Abstract
Discovered in the late-1970s, the pioneering drug ivermectin, a dihydro derivative of avermectin—originating solely from a single microorganism isolated at the Kitasato Intitute, Tokyo, Japan from Japanese soil—has had an immeasurably beneficial impact in improving the lives and welfare of billions of people throughout the world. Originally introduced as a veterinary drug, it kills a wide range of internal and external parasites in commercial livestock and companion animals. It was quickly discovered to be ideal in combating two of the world’s most devastating and disfiguring diseases which have plagued the world’s poor throughout the tropics for centuries. It is now being used free-of-charge as the sole tool in campaigns to eliminate both diseases globally. It has also been used to successfully overcome several other human diseases and new uses for it are continually being found. This paper looks in depth at the events surrounding ivermectin’s passage from being a huge success in Animal Health into its widespread use in humans, a development which has led many to describe it as a “wonder” drug.
Keywords: avermectin, ivermectin, mode of action, onchocerciasis, lymphatic filariasis, drug resistance
Introduction
There are few drugs that can seriously lay claim to the title of ‘Wonder drug’, penicillin and aspirin being two that have perhaps had greatest beneficial impact on the health and wellbeing of Mankind. But ivermectin can also be considered alongside those worthy contenders, based on its versatility, safety and the beneficial impact that it has had, and continues to have, worldwide—especially on hundreds of millions of the world’s poorest people. Several extensive reports, including reviews authored by us, have been published detailing the events behind the discovery, development and commercialization of the avermectins and ivermectin (22,23-dihydroavermectin B), as well as the donation of ivermectin and its use in combating Onchocerciasis and lymphatic filariasis.1–6) However, none have concentrated in detail on the interacting sequence of events involved in the passage of the drug into human use.
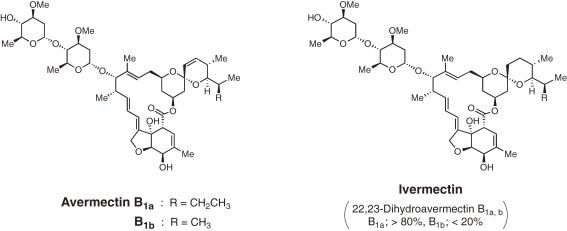
When it first appeared in the late-1970s, ivermectin, a derivative of avermectin (Fig. 1 ) was a truly revolutionary drug, unprecedented in many ways. It was the world’s first endectocide, forerunner of a completely new class of antiparasitic agents, potently active against a wide range of internal and external nematodes and arthropods. In the early-1970s, a novel international Public Sector–Private Sector partnership was initiated by one of us (Ōmura, then head of the Antibiotics Research Group at Tokyo’s Kitasato Institute), forming a collaboration with the US-based Merck, Sharp and Dohme (MSD) pharmaceutical company. Under the terms of the research agreement, researchers at the Kitasato Institute isolated organisms from soil samples and carried out preliminary in vitro evaluation of their bioactivity. Promising bioactive samples were then sent to the MSD laboratories for further in vivo testing where a potent and promising novel bioactivity was found, subsequently identified as being caused by a new compound, which was named ‘avermectin’.7) Despite decades of searching around the world, the Japanese microorganism remains the only source of avermectin ever found.1) Originating from a single Japanese soil sample and the outcome of the innovative, international collaborative research partnership to find new antiparasitics, the extremely safe and more effective avermectin derivative, ivermectin, was initially introduced as a commercial product for Animal Health in 1981. It is effective against a wide range of parasites, including gastrointestinal roundworms, lungworms, mites, lice and hornflies.7–12) Ivermectin is also highly effective against ticks, for example, the ixodid tick Rhipicephalus (Boophilus) microplus, one of the most important cattle parasites in the tropics and subtropics, which causes enormous economic damage. Indicative of the impact, in Brazil, where some 80% of the bovine herd is infested, losses total about $2 billion annually.13) Today, ivermectin is being used to treat billions of livestock and pets around the world, helping to boost production of food and leather products, as well as keep billions of companion animals, particularly dogs and horses, healthy. The ‘Blockbuster’ drug in the Animal Health sector, meaning that it achieved annual sales in excess of over US$1 billion, maintained that status for over 20 years. It is so useful and adaptable that it is also being used off-label, sometimes, illegally, for example to treat fish lice in the aquaculture industry, where it can have a negative impact on non-target organisms. It also has extensive uses in agriculture.2)
Figure 1.
Molecular diagrams of avermectin and the di-hydro derivative, ivermectin.
Ivermectin proved to be even more of a ‘Wonder drug’ in human health, improving the nutrition, general health and wellbeing of billions of people worldwide ever since it was first used to treat Onchocerciasis in humans in 1988. It proved ideal in many ways, being highly effective and broad-spectrum, safe, well tolerated and could be easily administered (a single, annual oral dose). It is used to treat a variety of internal nematode infections, including Onchocerciasis, Strongyloidiasis, Ascariasis, cutaneous larva migrans, filariases, Gnathostomiasis and Trichuriasis, as well as for oral treatment of ectoparasitic infections, such as Pediculosis (lice infestation) and scabies (mite infestation).14) Ivermectin is the essential mainstay of two global disease elimination campaigns that should soon rid the world of two of its most disfiguring and devastating diseases, Onchocerciasis and Lymphatic filariasis, which blight the lives of billions of the poor and disadvantaged throughout the tropics. It is likely that, throughout the next decade, well over 200 million people will be taking the drug annually or semi-annually, via innovative globally-coordinated Mass Drug Administration (MDA) programmes. Indeed, the discovery, development and deployment of ivermectin, produced by an unprecedented partnership between the Private Sector pharmaceutical multinational Merck & Co. Inc., and the Public Sector Kitasato Institute in Tokyo, aided by an extraordinary coalition of multidisciplinary international partners and disease-affected communities, has been recognized by many experts and observers as one of the greatest medical accomplishments of the 20th century.15) In referring to the international efforts to tackle Onchocerciasis in which ivermectin is now the sole control tool, the UNESCO World Science Report concluded, “the progress that has been made in combating the disease represents one of the most triumphant public health campaigns ever waged in the developing world”.16)
Onchocerciasis
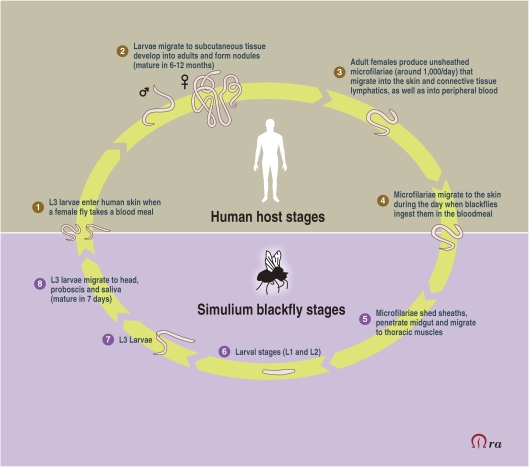
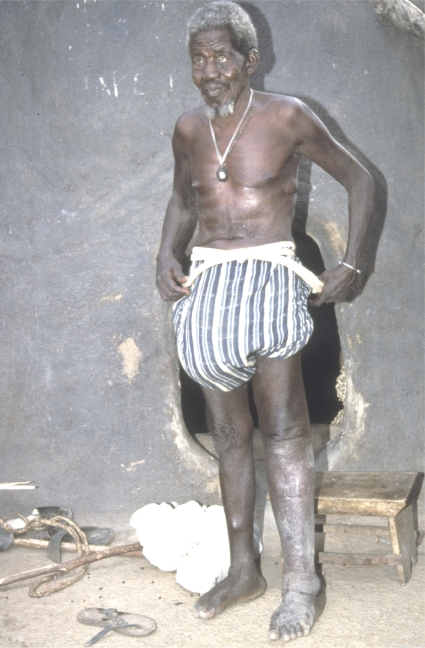
The origins of ivermectin as a human drug are inextricably linked with Onchocerciasis (or River Blindness), a chronic human filarial disease caused by infection with Onchocerca volvulus worms. The parasites are transmitted via the bite of infected blackflies of the genus Simulium, which breed in highly-oxygenated, fast-flowing rivers and watercourses. In the human body, immature larval forms of the parasite create nodules in subcutaneous tissue, where they mature into adult worms. After mating, female worms can release up to 1000 microfilariae a day for some 10–14 years. These move through the body, and when they die they cause a variety of conditions, including skin rashes, lesions, intense itching, oedema and skin depigmentation (Fig. 2 ). Microfilariae also invade the eye, causing visual impairment and loss of vision, onchocerciasis being the second leading cause of blindness caused by an infectious disease.17) The disease causes visual damage for some 1–2 million people, around half of who will become blind.18)
Figure 2.
Mali: an old man, blinded by onchocerciasis, with leopard skin on his legs and nodules on his abdomen. Credit line: WHO/TDR/Crump.
In the early-1970s, the disease was endemic in 34 countries: 27 in Africa; 6 in the Americas; and 1 in the Arabian Peninsula. The World Health Organization (WHO) later estimated that 17.7 million people were infected worldwide, of whom some 270,000 were blind, and another 500,000 severely visually disabled. The burden of onchocerciasis was particularly extreme in the hyper-endemic belt across sub-Saharan Africa. Communities in these areas exhibited high rates of visual disability caused by Onchocerciasis, up to 40% in some areas, which caused immeasurable negative impact on individual and community health, reducing economic capacity and productivity, and leading to the abandonment of fertile agricultural lands.19)
By 1973, Onchocerciasis had been recognised by the then head of the World Bank, Robert McNamara, as a major disease of massive health and socioeconomic importance and one in dire need of combating in West Africa, and he became the key agent for change. In 1974, following international recognition of the dramatic consequences of disabling and disfiguring Onchocerciasis in Africa, four United Nations agencies, including the World Bank, launched the Onchocerciasis Control Programme in West Africa (OCP). The programme covered 1.2 million km2, protecting 30 million people in 11 countries from River Blindness.
Drug donation
For over a decade, OCP operations were exclusively based on the spraying of insecticides by helicopters and aircraft over the breeding sites of vector blackflies in order to kill their larvae. Following the registration of ivermectin (produced under the brand name Mectizan®) for human use in 1987, in a hitherto unprecedented move and with unheralded commitment, Mectizan® was donated by the manufacturing company, Merck & Co. Inc., to treat onchocerciasis in all endemic countries for as long as it was needed. The resultant drug donation programme was the first, largest, longest running and most successful of all—and proved a model for all others that have followed. Ivermectin began to be distributed in 1988, with operations being organized through the independent Mectizan Donation Program (MDP) established and funded by Merck. Thereafter, OCP control operations changed from exclusive vector control to larviciding combined with ivermectin treatment or, in some areas, to ivermectin treatment alone. Ivermectin swiftly became the drug of choice for the treatment of Onchocerciasis due to its unique and potent microfilaricidal effects, the absence of severe side effects and its excellent safety. It is now the sole tool being used in disease elimination campaigns in the 16 other African countries where the disease exists, orchestrated by the African Programme for Onchocerciasis Control (APOC), which commenced operations in 1996. A single annual dose of 150 µg/kg of ivermectin, given orally, can reduce the level of skin microfilariae to zero and, by interfering with worm embryogenesis, can delay the build-up of new microfilariae for a period of up to two years. OCP was closed in December 2002 after virtually stopping disease transmission in all target nations except Sierra Leone where operations were hampered by civil war.
The process, from the discovery of ivermectin’s activity against onchocercal microfilariae to the successful distribution programme from 1988 onward, was neither an easy or direct path. Success was achieved through groundbreaking and innovative partnerships. The journey was a complex undertaking, incorporating scientific uncertainty, conflicting views, ambiguity, frustration, individual innovation and unexpected twists and turns. The actual discovery of ivermectin was an international team effort involving a unique, pioneering Public Sector/Private Sector partnership and the commitment and vision of several key individuals. Ivermectin’s development into a drug for human use also involved a number of organizational, individual and pharmacological variables—together with a large slice of luck, educated insight and personal commitment.
Development of ivermectin for human use
In the mid-1970s, the global community mobilized itself to address the major problems of neglected tropical diseases. Following the setting up of the OCP in 1974, the UN-based Special Programme for Research & Training in Tropical Diseases (TDR) was established in 1975.20) Onchocerciasis, one of two filarial infections among TDR’s eight target diseases, was at that time a major public health problem affecting 20–40 million people in endemic areas. At exactly this time, a specialized novel anthelmintic mouse screening model in Merck’s research laboratories was identifying the avermectins in the microbial sample sent by the Kitasato Institute, of which ivermectin would become the most successful derivative.
At the time, there were no safe and acceptable drugs available to treat Onchocerciasis, which had plagued Africa for centuries, effectively leading to the creation of the OCP and its vector control focus. TDR quickly found that, despite many pharmaceutical companies, such as Bayer, Hoffman-LaRoche, CIBA-Geigy and Rhône-Poulenc, carrying out routing screening for filaricidal compounds, no companies were interested in developing suitable anti-Onchocerca drugs, as there was no apparent commercial market. Worse still, Onchocerca species would not develop to maturity in any rodents, making it impossible to screen compounds in an animal model against the target organism.21) It had been shown that O. volvulus could infect chimpanzees (Pan troglodites) but it was deemed unethical to use these animals for the necessary large-scale research, even though some testing of compounds was undertaken.22,23) Consequently, the OCP opted to devote operations to aerial larviciding via helicopters and small fixed-wing planes. It was a very ‘vertical’ programme, mainly coordinated through the World Bank and other UN agencies, with multimillion dollar contracts given to a US-based helicopter company and to an American chemical company for the insecticides.
Meanwhile, with respect to research needs, TDR had identified six specific areas that required special attention, with the discovery of effective and safe chemotherapeutic agents considered to be the highest priority. In 1975, only two drugs were available for the treatment of onchocerciasis: diethylcarbamazine (DEC) and suramin. The use of both was highly unsatisfactory. DEC, which was known to kill microfilariae, caused violent and even dangerous hypersensitivity reactions in the human host. Suramin, developed 50 years previously for treatment of Sleeping Sickness, was the only drug considered for killing adult worms but was highly toxic, often causing severe and occasionally fatal reactions. Moreover, parasitological cure of patients using DEC and suramin required lengthy and expensive treatment given under medical supervision. Therefore, the TDR Scientific Working Group (SWG), composed of leading independent scientists in the field from around the globe, including industry, decided that the priority was a new and non-toxic macrofilaricide (to kill adult worms), a macrofilaricide being determined to be substantially preferable to a microfilaricide (which would target immature worms).24)
At the first meeting of TDR’s Filariasis Scientific Steering Committee in 1976, it was reported that Programme staff had visited 16 major pharmaceutical companies but had found none actively working on onchocerciasis. Nor was there any validated model for screening. The Committee agreed that the high cost of maintaining screening facilities for drugs against tropical diseases was a significant deterrent to industrial involvement.25) TDR acted to rectify this situation and thereby engage industry in the search for a new drug. Unfortunately, O. volvulus parasites can only develop fully in humans and a few primates. Fortunately, the closest relative to the human parasite is O. ochengi, found in cattle, which is restricted to Africa and which is also transmitted by the same vector. The O. ochengi cattle model thus facilitated experimental studies, in the field and laboratory-based, that were not possible in humans, leading to detailed knowledge of the parasite’s life cycle (Fig. 3 ). From 1977 on, TDR provided technical and financial support to establish a comprehensive screening system for Onchocercal filaricides. The Programme identified five academic and private research institutions with technical capacities and facilities for primary and secondary screens: the University of Georgia (USA), University of Giessen (Germany), the Wellcome Foundation (UK), the London School of Hygiene and Tropical Medicine (UK) and the University of Tokyo (Japan). TDR provided some US$2.25 million to these Public Sector institutions for primary and secondary screening of compounds, while pressing pharmaceutical companies to donate compounds for testing with the promise of full confidentiality. Additionally, TDR established a unique tertiary screen, using cattle, for compounds showing positive results in any secondary screen. Based at the James Cook University of North Queensland, Australia, the screen, costing almost US$435,000, was the best predictor of what a compound would do in humans. Some 10,000 compounds, many supplied by leading pharmaceutical companies as coded samples, passed through the screening network, including several from Merck.26)
Figure 3.
Life cycle of Onchocerca volvulus.
In reality, ivermectin’s role in human medicine effectively began in April 1978 inside the Merck company, several years before the drug emerged on the Animal Health market. The highly potent bioactivity of a fermentation broth of an organism isolated by the Kitasato Institute in Tokyo, which had been sent to Merck’s research laboratories in 1974, was first identified in 1975. The active compounds were identified by the international multidisciplinary collaborative team as the avermectins, with the subsequently-refined ivermectin derivative being designated the optimal compound for development. Merck scientists, under the direction of Dr William Campbell, found that the drug was active against a wide range of parasites of livestock and companion animals.10) The informed foresight of a Merck researcher, Ms. L.S. Blair, resulted in the discovery that the drug was effective against skin-dwelling microfilariae of Onchocerca cervicalis in horses. These did not actually cause clinical disease and so the finding was of little commercial significance. However, O. cervicalis belongs to the same genus as O. volvulus, and upon reading the experimental reports, Dr Campbell surmised that there might be some merit in testing for impact against the latter. In July 1978, he sent ivermectin (as a coded sample), together with the results of the horse trial, to the TDR-supported tertiary cattle screen in Australia. The results, obtained in November 1978, showed that ivermectin was “highly effective in preventing patent infections with both O. gibsoni and O. gutturosa”. This reinforced Campbell’s growing belief that ivermectin would be effective against human onchocerciasis. Consequently, in December, he proposed to the Merck Laboratories’ Research Management Council that “an avermectin could become the first means of preventing the blindness associated with onchocerciasis” and that “discussions be held with representatives of WHO to determine the most appropriate approach to the problem—from the medical, political and commercial points of view”.27,28) Senior management approved the lead taken by Campbell and research funding to investigate the potential use of ivermectin in humans was approved by Dr Roy Vagelos, then President of the research laboratories.
TDR reactions to the initial data about ivermectin were rather muted, especially as it was searching for a macrofilaricide and ivermectin appeared to have little impact on adult worms. In late-1979, a TDR official visited Merck and, although the meeting resulted in TDR’s technical contribution to Merck’s ivermectin research, there was no ensuing discussion about collaboration to develop ivermectin for use in human Onchocerciasis.
Fortunately for all, in January 1980, Merck decided to proceed independently to Phase I (safety) trials. Clinical trials of ivermectin began in 1981, with a Phase I trial in 32 patients in Senegal followed by another trial in Paris among 20 West African immigrants. These trials were independently organized and funded by Merck, with a staff member, Dr Mohamed Aziz, previously of WHO, being the caring and committed driving force behind them. Dr Aziz started the study in Senegal with safety uppermost in his mind. It began with a very low dose of 5 µg/kg and found that a single dose of ivermectin, 30 µg/kg, substantially decreased the number of skin microfilariae. It also established that the effect lasted for at least 6 months, with no serious adverse events being observed. The subsequent Paris study confirmed these results and showed that doses up to 200 µg/kg were well tolerated.29,30)
When Merck officials visited TDR and OCP in 1982 to present the results from the Phase I trials, each side recognised the immense potential and collaboration in earnest began.
Evidence suggests that collaboration between these major partners commenced in a complex environment of mutual wariness, suspicion and shared hope that ivermectin would indeed prove to be an effective treatment for Onchocerciasis. The situation was compounded by the fact that Merck saw ivermectin as a potentially commercial product to be used for individual patient treatment, and moved forward constantly seeking an income return on its investment. In contrast, TDR, together with OCP, saw the drug as a new community-level tool that could possibly interrupt parasite transmission and thereby help reduce the prevalence of the disease in endemic communities. TDR and OCP consequently regarded community-based trials under field conditions as an essential step towards mass-treatment programmes, as opposed to the individual treatment in hospitals favoured by the commercial partner. The continual negotiation with respect to the cost of the drug eventually resulted in a commitment from Merck in July 1985 to supply it in sufficient quantities and at the lowest possible price consistent with the interests of the company, later confirming that it would be made available to “… governments and patients at no cost to them for the treatment of Onchocerciasis”.31)
With respect to official registration of ivermectin for human use, Merck, focussing on the single-patient approach, pressed ahead on its own and submitted an application to the French health authorities in 1987 based solely on the studies of the first 1,206 onchocerciasis patients, expecting to receive approval later that year, which it subsequently did.24,32) In its submission, Merck indicated a price of $3 per tablet, meaning that a treatment dose would cost $6, well beyond an affordable amount for those most in need.
Prior to registration, the involvement of TDR and OCP increased substantially, as they organised field trials, including extremely expensive, large-scale trials of the effectiveness of ivermectin in community treatment programmes, and campaigned tirelessly to get the cost of treatment reduced to an acceptable level. During the trials to test the efficacy of the drug in field settings (Phase II trials starting in 1983), Merck continued to fund much of the work, with additional financial support from OCP and TDR. Fortunately, TDR’s existing international network facilitated Merck’s ability to develop workable relationships with researchers and institutions to conduct activities in Africa and South America. TDR was also able to influence the design of study protocols, and support applied research on onchocerciasis treatment at one of its specialized centres, the Onchocerciasis Chemotherapy Research Centre (OCRC) in Tamale, Ghana, where Dr Kwable Awadzi had devised a method to quantify clinical reactions to microfilaricides using a scoring system of commonly observed reactions.33) This made it possible to compare the degrees of systemic reactions for all compounds using a common metric, eventually confirming the promise of ivermectin as a safe and highly effective microfilaricide.
Thirteen community-level (Phase IV) trials were conducted between 1987–1989, with over 120,000 individual doses of ivermectin administered. Of the 13 community trials, TDR funded five in Liberia, Cameroon, Malawi, Guatemala and Nigeria, and spent US$2.35 million in total. Over the period, TDR spent between 25–35% of its total annual budget for all filariasis work on ivermectin. OCP funded the eight other studies in Ghana, Mali, Togo, Benin, Ivory Coast, Guinea, Burkina Faso and Senegal. As a private sector company, Merck’s financial contributions to the development of ivermectin for human use, although substantial, remain unknown.
Advantages of ivermectin for treating Onchocerciasis
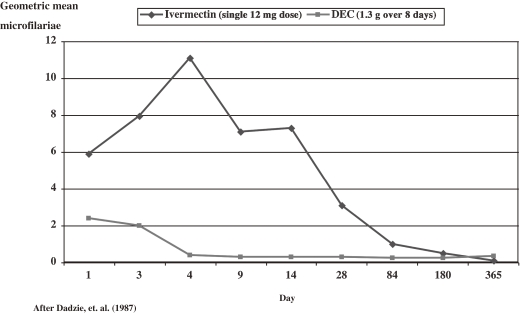
Ivermectin proved to be virtually purpose-built to combat Onchocerciasis, which has two main manifestations, dermal damage resulting from microfilariae in the skin and ocular damage arising from microfilariae in the eye. Until the advent of ivermectin, despite its drawbacks, DEC was the drug of choice traditionally used to treat patients with onchocercal infection. DEC acts quickly to eliminate microfilariae from the anterior chamber of the eye and keeps the eye clear for a year or more. However, the rapidity of clearance often causes ocular damage as a result of an exaggerated inflammatory reaction. Conversely, ivermectin proved to slightly increase microfilariae in the eye upon treatment, followed by a gradual reduction, reaching to near zero, similar to DEC, within six months (Fig. 4 ). Most significantly, little or no resultant ocular damage occurs. Unlike DEC, it is believed that the large molecular size of ivemectin, a macrocylic lactone, prevents it from crossing the blood/aqueous humour barrier, stopping it entering the anterior chamber and exerting an effect directly on microfilariae.34) This makes ivermectin an ideal treatment for patients with ocular involvement.
Figure 4.
Effect of ivermectin and diethylcarbamazine (DEC) on microfilariae in the Anterior Chamber of the eye.
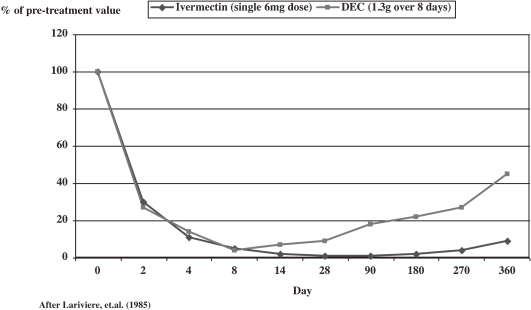
Similarly, evaluation of the impact of DEC and ivermectin on dermal microfilariae, confirmed that both caused almost complete clearance within two days after treatment, reducing the load to virtually zero within eight days. However, although both drugs produce long-term suppression of the reappearance of microfilariae, ivermectin is superior, virtually eliminating all microfilariae and maintaining that status for some 90 days, whereas the effect of DEC wanes after little more than a week (Fig. 5 ). Thus, ivermectin is also an ideal treatment for dermal involvement.35) In addition to being perfectly tailor-made for Onchocerciasis, ivermectin has progressed to become a ‘wonder drug’ for other diseases too.
Figure 5.
Effect of ivermectin and diethylcarbamazine (DEC) on microfilariae in the skin.
Effectiveness against other filarial diseases
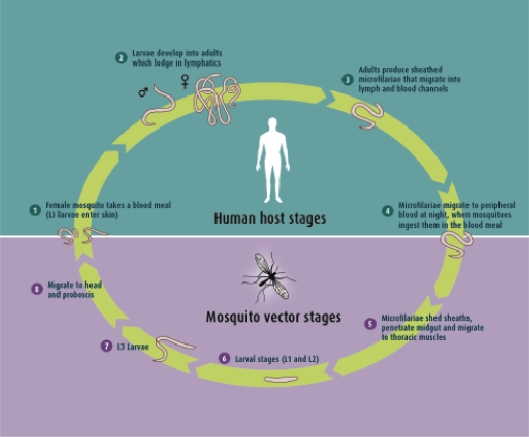
Lymphatic Filariasis, also known as Elephantiasis, is another devastating, highly debilitating disease that threatens over 1 billion people in more than 80 countries. Over 120 million people are infected, 40 million of whom are seriously incapacitated and disfigured. The disease results from infection with filarial worms, Wuchereria bancrofti, Brugia malayi or B. timori. The parasites are transmitted to humans through the bite of an infected mosquito and develop into adult worms in the lymphatic vessels, causing severe damage and swelling (lymphoedema) (Fig. 6 ). Adult worms are responsible for the major disease manifestations, the most outwardly visible forms being painful, disfiguring swelling of the legs and genital organs (Fig. 7 ). The psychological and social stigma associated with the disease are immense, as are the economic and productivity losses it causes.
Figure 6.
Life cycle of Wuchereria bancrofti.
Figure 7.
Ghana: an old man co-infected with onchocerciasis and lymphatic filariasis. He is partially sighted, with a worm nodule on his right leg and leopard skin on his left leg. He also displays elephantiasis of the left leg and has a large hydrocele. Credit line: WHO/TDR/Crump.
With respect to the use of ivermectin for Lymphatic filariasis, again Merck took the initial lead, with TDR being involved in organising, expanding and broadening the research and clinical trials. In the mid-1980s, well before ivermectin was approved for human use to treat onchocerciasis, Merck were also undertaking trials of ivermectin to measure its impact against lymphatic filariasis and to find optimal treatment dosages.36) Meanwhile, TDR was carrying out multi-centre field trials in Brazil, China, Haiti, India, Indonesia, Malaysia, Papua New Guinea, Sri Lanka and Tahiti to evaluate ivermectin, the existing treatment drug, DEC, and combinations of the two. The results showed that single-dose ivermectin and single-dose DEC worked as well as each other. The combination, even at low dose, proved even more effective, decreasing microfilarial density by 99% after one year and 96% after two years.20,37–39) DEC was also found to be effective in killing adult parasites.
Despite these findings, ivermectin remained unregistered for treatment of lymphatic filariasis for several years. Indeed it was not until 1998 that registration was forthcoming from the French authorities. Several years earlier another drug, albendazole, produced by SmithKlineBeecham (now GlaxoSmithKline – GSK) had also been shown to be effective in killing both immature and adult worms. Indeed, field trials had confirmed that once-yearly combinations of albendazole plus DEC or ivermectin were 99% effective in ridding the blood of microfilariae for at least a year after treatment. The primary goal of treating affected communities thus became elimination of microfilariae from the blood of infected individuals so that transmission of infection is interrupted. This opened up the prospect of actually eliminating the disease, something that was made eminently possible thanks to GSK agreeing to donate albendazole. In 1997, following advances in both diagnosis and treatment, WHO classified lymphatic filariasis as one of six “eradicable” or “potentially eradicable” infectious diseases and requested Member States to initiate steps to eliminate lymphatic filariasis as a public health problem.40) In late-1998, following registration of the drug for lymphatic filariasis, Merck extended its ivermectin donation programme to cover lymphatic filariasis in areas where it co-existed with Onchocerciasis. Subsequently, in 1999/2000, the WHO launched the Global Programme to Eliminate Lymphatic Filariasis (GPELF).
In summary, the vision of ivermectin as a potential drug for human onchocerciasis emanated from Merck’s research team. TDR facilitated the realisation of that vision though its initial recognition of the lack of an effective tool to identify potential anti-Onchocerca filaricides, its proactive engagement with pharmaceutical companies; its creation of and funding for animal model and screening systems; and by mobilizing and engaging its international network of researchers and institutions. TDR’s unique position as an international body with a mandate to coordinate research work and provide funds in tropical diseases facilitated and made possible the passage of Merck’s compound through to field use in Africa and elsewhere, allowing the foresight of Merck scientists and the enormous resources devoted by the company to result in immeasurable public health benefits.
Mode of action
Initially, researchers working on the development of ivermectin believed that it blocked neurotransmitters, acting on GABA-gated Cl− channels, exhibiting potent disruption at GABA receptors in invertebrates and mammals. GABA is recognised as the primary inhibitory neurotransmitter in the somatic neuromuscular system of nematodes. Subsequently, they discovered that it was in fact glutamate-gated Cl− channels (GUCl−) that were the target of ivermectin and related drugs. This discovery opened up a completely new spectrum of possibilities, as these channels, although playing fundamental roles in nematodes and insects, are not accessible in vertebrates.41–43) Ivermectin, while paralyzing body-wall and pharyngeal muscle in nematodes has no such impact in mammals, as it cannot cross the blood-brain barrier into the mammalian Central Nervous System, where GABA receptors are located. For a long time, it was believed that ivermectin was contra-indicated in children under the age of five or who weighed less than 5 kg, as there was a fear of neurotoxicity, the drug possibly being able to cross the as yet not fully developed blood/brain barrier. However, evidence has emerged that is probably not the case.44)
In the human body, ivermectin exerts a peculiar and singular effect that remains poorly understood. The immune response to filarial infection is complex, involving Th2-type systems which counter infective L3 larvae and microfilariae, whereas a combination of Th1 and Th2 pathways are involved in resisting adult worms. It is believed that female adult worms are able to manipulate the immunoregulatory environment, possibly via interleukin 10 (IL-10) levels, to ensure the survival of their microfilarial offspring.45) Ivermectin treatment of Onchocercal filarial infection causes the disappearance of microfilariae from the peripheral skin lymphatics. It does so relatively quickly and with long-lasting effect, while also inhibiting adult female worms from releasing additional microfilariae.46) Dermal microfilarial loads are generally reduced by 78% within two days, and by some 98% two weeks after treatment. They remain at extremely low levels for about 12 months, with 70% of female worms slowly resuming production of microfilaria 3–4 months after treatment, but at an irreversibly curtailed 35% of original production.47) Regular treatment consequently decreases incidence of infection, interrupts transmission and reduces morbidity and disability. However, the actual mechanism by which ivermectin exerts its effect on Onchocercal microfilariae remains unclear.48) In binding to GUCl−, ivermectin disrupts neurotransmission that is regulated via these channels in nematodes. But in culture, the drug has little direct effect on microfilariae when administered at pharmacologically relevant concentrations. It is now believed that the drug actually disrupts the fundamental host-parasite equilibrium. The half-life of ivermectin in humans is 12–36 hours, while metabolites may persist for up to three days. As lowest levels of dermal microfilariae occur well after this timeframe, it suggests that not all microfilariae affected by ivermectin are killed in the first few days. This is augmented by reports that microfilariae migrate into deeper dermal layers, sub-cutaneous fat, connective tissue and lymph nodes following administration of the drug.49) The prevailing school of thought is that ivermectin actually interferes with the ability of microfilariae to evade the human immune system, resulting in the host’s own immune response being able to overcome the immature worms and so kill them.50) Recently published research has indicated that GUCl− activity is solely expressed in musculature surrounding the microfilarial excretory–secretory (ES) vesicle, suggesting that any compound originating from the ES vesicle is regulated by the activity. The addition of ivermectin markedly reduces the amount of a protein (which is postulated to play a role in helping the parasite elude the host’s immune system) that is released from the ES in microfilariae.51) The growing body of evidence supports the theory that the rapid microfilarial clearance following ivermectin treatment results not from the direct impact of the drug but via suppression of the ability of the parasite to secrete proteins that enable it to evade the host’s natural immune defence mechanism.
Animal models have indicated conclusively that Th2 responses instil protective immunity against both L3 infective larvae and the microfilaria stage but that parasites are generally able to avoid these responses. This indicates that development of an effective vaccine may be possible, once a more comprehensive understanding of the process has been established.52) This overview may help explain the absence or comparatively slow development of drug resistance in the parasites in individuals, many of whom have been exposed to over 20 years of regular ivermectin treatment.
Drug resistance
Soon after its use became widespread in animal health, ivermectin resistance began to appear, at first in small ruminants but also, more significantly in cattle parasites, especially Cooperia spp.53) It is well known that high-level resistance to ivermectin appears in free-living Caenorhabditis elegans.54) Thankfully, despite 30 years of constant worldwide use, there have been no reports of resistance in canine heartworms or among equine Strongyloides parasites. More importantly, despite some 22 years of constant monotherapy in humans, no convincing evidence of resistance in Onchocerca volvulus has yet been found, although there are indications that resistance may be starting to develop and that resistant parasites are being selected.55,56)
New horizons
Ivermectin has continually proved to be astonishingly safe for human use. Indeed, it is such a safe drug, with minimal side effects, that it can be administered by non-medical staff and even illiterate individuals in remote rural communities, provided that they have had some very basic, appropriate training. This fact has helped contribute to the unsurpassed beneficial impact that the drug has had on human health and welfare around the globe, especially with regard to the campaign to fight Onchocerciasis.57)
Today, ivermectin is being increasingly used worldwide to combat other diseases in humans, such as Strongyloidiasis (which infects some 35 million each year), scabies (which causes 300 million cases annually), Pediculosis, Gnathostomiasis and Myiasis—and new and promising properties and uses for ivermectin and other avermectin derivatives are continuing to be found.58) These include activity against another neglected tropical disease, Leishmaniasis.59,60) Of perhaps even greater significance is the evidence that the use of ivermectin has both direct and indirect beneficial impact on improving community health. Studies of long-term treatment with ivermectin to control Onchocerciasis have shown that use of the drug is additionally associated with significant reduction in the prevalence of infection with any soil-transmitted helminth parasites (including Ascaris, Trichuris and hookworm), most or all of which are deemed to be major causes of the morbidity arising from poor childhood nutrition and growth.61) It is also known that the prevalence of head lice is markedly reduced in children taking ivermectin tablets62) and that scabies is markedly reduced in populations taking the drug regularly.63) Above all, ivermectin has proved to be a medicine of choice for the world’s rural poor. In many underprivileged communities throughout the tropics, intestinal worms and parasitic skin diseases are extremely common and associated with significant morbidity. They usually co-exist, with many individuals infected with both ecto- and endoparasites.64,65) Mass treatment of poly-parasitized populations is deemed to be the best means of control and ivermectin is the ideal drug for such interventions. A recent study in Brazil, using locally produced ivermectin, looked at the impact on internal helminthes and parasitic skin diseases. The researchers concluded that “mass treatment with ivermectin was an effective and safe means of reducing the prevalence of most of the parasitic diseases prevalent in a poor community in North-East Brazil. The effects of treatment lasted for a prolonged period of time”. This study also represented the first published report of human medical intervention using ivermectin that had not been produced by the hitherto traditional manufacturer, Merck & Co. Inc., the patent on the drug expiring in 1997.66)
In reality, the renewed interest in fighting tropical diseases, including the involvement of the pharmaceutical industry, which has become increasingly evident over the past three decades, and which has saved lives and improved the welfare of billions of people, notably the poor and disadvantaged in the topics, can be traced back to the 1987 introduction of ivermectin for use in humans. According to a recent report, International Federation of Pharmaceutical Manufacturers & Associations (IFPMA) data show that the global pharmaceutical industry provided over $9.2 billion in health interventions (medicines and equipment) between 2000–2007 alone, benefitting 1.75 billion people worldwide.67) The hitherto unprecedented donation of ivermectin in 1987 can rightly be seen to be the origin of this philanthropic outpouring.
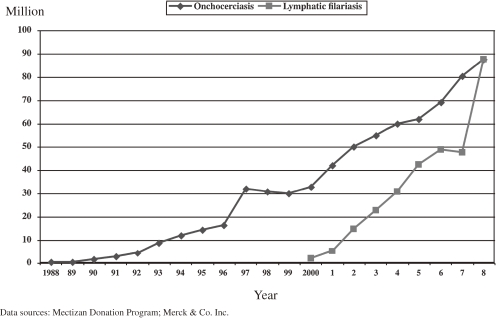
Since the inception of the Mectizan Donation Programme, Merck has donated well over 2.5 billion Mectizan® tablets for Onchocerciasis treatment, with in excess of 700 million treatments authorised. Currently, some 80–90 million people are taking the drug annually through MDA in Africa, Latin America and Yemen. A further 300 million total treatments have been approved for lymphatic filariasis, with around 90 million treatments being administered annually (Fig. 8 ). At present 33 countries are receiving ivermectin for Onchocerciasis and 15 for Lymphatic filariasis. Consequently, around US$4 billion worth of ivermectin tablets have been donated to date. In 2010, Ecuador became the second country in the Americas to halt River Blindness transmission. It is hoped that transmission of the disease in the Western hemisphere will be stopped by 2012—a goal that will have been achieved thanks to twice-yearly MDA with ivermectin. Lymphatic filariasis is targeted for global elimination by 2020, and, if all goes well, Onchocerciasis may well be eliminated from Africa soon thereafter.
Figure 8.
Trend in ivermectin treatments approved (1988–2008).
It has, thus far, been a long and eventful journey from ivermectin’s origins in Japanese soil. Fortunately, and contrary to the position seen with most antibiotics, despite several decades of monotherapy and occasional suboptimal responses observed in some individuals, there is no conclusive evidence that drug resistance is developing in human Onchocercal parasites. Not surprisingly, public health specialists worldwide are now calling for greater and more extensive use of ivermectin,68) labelling MDA of the ‘wonder drug’ quite simply as “an underutilized public health strategy”. In response, the Kitasato Institute has initiated a global collaboration to investigate all properties and potential of a range of ivermectin analogues, both individually and in combination, particularly with a view to having a ready-made alternative should resistance to current ivermectin monotherapy ever threaten ongoing disease elimination campaigns.
Acknowledgement
We would like to thank Prof. W.C. Campbell for his valuable, long-term collaboration, including his critical reading of a draft of this paper and for his constructive comments.
Biographies
Profile
Satoshi Ōmura is Professor Emeritus of Kitasato University and Special Coordinator of the Drug Discovery Project from Natural Products. He was born in 1935 and received his Ph.D. in Pharmaceutical Sciences from the University of Tokyo in 1968 and in Chemistry from Tokyo University of Science in 1970. He held a Visiting Professor post at Wesleyan University in the USA before returning to the Kitasato Institute and being appointed as a Professor of the School of Pharmaceutical Sciences, Kitasato University in 1975. He served as President of The Kitasato Institute from 1990 to 2008. His research interests are the discovery of useful compounds from microorganisms, the biosynthesis and hybrid biosynthesis of new macrolide antibiotics, the breeding, genetic analysis, and mapping of Streptomyces avermectinius, the synthesis of novel semisynthetic macrolides, and the organic synthesis of new compounds. His work has led to the discovery of well over 400 new chemicals, several of which have become leading drugs that have improved the lives and welfare of billions of people worldwide. He is a recipient of the Japan Academy Prize (1990), ACS Nakanishi Prize (2000), ACS Ernest Guenther Award in the Chemistry of Natural Products (2005), ICID Hamao Umezawa Memorial Award (2007), Tetrahedron Prize (2010) and many other national and international awards. He is a member of the German Academy of Sciences Leopoldina (1992), National Academy of Sciences, USA (1999), the Japan Academy (2001), Institut de France, Académie des Sciences (2002), Russian Academy of Sciences (2004), and Chinese Academy of Engineering (2005), and is an honorary member of Royal Society of Chemistry (2006).
Profile
Andy Crump was born in the UK and graduated from universities in the UK and USA with degrees in Biological Sciences and Ecology/Ethology. His initial biological research work in the USA focussed on cold-tolerance and supercooling in insects, funded by the National Science Foundation as part of an investigation of the feasibility of freezing and reviving humans for possible space flight. This was followed by teaching and Environmental Impact Assessment work in the USA, and several years as a Research Biologist at Imperial College, London working on a UK government-supported project investigating the behaviour and biocontrol of tsetse flies. Since then, he has travelled, observed and reported, living and working in several countries in Europe, North America, Africa, Asia and the Pacific Islands.
During his career, he has devoted over 30 years toward developing expertise in all aspects of communications and Information Design, with a particular interest in visual and cultural literacy. He has carried out numerous video, photo and journalistic missions in Asia, Africa, Latin America and Oceania, including those undertaken after he was asked to help set up the audiovisual components of the Panos Institute in London (in 1988) and the TDR Image Library at the WHO in Geneva (in 1991), the latter quickly becoming the world’s premier resource for still and moving images on all aspects of Neglected Tropical Diseases. An accomplished author and producer, his work in communications, especially in the science and health fields, is wide-ranging and diverse. During his time at the Panos Institute, well over a decade in the UNICEF/UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases (TDR) and for a wide variety of clients, his work has encompassed conceptualizing, researching, writing, scripting, and producing a wide range of books, articles, multimedia products and interactive packages, with the goal of disseminating scientific information to all varieties, and differing levels, of audience—utilizing a wide range of dissemination options, including scientific journals, the general press, reference books, technological journals and audiovisual media. He has also undertaken photojournalism presentations, exhibitions, and various electronic publishing activities (including video, television, CD-ROM and website projects). Clients have included NGOs, industry, academia, several UN bodies, the European Union, etc. He relocated to Tokyo in 2004 and has been involved with the Kitasato Institute and Kitasato University ever since. He currently lectures at Kitasato University, which has introduced Japan’s first ever Science Communication course, as well as Keio University, and continues to work with many international partners and clients, including several UN agencies, continuing to create significant international partnerships in the process.
References
- 1).Ōmura S., Crump A. (2005) The life and times of ivermectin: A success story. Nat. Rev. Microbiol. 2 (12), 984–989 [DOI] [PubMed] [Google Scholar]
- 2).Ōmura S. (2008) Ivermectin: 25 years and still going strong. Int. J. Antimicrob. Agents 31, 91–98 [DOI] [PubMed] [Google Scholar]
- 3).Campbell, W.C. (1992) The genesis of the antiparasitic drug ivermectin. In Inventive Minds (eds. Weber, R.J. and Perkins, D.N.). Oxford University Press, New York, pp. 194–214. [Google Scholar]
- 4).Frost, L., Reich, M.R. and Fujisaki, T. (2002) A partnership for ivermectin: Social Worlds and Boundary Objects. In Public-Private: Partnerships for Public Health (ed. Reich, M.R.). Harvard University Press, Cambridge, Mass., pp. 87–114. [Google Scholar]
- 5).Tavis, L.A. (1997) River Blindness: The Merck Decision to Develop and Donate MECTIZAN. In Power and Responsibility: Multinational Managers and Developing Country Concerns. University of Notre Dame Press, Indiana, pp. 87–113. [Google Scholar]
- 6).Thylefors B. (2008) The Mectizan donation program. Ann. Trop. Med. Parasitol. 102 (Suppl. 1), 39–44 [DOI] [PubMed] [Google Scholar]
- 7).Burg R.W., Miller B.M., Baker E.E., Birnbaum J., Currie S.A., Hartman R., Kong Y.L., Monaghan R.L., Olson G., Putter I., Tunac J.B., Wallick H., Stapley E.O., Oiwa R., Ōmura S. (1979) Avermectins, new family of potent anthelmintic agents: producing organisms and fermentation. Antimicrob. Agents Chemother. 15 (3), 361–367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Miller T.W., Chaiet L., Cole D.J., Cole L.J., Flor J.E., Goegleman R.T., Gullo V.P., Joshua H., Kempf A.J., Krellwitz W.R., Monaghan R.L., Ormond R.E., Wilson K.E., Albers-Schönberg G., Putter I. (1979) Avermectins, new family of potent anthelmintic agents: isolation and chromatographic properties. Antimicrob. Agents Chemother. 15 (3), 368–371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9).Egerton J.R., Ostlind D.A., Blair L.S., Eary C.H., Suhayda D., Cifelli S., Riek R.F., Campbell W. (1979) Avermectins, new family of potent anthelmintic agents: efficacy of the B1A component. Antimicrob. Agents Chemother. 15 (3), 372–378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Chabala J.C., Mrozik H., Tolman R.L., Eskola P., Lusi A., Peterson L.H., Woods M.F., Fisher M.H., Campbell W.C. (1980) Ivermectin, a new broad-spectrum antiparasitic agent. J. Med. Chem. 23, 1134–1136 [DOI] [PubMed] [Google Scholar]
- 11).Campbell W.C., Fisher M.H., Stapley E.O., Albers-Schönberg G., Jacob T.A. (1983) Ivermectin: a potent antiparasitic agent. Science 221, 823–828 [DOI] [PubMed] [Google Scholar]
- 12).Burg, R.W. and Stapley, E.O. (1989) Isolation and characterization of the producing organism. In Ivermectin and Abamectin (ed. Campbell, W.C.). Springer, New York, pp. 24–32. [Google Scholar]
- 13).Grisi L., Massard C.L., Moya-Borja G.E., Pereira J.B. (2002) Impacto econômico das principais ectoparasitoses em bovinos no Brasil. Hora Veterinária 21, 8–10 [Google Scholar]
- 14).Ottesen E., Campbell W. (1994) Ivermectin in human medicine. J. Antimicrob. Chemother. 34, 195–203 [DOI] [PubMed] [Google Scholar]
- 15).Eckholm E. (1989) Conquering an ancient scourge; river blindness. N.Y. Times Mag., 20–27 (Jan 8, 1989).11647870 [Google Scholar]
- 16).UNESCO (2005) World Science Report (2005) UNESCO, Paris, p. 198. [Google Scholar]
- 17).WHO (2010) Onchocerciasis (http://www.who.int/topics/onchocerciasis/en/).
- 18).Taylor H.R., Pacqué M., Muñoz B., Greene B.M. (1990) Impact of mass treatment of onchocerciasis with ivermectin on the transmission of infection. This Week in Science 250 (5 October), 116–118 [DOI] [PubMed] [Google Scholar]
- 19).WHO (1995) Onchocerciasis and its control. Report of a WHO Expert Committee on Onchocerciasis Control Technical Report Series, No. 852 World Health Organization, Geneva, pp. 1--110. [PubMed] [Google Scholar]
- 20).WHO/TDR (1995) Tropical Disease Research: Progress 1975–94. WHO, Geneva, p. 95. [Google Scholar]
- 21).Denham, D.A. and Barrett, J. (1987) The chemotherapy of filarial nematode infections of man: aspirations and problems. In Chemotherapy of Tropical Diseases: The problem and the challenge (ed. Hooper, M.). John Wiley & Sons. Ltd., pp. 45–68. [Google Scholar]
- 22).Duke B.O. (1962) Experimental transmission of Onchocerca volvulus to chimpanzees. Trans. R. Soc. Trop. Med. Hyg. 56, 271 [Google Scholar]
- 23).Duke B.O. (1977) The effects of some drugs—pentamidine, stibocaptate, Hoechst 33258, F 151, compound ‘E’ and Nifurtimox—on Onchocerca volvulus in chimpanzees. Tropenmed. Parasitol. 28 (4), 447–455 [PubMed] [Google Scholar]
- 24).Fujisaki, T. and Reich, M. (1998) TDR’s contribution to the development of ivermectin for onchocerciasis. TDR, Geneva (TDR/ER/RD/98.3). [Google Scholar]
- 25).WHO/TDR (1976) Participation of the Pharmaceutical sector (TDR/WP/76.30).
- 26).Lucas, A.O. (2002) Public-private partnerships: illustrative examples. In Public-Private Partnerships for Public Health (ed. Reich M.). Harvard University Press, Cambridge, Mass., pp. 19–39. [Google Scholar]
- 27).Campbell W.C. (1991) Ivermectin as an antiparasitic agent for use in humans. Annu. Rev. Microbiol. 45, 445–474 [DOI] [PubMed] [Google Scholar]
- 28).Sturchio, J.L. (1992) The Decision to Donate Mectizan: Historical Background. Merck & Co., Inc. Rahway, New Jersey, USA (unpublished document). [Google Scholar]
- 29).Aziz M.A., Diallo S., Diop I.M., Larivière M., Porta M. (1982) Efficacy and tolerance of ivermectin in human onchocerciasis. Lancet 2, 171–173 [DOI] [PubMed] [Google Scholar]
- 30).Coulaud J.P., Larivière M., Gervais M.C., Gaxotte P., Aziz A., Deluol A.M., Cenac J. (1983) Treatment of human onchocerciasis with ivermectin. Bull. Soc. Pathol. Exot. Filiales 76, 681–688 [PubMed] [Google Scholar]
- 31).Telex from Robert D. Fluss of Merck & Co. Inc’s Division of International Public Affairs sent to the Director of WHO/TDR, Dr Adetokunbo Lucas, on 20 June, 1986.
- 32).Campbell W.C. (2010) History of avermectin and ivermectin, with notes on the history of other macrocyclic lactone antiparasitic agents. In The Chemotherapy of Parasitic Diseases: Macrocyclic Lactones. Curr. Pharm. Biotechnol. 11 (In press) [DOI] [PubMed] [Google Scholar]
- 33).Awadzi K. (1980) The chemotherapy of onchocerciasis II: Quantification of the clinical reaction to microfilaricides. Ann. Trop. Med. Parasitol. 74 (2), 189–197 [DOI] [PubMed] [Google Scholar]
- 34).Dadzie K.Y., Bird A.C., Awadzi K., Schulz-Key H., Gilles H.M., Aziz M.A. (1987) Ocular findings in a double-blind study of ivermectin versus diethylcarbamazine versus placebo in the treatment of onchocerciasis. Br. J. Ophthalmol. 71, 78–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35).Larivière M., Aziz M., Weimann D., Ginoux J., Gaxotte P., Vingtain P., Beauvais B., Derouin F., Schultz-Key H., Basset D., Sarfati C. (1985) Double-blind study of ivermectin and diethylcarbamazine in African onchocerciasis patients with ocular involvement. Lancet 326, 174–177 [DOI] [PubMed] [Google Scholar]
- 36).Diallo S., Aziz M.A., Ndir O., Badiane S., Bah I.B., Gaye O. (1987) Dose-ranging study of ivermectin in the treatment of Filariasis due to Wuchereria bancrofti. Lancet (320), 1030. [DOI] [PubMed] [Google Scholar]
- 37).Kumaraswami V., Ottesen E.A., Vijayasekran V. (1988) Ivermectin for treatment of Wuchereria bancrofti filariasis: efficacy and adverse reactions. JAMA 259, 3150–3153 [PubMed] [Google Scholar]
- 38).Ottesen E.A., Kumaraswami V., Vijayasekran V. (1990) A controlled trial of ivermectin and diethylcarbamazine in lymphatic filariasis. N. Engl. J. Med. 322, 1113–1117 [DOI] [PubMed] [Google Scholar]
- 39).Richards F.O., Jr., Eberhard M.L., Bryan R.T., Mcneeley D.F., Lammie P.J., Mcneeley M.B., Bernard Y., Hightower A.W., Spencer H.C. (1991) Comparison of high-dose ivermectin and diethylcarbamazine for activity against Bancroftian filariasis in Haiti. Am. J. Trop. Med. Hyg. 44, 3–10 [DOI] [PubMed] [Google Scholar]
- 40).WHO (1997) World Health Assembly Resolution WHA 50.29 (http://www.who.int/lymphatic_filariasis/resources/WHA_50%2029.pdf).
- 41).Turner, M. and Schaeffer, J.M. (1989) Mode of action of ivermectin. In Ivermectin and Avermectin (ed. Campbell, W.). Springer-verlag, New York, pp. 73–88. [Google Scholar]
- 42).Campbell W.C. (1985) Ivermectin: an update. Parasitol. Today 1, 10–16 [DOI] [PubMed] [Google Scholar]
- 43).Omura, S. (2002) Mode of action of avermectin. In Macrolide antibiotics; Chemistry, Biology & Practice (2nd Edition) (ed. Omura, S.). Academic Press, San Diego, pp. 571–575. [Google Scholar]
- 44).del Mar Saez-De-Ocariz M., McKinster C.D., Orozco-Covarrubias L., Tamayo-Sánchez L., Ruiz-Maldonaldo R. (2002) Treatment of 18 children with scabies or cutaneous larva migrans using ivermectin. Clin. Exp. Dermatol. 27, 264–267 [DOI] [PubMed] [Google Scholar]
- 45).Maizels R.M., Lawrence R.A. (1991) Immunological tolerance: the key feature in human filariasis? Parasitol. Today 7, 271–276 [DOI] [PubMed] [Google Scholar]
- 46).Taylor H.R., Greene B.M. (1989) The status of ivermectin in the treatment of human onchocerciasis. Am. J. Trop. Med. Hyg. 41, 460–466 [DOI] [PubMed] [Google Scholar]
- 47).Plaisier A.P., Alley E.S., Boatin B.A., Van Oortmarssen G.J., Remme H., De Vlas S.J., Bonneux L., Habbema J.D. (1995) Irreversible effects of ivermectin on adult parasites in onchocerciasis patients in the Onchocerciasis Control Programme in West Africa. J. Infect. Dis. 172, 204–210 [DOI] [PubMed] [Google Scholar]
- 48).Basáñez M.-G., Pion S.D., Boakes E., Filipe J.A., Churcher T.S., Boussinesq M. (2008) Effect of single-dose ivermectin on Onchocerca volvulus: s systematic review and meta-analysis. Lancet Infect. Dis. 8 (5), 310–322 [DOI] [PubMed] [Google Scholar]
- 49).Duke B.O., Soula G., Zea-Flores G., Bratthauer G.L., Doumbo O. (1991) Migration and death of skin-dwelling Onchocerca volvulus microfilariae after treatment with ivermectin. Trop. Med. Parasitol. 42, 25–30 [PubMed] [Google Scholar]
- 50).Mackenzie C.D., Geary T.G., Gerlach J.A. (2003) Possible pathogenic pathways in the adverse clinical events seen following ivermectin administrations in onchocerciasis patients. Filaria J. 2 (Suppl. 1), S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51).Moreno Y., Nabhan J.F., Solomon J., MacKenzie C.D., Geary T.G. (2010) Ivermectin disrupts the function of the excretory-secretory apparatus in microfilariae of Brugia malayi. Proc. Natl. Acad. Sci. USA 107 (46), 20120–20125 (doi:10.1073/pnas.1011983107). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52).Allen J.E., Adjei O., Bain O., Hoerauf A., Hoffmann W.H., Makepeace B.L., Schulz-Key H., Tanya V.N., Trees A.J., Wanji S., Taylor D.W. (2008) Of mice, cattle and humans: The immunology and treatment of River Blindness. PLoS Negl. Trop. Dis. 2 (4), e217 (doi:10.1371.pntd.0000217). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53).Kaplan R.M. (2004) Drug resistance in nematodes of veterinary importance: a status report. Trends Parasitol. 20, 477–481 [DOI] [PubMed] [Google Scholar]
- 54).Dent J.A. (2000) The genetics of ivermectin resistance in Caenorhabditis elegans. Proc. Natl. Acad. Sci. USA 97, 2674–2679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55).Wolstenholme A.J. (2004) Drug resistance in veterinary helminths. Trends Parasitol. 20, 469–476 [DOI] [PubMed] [Google Scholar]
- 56).Lustigman S., McCarter J.P. (2007) Ivermectin resistance in Onchocerca volvulus: Toward a genetic basis. PLoS Negl. Trop. Dis. 1 (1), e76 (doi:10.1371/journal.pntd.0000076). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57).Ōmura, S. and Crump, A. (2009) Community-directed intervention: replicating Japan’s health successes in Africa? In Innovating for the health of all. Global Forum Update on Research for Health (6), Global Forum for Health Research, Geneva, pp. 87–90. [Google Scholar]
- 58).Geary T.G. (2005) Ivermectin 20 years on: maturation of a wonder drug. Trends Parasitol. 21 (11), 530–532 [DOI] [PubMed] [Google Scholar]
- 59).dos Santos A.R., Falcão C.A., Muzitano M.F., Kaiser C.R., Rossi-Bergmann B., Férézou J.P. (2009) Ivermectin-derived leishmanicidal compounds. Bioorg. Med. Chem. 17 (2), 496–502 [DOI] [PubMed] [Google Scholar]
- 60).Pitterna T., Cassayre J., Hüter O.F., Jung P.M., Maienfisch P., Kessabi F.M., Quaranta L., Tobler H. (2009) New ventures in the chemistry of avermectins. Bioorg. Med. Chem. 17 (12), 4085–4095 [DOI] [PubMed] [Google Scholar]
- 61).Moncayo A.L., Vaca M., Amorim L., Rodriguez A., Erazo S., Oviedo G., Quinzo I., Padilla M., Chico M., Lovato R., Gomez E., Barreto L.B., Cooper P.J. (2008) Impact of long-term treatment with ivermectin on the prevalence and intensity of soil-transmitted helminth infections. PLoS Negl. Trop. Dis. 2 (9), e293 (doi:10.1371/journal.pntd.000293). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62).Dunne C.L., Malone C.J., Whitworth J.A. (1991) A field study of the effects of ivermectin on ectoparasites of Man. Trans. R. Soc. Trop. Med. Hyg. 85, 550–551 [DOI] [PubMed] [Google Scholar]
- 63).Bockarie M.J., Alexander N.D., Kazura J.W., Bockarie F., Griffin L., Alpers M.P. (2000) Treatment with ivermectin reduces the high prevalence of scabies in a village in Papua New Guinea. Acta Trop. 75, 127–130 [DOI] [PubMed] [Google Scholar]
- 64).Albonico M., Crompton D.W., Savioli L. (1999) Control strategies for human intestinal nematode infections. Adv. Parasitol. 42, 277–341 [DOI] [PubMed] [Google Scholar]
- 65).Heukelbach J. (2004) Ectoparasites—the underestimated realm. Lancet 363, 889–891 [DOI] [PubMed] [Google Scholar]
- 66).Heukelbach J., Winter B., Wilcke T., Muehlen M., Albrecht S., de Oliviera F.A., Kerr-Pontes L.R., Liesenfeld O., Feldmeier H. (2004) Selective mass treatment with ivermectin to control intestinal helminthiasis and parasitic skin diseases in a severely affected population. Bull. World Health Organ. 82 (8), 559–636 [PMC free article] [PubMed] [Google Scholar]
- 67).Editorial (2010) Nat. Rev. Microbiol. 8, 244 (doi:10.1038/nrmicro2345).20344825 [Google Scholar]
- 68).Speare R., Durrheim D. (2004) Mass treatment with ivermectin: an underutilized public health strategy. Bull. World Health Organ. 82 (8), 559–636 [PMC free article] [PubMed] [Google Scholar]