conditions: vehicle control, ANP, rolipram, and ANP plus rolipram. Rolipram reduced the ANP-induced increase in 30 min clearance to values close to vehicle control. B, the 30 min albumin clearances are normalized to local plasma volumes for the same data as in A. The results demonstrate significant increases in vascular permeability with ANP and significant reductions in vascular permeability with rolipram pre-treatment. *Significant increase relative to control; **significant decrease relative to ANP.
Intravenous administration of ANP increased 30 min clearance of albumin compared to control by 2.3-fold in back skin and 1.3-fold in quadriceps muscle (P < 0.05, ANOVA). The 1.25-fold increase in hamstring muscle was borderline significant (ANOVA), but was significant with a one-tailed t test (P = 0.03). There was no trend for ANP alone to increase local vascular volume in skin and muscle, but with rolipram pre-treatment, ANP tended to increase the local vascular volume in skin and muscle. For example, in quadriceps muscle, local vascular volume in animals pre-treated with rolipram was significantly larger than either control or ANP alone (P < 0.05). An increase in local vascular volume is likely to reflect increased local perfusion due to vasodilatation with associated increased surface area for exchange. Thus, the increased 30 min clearance of albumin may be due to either an increased permeability or an increased surface area available for exchange, or a combination of the two. Thus, the observation that rolipram decreased albumin clearance even with increased local perfusion is consistent with a predominant action of rolipram to attenuate ANP-increased permeability in these tissues.
In order to distinguish potential changes in the vascular exchange surface between the groups that would contribute to the measured clearance, the ratio of 30 min clearance in μl (g dry weight)−1 to local vascular volume in μl (g dry weight)−1 was compared between the four groups. If the ratio of clearance to local vascular volume was not significantly different from control, the result would indicate that there was no real increase in vascular permeability and that most of the increase in clearance was due to increased local vascular volume and increased surface area for exchange. On the other hand, an increase in the ratio above control indicates a real increase in the apparent permeability of the vessel wall, especially if vascular volume tends to increase at the same time. The normalised 30 min clearance (Fig. 1B) showed a significant increase from control with ANP, and a significant decrease in the ANP normalized clearance with rolipram pre-treatment (P < 0.001, ANOVA) and support the conclusion that ANP caused real increases in microvascular permeability in skin and muscle tissue and this increased vascular permeability was significantly attenuated by rolipram pre-treatment.
Rolipram also tended to reduce baseline 30 min clearance in the groups receiving rolipram alone. The 30 min albumin clearances with rolipram plus ANP were also significantly reduced relative to vehicle control group (P < 0.05). Table 1 also includes measurements of total tissue water for all treatments in muscle and skin on a gram dry weight basis. There was no significant effect of ANP or rolipram on water content in skin or muscle. This was not surprising given that the water content expressed on a wet weight basis (600 μl g−1 in skin and >800 μl g−1 in muscle) is large compared with the volume shifts of the order of 200 μl per animal (approximately 7 μl g−1) required to account for haematocrit changes (see details below).
Table 2 summarizes measurements of 30 min albumin clearances in GI tissues and heart. Baseline clearances in all these tissues were 5 to 10 times larger than 30 min clearances in skin and muscle and there was more variability in the measurements than in skin and muscle for all treatments. In spite of larger clearances, the contribution of these GI segments to whole body albumin clearance is proportional to their weight, which is much smaller than for muscle and skin. Total GI tissue weight investigated was close to 0.5 g, about 2% of body weight. ANP tended to increase 30 min albumin clearance in all segments. Fold increases relative to control were: duodenum, 1.2 (P = 0.2); jejunum 1.7 (P = 0.06); ileum 2.2 (P = 0.03); colon 2.2 (P = 0.045); cecum 2.0 (P = 0.06); and rectum 2.7 (P = 0.08). P values are one-tailed t test. The tendency for local vascular volume to increase with ANP was much greater than in skin and muscle. For example, in jejunum, local vascular volume increased by the same ratio as 30 min clearance. Thus, as illustrated in Fig. 2, the 30 min clearances for jejunum and duodenum with ANP (Fig. 2A) when normalized to local vascular volume do not increase relative to control values. These results suggest that the ANP-induced 30 min clearance in duodenum and jejunum may be due, in large part, to local vasodilatation and increased area for exchange. When animals were pre-treated with rolipram, the ANP-dependent increase in 30 min clearance tended to be attenuated in ileum, cecum and rectum. As shown below, the contribution of changes in whole body albumin clearance in the presence of ANP or ANP plus rolipram in GI tissue calculated on the basis of these results is close to 10% of total changes in clearance so the additional experiments needed to further describe these small contributions were not justified. Most importantly, these data suggested that fluid shifts associated with vasodilatation in the absence of significant changes in permeability needed to be evaluated (see Discussion).
Table 2.
Local vascular volumes (μl (g dry wt)−1); 30 min albumin clearances (μl (g dry wt)−1); normalized albumin clearances, and water content (ml (g dry wt)−1) in heart and GI tissues
| Vehicle | ANP | Rolipram | Rolipram + ANP | |
|---|---|---|---|---|
| Vascular volume | ||||
| Heart | 160.3 ± 18.0 | 141.2 ± 15.9 | 160.6 ± 11.2 | 155.0 ± 31.8 |
| Duodenum | 140.4 ± 17.7 | 177.4 ± 30.2 | 155.7 ± 13.6 | 198.5 ± 21.6 |
| Jejunum | 78.6 ± 11.4 | 133.9 ± 13.4 | 79.4 ± 3.82 | 105.3 ± 13.52 |
| Ileum | 65.2 ± 11.3 | 102.1 ± 13.6 | 60.5 ± 4.9 | 83.3 ± 9.6 |
| Colon | 51.0 ± 16.5 | 60.2 ± 9.6 | 45.3 ± 9.5 | 70.2 ± 11.9 |
| Cecum | 50.5 ± 15.8 | 65.5 ± 7.5 | 48.8 ± 5.3 | 58.4 ± 4.6 |
| Rectum | 28.5 ± 4.3 | 45.6 ± 7.7 | 37.9 ± 7.6 | 55.6 ± 9.8 |
| Clearance | ||||
| Heart | 180.8 ± 25.9 | 204.0 ± 21.3 | 163.8 ± 29.2 | 131.8 ± 24.9 |
| Duodenum | 494.5 ± 81.1 | 577.3 ± 104.6 | 504.4 ± 16.5 | 702.9 ± 117.0 |
| Jejunum | 256.8 ± 49.2 | 441.2 ± 64.5 | 288.5 ± 64.8 | 331.2 ± 42.2 |
| Ileum | 135.1 ± 38.3 | 299.6 ± 58.01 | 149.4 ± 28.9 | 195.5 ± 32.8 |
| Colon | 99.8 ± 29.6 | 220.3 ± 56.71 | 195.7 ± 5.0 | 256.3 ± 45.9 |
| Cecum | 120.7 ± 36.7 | 245.8 ± 53.0 | 141.0 ± 12.8 | 173.5 ± 21.1 |
| Rectum | 70.9 ± 27.6 | 192.5 ± 47.8 | 112.5 ± 8.9 | 157.5 ± 49.5 |
| Normalized clearance | ||||
| Heart | 1.20 ± 0.18 | 1.52 ± 0.22 | 1.02 ± 0.17 | 0.89 ± 0.16 |
| Duodenum | 3.52 ± 0.46 | 3.39 ± 0.56 | 3.34 ± 0.41 | 3.52 ± 0.37 |
| Jejunum | 3.38 ± 0.57 | 3.48 ± 0.71 | 3.55 ± 0.66 | 3.26 ± 0.47 |
| Ileum | 2.18 ± 0.66 | 3.44 ± 0.98 | 2.61 ± 0.68 | 2.36 ± 0.35 |
| Colon | 2.55 ± 0.69 | 4.12 ± 1.11 | 4.89 ± 0.91 | 3.86 ± 0.82 |
| Cecum | 2.46 ± 0.76 | 4.07 ± 1.13 | 3.07 ± 0.56 | 3.04 ± 0.51 |
| Rectum | 2.41 ± 0.82 | 4.52 ± 1.17 | 3.30 ± 0.59 | 2.74 ± 0.56 |
| Water content | ||||
| Heart | 3.50 ± 0.11 | 3.16 ± 0.09 | 3.42 ± 0.20 | 3.68 ± 0.28 |
| Duodenum | 6.22 ± 0.57 | 6.17 ± 0.40 | 6.33 ± 1.07 | 6.18 ± 0.45 |
| Jejunum | 4.86 ± 0.36 | 5.80 ± 0.48 | 4.83 ± 0.21 | 4.53 ± 0.35 |
| Ileum | 4.51 ± 0.33 | 4.80 ± 0.15 | 4.34 ± 0.30 | 4.90 ± 0.30 |
| Colon | 5.04 ± 0.20 | 4.68 ± 0.17 | 5.27 ± 0.19 | 5.39 ± 0.20 |
| Cecum | 5.73 ± 0.33 | 6.11 ± 0.13 | 5.68 ± 0.17 | 6.19 ± 0.25 |
| Rectum | 4.33 ± 0.08 | 4.65 ± 0.22 | 4.63 ± 0.21 | 4.72 ± 0.16 |
P < 0.05:
when compared to Control;
when compared to ANP; Means ± SEM.
Figure 2. Thirty minute albumin clearances in GI tissues.
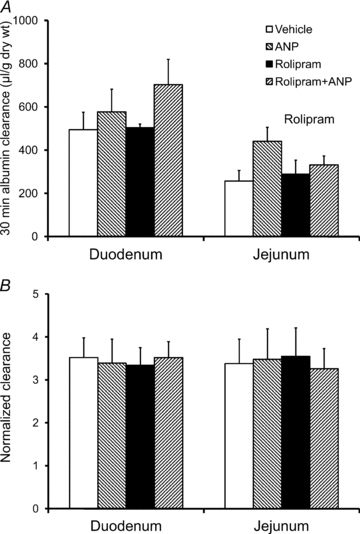
A, the 30 min albumin clearances are shown for duodenum and jejunum under the same 4 conditions as described in Fig. 1A: vehicle control, ANP, rolipram, and ANP plus rolipram. The variability reflects changes in both permeability and vascular perfusion. B, although ANP tends to increase 30 min clearance in duodenum and jejunum (Fig. 2A), the normalized clearances (30 min clearance divided by local vascular volume, Table 2) indicate no significant increase in real vascular permeability. The result indicates that changes in vascular perfusion (i.e. surface area for exchange) may account for the increased clearance in these tissues.
Rolipram pre-treatment significantly attenuated the loss of plasma volume caused by ANP. There was a significant increase in haematocrit measured 35 min after ANP infusion (46.8 ± 0.3 vs. 40.8 ± 0.6; P < 0.0001) (Fig. 3A). Rolipram alone did not change control haematocrit (P = 0.74). Haematocrit after ANP plus rolipram, 42.8 ± 1.2, was not significantly different from vehicle control (P = 0.13) and is significantly reduced compared with ANP (P = 0.0066). All measurements of haematocrit were measured on the single small blood sample drawn at the end of the experiment. The mean plasma volume in control experiments was 34.3 ± 1.3 μl g−1 (3.5% body weight). Taking the average plasma volume of a 30 g mouse as 1050 μl, the increase in haematocrit after ANP corresponded to a mean loss of 227 μl from the plasma volume. The error in this volume is estimated to be ±14%. We measured the increase in renal water excretion in animals with ANP treatment from a baseline of 75 ± 8 μl over a 65 min experimental period (30 min baseline infusion plus 35 min clearance measurement) to values close to 142 ± 28 μl for the same period (baseline plus 35 min with ANP). Assuming the 70 μl increase in water excretion is due only to ANP, and is added to the baseline level, the water excretion rate during ANP is 3.2 μl min−1 (70 + (75 × (35/65))/35), a 3-fold increase in water excretion rate relative to control (1.1 μl h−1). The extra 70 μl of renal water excretion with ANP is only 30% of the plasma volume loss during the same period (70/227), indicating that most of the plasma fluid was lost into the extravascular space, and not the result of urine excretion. Rolipram reduced renal water excretion back to values close to control (83 ± 11 μl), a reduction in renal water excretion of 60 μl. Since the plasma volume was restored to close to control values with rolipram, and renal water excretion was also restored to near control, the action of rolipram to reduce renal water excretion cannot account for all the fluid retained. In fact, rolipram pre-treatment accounts for almost the same fraction of the fluid retained as increased water excretion accounted for fluid loss with ANP.
Figure 3. Plasma volumes determined from haematocrit.
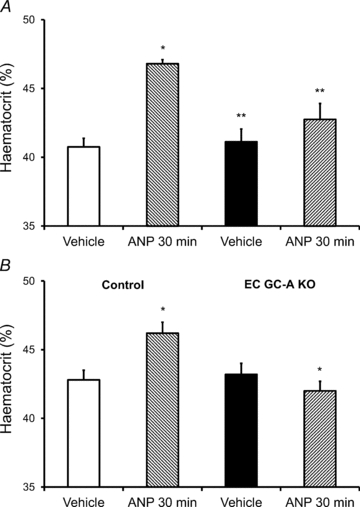
A, ANP caused a significant loss of plasma water as measured from the increase in haematocrit at the end of the ANP infusion. Rolipram significantly attenuated the loss of plasma fluid. *Significant increase relative to control (t test); **significant decrease relative to ANP alone. B, mice pre-treated with rolipram retain infused albumin solution to the same extent as mice lacking the receptor to ANP in endothelium (see Discussion (Sabrane et al. 2005)).
We also investigated albumin clearances in other tissues with low overall tissue masses similar to GI tissue. In heart tissue (0.3% BW) ANP tended to increase 30 min clearance but the increase was not significant (Table 2). Rolipram with ANP caused a decrease in 30 min clearance to less than control value, which was borderline significant compared with ANP alone (P = 0.06). There was no significant change in local vascular volume with ANP or rolipram. When 30 min clearances from heart were normalized to vascular volumes all changes in clearance were too small to achieve significance. In kidney (1% BW), ANP increased the 30 min albumin clearance from a baseline value of 590 ± 67 to 780 ± 81 μl(g dry weight)−1 (P = 0.05). This was decreased to 434.9 ± 31.4 μl(g dry weight)−1 with rolipram pre-treatment (P = 0.05, ANOVA). Rolipram pre-treatment reduced control clearance to 413.4 ± 36.6 μl(g dry weight)−1. Vascular volume also increased with ANP and was reduced with rolipram. The normalized clearance showed no significant difference with treatment suggesting local perfusion or other factors modulated kidney clearance. Calculations based on less than 0.3% free dye showed that the amount of free dye filtered at the glomerulus could not contribute significantly to the measured tissue clearances. The control 30 min albumin clearance in liver was 411 ± 56 μl(g dry weight)−1 and was not significantly modified by ANP or rolipram. This probably represents accumulation of labelled plasma proteins by the liver. We found a small decrease in spleen weight after treatment with ANP compared with control (67.3 ± 2.8 mg control vs. 60.7 ± 6.4 mg) and no change with rolipram treatment (rolipram plus ANP was 65.9 ± 2.7 mg) indicating no significant loss of plasma water into this organ in the mouse.
Discussion
Our results conform to the hypothesis that an agent that can stabilize endothelial barriers by increasing endothelial cell intracellular cAMP (in this case rolipram, an inhibitor of PDE4) significantly attenuates the ANP-dependent increases in albumin clearance in some, but not all organs of the mouse. Rolipram also attenuated the ANP-dependent fluid loss from the vascular space as measured by changes in haematocrit. These data enable the contribution of each of the different organs to plasma volume regulation by ANP to be evaluated as discussed in more detail below. After expressing the albumin clearances relative to measured local vascular volumes, our results suggest that the action of rolipram was to attenuate real increases in the ANP-dependent vascular permeability of the endothelium in skin, muscle and some GI tissue (ileum, colon, cecum and rectum). These are the tissues where there is normally a net reabsorption of fluid from the GI tract. On the other hand, an increase in surface area for exchange (associated with increased local plasma volume) appeared to account for ANP-dependent increases in albumin clearance in duodenum and jejunum. Most of the actions of rolipram to modify the ANP-dependent increase in clearance in duodenum, jejunum and the kidney could be attributed to changes in vascular perfusion. Overall, the tissues that responded to ANP by increasing vascular permeability also responded to rolipram with reduced permeability. Furthermore, in skin and muscle rolipram decreased baseline albumin clearance. Before we discuss these mechanistic insights below, we evaluate the methods to measure vascular and extravascular albumin accumulation and clearance using long-wavelength fluorescent tracers.
Analysis of methods and comparison of fluorescent vs. isotope measurements
We have recently described the application of the two tracer method to measure albumin blood-to-tissue clearance in mouse tissues using albumin labelled with 125I and 131I, and outlined in detail the strengths and limitations of the approach as previously reviewed for the methods as applied in the rat (Renkin & Tucker, 1998; Curry et al. 2010). The strengths include the ability to correct for albumin vascular content which can be as large as the 30 min albumin accumulation as illustrated in Tables 1 and 2. This correction for vascular content is often ignored in single tracer methods including forms of the Miles Assay (Nagy et al. 2008; Bates, 2010). Another strength is the ability to normalize the 30 min albumin clearance to vascular volume as a step towards distinguishing between real increases in microvascular permeability and increased clearance due to changes in microvascular perfusion, especially the effect of an increased number of perfused microvessels after vasodilatation. The further development of the method using long-wavelength fluorescent tracers was undertaken to overcome the problems of isotope availability and costs associated with the use of isotopes in animal experiments. Long-wavelength fluorescent tracers also offered the possibility of improved recovery and quantification of tracer accumulation with less problems posed by quenching compared with previously available fluorescent tracers including FITC and rhodamine-based tracers. Building on our experience to date, we conclude that the fluorescent method does overcome these problems but both methods remains technically demanding and time consuming. Both methods require the use of internal standards to correct for cross-talk between isotope counts or fluorescent intensity signals when both tracers are present in the tissue extract. The fluorescent method requires such standards for each tissue because of quenching and non-specific fluorescence interference after tracer extraction, and the extent of this problem varies with tissue. Isotope measurements are simpler and less time consuming, only involving radioactivity determination for isotopes in question and subsequent calculations, and not requiring the tissue extraction of tracers needed for the fluorescent technique. Both methods require that the amount of free dye be reduced to less than 0.3% of total label. This is because free label, having permeability up to three orders of magnitude greater than albumin, will result in an overestimate of tracer accumulation. In mice, both methods use very small sample size.
Table 3 compares the control values of mean albumin clearances in muscle and skin measured using fluorescent methods with the corresponding value measured using isotopes in wild-type mice (C57BL/6J) and with values in rat muscle and skin (Tucker et al. 1992). There is no clear trend in difference between the two techniques. Local plasma volumes measured using fluorescently labelled tracers are also compared. It is important to note that local plasma volumes in skin and muscle are low compared with other tissues. Typical values in muscle are close to 20 μl g−1 but local plasma volume range up to close to 100 μl g−1 in the heart and 500 μl g−1 in the kidney. Values of local plasma volume in all tissues on a per gram dry weight basis are similar to those measured in the rat.
Table 3.
Comparison of vehicle control albumin clearances and local plasma volumes measured using fluorescent method with values estimated using isotope methods in skin and muscle tissue of mouse and rat (units of clearance are μl min−1 (g dry wt)−1); units of local plasma volume are μl (g dry wt)−1)
| Mouse fluorescence1 | Mouse isotope2 | Rat isotope3 | |
|---|---|---|---|
| Clearance | |||
| Hamstring muscle | 0.38 | 0.22 | 0.15–0.17 |
| Quadriceps muscle | 0.30 | 0.35 | |
| Skin | 0.52 | 0.65 | 0.23–0.27 |
| Local vascular volume | |||
| Muscle | 23 | 20 | 23 |
| Skin | 9 | 20 | 17 |
Values from Fig. 1A divided by 30 (units per min);
From Curry et al. 2010;
From Tucker et al. 1992.
An estimate of apparent permeability to albumin is obtained by expressing the 30 min normalized clearances in Tables 1 and 2 as a rate (1 s−1, using 1800 s for the 30 min period) and multiplying by an estimate of the mean value of local vascular volume/surface area (Curry et al. 2010). Using a mean value of this ratio from measurements made from muscle and skin from MRI images in mice (4.4 × 10−4 cm; the estimate excludes vessels greater than 50 μm diameter), the mean baseline apparent albumin permeability coefficients estimated from the fluorescent measurements range from 1.3 × 10−7 cm s−1 in muscle to 6–8 × 10−7 cm s−1 in GI tissues. In muscle pre-treated with rolipram values fall as low as 0.9 × 10−7 cm s−1. These estimates would be larger if the local vascular volume contained vessels larger than 50 μm that do not contribute to exchange (for example, they increase 2-fold if half the local volume is not in exchange vessels). On the other hand, these values for apparent albumin permeability coefficients are 2–5 times larger than earlier estimates based on measurement of total microvessel exchange area (Renkin, 1977). We conclude that the fluorescence method provides reliable and consistent values of albumin clearance and is especially useful to overcome the safety, supply and regulatory issues associated with isotope usage.
Mechanism of action of rolipram and ANP
One action of ANP in normal endothelium is to increase hydrolysis of cAMP. For example, acting via the guanylate cyclase A (GC-A) receptor, ANP increases cGMP levels, which can cause cAMP hydrolysis by stimulating cGMP-dependent PDE2 (Lugnier, 2006; Surapisitchat et al. 2007). Rolipram will counter the fall in ANP-stimulated cAMP levels by inhibiting the PDE4-dependent hydrolysis of cAMP (Suttorp et al. 1993; Netherton & Maurice, 2005). As cAMP regulates the stability of intercellular junctions via the Epac–Rap–Rac pathway (Bos, 2005; Cullere et al. 2005; Adamson et al. 2008), the tendency of permeability of intercellular junctions to increase as local levels of cAMP falls is offset as cAMP levels rise. Local increases in cAMP levels also explain the action of rolipram to decrease permeability in skin and muscle below baseline values. This is consistent with a few previous observations indicating that baseline permeability to macromolecules can be decreased (Kramer et al. 1982; Yuan et al. 1993; Fu et al. 1998; Varma et al. 2002). On the other hand, in duodenum and jejunum the increase in albumin clearance with ANP could be understood as the predominant effect of ANP to relax vascular smooth muscle to cause vasodilatation in these tissues and increase clearance by increasing surface area for exchange (Renkin, 1984). The failure of rolipram to significantly attenuate ANP action is not unexpected because rolipram itself would cause vasodilatation if it raised cAMP levels in vascular smooth muscle (β-2 adrenergic effect). The actions of ANP and rolipram in the kidney are more complicated. It is known that molecules such as labelled albumin are exchanged into the medullary interstitium (Tenstad et al. 2001) and these proteins are shuttled back into the plasma via mechanisms that depend on the pressure difference between microvessels in the vasa recta and the high interstitial pressure in the kidney. Thus, it is likely that the predominant effects of ANP and rolipram are to modulate ANP-dependent changes in microvascular pressures in the renal medulla. However, their net effect to move albumin out of the plasma space over time periods comparable to our experiments is expected to be small. In the section below, we focus mainly on the action of ANP and rolipram to modulate net renal water excretion.
Rolipram attenuation of ANP permeability and volume changes
One fundamental question in investigations of plasma volume changes using intact animals is the contribution of renal water excretion, relative to transvascular water exchange, to the measured plasma volume changes. Our measurement of renal water excretion demonstrates that ANP does increase water excretion and rolipram pre-treatment does reduce this water loss. However, increased water excretion accounts for only 30% of the reduction of plasma volume after exposure to ANP. Furthermore, although renal water excretion is reduced by rolipram pre-treatment, this reduction also accounts for only 30% of the fluid retained in the plasma space when rolipram attenuates the ANP-induced fluid loss. Thus, the primary action of rolipram to attenuate ANP-dependent plasma fluid loss is a reduction in transvascular exchange of water and plasma proteins as evaluated further below.
Table 4 summarizes calculations of whole body albumin clearance taking into account individual tissue weights to obtain representative values in different organs for ANP- and rolipram-modulated changes in albumin distribution. In the baseline state total albumin clearance from skin, muscle, heart, GI tissues and kidney was 134 μl in 30 min. ANP increased the albumin clearance to 227 μl in 30 min, and rolipram pre-treatment reduced the clearance in the presence of ANP to 125 μl, close to the clearance with rolipram alone (107 μl). Thus, the increase in albumin clearance with ANP (93 μl) is more than offset by the reduction in ANP-induced albumin clearance by rolipram (102 μl). The tissues that contribute most significantly to the reduction in the ANP-induced increases in total clearance are skin and muscle, which together account for 70% of the total (70.1/102) while the GI tissues contribute 3% (3.3/102) to the rolipram reduction in whole body clearance. The conclusion that skin and muscle are the main sites determining blood-to-tissue redistribution of albumin is consistent with our previous investigations comparing albumin clearances in EC GC-A KO mice and their control littermates (Curry et al. 2010).
Table 4.
Contribution of tissue to total albumin clearance
| Tissue weight (g) | Control | ANP | Rolipram | Rolipram + ANP | |
|---|---|---|---|---|---|
| Muscle | 12 | 27.6 | 35.7 | 19.2 | 20.7 |
| Skin | 6 | 38.0 | 86.4 | 22.8 | 31.9 |
| Kidney | 0.3 | 40.5 | 58.5 | 32.4 | 31 |
| Heart | 0.1 | 4.5 | 5.1 | 4.1 | 3.3 |
| GI | 0.5 | 23.7 | 41.1 | 28.9 | 37.8 |
| Total | 134.3 | 226.8 | 107.4 | 124.7 |
All values are μl (30 min) −1 (30 g body wt) −1. To calculate total tissue clearance by adding the contributions from each tissue take the mean 30 min clearance on a dry weight basis (Table 1 or 2), divide by wet/dry ratio (2.5 for skin and 4 for all other tissues) to give clearance on a per gram wet weight basis, then multiply by average tissue weight.
While it is reasonable to conclude from the above calculations that plasma-to-tissue movement of macromolecules such as albumin in GI tissues does not contribute significantly to plasma volume regulation by changing the oncotic pressure differences, the role of increased filtration into tissues such as GI must also be considered. For example, if most of the increase in albumin clearance in GI tissue was the result of vasodilatation with increased surface area for exchange and increased filtration through microvessels, an increase in clearance by 5–7 μl (approximately half the total GI increase in clearance) could be accounted for by the mechanism of solvent drag caused by the additional filtration of 50–70 μl of fluid through the vascular wall having a reflection coefficient (σ) of 0.9 (ΔClearance = ΔJv(1 − σ) where ΔJv is the increase in filtration rate and is calculated as ΔClearance/(1 − σ)). The tissue where this mechanism appears to be most effective is the jejunum where normalized clearance ratios are consistent with changes in vascular perfusion rather than real increases in permeability, but both albumin clearance and water content are increased by ANP, and reduced by rolipram pre-treatment. On the other hand, a real increase in vascular permeability increases the plasma-to-tissue water exchange by reducing the effective oncotic pressure opposing filtration, and possibly increasing the hydraulic conductivity of the microvessels. We expect that this mechanism is dominant in skin and muscle tissue. Evaluation of these fluid shifts from the water content of individual tissues is difficult, because the amount of fluid responsible for changes in plasma volume (average values <10 μl g−1) are small compared with total water content (greater than 1000 μl g−1; see Tables 1 and 2). However, if we assume that some portion of the estimated 227 μl lost from the plasma with ANP that does not occur via renal excretion (70 μl) or GI tissue (80 μl) moves into skin and muscle tissue, then one estimate of this volume (227–70–80 μl) is approximately 80 μl. This volume can be accounted for if increased albumin clearance into skin and muscle increases the net effective filtration pressure by <2.0 mmHg over 30 min. The calculation assumes the average filtration coefficient of mouse skin and muscle is close to 0.01 ml min−1 mmHg−1 for 100 g tissue (an average value for mammalian skin and muscle; Landis & Pappenheimer, 1963; Michel & Curry, 1999) and corresponds to a change in transvascular albumin concentration difference of less than 10% of the normal plasma albumin concentration (25 mg ml−1). This estimate is consistent with the net increase in albumin clearance with ANP of 93 μl which is <10% of the total plasma protein when the plasma volume is close to 1000 μl.
Rolipram and volume expansion
The results using rolipram to attenuate ANP-induced changes of albumin clearance and haematocrit are consistent with our previous conclusions based on measurements of ANP clearances in EC GC-A KO mice. Figure 3 compares haematocrit in EC GC-A KO mice with and without ANP (Fig. 3B) to haematocrit in rolipram pre-treated mice with and without ANP (Fig. 3A). Rolipram attenuated the ANP-induced increase in haematocrit to the same extent as endothelial-specific knockout of the ANP receptor. The phenotype that develops in the EC GC-A KO mouse is a hypervolumic, hypertensive mouse with cardiac hypertrophy but with normal vasodilator and renal function. When these mice were subjected to a plasma volume expansion, the infused fluid was retained in the plasma space, even though ANP increased (Schreier et al. 2008). These responses can be explained at least in part by the failure of ANP to regulate plasma volume. The main conclusion from the present experiments is that pharmacological attenuation of ANP-dependent increases in vascular albumin permeability using PDE4 inhibition attenuates ANP-dependent fluid shifts from the plasma volume. The present experiments therefore suggest that an acute attenuation of ANP responses to increase vascular endothelial permeability using agents that increase endothelial cAMP may be useful to explore as part of a strategy to stabilize the endothelium under conditions when ANP is released (e.g. intravenously infused fluids for pre-surgical volume expansion). In this regard it is of interest that pre-treatment of sheep with adrenergic agents such as isoproterenol (isoprenaline) enhance fluid retention (Vane et al. 2004; Kinsky et al. 2008).
Acknowledgments
This work was supported by a grant from the National Institutes of Health, Heart Lung, and Blood Institute HL28607, and by pilot funds from the Clinical and Translational Science Center, UC Davis, made possible by a grant from the National Center for Research Resources UL1 RR024146.
Glossary
Abbreviations
- ANP
atrial natriuretic peptide
- BK
bradykinin
- BSA
bovine serum albumin
- BW
body weight
- EC
endothelial cell
- GC-A
guanylyl cyclase-A receptor
- GI
gastrointestinal
- IP
intra-peritoneal
- KO
knock-out
- PBS
phosphate-buffered saline
- PDE2
phosphodiesterase 2
- PDE4
phosphodiesterase 4
- PKA
protein kinase A
Author contributions
Y.-C.L., H.S., F.E.C., R.K.R., E.M.R. and R.H.A. contributed to the conception and design of experiments. J.F.C., Y.-C.L., H.S., R.H.A., F.E.C. and R.K.R. contributed to the collection, analysis and interpretation of experiments. F.E.C. wrote the initial draft of the manuscript and Y.-C.L., R.K.R., R.H.A. and J.F.C. contributed to writing and revising the manuscript. The experiments were carried out in Davis. All authors approved the final version of the manuscript.
References
- Adamson RH, Ly JC, Sarai RK, Lenz JF, Altangerel A, Drenckhahn D, Curry FE. Epac/Rap1 pathway regulates microvascular hyperpermeability induced by PAF in rat mesentery. Am J Physiol Heart Circ Physiol. 2008;294:H1188–H1196. doi: 10.1152/ajpheart.00937.2007. [DOI] [PubMed] [Google Scholar]
- Alvarez A, Piqueras L, Blazquez MA, Sanz MJ. Cyclic AMP elevating agents and nitric oxide modulate angiotensin II-induced leukocyte-endothelial cell interactions in vivo. Br J Pharmacol. 2001;133:485–494. doi: 10.1038/sj.bjp.0704096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates DO. Vascular endothelial growth factors and vascular permeability. Cardiovasc Res. 2010;87:262–271. doi: 10.1093/cvr/cvq105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bos JL. Linking Rap to cell adhesion. Curr Opin Cell Biol. 2005;17:123–128. doi: 10.1016/j.ceb.2005.02.009. [DOI] [PubMed] [Google Scholar]
- Cullere X, Shaw SK, Andersson L, Hirahashi J, Luscinskas FW, Mayadas TN. Regulation of vascular endothelial barrier function by Epac, a cAMP-activated exchange factor for Rap GTPase. Blood. 2005;105:1950–1955. doi: 10.1182/blood-2004-05-1987. [DOI] [PubMed] [Google Scholar]
- Curry FR, Rygh CB, Karlsen T, Wiig H, Adamson RH, Clark JF, Lin YC, Gassner B, Thorsen F, Moen I, Tenstad O, Kuhn M, Reed RK. Atrial natriuretic peptide modulation of albumin clearance and contrast agent permeability in mouse skeletal muscle and skin: role in regulation of plasma volume. J Physiol. 2010;588:325–339. doi: 10.1113/jphysiol.2009.180463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elwood W, Sun J, Barnes PJ, Giembycz MA, Chung KF. Inhibition of allergen-induced lung eosinophilia by type-III and combined type III- and IV-selective phosphodiesterase inhibitors in brown-Norway rats. Inflamm Res. 1995;44:83–86. doi: 10.1007/BF01793218. [DOI] [PubMed] [Google Scholar]
- Fu BM, Adamson RH, Curry FE. Test of a two-pathway model for small-solute exchange across the capillary wall. Am J Physiol Heart Circ Physiol. 1998;274:H2062–H2073. doi: 10.1152/ajpheart.1998.274.6.H2062. [DOI] [PubMed] [Google Scholar]
- Fukuhara S, Sakurai A, Sano H, Yamagishi A, Somekawa S, Takakura N, Saito Y, Kangawa K, Mochizuki N. Cyclic AMP potentiates vascular endothelial cadherin-mediated cell-cell contact to enhance endothelial barrier function through an Epac-Rap1 signaling pathway. Mol Cell Biol. 2005;25:136–146. doi: 10.1128/MCB.25.1.136-146.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinsky MP, Vaid SU, Vane LA, Prough DS, Kramer GC. Effect of esmolol on fluid therapy in normovolemia and hypovolemia. Shock. 2008;30:55–63. doi: 10.1097/SHK.0b013e31815d1a85. [DOI] [PubMed] [Google Scholar]
- Kooistra MR, Corada M, Dejana E, Bos JL. Epac1 regulates integrity of endothelial cell junctions through VE-cadherin. FEBS Lett. 2005;579:4966–4972. doi: 10.1016/j.febslet.2005.07.080. [DOI] [PubMed] [Google Scholar]
- Kramer GC, Harms BA, Bodai BI, Demling RH, Renkin EM. Mechanisms for redistribution of plasma protein following acute protein depletion. Am J Physiol Heart Circ Physiol. 1982;243:H803–H809. doi: 10.1152/ajpheart.1982.243.5.H803. [DOI] [PubMed] [Google Scholar]
- Landis EM, Pappenheimer JR. Exchange of substances through the capillary walls. In: Hamilton WF, editor. Handbook of Physiology Circulation. Washington, DC: American Physiological Society; 1963. pp. 961–1034. [Google Scholar]
- Lugnier C. Cyclic nucleotide phosphodiesterase (PDE) superfamily: a new target for the development of specific therapeutic agents. Pharmacol Ther. 2006;109:366–398. doi: 10.1016/j.pharmthera.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Michel CC, Curry FE. Microvascular permeability. Physiol Rev. 1999;79:703–761. doi: 10.1152/physrev.1999.79.3.703. [DOI] [PubMed] [Google Scholar]
- Moy AB, Bodmer JE, Blackwell K, Shasby S, Shasby DM. cAMP protects endothelial barrier function independent of inhibiting MLC20-dependent tension development. Am J Physiol Lung Cell Mol Physiol. 1998;274:L1024–L1029. doi: 10.1152/ajplung.1998.274.6.L1024. [DOI] [PubMed] [Google Scholar]
- Nagy JA, Benjamin L, Zeng H, Dvorak AM, Dvorak HF. Vascular permeability, vascular hyperpermeability and angiogenesis. Angiogenesis. 2008;11:109–119. doi: 10.1007/s10456-008-9099-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nedrebo T, Reed RK, Berg A. Effect of α-trinositol on interstitial fluid pressure, edema generation, and albumin extravasation after ischemia-reperfusion injury in rat hind limb. Shock. 2003;20:149–153. doi: 10.1097/01.shk.0000072128.33223.15. [DOI] [PubMed] [Google Scholar]
- Netherton SJ, Maurice DH. Vascular endothelial cell cyclic nucleotide phosphodiesterases and regulated cell migration: implications in angiogenesis. Mol Pharmacol. 2005;67:263–272. doi: 10.1124/mol.104.004853. [DOI] [PubMed] [Google Scholar]
- Pedram A, Razandi M, Levin ER. Deciphering vascular endothelial cell growth factor/vascular permeability factor signaling to vascular permeability. Inhibition by atrial natriuretic peptide. J Biol Chem. 2002;277:44385–44398. doi: 10.1074/jbc.M202391200. [DOI] [PubMed] [Google Scholar]
- Qiao J, Huang F, Lum H. PKA inhibits RhoA activation: a protection mechanism against endothelial barrier dysfunction. Am J Physiol Lung Cell Mol Physiol. 2003;284:L972–L980. doi: 10.1152/ajplung.00429.2002. [DOI] [PubMed] [Google Scholar]
- Renkin EM. Multiple pathways of capillary permeability. Circ Res. 1977;41:735–743. doi: 10.1161/01.res.41.6.735. [DOI] [PubMed] [Google Scholar]
- Renkin EM. Control of microcirculation and blood-tissue exchange. In: Renkin EM, Michel CC, editors. Handbook of Physiology. Bethesda, MD: American Physiological Society; 1984. pp. 375–409. [Google Scholar]
- Renkin EM, Tucker VL. Measurement of microvascular transport parameters of macromolecules in tissues and organs of intact animals. Microcirculation. 1998;5:139–152. [PubMed] [Google Scholar]
- Sabrane K, Kruse MN, Fabritz L, Zetsche B, Mitko D, Skryabin BV, Zwiener M, Baba HA, Yanagisawa M, Kuhn M. Vascular endothelium is critically involved in the hypotensive and hypovolemic actions of atrial natriuretic peptide. J Clin Invest. 2005;115:1666–1674. doi: 10.1172/JCI23360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreier B, Borner S, Volker K, Gambaryan S, Schafer SC, Kuhlencordt P, Gassner B, Kuhn M. The heart communicates with the endothelium through the guanylyl cyclase-A receptor: acute handling of intravascular volume in response to volume expansion. Endocrinology. 2008;149:4193–4199. doi: 10.1210/en.2008-0212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stelzner TJ, Weil JV, O’Brien RF. Role of cyclic adenosine monophosphate in the induction of endothelial barrier properties. J Cell Physiol. 1989;139:157–166. doi: 10.1002/jcp.1041390122. [DOI] [PubMed] [Google Scholar]
- Surapisitchat J, Jeon KI, Yan C, Beavo JA. Differential regulation of endothelial cell permeability by cGMP via phosphodiesterases 2 and 3. Circ Res. 2007;101:811–818. doi: 10.1161/CIRCRESAHA.107.154229. [DOI] [PubMed] [Google Scholar]
- Suttorp N, Weber U, Welsch T, Schudt C. Role of phosphodiesterases in the regulation of endothelial permeability in vitro. J Clin Invest. 1993;91:1421–1428. doi: 10.1172/JCI116346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teixeira MM, Rossi AG, Williams TJ, Hellewell PG. Effects of phosphodiesterase isoenzyme inhibitors on cutaneous inflammation in the guinea-pig. Br J Pharmacol. 1994;112:332–340. doi: 10.1111/j.1476-5381.1994.tb13073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenstad O, Heyeraas KJ, Wiig H, Aukland K. Drainage of plasma proteins from the renal medullary interstitium in rats. J Physiol. 2001;536:533–539. doi: 10.1111/j.1469-7793.2001.0533c.xd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker VL, Simanonok KE, Renkin EM. Tissue-specific effects of physiological ANP infusion on blood-tissue albumin transport. Am J Physiol Regul Integr Comp Physiol. 1992;263:R945–R953. doi: 10.1152/ajpregu.1992.263.4.R945. [DOI] [PubMed] [Google Scholar]
- van Nieuw Amerongen GP, van Hinsbergh VW. Targets for pharmacological intervention of endothelial hyperpermeability and barrier function. Vascul Pharmacol. 2002;39:257–272. doi: 10.1016/s1537-1891(03)00014-4. [DOI] [PubMed] [Google Scholar]
- Vane LA, Prough DS, Kinsky MA, Williams CA, Grady JJ, Kramer GC. Effects of different catecholamines on the dynamics of volume expansion of crystalloid infusion. Anesthesiology. 2004;101:1136–1144. doi: 10.1097/00000542-200411000-00013. [DOI] [PubMed] [Google Scholar]
- Varma S, Breslin JW, Lal BK, Pappas PJ, Hobson RW, 2nd, Duran WN. p42/44MAPK regulates baseline permeability and cGMP-induced hyperpermeability in endothelial cells. Microvasc Res. 2002;63:172–178. doi: 10.1006/mvre.2001.2381. [DOI] [PubMed] [Google Scholar]
- Waschke J, Drenckhahn D, Adamson RH, Barth H, Curry FE. cAMP protects endothelial barrier functions by preventing Rac-1 inhibition. Am J Physiol Heart Circ Physiol. 2004;287:H2427–H2433. doi: 10.1152/ajpheart.00556.2004. [DOI] [PubMed] [Google Scholar]
- Yuan Y, Granger HJ, Zawieja DC, DeFily DV, Chilian WM. Histamine increases venular permeability via a phospholipase C-NO synthase-guanylate cyclase cascade. Am J Physiol Heart Circ Physiol. 1993;264:H1734–H1739. doi: 10.1152/ajpheart.1993.264.5.H1734. [DOI] [PubMed] [Google Scholar]


