Abstract
The purpose of our study was to extract the two-dimensional (2D) cardiothoracic ratio from digital chest radiographs using image analysis software on a Magic View 300 system. We also wanted to investigate its correlation with cardiac function, as defined by left ventricular ejection fraction from MUGA scanning, and with the traditional one-dimensional cardiothoracic ratio. One hundred patients undergoing radionuclide ventriculography and concurrent digital PA chest radiography using a commercial selenium detector system were studied. The 2D cardiothoracic ratio was extracted by defining a region of interest around the cardiac and thoracic areas and calculating a ratio of the two pixel counts obtained. The one-dimensional cardiothoracic ratio was calculated in the traditional manner. Regression analysis was used to study the association between these ratios and the ejection fraction. The 2D ratio could be achieved on all radiographs after image manipulation. The traditional linear cardiothoracic ratio showed an inverse correlation with left ventricular ejection fraction (r = −0.45). The 2D cardiothoracic ratio showed an improved correlation (r = −0.52). Assuming that a left ventricular ejection fraction of 55% or more indicates normal cardiac function, the normal 2D cardiothoracic ratio is 0.23 or less and a ratio of 1:4 is suggested. The ratio of cardiac and thoracic area correlates better with cardiac function as assessed by left ventricular ejection fraction than the traditional linear cardiothoracic ratio. Two-dimensional cardiothoracic ratio is easily extracted and improves the data yield from digital PA chest radiographs on PACS systems.
Keywords: Cardiothoracic ratio, chest, digital radiography, computed radiography
The advent of digital radiology and computerized workstations renders it very easy to measure both the traditional one-dimensional (1D-CTR) and two-dimensional cardiothoracic ratios (2D-CTR) routinely on digital chest radiographs. The CTR was first proposed by Danzer in 1919 to screen military recruits.1 Many other cardiac area and volume measurements derived from chest radiographs have been described and correlated with other measures of cardiac status, but, because they were tedious to measure and calculate manually, they have been generally neglected. This study was undertaken to assess whether 2D-CTR correlates better than the 1D-CTR with an objective measure of cardiac function (left ventricular ejection fraction [LVEF] assessed by multiple uptake gated acquisition [MUGA] scan). A minor enhancement of data yield from the plain chest radiograph would be significant because it is still the most common investigation performed in the radiology department.
MATERIAL AND METHODS
Standard 6-FtPA digital chest radiographs were obtained (Thorovision, Phillips Medical, Shelton, CT) on 100 patients undergoing concurrent radionuclide ventriculography. These were transmitted to a PACS (Siemens, Erlangen, Germany) network for analysis. Standard image analysis software was used to study the images. The 1D-CTR was calculated in the conventional manner as the ratio between the maximum transverse cardiac diameter and the maximum thoracic diameter measured between the inner margins of the ribs (Fig 1). The cardiac area and total thoracic area were measured in pixel numbers (Fig 2). The cardiac boundary was delineated inferiorly by drawing a line from the right cardiophrenic angle to the line of intersection of the left cardiac border and the left hemidiaphragm, superiorly by the inferior margins of the right and left main bronchi, laterally by direct inspection. These boundaries were found to be most reproducible as image manipulation on a workstation invariably permits easy observation of the margins of the main bronchi. The thoracic area was measured using a mouse and linear trace to define a region of interest along the inner costal margin and diaphragm. The 2D-CTR is taken as the ratio between the pixel counts of the cardiac outline and the whole thorax as described. Patients underwent radionuclide venriculography for the purpose of renal transplant workup (16 patients), for assessment of known ischemic cardiac disease (46 patients) or for cardiac assessment in patients with peripheral vascular disease (38 patients). Patients with known valvular heart disease were excluded from our study.
Figure 1.
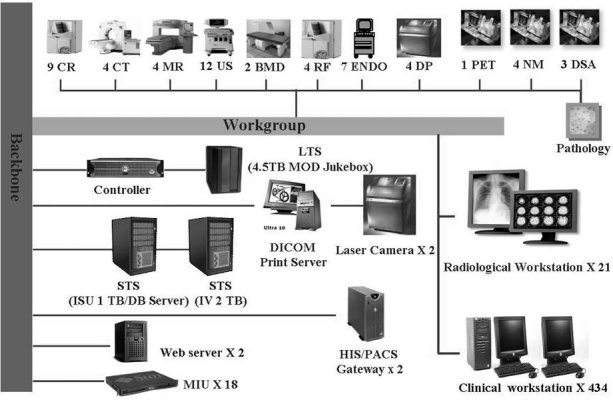
The traditional one-dimensional cardiothoracic ratio.
Figure 2.
The margins of the thoracic area and the cardiac area are outlined, as used to give the two-dimensional cardiothoracic ratio.
Equilibrium radionuclide ventriculography was used to estimate the LVEF. Red blood cells were labeled in vivo by injecting 5 mg of stannous pyrophosphate followed 20 min later by 740 Mbq of technetium 99m. Imaging was carried out on a Toshiba 7100A gamma camera using a LEGP parallel whole collimator. Multiple gated acquisition was performed using a left anterior oblique view of between 30 and 45 degrees. Images were acquired in a 64 × 64-pixel matrix, in 24 frames, for 15 min. A 15% arrhythmia rejection test was applied. Background subtraction was performed using a curvilinear area of interest lateral to the left ventricle. A ventricular time activity curve was produced and the LVEF was calculated using standard software.
RESULTS
Regression analysis was used to examine the data set for an association between the ejection fraction and the traditional and 2D-CTR. The correlation between the 1D-CTR and LVEF was inverse and somewhat limited (r = −0.45) (P < 0.01). The inverse correlation between the 2D-CTR and LVEF was improved (r = −0.52) (P < 0.01). The association between the 1D- and 2D-CTR predictably showed a strong correlation (r = 0.82). Finally, each of the patient subgroups in turn was examined for an association between the ejection fraction and the 1D- and 2D- CTR using regression analysis. None of these subgroups showed any significant improvement in correlation either for the 1D- or 2D-CTR.
The data were then used to calculate a value for a 2D-CTR that might be used as an indicator of normal cardiac function. If it is assumed that an ejection fraction of 55% or more indicates normal cardiac function, then, using the regression equations, a figure of 0.23 is calculated for 2D-CTR. A similar calculation for the 1D data estimates a figure of 0.49 for the CTR which is in good agreement with the established value of 0.5. Thus, it can be concluded that by using 2D data for the cardiothoracic ratio, a value of 0.23 or less can be taken as normal.
DISCUSSION
The status of the traditional 1D-CTR in the radiological literature reflects a balance between the benefit of having a numerical value that can be followed up on sequential examinations and a realization of the numerous reasons why the CTR varies and correlates poorly with cardiac function.2 The depth of inspiration, the stage of the cardiac cycle, body habitus, and the fact that cardiac size may be unchanged in all but later stages of cardiac disease all cause poor CTR correlation with cardiac function studies.
Until the advent of digital images and workstations, geometrical calculations on plain chest films more complex than CTR assessment were too time-consuming for general use.3 A digital chest radiograph contains 12 MB of data but is generally reported on without further analysis. By contrast, computed tomography and magnetic resonance images have less digital data but use computer analysis much more to enrich the information yield. We describe a technique to enhance cardiac assessment and thereby improve the information yield from the digital PA chest radiograph.
On a chest film the heart size is seen as a two-dimensional structure and is invariably correlated with chest size by the radiologist. However, the size of the cardiac outline varies with the cardiac cycle, the size of the chest, the level of inspiration, patient posture, and the radiographic projection,4, 5 and the thoracic area may be affected by pulmonary or abdominal pathology. The CTR is more valuable than absolute measurement of cardiac diameters or area as the patient’s habitus corrects for itself, with larger patients generally having a larger thorax to amend the ratio for a larger heart size and the 2D-CTR allows for this correction in two dimensions. CTR uses a measure of cardiac size that correlates to a degree with cardiac function.6 MUGA measures data only from a single cardiac chamber (LV function) but is a good overall test of cardiac function and is known to correlate somewhat with cardiac size.7
It is difficult to find a suitable index of cardiac function for comparison with the CTR. MUGA takes information only from a single chamber, and it can be argued that LVEF can be normal in the presence of a grossly abnormal heart size, eg, mitral stenosis. However, patients with known valvular heart disease were not included in our study, and it is likely that the left ventricle will be the predominant chamber in most patients. Our study shows an improved correlation between CTR and LVEF than that found in other studies8 and 2D-CTR shows further improvement.
The relationships between measurements of cardiac dimensions on plain chest radiography on the one hand and cardiac function, disease, and prognosis on the other have been discussed in the literature for 80 years without final agreement because there has been poor correlation. A positive correlation has been described between three-dimensional cardiac volume derived from plain chest films and ejection fraction.9 A positive correlation is also described between three-dimensional and one-dimensional heart measurements on chest radiographs and left ventricular enlargement measured by quantitative angiographic findings.10, 11 Recent studies have shown the chest radiograph to have relatively high specificity in predicting cardiac enlargement on echocardiography.12 A positive association has been found between three- and two-dimensional echocardiography and LVEF with MUGA.6, 13, 14 Two-dimensional partial cardiac area has also been shown to correlate positively with post mortem studies of cardiac size.15 However, no useful correlation has been reported in other studies between 1D-CTR and determination of left ventricular size or structure.16, 17 In other studies, CTR has been shown to correlate poorly with echocardiographic function.8, 18 We feel the 2D-CTR offers a numerical estimate that correlates better with LV function than the CTR and can be estimated on initial and sequential examinations as a cardiac assessment measurement. Although not appropriate in all patients, we believe the small increase in analysis time is justifiable in those patients with a borderline CTR or in the sequential follow-up of known cardiac disease, where subtle changes in cardiac function are important.
In the future, three-dimensional cardiac volume calculations from PA and lateral chest radiographs will be easier to achieve with appropriate computer programs on workstations. Previous methods of cardiac measurement calculation requiring manual measurements on plain films have been tedious, whereas with workstations these measurements may be used routinely to enrich the information yield on basic chest films.
We describe a simple method of improving the data yield from digital chest radiographs by simple image manipulation on workstations. Our 2D-CTR shows an improved correlation with cardiac function compared with the traditional CTR. We concur with other authors8 in accepting that radiographic assessment of the heart cannot replace LVEF measurement by echocardiographic or radionuclide means, but we believe that the 2D-CTR can be of help to the radiologist in the initial and subsequent assessment of the heart on digital chest radiographs. Further studies are required to determine the sensitivity of follow-up 2D-CTR in detecting changing cardiac function, as detected on other indices.
References
- 1.Danzer CS. The cardiothoracic ratio: an index of cardiac enlargement. Am J Med Sci. 1919;157:513–521. [Google Scholar]
- 2.Dinsmore RE, Goodman DJ, Sanders CA. Some pitfalls in the evaluation of cardiac chamber enlargement on chest roentgenograms. Radiology. 1966;87(2):267–273. doi: 10.1148/87.2.267. [DOI] [PubMed] [Google Scholar]
- 3.Schwarz GS. Determination of frontal plane area from the product of the long and short diameters of the cardiac silhouette. Radiology. 1946;47:360–370. doi: 10.1148/47.4.360. [DOI] [PubMed] [Google Scholar]
- 4.Jagt EJ, Smits HJ. Cardiac size in the supine chest film. Eur J Radiol. 1992;14(3):173–177. doi: 10.1016/0720-048x(92)90080-s. [DOI] [PubMed] [Google Scholar]
- 5.Meyer RR. Heart measurement. A simplified method. Radiology. 1949;52:691–699. doi: 10.1148/52.5.691. [DOI] [PubMed] [Google Scholar]
- 6.Gopal AS, Shen Z, Sapin PM, et al. Assessment of cardiac function by three-dimensional echocardiography compared with conventional noninvasive methods. Circulation. 1995;92(4):842–853. doi: 10.1161/01.cir.92.4.842. [DOI] [PubMed] [Google Scholar]
- 7.Massie BM, Kramer BL, Gertz EW, et al. Radionuclide measurement of left ventricular volume: comparison of geometric and counts-based methods. Circulation. 1982;65(4):725–730. doi: 10.1161/01.cir.65.4.725. [DOI] [PubMed] [Google Scholar]
- 8.Philbin EF, Garg R, Danisa K, et al. The relationship between cardiothoracic ratio and left ventricular ejection fraction in congestive heart failure. Digitalis Investigation Group. Arch Intern Med. 1998;158(5):501–506. doi: 10.1001/archinte.158.5.501. [DOI] [PubMed] [Google Scholar]
- 9.Hammermeister KE, Chikos PM, Fisher L, et al. Relationship of cardiothoracic ratio and plain film heart volume to late survival. Circulation. 1979;59(1):89–95. doi: 10.1161/01.cir.59.1.89. [DOI] [PubMed] [Google Scholar]
- 10.Chikos PM, Figley MM, Fisher L. Correlation between chest film and angiographic assessment of left ventricular size. Am J Roentgenol. 1977;128(3):367–373. doi: 10.2214/ajr.128.3.367. [DOI] [PubMed] [Google Scholar]
- 11.Chikos PM, Figley MM, Fisher L. Visual assessment of total heart volume and specific chamber size from standard chest radiographs. Am J Roentgenol. 1997;128(3):375–380. doi: 10.2214/ajr.128.3.375. [DOI] [PubMed] [Google Scholar]
- 12.Satou GM, Lacro RV, Chung T, et al. Heart size on chest x-ray as a predictor of cardiac enlargement by echocardiography in children. Pediatr Cardiol. 2001;22(3):218–222. doi: 10.1007/s002460010207. [DOI] [PubMed] [Google Scholar]
- 13.Nosir YF, Fioretti PM, Vletter WB, et al. Accurate measurement of left ventricular ejection fraction by three-dimensional echocardiography. A comparison with radionuclide angiography. Circulation. 1996;94(3):460–466. doi: 10.1161/01.cir.94.3.460. [DOI] [PubMed] [Google Scholar]
- 14.Naik MM, Diamond GA, Pai T, et al. Correspondence of left ventricular ejection fraction determinations from two-dimensional echocardiography, radionuclide angiography and contrast cineangiography. J Am Coll Cardiol. 1995;25(4):937–942. doi: 10.1016/0735-1097(94)00506-L. [DOI] [PubMed] [Google Scholar]
- 15.Murphy ML, Blue LR, Thenabadu PN, et al. The reliability of the routine chest roentgenogram for determination of heart size based on specific ventricular chamber evaluation at postmortem. Invest Radiol. 1985;20(1):21–25. doi: 10.1097/00004424-198501000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Ten Cate FJ, Vletter WB, Brand MB, et al. The plain chest film as an unreliable method to determine left ventricular size. Jpn Heart J. 1977;18(6):878–882. doi: 10.1536/ihj.18.878. [DOI] [PubMed] [Google Scholar]
- 17.Rose CP, Stolberg HO. The limited utility of the plain chest film in the assessment of left ventricular structure and function. Invest Radiol. 1982;17(2):139–144. doi: 10.1097/00004424-198203000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Hada Y. Cardiothoracic ratio. J Cardiol. 1995;26(1):51–54. [PubMed] [Google Scholar]


