In patients with severe gastroesophageal reflux disease post gastric bypass surgery, endoscopic plication with revision of the gastric pouch may be beneficial.
Keywords: Gastric bypass, Bariatric, Natural orifice, Revision, Endoscopic, Plication
Abstract
Objective:
A new technique for endoscopic plication and revision of the gastric pouch (EPRGP) for patients who underwent gastric bypass (RGB) surgery was evaluated in patients with severe GERD, dumping syndrome, failure of weight loss, or all of these.
Patients and Methods:
Patients underwent EPRGP over a 12-month period. The StomaphyX device (Endogastric Solutions, Redmond, WA) was utilized over a standard flexible gastroscope. Patients were kept on a liquid diet for 1 week.
Results:
The study included 64 patients with a mean age of 48 years who underwent 67 procedures. EPRGP was performed an average of 5 years after RGB. The mean preoperative BMI was 39.5 kg/m2. The primary indications for the procedure were inadequate weight loss, dumping syndrome (42), and GERD (15). The mean follow-up period was 5.8 months (range, 3 to 12). The average operative time was 50 minutes, with a significant reduction with increased operator experience. There were only 2 (3%) intraoperative complications during the early period (equipment failure), which did not result in any morbidity. All symptoms from dumping syndrome or reflux improved, with no further operative-related complications. The mean weight loss was 7.3kg.
Conclusions:
This study demonstrates the technical feasibility, safety, and efficacy of EPRGP.
INTRODUCTION
Dilation of the gastrojejunal anastomosis and the gastric pouch may result in weight regain, worsening dumping syndrome, and bile reflux following Roux-en-Y gastric bypass for morbid obesity. Allthough some long-term weight gain after obesity surgery is considered normal or physiologic, significant weight gain years after surgery can be heartbreaking for patients. Anatomic causes, such as dilation and gastro-gastric fistula, have become an increasing concern.1 Gastro-gastric fistula has been reported to occur in 1% to 4% of patients but may be underreported or asymptomatic until patients are evaluated for causes of failure to lose weight.2 Significant weight gain has been reported in up to 25% of patients following gastric bypass surgery.3 Up to 12% of patients will have some type of surgical revision following gastric bypass surgery due to weight gain or postoperative symptoms related to stomal dilation.4 Reoperation can present significant technical challenges to the surgeon and result in appreciable morbidity or mortality.5 Patients who undergo operative revision have a lengthy operation, a major complication rate of 14%, and a mortality rate of 1.3%.6,7
Newer technologies, such as injection with sodium morrhuate8 and transoral endoscopic plication9 have been recently used to minimize the need to operatively revise the gastrojejunostomy and may minimize these risks.
The present study prospectively evaluates the safety and early outcomes of endoscopic plication and revision of the gastric pouch (EPRGP) for dumping syndrome, bile reflux, weight regain, and gastro-gastric fistula.
METHODS
Over a 1-year period from June 2008 to June 2009, 64 adult patients who had previously undergone Roux-en-Y gastric bypass surgery underwent EPRGP at a single hospital. Bariatric surgeons performed all procedures. Only patients who had their original gastric bypass operation more than 2 years earlier were considered for endoscopic revision. All patients underwent preoperative upper gastrointestinal series and upper gastrointestinal endoscopy. EPRGP was advised for patients who failed to lose sufficient weight after gastric bypass surgery or for severe dumping or reflux. Severity of gastrointestinal symptoms was elicited before and after endoscopic surgery using a questionnaire.10 Severe dumping syndrome was defined as more than 3 episodes of postprandial diarrhea per week. GERD symptoms were confirmed radiologically or by endoscopic observation of bile reflux into the gastric pouch. The location and diameter of the gastrojejunal anastomosis and gastroesophageal junction was recorded. The length of the gastric pouch was calculated. All patients were admitted to the hospital the day of surgery and underwent general endotracheal anesthesia. The StomaphyX device (EndoGastric Solutions, Redmond, WA) was placed over a standard 9-mm endoscope in all cases. The gastroscope was used to calibrate the new anastomotic diameter. Suction was used through the endoscope and through the StomaphyX device to draw the gastric wall into the operative chamber. Serial endoscopic placations with 3-0 polypropylene “H” fasteners started approximately 1cm above the gastrojejunostomy and proceeded circumferentially to approximately 1cm below the gastroesophageal junction. Two fasteners were placed at each location. Fasteners were placed at 6 locations at each level, generally spaced 1cm to 2cm apart. Following the completion of the procedure, repeat upper gastrointestinal endoscopy was performed to inspect the revised stoma and gastric pouch. Repeat measurements were taken, and the operative site was inspected for hemostasis and parietal integrity. All patients were extubated in the operating room. Patients who developed postoperative emesis were given intravenous odansteron and decadron for persistent emesis.
Following hospital discharge, all patients were maintained on a liquid diet for one week and received postprocedure dietary counseling. Patients were followed for a minimum of 3 months (range 3 to 12). Patients with gastro-gastric fistula were evaluated in the postoperative period with a Gastrografin upper GI series.
RESULTS
Fifty-nine females and 5 males with a mean age of 48 years underwent per-oral EPGRP. Three patients underwent a second procedure less than one year later due to disappointing clinical and radiological results. The mean body mass index (BMI) before gastric bypass surgery was 48.5kg/m2. Patients had reached an average nadir BMI of 31kg/m2 and had an average BMI of 39.5kg/m2 just before endoscopic revision. Revision was performed an average of 5 years (range, 2 to 10) after the original gastric bypass operation. An average of 23 “H” fasteners were used per case (range, 20 to 40). The mean operating room time was 50 minutes. All but 2 patients were discharged to home within 24 hours. One patient was observed for bleeding from the site of plication but never required transfusion. The other remained in the hospital because of transient emesis that required parenteral therapy. There were no major complications or deaths. Two cases of device failures occurred during the study, and the procedure was eventually performed with another device and without complication. Most patients had complaints of a minor irritation of the pharynx. Sixty-five percent of patients experienced some epigastric pain and about half required intravenous medication for nausea or emesis. The mean follow-up was 5.8 months.
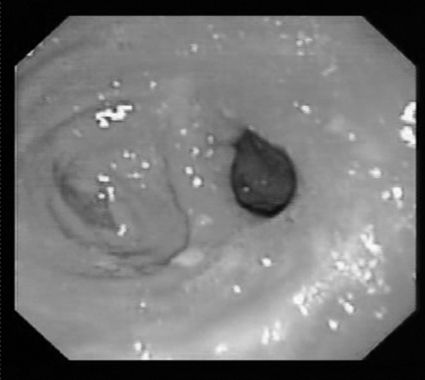
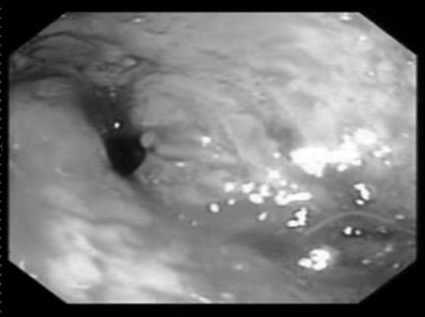
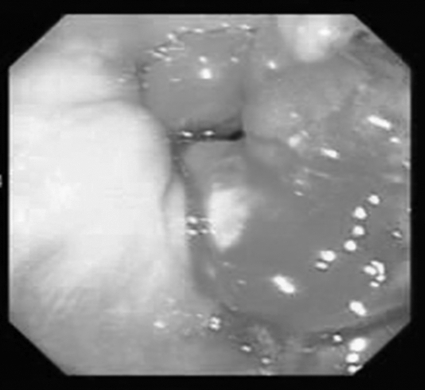
The diameter of the anastomosis was reduced from an average of 2.2cm to about 9mm. The length of the gastric pouch was reduced by about 33%. Figures 1 and 2 are endoscopic photographs of the preoperative appearance of the dilated and postoperatively reduced diameter of the gastrojejunostomy. Figure 3 shows the appearance of the gastroesophageal junction and reduced gastric pouch following endoscopic revision.
Figure 1.
Preoperative endoscopic photograph of the gastrojejunostomy.
Figure 2.
Endoscopic photograph of gastrojejunostomy following endoscopic revision.
Figure 3.
Endoscopic photograph of the gastroesophageal junction and endoscopically reduced gastric pouch.
Forty-two patients (66%) underwent the procedure due to severe dumping syndrome. Symptoms were improved in all patients and completely relieved in 30 patients (71%). Fifteen patients had severe reflux resulting from a patulous gastrojejunal anastomosis. GERD symptoms were improved in 80% of patients and completely relieved in 20%. Four patients were found on endoscopic inspection to have a gastro-gastric fistula, which was successfully closed using the StomaphyX device and verified by a postoperative Gastrografin upper GI series.
Weight loss ranged from 0kg to 31kg (mean 7.3), and 79% of patients never regained weight during follow-up.
DISCUSSION
Per-oral endoscopic plication and revision of the gastric pouch is a safe and technically simple procedure to perform for bariatric surgeons comfortable with gastrointestinal endoscopy. The early outcomes of this natural orifice technique demonstrate that it offers some weight loss and remediation of symptoms of dumping syndrome and gastroesophageal reflux, without the need to perform open or laparoscopic revision. Weight loss may be modest, but patients with progressive weight gain following gastric bypass surgery benefit from this procedure, if radiological or endoscopic inspection demonstrates an anatomic cause, such as stomal or pouch dilation.
Endoscopic plication of the stoma following Roux-en-Y gastric bypass surgery was initially reported in 2004.11 Studies have reported the benefits of reduction of the diameter of the gastrojejunostomy. Thompson and coworkers12 reported on 11 patients who underwent stomal reduction with endoscopic suturing without complication and resulting in modest weight loss. Other techniques to reduce the stomal diameter have included the injection of sodium morrhuate. Catalano13 reported success in reducing the stomal diameter to 1.2cm in 64% of patients but required up to 3 sessions. One patient developed an anastomotic stricture that required endoscopic balloon dilation.13 The Food and Drug Administration approved the StomaphyX device in 2007. Since that time, its application for the endoscopic revision of postbariatric surgical patients has increased dramatically. It offers the endoscopic bariatric surgeon the ease, safety, and reliability of plication of the gastric pouch with nonabsorbable polypropylene fasteners. Surgeons have begun to utilize this device to not only reduce the diameter of the gastrojejunostomy, but also to reduce the size of the gastric pouch, repair acquired gastro-gastric fistulas, and even remediate early postoperative leaks.14 To date, published prospective experience with this technique has been limited. Mikami et al15 reported on a group of 39 similar patients who underwent endoscopic revision. They reported an average weight loss of 10kg at one year. They also describe minimal postprocedure complications limited to transient pharyngitis and epigastric pain. The ROSE procedure utilizes a different technique to reduce stomal diameter. This also appears to be a safe procedure.16 Results are similar in the success rate of reducing the diameter of the gastrojejunostomy and an average weight loss of 8.8kg.17
Although the weight loss is modest, there is a clear benefit to patients with bile reflux or severe dumping syndrome. With more than a million patients having had gastric bypass surgery in the past 10 years, it is anticipated that many patients will require some revision as a result of anatomical failure of their procedure, resulting in weight gain, severe dumping, or gastroesophageal reflux. As natural orifice techniques are refined, they should be more applicable to patients who require revision, and reduce the number of laparoscopic and open surgical revision procedures thus minimizing the morbidity of patients who require it after gastric bypass surgery. Longer follow-up will be necessary to determine whether the benefits presented in the present study are durable.
Footnotes
Presented at the 18th Society of Laparoendoscopic Surgeons Annual Meeting and Endo Expo 2009, Boston, Massachusetts, USA, September 9–12, 2009.
Contributor Information
I. Michael Leitman, Department of Surgery, Beth Israel Medical Center, New York, New York, USA..
Chiranjiv S Virk, Department of Surgery, Beth Israel Medical Center, New York, New York, USA..
Dimitrios V. Avgerinos, Department of Surgery, Beth Israel Medical Center, New York, New York, USA..
Radha Patel, Department of Surgery, Beth Israel Medical Center, New York, New York, USA..
Valentina Lavarias, Department of Surgery, Beth Israel Medical Center, New York, New York, USA..
Burton Surick, Department of Surgery, Beth Israel Medical Center, New York, New York, USA..
John L. Holup, Department of Surgery, Beth Israel Medical Center, New York, New York, USA..
Elliot R. Goodman, Department of Surgery, Beth Israel Medical Center, New York, New York, USA..
Martin S. Karpeh, Jr., Department of Surgery, Beth Israel Medical Center, New York, New York, USA..
References:
- 1. Campos GM, Rabl C, Mulligan K, et al. Factors associated with weight loss after gastric bypass. Arch Surg. 2008. September;143(9):877–883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Carrodeguas L, Szomstein S, Soto F, et al. Management of gastrogastric fistulas after divided Roux-en-Y gastric bypass surgery for morbid obesity: analysis of 1,292 consecutive patients and review of literature. Surg Obes Relat Dis. 2005;1(5):467–474 [DOI] [PubMed] [Google Scholar]
- 3. Shah M, Simha V, Garg A. Review: long-term impact of bariatric surgery on body weight, comorbidities, and nutritional status. J Clin Endocrinol Metab. 2006;91(11):4223–4231 [DOI] [PubMed] [Google Scholar]
- 4. Gagner M, Gentileschi P, de Csepel J, et al. Laparoscopic Reoperative Bariatric Surgery: Experience from 27 consecutive patients. Obes Surg. 2002;12(2):254–260 [DOI] [PubMed] [Google Scholar]
- 5. Hallowell PT, Stellato TA, Yao DA, Robinson A, Schuster MM, Graf KN. Should bariatric revisional surgery be avoided secondary to increased morbidity and mortality? Am J Surg. 2009;197(3):391–396 [DOI] [PubMed] [Google Scholar]
- 6. Jones KB. Revisional bariatric surgery-potentially safe and effective. Surg Obes Rel Dis. 2005;1(6):599–603 [DOI] [PubMed] [Google Scholar]
- 7. Poulose BK, Griffin MR, Moore DE, et al. Risk factors for post-operative mortality in bariatric surgery. J Surg Res. 2005;127(1):1–7 [DOI] [PubMed] [Google Scholar]
- 8. Morton JM. Weight gain after bariatric surgery as a result of large gastric stoma: endotherapy with sodium morrhuate to induce stomal stenosis may prevent the need for surgical revision. Gastrointest Endosc. 2007. August;66(2):246–247 [DOI] [PubMed] [Google Scholar]
- 9. Herron DM, Birkett DH, Thompson CC, Bessler M, Swanström LL. Gastric bypass pouch and stoma reduction using a transoral endoscopic anchor placement system: a feasibility study. Surg Endosc. 2008. April;22(4):1093–1099 [DOI] [PubMed] [Google Scholar]
- 10. Suter M, Calmes JM, Paroz A, Giusti V. A new questionnaire for quick assessment of food tolerance after bariatric surgery. Obes Surg. 2007;17(1):2–8 [DOI] [PubMed] [Google Scholar]
- 11. Schweitzer M. Endoscopic intraluminal suture plication of the gastric pouch and stoma in postoperative Roux-en-Y gastric bypass patients. J Laparoendosc Adv Surg Tech A. 2004;14(4):223–226 [DOI] [PubMed] [Google Scholar]
- 12. Thompson CC, Slattery J, Bundga ME, Lautz DB. Peroral endoscopic reduction of dilated gastrojejunal anastomosis after Roux-en-Y gastric bypass: a possible new option for patients with weight regain. Surg Endosc. 2006;20(11):1744–1748 [DOI] [PubMed] [Google Scholar]
- 13. Catalano MF, Rudic G, Anderson AJ, Chua TY. Weight gain after bariatric surgery as a result of a large gastric stoma: endotherapy with sodium morrhuate may prevent the need for surgical revision. Gastrointest Endosc. 2007;66(2):240–245 [DOI] [PubMed] [Google Scholar]
- 14. Overcash WT. Natural orifice surgery (NOS) using StomaphyX for repair of gastric leaks after bariatric revisions. Obes Surg. 2008;18(7):882–885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mikami D, Needleman B, Narula V, Durant J, Melvin WS. Natural orifice surgery: initial US experience utilizing the StomaphyX device to reduce gastric pouches after Roux-en-Y gastric bypass. Surg Endosc. 2010;24(1):223–228 [DOI] [PubMed] [Google Scholar]
- 16. Ryou M, Mullady DK, Lautz DB, Thompson CC. Pilot study evaluating technical feasibility and early outcomes of second-generation endosurgical platform for treatment of weight regain after gastric bypass surgery. Surg Obes Relat Dis. 2009;5(4):450–454 [DOI] [PubMed] [Google Scholar]
- 17. Mullady DK, Lautz DB, Thompson CC. Treatment of weight regain after gastric bypass surgery when using a new endoscopic platform: initial experience and early outcomes (with video). Gastrointest Endosc. 2009;70(3):440–444 [DOI] [PubMed] [Google Scholar]