Single incision laparoscopic access appears to be a safe, feasible technique for performing laparoscopic sleeve gastrectomy.
Keywords: Bariatric surgery, Laparoscopic sleeve gastrectomy, Single-incision laparoscopic surgery, Liver retraction
Abstract
Introduction:
Laparoscopic sleeve gastrectomy has rapidly gained popularity in the field of bariatric surgery, mainly due to its low morbidity and mortality. Traditionally, 4 to 6 trocars are used. Single-access surgery has emerged as an attempt to decrease incisional morbidity and enhance cosmetic benefits. We present our initial 7 patients undergoing single-incision laparoscopic sleeve gastrectomy using a novel technique for liver retraction.
Methods:
Patients who underwent single-incision laparoscopic sleeve gastrectomy between March 2009 and May 2009 were analyzed. A 4-cm left paramedian incision was used. Laparoscopic sleeve gastrectomy was performed in a standard fashion using a 40 French bougie.
Results:
Seven patients underwent single-incision sleeve gastrectomy at the University of Illinois at Chicago. They were all female with a mean age of 34 years. Preoperative BMI was 49kg/m2 (range, 39 to 64). There were no intraoperative complications. Mean operative time was 103 minutes. Estimated blood loss was minimal. All 7 patients were discharged on postoperative day 2 and were doing well without any complications at 3.1±0.7 months after surgery.
Conclusion:
Single-incision laparoscopic sleeve gastrectomy is safe and feasible and can be performed without changing the existing principles of the procedure. Our technique for internal liver retraction provides adequate exposure and is reproducible. Development of improved standard instrumentation is required for this technique to become popular.
INTRODUCTION
Advances in minimally invasive surgery have revolutionized the field of bariatric surgery. All major bariatric operations are routinely performed laparoscopically, and numerous technological advancements have led to innovations that push the boundaries of defining minimally invasive surgery. Natural orifice transluminal endoscopic surgery (NOTES) techniques are developing worldwide to perform intraabdominal operations without a skin incision; however, concerns about safety and technical limitations have slowed its introduction into mainstream clinical practice. For these reasons, single-incision laparoscopic techniques have gained in popularity, in addition to the ability to reproduce the same surgical procedures with a less invasive approach.1–3 Nevertheless, the application of single-incision techniques in the field of bariatric surgery has yet to be established. Clearly, the high-risk patient population, the complexity of the procedures, and the current instrumentation are some of the major impediments to the wide implementation of these techniques. To date, only a handful of reports on this topic are available in the literature.4–6 One of the major limitations to the widespread use of single-incision bariatric procedures has been the adequate retraction of the left lobe of the liver. Several techniques for replacing the liver retractor have been described in the literature.5–8 Others instead settled on a dual-incision procedure by using a liver retractor in the epigastrium.9 With regards to sleeve gastrectomy, one case series and a case report have been published.9,10 Specifically, Saber and colleagues9 reported on their first 7 cases of a transumbilical incision utilizing an additional incision for retraction of the left lobe of the liver. Later, Reavis et al10 reported their first case using a single paramedian incision. In this case, no liver retractor was required. Both reports concluded that the operation was safe and technically feasible.
The purpose of this report is to evaluate the safety and feasibility of our initial clinical experience with single-incision laparoscopic sleeve gastrectomy using a novel technique for retraction of the liver.
MATERIALS AND METHODS
We prospectively studied 7 consecutive patients who underwent single-incision laparoscopic sleeve gastrectomy between March and May 2009. All patients underwent a routine preoperative evaluation before being considered for sleeve gastrectomy and met the criteria for bariatric surgery according to the NIH.11
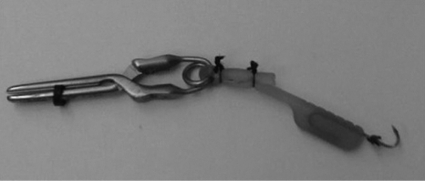
Two techniques of liver retraction were used for the procedure. In the first patient in the series, the Nathanson liver retractor was used. For the rest of the group, an internal liver retractor was utilized. The internal retractor was developed by attaching a Lone Star retractor hook (Lone Star Medical Products, Stafford, TX) to a laparoscopic bulldog clamp (Aesculap, Tuttlingen, Germany) (Figure 1). For this purpose, the back of the bulldog clamp is encircled with the Lone Star retractor, and then the retractor is tied to itself with 2 silk sutures. The bulldog was then introduced into the abdomen and attached to the pars flaccida. The elastic portion of the Lone Star retractor was used to retract the liver, while the hook was secured to the parietal peritoneum or the falciform ligament as needed. If additional retraction of the liver is necessary, a second laparoscopic bulldog could be used. All the cases were performed through a left paramedian incision (Figure 2).
Figure 1.
Internal retractor developed by securing a Lone Star retractor hook (Lone Star Medical Products, Stafford, TX) to a laparoscopic bulldog clamp (Aesculap, Tuttlingen, Germany).
Figure 2.
A 4-cm incision is made superior and left of the umbilicus.
In addition, the first 4 cases were carried out with a single incision, and the insertion of 3 separate trocars (single-incision laparoscopic surgery), as opposed to the last 3 cases in which a single port with 3 working channels was used (SILS port, Covidien, Norwalk, CT).
Operative Technique
The patient is placed on the operating table with a “beanbag.” The regular use of the beanbag permits securing the patient to the table when a steep reverse Trendelenburg is needed. Tape is used as an additional measure to support the patient in this position. Split-leg table attachments are used to allow the operating surgeon to stand between the patient's legs. Pneumatic compression stockings are routinely placed on both of the patient's legs. A Foley catheter is inserted, and an orogastric tube is placed at the beginning of the case to decompress the stomach.
A 4-cm incision is made superior and left of the umbilicus (Figure 2). This incision is carried down to the fascia, and superior and inferior flaps are formed to create an adequate working space. For the 3-trocar technique, a 5-mm optical trocar is inserted under direct vision in the external aspect of the space, and the abdomen is insufflated to 20mm Hg. A 15-mm trocar is inserted on the medial aspect of the incision, and a 5-mm low profile trocar is placed inferiorly in between the previous 2 trocars.
For the single-port technique, after the flaps are created, the anterior sheath of the rectus muscle is incised for about 3-cm, and the muscle fibers are spread in a vertical direction to expose the posterior rectal sheath. A 2-cm incision is carried down on the posterior rectal sheath and peritoneum. Next, the SILS port (SILS port, Covidien, Norwalk, CT) is introduced into the abdominal cavity. Then, two 5-mm and one 15-mm trocar are introduced into the working channels of the SILS port. A 5-mm, 30-degree laparoscope is used for the entire case. Standard extra long laparoscopic instruments were used in all cases.
The laparoscopic bulldog clamp (Aesculap, Tuttlingen, Germany) is inserted through the 15-mm trocar and attached to the pars flaccida with the bulldog applicator. The hook of the Lone Star retractor (Lone Star Medical Products, Stafford, TX) is secured to the parietal peritoneum or the falciform ligament as needed. This provides adequate visualization of the entire stomach, gastroesophageal junction, and the angle of His (Figure 3).
Figure 3.
Left lobe of the liver before and after placement of the internal liver retractor. The bulldog is introduced into the abdomen and attached to the pars flaccida, while the hook is secured to the parietal peritoneum or the falciform ligament as needed.
The operation begins with mobilization of the greater curve of the stomach. This is performed with the use of the Harmonic scalpel. A Raytec sponge is inserted and used for lateral retraction of the gastrosplenic omentum. Dissection of the greater curve and division of the short gastric vessels is performed all the way up to the angle of His. The dissection is stopped once the fundus is completely mobilized and the left crura are exposed. The dissection is then continued distally along the greater curvature, until the stomach is fully mobilized to a point approximately 2cm to 3cm proximal to the pylorus. Posterior adhesions to the pancreas are divided using medial retraction of the stomach.
At this point, the greater curvature of the stomach is folded medially to help guide the bougie placement. A 40 French bougie is inserted by the anesthesia team and guided along the lesser curvature towards the antrum of the stomach. The articulating linear cutting stapler with 60-mm, 4.8-mm stapler loads (endoGIA, Covidien, Norwalk, CT) with Bioabsorbable Staple Line Reinforcement (Gore Seamguard W.L. Gore and Associates, Flagstaff, AZ) is then used to begin division of the antrum. After the first 2 fires, 3.5-mm stapler loads (endoGIA, Covidien, Norwalk, CT) with staple-line reinforcement are then used to complete division of the stomach along the Bougie up to the angle of His.
Once the stomach is completely divided, the staple line and divided omentum are checked for hemostasis. The bougie is removed and an orogastric tube is inserted by anesthesia. The staple line is checked for leaks by occluding the prepyloric region with a bowel clamp and instilling 150mL of dilute methylene blue via the orogastric tube. The stomach is then placed in a 15-mm retrieval bag and removed from the abdomen at the end of the procedure. The abdomen is deflated and either trocars or the SILS port are removed. If the single-incision technique was used, the 15-mm trocar site is enlarged to allow the extraction of the surgical specimen. On the other hand, with the single-port technique, the fascial incision is enlarged to about 2cm to 2.5cm at the outset for satisfactory placement of the port. The fascial defect is closed with a running #1 Maxon suture.
Postoperative Protocol
No nasogastric tube is placed, and no drains are used. Both mechanical and pharmaceutical deep venous thrombosis prophylaxis is started before the induction of general anesthesia and continued throughout the postoperative period. On postoperative day one, the urinary catheter is removed, and patients are started on a clear liquid diet. If they tolerate the clear liquids, they are transitioned to oral pain medication and discharged on postoperative day 2 if there is no evidence of complications.
RESULTS
Eight patients underwent single-incision sleeve gastrectomy at the University of Illinois at Chicago. Patient demographics and operative characteristics are described in Table 1. For the first case (patient #1), an additional subxiphoid incision for placement of a Nathanson liver retractor was used. The following 7 consecutive cases were performed using the above-described technique with an internal liver retractor. No second retractor was needed in this series. All patients were female with a mean age of 34.1 years (range, 24 to 48). Mean BMI was 49kg/m2 (range, 39 to 64). Mean OR time was 103.8 minutes (range, 75 to 150). Blood loss was minimal in all cases. All 7 patients were discharged on postoperative day 2 after following the above-mentioned protocol and were doing well without any complications 3.1±0.7 months after surgery.
Table 1.
Demographic and Perioperative Data for 8 Patients Who Underwent Single-incision Laparoscopic Sleeve Gastrectomy
| Patient | Age | Sex | Height (in) | Weight (lbs) | BMI* | OR* Time | EBL* |
|---|---|---|---|---|---|---|---|
| 1 | 31 | F | 66 | 275 | 44 | 95 | 5 |
| 2 | 35 | F | 67 | 247 | 39 | 150 | 10 |
| 3 | 24 | F | 63 | 257 | 46 | 100 | 10 |
| 4 | 36 | F | 66 | 301 | 49 | 105 | 5 |
| 5 | 24 | F | 59 | 231 | 47 | 75 | 5 |
| 6 | 48 | F | 63 | 359 | 64 | 105 | 10 |
| 7 | 41 | F | 64 | 263 | 45 | 80 | 5 |
| 8 | 35 | F | 64 | 341 | 58 | 120 | 10 |
BMI=Body Max Index; OR=time Operating Room time; EBL=Estimated blood loss.
DISCUSSION
The laparoscopic sleeve gastrectomy was initially reported by Ren et al12 in 2000 as part of the duodenal switch for super-super morbidly obese patients and later described by Regan13 as a staged operation for morbid obesity in 2003. The rationale for sleeve gastrectomy was initially to lower the morbidity of this complex surgical procedure by offering a less challenging operation, decreasing operative time, and allowing patients to lose weight before proceeding with the second stage. Because of the excellent results in these patients, several studies14 have supported the use of the sleeve gastrectomy as a primary bariatric operation.
The main advantages of this operation are that it is not as technically challenging as gastric bypass or biliopancreatic diversion-duodenal switch (BPD-DS), thereby decreasing operative times and morbidity. Further refinements in surgical technique, specifically starting the sleeve closer to the pylorus and using a smaller caliber Bougie, have led to improved short-term excess weight loss.15
The initial operative technique of Moy et al16 used six 10-mm or 15-mm trocars. Nowadays, most surgeons use a 4- to 6-trocar technique, as well as an additional incision for a liver retractor. In general, this technique offers patients all the benefits of laparoscopic surgery; however, new developments in the field of minimally invasive surgery are aimed at further decreasing the invasiveness of laparoscopic procedures. Specifically, single-incision laparoscopic surgery (SILS) consists of only one incision in the patient's abdomen, and either the introduction of multiple trocars through that incision or one port with 3 or more working channels. Since its introduction, several reports1–3 have documented the safety and feasibility of these techniques. Unquestionably, SILS or single-port laparoscopy operations are more technically demanding, and for that reason, their use in bariatric surgery is in its early stages. The main reasons for this holdup are related to the complexity of these procedures in an already high-risk population. Consequently, it is not surprising that the initial reports in the literature are regarding the application of the SILS techniques for laparoscopic gastric banding.5,8 The next logical step in the evolution of minimally invasive bariatric surgery was the implementation of single-access surgery to the sleeve gastrectomy. In October 2008, Saber et al9 reported on a series of 7 patients undergoing a technique using a single peri-umbilical incision for laparoscopic sleeve gastrectomy. In this initial experience, the authors used one umbilical incision for placement of 3 laparoscopic trocars, and a second subxiphoid incision was made for placement of the Nathanson liver retractor. They reported that the technical challenges encountered with this technique may limit its widespread application and that this approach entails a unique learning curve. Later on, Reavis and colleagues10 reported a single case of sleeve gastrectomy through a 4-cm paramedian incision. These authors reiterate that a new set of laparoscopic skills are required for the successful completion of these procedures in addition to special laparoscopic instrumentation; nonetheless, they corroborate the feasibility of performing single-incision sleeve gastrectomy.
Several authors have outlined in the literature some of the limitations encountered during single-incision bariatric procedures, such as limited space for trocar placement, unwanted friction between trocars, and an enlarged left lobe of the liver. The latter has been of concern among experienced bariatric surgeons since all major bariatric procedures require adequate exposure of the upper stomach to enable the operation to be performed safely and with precision. As a consequence, to substitute the liver retractor several different techniques have been described in the literature.5–8 Texeira8 and Nguyen5 reported a similar technique for liver retraction, by introducing a 5-mm liver retractor through the same 4-cm incision where the trocars were placed to avoid any additional incision. The main drawback of this technique is the insertion of an additional instrument in an already crowded space. de la Torre et al7 instead placed a suture in the upper portion of the right crus and exteriorized the 2 ends of the suture with a suture passer at separate points. They reported that the 2 sutures could be positioned under the liver as needed to provide adequate retraction. Huang and colleagues6 described another interesting technique that consists of a suspension tape with 2 straight needles (Keith needle). The 2 needles penetrate the liver medially and externally and are then brought out under the left costal margin. Even though the above-described techniques are attractive, one of their main limitations is that the sutures can only be brought out under the left costal margin, thereby limiting the efficacy of the retractor. The first model of our internal retractor had an umbilical tape attached to the bulldog clamp. The umbilical tape was then exteriorized under the left costal margin. We found that this technique did not provide the required exposure of the upper stomach. As an alternative, the current version allows the hook needle of the Lone Star to be anchored to the abdominal wall as necessary.
To our knowledge, no complete intracorporeal device for retraction of the liver has been described. Advantages of the internal retractor are mainly eliminating the need for either a separate skin incision or the introduction of the retractor in an already cluttered space. In addition, the technique is reproducible, the bulldog clamp is reusable, and the bulldog applicator ensures ease of intraoperative repositioning and maneuverability. In patients with an enlarged left lobe of the liver, a second retractor can be used to enhance exposure. Additionally, we have utilized this internal retractor for procedures like laparoscopic adjustable gastric banding and laparoscopic cholecystectomies with promising results. Some of the drawbacks of this technique include the need for a 10-mm trocar for the introduction of the bulldog clamp. In their current version, bulldog clamps are atraumatic; therefore, excessive retraction may result in slipping of the clamp from its position. Our limited experience with single-incision sleeve gastrectomy is comparable to that reported in the literature. Nonetheless, a few technical considerations are worth mentioning, because they have made the surgery viable for us.
Since the first case, we decided not to use the umbilicus for our sleeve gastrectomies. Compared with our approach, theoretical advantages of the transumbilical route are better cosmesis, reduction in postoperative pain, and minimization of instrument torching.9 Our rationale was to simplify the procedure and enhance exposure of the gastroesophageal junction. It is well known that in morbidly obese patients the distance between the umbilical area and the gastroesophageal junction can be increased, therefore limiting the reach of the current laparoscopic instrumentation (Figure 2). Nonetheless, we acknowledge that with adequate instrumentation the umbilical route is promising.
Secondly, the use of a flexible stapler with staple-line reinforcement also facilitated the operation. The articulation of the stapler facilitated the transection of the stomach in spite of the limited lateral retraction of the single-incision approach, taking into account that for all our procedures we used straight laparoscopic instruments. Even though we did not find articulated instruments necessary for this particular operation, we recognize that they may facilitate certain procedures. Thirdly, after the first 5 cases, we decided to transition our technique to single-port laparoscopy, because it was necessary to enlarge the 15-mm trocar site to about 2cm to 2.5cm to remove the specimen from the abdomen. Consequently, to introduce the port, a 2-cm fascial incision was carried out at the beginning of the case. This latter change did not seem to compromise our standard surgical procedure and expedited the surgical specimen extraction.
In summary, as stated previously, single-incision laparoscopy has a particular learning curve, because there is a very limited working space that decreases the range of motion of the instrumentation. Nonetheless, because laparoscopic sleeve gastrectomy is less technically demanding, it is potentially a suitable procedure for single-incision surgery without changing the existing principles of the operation.
CONCLUSION
Single-incision sleeve gastrectomy is a feasible alternative to standard laparoscopic sleeve gastrectomy. Adequate exposure, with a simple but effective method of liver retraction, enables the operation to be performed safely. We are satisfied with this initial experience, and we plan to continue using this approach whenever possible. As the technology continues to evolve, single-incision surgery will become a very attractive alternative for the performance of other bariatric surgical procedures.
Footnotes
Disclosure Statement and Conflict of Interest: Nothing to disclose.
Contributor Information
Carlos A. Galvani, Minimally Invasive Surgery, Department of Surgery, University of Arizona, Tucson, Arizona, USA..
Mark Choh, Division of General, Minimally Invasive, and Robotic Surgery, University of Illinois at Chicago, Chicago, Illinois, USA..
Maria V. Gorodner, Division of General, Minimally Invasive, and Robotic Surgery, University of Illinois at Chicago, Chicago, Illinois, USA..
References:
- 1. Remzi FH, Kirat HT, Kaouk JH, Geisler DP. Single-port laparoscopy in colorectal surgery. Colorectal Dis. 2008;10:823–826 [DOI] [PubMed] [Google Scholar]
- 2. Aron M, Canes D, Desai MM, Haber GP, Kaouk JH, Gill IS. Transumbilical single-port laparoscopic partial nephrectomy. BJU Int. 2009;103:516–521 [DOI] [PubMed] [Google Scholar]
- 3. Hodgett SE, Hernandez JM, Morton CA, Ross SB, Albrink M, Rosemurgy AS. Laparoendoscopic single site (LESS) cholecystectomy. J Gastrointest Surg. 2009;13:188–192 [DOI] [PubMed] [Google Scholar]
- 4. Oltmann SC, Rivas H, Varela E, Goova MT, Scott DJ. Single-incision laparoscopic surgery: case report of SILS adjustable gastric banding. Surg Obes Relat Dis. 2009;5:362–364 [DOI] [PubMed] [Google Scholar]
- 5. Nguyen NT, Hinojosa MW, Smith BR, Reavis KM. Single laparoscopic incision transabdominal (SLIT) surgery-adjustable gastric banding: a novel minimally invasive surgical approach. Obes Surg. 2008;18:1628–1631 [DOI] [PubMed] [Google Scholar]
- 6. Huang CK, Houng JY, Chiang CJ, Chen YS, Lee PH. Single incision transumbilical laparoscopic Roux-en-Y gastric bypass: a first case report. Obes Surg. 2009;19(12):1711–1715 [DOI] [PubMed] [Google Scholar]
- 7. de la Torre RA, Satgunam S, Morales MP, Dwyer CL, Scott JS. Transumbilical single-port laparoscopic adjustable gastric band placement with liver suture retractor. Obes Surg. 2009;19(12):1707–1710 [DOI] [PubMed] [Google Scholar]
- 8. Teixeira J, McGill K, Koshy N, McGinty J, Todd G. Laparoscopic single-site surgery for placement of adjustable gastric band-a series of 22 cases. Surg Obes Relat Dis. 2009. April 16 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 9. Saber AA, Elgamal MH, Itawi EA, Rao AJ. Single incision laparoscopic sleeve gastrectomy (SILS): a novel technique. Obes Surg. 2008;18:1338–1342 [DOI] [PubMed] [Google Scholar]
- 10. Reavis KM, Hinojosa MW, Smith BR, Nguyen NT. Single-laparoscopic incision transabdominal surgery sleeve gastrectomy. Obes Surg. 2008;18:1492–1494 [DOI] [PubMed] [Google Scholar]
- 11. Gastrointestinal surgery for severe obesity. Proceedings of a National Institutes of Health Consensus Development Conference March 25–27, 1991, Bethesda, MD Am J Clin Nutr. 1992;55:487S–619S [DOI] [PubMed] [Google Scholar]
- 12. Ren CJ, Patterson E, Gagner M. Early results of laparoscopic biliopancreatic diversion with duodenal switch: a case series of 40 consecutive patients. Obes Surg. 2000;10:514–523, discussion 524 [DOI] [PubMed] [Google Scholar]
- 13. Regan JP, Inabnet WB, Gagner M, Pomp A. Early experience with two-stage laparoscopic Roux-en-Y gastric bypass as an alternative in the super-super obese patient. Obes Surg. 2003;13:861–864 [DOI] [PubMed] [Google Scholar]
- 14. Lee CM, Cirangle PT, Jossart GH. Vertical gastrectomy for morbid obesity in 216 patients: report of two-year results. Surg Endosc. 2007;21:1810–1816 [DOI] [PubMed] [Google Scholar]
- 15. Deitel M, Crosby RD, Gagner M. The First International Consensus Summit for Sleeve Gastrectomy (SG), New York City, October 25–27, 2007. Obes Surg. 2008;18:487–496 [DOI] [PubMed] [Google Scholar]
- 16. Moy J, Pomp A, Dakin G, Parikh M, Gagner M. Laparoscopic sleeve gastrectomy for morbid obesity. Am J Surg. 2008;196:e56–e59 [DOI] [PubMed] [Google Scholar]