Abstract
The transformation from film-based to filmless operation has become more and more challenging, as imaging studies expand in size and complexity. To adapt to these changes, radiologists must proactively develop new workflow strategies to compensate for increasing work demands and the existing workforce shortage. This article addresses the evolutionary changes underway in the radiology interpretation process and reviews changes that have occurred in the past decade. These include a number of developments in soft-copy interpretation, which is migrating from a relatively static process, duplicating film-based interpretation, to a dynamic process, using multi-planar reconstructions, volumetric navigation, and electronic decision support tools. The result is optimization of the human–computer interface with improved productivity, diagnostic confidence, and interpretation accuracy.
Keywords: evolution of radiology practice, radiology interpretation, Transforming the Radiology Interpretation Process (TRIP)
THE EVOLUTIONARY FORCES underway within radiology are occurring at a faster pace than ever before. Technology expansion is evident throughout all medical disciplines, but no area is more affected than radiology, the only medical specialty that is 100% technology driven. This dependence on technology is a double-edged sword for medical practitioners. It creates a unique opportunity for economic growth and expansion while solidifying the position of its specialists within the medical community. At the same time, however, new imaging and computer technologies present an entirely new set of clinical, educational, and political challenges for the radiologist. As new technologies are introduced into the practice of radiology, so are heightened expectations concerning the timeliness of information delivery, the accuracy of radiologic diagnosis, and the overall standard of patient care.
The evolving technologies within medical imaging take on a variety of forms including imaging modalities to information systems, and picture archiving and communication systems (PACS). Radiologists, clinicians, technologists, and information technology (IT) personnel are bombarded daily with new medical imaging and computer applications that surpass their predecessors in speed, complexity, and sophistication. This creates a series of economic, educational, integration, and implementation challenges. The long-term success of these professionals will be tied in large part to their ability to incorporate the changing technologies into their workplace. This article, written from the perspective of the clinical radiologist, discusses how these evolutionary pressures are changing the way radiology is being practiced. We begin by analyzing current trends and then attempt to predict how future technology developments will change radiologist workflow and the interpretation process.
JUSTIFICATION FOR FILMLESS RADIOLOGY
To address the justification of filmless radiology, we must understand the existing factors contributing to the adoption of PACS and digital radiography. For most hospital-based imaging practices, PACS justification is primarily an economic issue. Hospital administrators generally argue that PACS, in and of itself, is not revenue generating and therefore cannot be cost-justified. Application of this “economic litmus test” for PACS is ironic when one considers that other digital information technologies, such as the hospital or radiology information system, have never required cost-justification.This may be merely an accident of timing. As more and more medical institutions strive to digitize all medical data through the electronic medical record, PACS becomes a necessary intermediary.
What if a hospital CEO does not see the inherent wisdom in these arguments and continues to justify film-based radiology? Will the radiologists affiliated with that film-based hospital be placing themselves at a competitive disadvantage or incur additional medical liability, when compared to their filmless radiologist counterparts? To answer these questions we must explore the existing radiologist market and explore what role PACS may play on radiologist staffing and performance.
In 1998, according to the American College of Radiology’s Professional Bureau, there were 1.3 job listings per job seeker.1 By 2000, this ratio of job listings to job seekers increased to 3.8,2 reflecting the existing crisis in the radiologist workforce. The recent article by Bhargavan et al.2 postulates that if the growth demand for imaging services continues to increase at its current rate and radiologist productivity enhancements are not achieved, then the radiologist shortage could increase by another 250%. The authors of the study postulated that PACS-related productivity enhancements could decrease the demand for radiologists by 20% over the next 10 years. This hypothesis that PACS can improve radiologist productivity has been reported in a number of other studies as well.3, 4, 5, 6 Such an increase in productivity is believed to be multi-factorial in nature. Some of the factors contributing to this improved radiologist workflow and productivity with PACS include automation of manual tasks (i.e., image display), electronic access to patient data (through integration of PACS and HIS/RIS), prefetching of historical comparison studies, use of electronic window/level presets, decreased interruptions, and reduced fatigue. At the same time, studies have demonstrated striking productivity gains for technologists as well associated with the use of PACS, when compared with film-based operation.7, 8, 9
In addition to improving radiologist workflow, PACS has the added theoretical benefit of improving interpretation accuracy. In a study by Reiner et al.10 soft-copy interpretation of computed tomography (CT) exams was associated with significant improvement in interpretation accuracy when compared with comparable hard-copy CT interpretation using film. This improvement is believed in large part to be the result of more liberal use of multiple window/level settings when using a computer workstation. This observation was substantiated in a study by Pomerantz et al.11 who found that routine review of additional window/level settings using a computer workstation (beyond those typically printed onto film) resulted in improved conspicuity and characterization of abnormalities in 67% of cases and additional findings of clinical significance in 18% of CT exams.
Although the combined effects of improving productivity and interpretation accuracy should justify the transition to filmless operation, additional factors add to the overall justification. Filmless operation with PACS has been shown to contribute to increased utilization of imaging services (which becomes revenue generating), reduced report turnaround time, improved clinician access to medical images, and decreased exam backlog. 12, 13, 14
TRANSFORMATION OF THE IMAGE-INTERPRETATION PROCESS
Once PACS and filmless imaging are shown to be justified, the next step is to understand how to maximize the technology to achieve its potential. To accomplish this, one must realize how much the technology has been transformed in its relatively short life-span. Although enterprise-wide filmless operation has been in existence for only a decade, several evolutionary changes have already been realized in the image-interpretation process. These are well illustrated with CT, which has undergone its own parallel transformation during this time period, from single-slice, to helical single channel, to helical multi-channel. During this relatively short time period of 10 years, typical abdominal/pelvic CT exams have gone from approximately 80 images to 1,000 images. This exponential increase in image number has effectively eliminated film as a practical form of image display. A 1,000-image exam printed on a 12-on-1 image format would require 84 individual sheets of film, for a single window/level setting only. The need to film images at lung, liver, soft tissue, and/or osseous settings may increase this estimated number of sheets of film by a factor of two to five. Conventional film display devices are equally obsolete for image interpretation. An eight-panel viewbox would require 11 separate “hangings” to accommodate the 84 sheets of film (single window/level setting), and this doesn’t take into account the need to hang comparison studies. Alternatively, the four-panel film alternator would require 21 individual stations, resulting in loss of radiologist spatial memory, highly inefficient workflow, and the potential to overlook subtle interval change when comparing serial examinations.
Radiologist workflow (in the soft-copy interpretation of CT exams) has undergone significant change during the first decade of PACS, with several different display/interpretation strategies employed (fig. 1). In the beginning, when hard-copy film images were replaced initially with soft-copy images, image display and navigation remained relatively static. Radiologists (and PACS vendors) elected to reproduce the “look and feel” of film images on the computer workstation, which typically contained four monitors, with images displayed in tile format. This was a logical extension when one considers the fact that these early PACS adopters were entirely trained in a film-based imaging environment and therefore elected to reproduce what they were familiar with. Unfortunately, many radiologists have remained fixed in this “soft-copy film” paradigm, not taking full advantage of the workflow and interpretation opportunities that are available. Many Radiologists also remained static in their approach to image manipulation, often trying to reproduce the digital image in the likeness of the film image. This was particularly true for digital radiography, where computed radiography (CR) adopters chose to ignore the ability of the computer to apply advanced processing techniques for accentuation of specific anatomic/pathologic features. Instead, many radiologists have maintained static image display, with a “single best” image presentation state.
Figure 1.
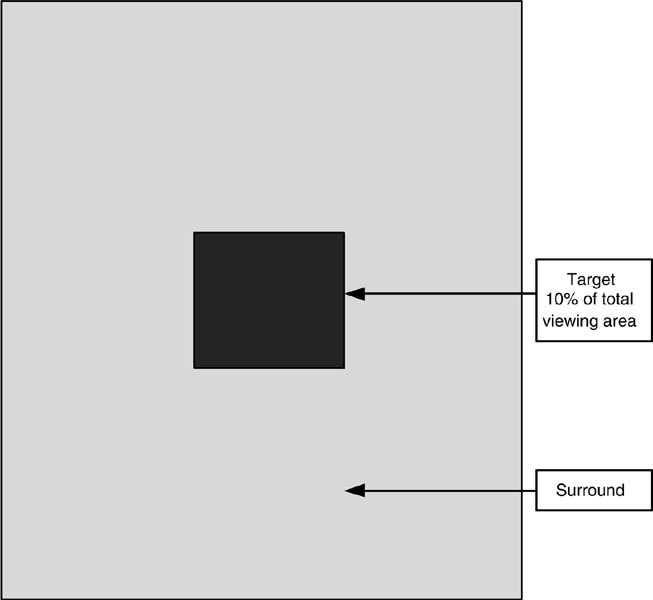
Stages in the evolution of medical image interpretation.
As radiologists and PACS vendors became more experienced with soft-copy interpretation, a number of workflow enhancements were incorporated into the next stage, dynamic soft-copy. The radiologist could now became an active participant in the image interpretation process, with active use of a variety of workstation tools including window/level adjustment, magnification, zoom and pan, and linear/region of interest measurements. In addition, workflow was enhanced by the ability to quickly and efficiently display comparison studies using automated hanging protocols, directly review historical reports (from the PACS/RIS interface), and incorporate customized window/level presets. It was this stage in which the previously cited studies by Reiner et al.3, 10 and Pomerantz et al.11 demonstrated improved radiologist productivity and interpretation accuracy. Even though this strategy was an improvement over conventional film display/interpretation, it lacked many of the current advances in workstation functionality.
The fourth stage in the interpretation paradigm shifted from “frame” or “tile” mode display to “stacked” or “cine” display. This allowed radiologists to navigate rapidly through cross-sectional imaging data sets by sequentially displaying consecutive images in the form of a cine loop. This strategy offers several theoretical advantages over tile mode. Reading large image data sets (like multi-slice CT) require considerable eye and head movement, which is significantly reduced with stack imaging.15 Stack viewing also takes better advantage of the human visual system’s ability to detect motion or subtle change. Because stack viewing allows for viewers to maintain their gaze on a specific spatial location as images change, the three-dimensional relationship of various structures is better realized, when compared with tile mode, where gaze is shifted between images.16 This difference is best illustrated by the process of detecting pulmonary nodules on a chest CT. The ability to sequentially maintain a fixed gaze allows for the reader to better appreciate the course of the pulmonary vessels and to differentiate a vessel en face from a pulmonary nodule.
The next stage in the interpretation process is an advanced iteration of the stacked mode, which allows for synchronization of two or more individual “stacks.” This can take the form of linking two historical comparison studies or two or more individual sequences within a single exam. An example of synchronized stacking would be a magnetic resonance imaging (MRI) exam that has separate T1 and T2 weighted sequences in various planes. Synchronizing the axial T1 (pre-contrast), axial T1 (post-contrast), and axial T2 sequences allows the viewer to correlate comparable anatomic images (in the same plane) for the different techniques being employed. By adding the comparison study, extremely subtle differences can be detected that may otherwise be missed. Unfortunately, many existing PACS workstations have not optimally implemented this feature, thereby limiting radiologist workflow.
The sixth and seventh stages in the CT interpretation paradigm have not yet been incorporated into the radiology mainstream, but they are not far away. Computer processing tools are now available to rapidly reconstruct large volumetric data sets into 2-dimensional and 3-dimensional reconstructions. These multi-planar reconstructed images can be customized to the unique specifications of the individual user. Use of this technology could potentially obviate the need to review each axial image, thereby enhancing radiologist productivity and workflow. In the near future, multi-planar capabilities will become directly incorporated into existing PACS workstations, enabling radiologists to review and interpret images on a single “all inclusive” workstation. Four-dimensional reconstructions will also soon be available, along with complex image segmentation, texture and tone processing, and incorporation of computer-aided detection software. These segmentation templates will allow radiologists to review selected portions of the entire data set rapidly selecting out the specific organ systems or anatomy of interest. The volumetric data from a single multi-slice chest CT exam, for example, can be reviewed in parallel as a CT angiographic study (for detection of pulmonary embolus), CT bronchoscopy (for detection of endobronchial pathology), high-resolution exam (for the detection of interstitial lung disease), and a conventional screening study for cancer, using a computer-aided detection program for pulmonary nodule detection. At the same time, multi-modality overlays can be applied to enhance diagnostic accuracy. In the example of a multi-slice chest CT with a newly diagnosed pulmonary nodule, functional positron emission tomography (PET) data can be combined with the CT data set to produce physiologic information as to the likelihood of malignancy. With this combined technology, areas of pathology can be highlighted on the computer workstation with graphic presentation, displaying the statistical likelihood of malignancy.17
EDUCATION FOR USERS
Educational programs for training and workflow optimization have largely been the domain of the PACS vendor with additional peer-to-peer assistance. Radiologists, like other physician groups have different levels of computer literacy; depending on age, computer experience, and personality profile.18 Radiologist PACS educational programs have traditionally consisted of one-on-one, hands-on training with an applications specialist, who reviews basic workstation functions, reading worklists, and hanging protocols. After conclusion of this basic training program the radiologist must manage alone, with trouble-shooting available from the PACS administrator, a fellow radiologist, or a computer savvy technologist. This limited amount of training often results in stagnation; new skills to optimize workflow and interpretation accuracy cannot be learned easily by minimally trained PACS users. As new software applications are adopted, many radiologists are not given additional training to take advantage of the added functionality. This can result in growing frustration among end users, particularly as demands are increased, with increasing complexity and size of the data sets.
Development of new educational resources should be a high priority if the full functionality and potential of the technology is to be realized. Computer-based educational programs would be one strategy, which would allow users to train at a convenient time, and at a speed most comfortable to them. Educational software programs should be developed for users with different levels of computer skill and experience. At present, these software programs would have to be vendor-specific, but eventually generic programs could be implemented as industry-wide standards become adopted. Professional societies such as the Radiological Society of North America (RSNA) and the Society for Computer Applications in Radiology (SCAR) offer a number of on-line and on-site PACS-related educational programs.
For the existing group of radiologists trained in film-based operation, the concept of multi-planar and 3-D reconstructions can be daunting. Radiologist training for CT interpretation typically focuses on the axial plane, and this uni-planar approach places radiologists at a disadvantage when they try to interpret cross-sectional imaging studies in alternative planes and formats. Surgeons on the other hand, who operate in a 3-dimensional world, feel more comfortable reviewing imaging studies in three dimensions. Newer strategies for viewing volumetric data sets, such as volume rendering and augmented (virtual) reality, are totally within the comfort zone of surgeons, who often prefer them over the traditional axial plane for surgical planning. Virtual reality programs can be used to facilitate radiologist re-learning of imaging anatomy in three planes and to assist with the natural evolution of the interpretation process as we move into multi-planar volumetric navigation.
As new navigational devices are employed, such as video game controls and gloves, radiologists may be required to improve their dexterity and hand-eye coordination. This should be relatively easy for the next generation of radiologists, who have grown up playing video games. This “gaming” generation will undoubtedly become early adopters of these new navigational devices and help drive further innovation. The current computer mouse will give way to new “species” that will become integrated into the volumetric paradigm. These navigational devices will include devices such as the programmable gyroscopic “air mouse” which allows pre-programmed individual controls and also permits freedom from the traditional “mouse pad” by allowing users to navigate using input based on radiologist hand movements.
OPTIMIZING THE HUMAN–COMPUTER INTERFACE
The diagnostic interpretation of medical images is a complex task consisting of two distinct processes: perception and reasoning. Image perception is the process of recognizing unique patterns in the image, whereas reasoning evaluates the relationship between perceived patterns and potential diagnoses.19 These processes depend on a radiologist’s overall empirical knowledge, memory, intuition, and diligence. The ultimate synergy exists in combining the flexibility and common sense inherent to radiologists with the analytical, repetitive capabilities of a computer. It is interesting to note that the majority of radiology malpractice lawsuits are brought as a result of errors in perception20, 21 or judgment.22 Computers offer the potential to assist radiologists by deconstructing the complex processes in image perception and diagnostic reasoning into a series of well-defined tasks.19 In addition, computers can assist radiologists by reducing the “human weaknesses” of bias, fatigue, and inconsistency. Radiologists should use this computer-derived capability not only as an independent “reader,” but as an adjunct to their own analysis. By exploiting the inherent advantages of computers (processing speed, memory, consistency), radiologists can improve their own diagnostic accuracy in much the same way that chess master Gary Kasparov’s technique of improving his chess game by playing against the strongest computer programs. This “partnership” between radiologist and computer mandates the transition to a digital environment.
FUTURE CONSIDERATIONS
Although the future can never be accurately predicted, several trends can be extrapolated to provide a glimpse of things to come. The first and probably the most important trend is the development of industry-wide standards that convert hardware into an off-the-shelf, nonproprietary commodity. Standards provided by HL-7, Digital Imaging and Communication in Medicine (DICOM), and Integrating the Health Care Enterprise (IHE) have transformed the integration process, and change will continue as proprietary 3-D/multi-planar workstations become fully integrated components of the PACS workstation, allowing radiologists to interface with a single, multi-function computer for all interpretation needs. As reading and interpretation demands continue to grow, as imaging studies produce larger and more complex data sets, navigational tools will become embedded into the workstation to improve workflow.
In addition to gaming, the movie industry has provided us with a futuristic view of idealized image-display devices and functionality. In the movie Minority Report, Tom Cruise plays the role of a detective investigating crimes before they are actually committed. The mental images from a “Pre-cog” with the ability to see into the future were transformed into visual images, which in turn were displayed on a single large flat screen and manipulated by the user with a glove, similar to that used in virtual reality games. A radiologist of the future could, in effect, function in a similar fashion, displaying multiple images from a variety of imaging modalities devices onto a single large screen and navigating by means of a combination of hand gestures, eye movements, and voice commands. The data from these acquisition devices could be displayed, processed, and manipulated according to a complex set of rules customized to the preferences of the user. These display and manipulation profiles could be constantly updated based upon the computer’s observational analysis of user practice patterns over time, with an electronic “wizard” recommending new display, perception, and interpretation strategies based on stored data from a master database.
Database mining will take on greater importance as the already vast array of imaging and clinical data grows at exponential rates. The repository of data to be mined will come from structured radiology reports, correlative imaging studies, and the electronic medical record. Intelligent mining of these databases will allow for image processing and data extraction before the current volumetric data set is presented to the radiologist for interpretation and will drive the navigation process. Large computerized reference data sets, computer cuing, computer-assisted diagnosis, and other forms of artificial intelligence will assist the radiologist in the interpretation process. The human–computer interface will be redefined as the burgeoning field of decision support provides radiologists with a wide array of software tools to improve productivity, interpretation accuracy, and diagnostic confidence.
CONCLUSIONS
When everything is said and done, the transition from film-based to filmless imaging is a foregone conclusion. The practice of diagnostic radiology must not only convert to filmless interpretation, radiologists must also become active participants in the evolutionary process already underway. If we elect to ignore these inevitable changes in technology and its applications, we risk being marginalized by our peers and the community we serve. Future applications of imaging technologies will be driven in large part by research in the area of medical imaging informatics. It is imperative that radiologists embrace research and educational opportunities now if their importance within the medical community is to be fully realized. The only constant in technology is change, and we must be willing to embrace the evolutionary forces already in place.
References
- 1.Sunshine JH, Lewis RS, Schepps B, et al. Data from a professional society placement service as a measure of the employment market for physicians. Radiology. 2002;224:193–198. doi: 10.1148/radiol.2241011150. [DOI] [PubMed] [Google Scholar]
- 2.Bhargavan M, Sunshine JH, Schepps B. Too few radiologists? AJR Am J Roentgenol. 2002;178:1075–1082. doi: 10.2214/ajr.178.5.1781075. [DOI] [PubMed] [Google Scholar]
- 3.Reiner BI, Siegel EL, Hooper FJ, et al. Radiologists’ productivity in the interpretation of CT scans: a comparison of PACS with conventional film. AJR Am J Roentgenol. 2002;176:861–864. doi: 10.2214/ajr.176.4.1760861. [DOI] [PubMed] [Google Scholar]
- 4.Reiner BI, Siegel EL. The cutting edge: strategies to enhance radiologist workflow in a filmless/paperless imaging department. J Digit Imaging. 2002;15:178–190. doi: 10.1007/s10278-002-0029-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gay SB, Sobel AH, Young LQ, et al. Processes involved in reading imaging studies: workflow analysis and implications for workstation development. J Digit Imaging. 1997;10:40–45. doi: 10.1007/BF03168549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reiner B, Siegel E, Protopapas Z, et al. Impact of filmless radiology on the frequency of clinician consultations with radiologists. AJR Am J Roentgenol. 1999;173:1169–1172. doi: 10.2214/ajr.173.5.10541082. [DOI] [PubMed] [Google Scholar]
- 7.Reiner B, Siegel E, Scanlon M. Changes in technologist productivity with implementation of an enterprise-wide PACS. J Digit Imaging. 2002;15:22–26. doi: 10.1007/s10278-002-0999-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reiner BI, Siegel EL, Carrino JA, et al. SCAR radiologic technologist survey: analysis of the impact of digital technologies on productivity. J Digit Imaging. 2002;15:132–140. doi: 10.1007/s10278-002-0021-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reiner BI, Siegel EL. Technologists’ productivity when using PACS: comparison of film-based versus filmless radiography. AJR Am J Roentgenol. 2002;179:33–37. doi: 10.2214/ajr.179.1.1790033. [DOI] [PubMed] [Google Scholar]
- 10.Reiner BI, Siegel EL, Hooper FJ. Accuracy of interpretation of CT scans: comparing PACS monitor displays and hard-copy images. AJR Am J Roentgenol. 2002;179:1407–1410. doi: 10.2214/ajr.179.6.1791407. [DOI] [PubMed] [Google Scholar]
- 11.Pomerantz SM, White CS, Krebs TL, et al. Liver and bone window settings for soft-copy interpretation of chest and abdominal CT. AJR Am J Roentgenol. 2000;174:311–314. doi: 10.2214/ajr.174.2.1740311. [DOI] [PubMed] [Google Scholar]
- 12.Siegel EL, Diaconis JN, Pomerantz S, et al. Making filmless radiology work. J Digit Imaging. 1995;8:151–155. doi: 10.1007/BF03168713. [DOI] [PubMed] [Google Scholar]
- 13.Reiner BI, Siegel EL, Hooper F, et al. Impact of filmless imaging on the frequency of clinician review of radiology images. J Digit Imaging. 1998;11:149–150. doi: 10.1007/BF03168288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reiner B, Siegel E, Flagle C, et al. Impact of filmless imaging on utilization of radiology services. Radiology. 2000;215:163–167. doi: 10.1148/radiology.215.1.r00ap41163. [DOI] [PubMed] [Google Scholar]
- 15.Beard DV, Hemminger BM, Denelsbeck KM, et al. How many screens does a CT workstation need? J Digit Imaging. 1994;7:69–76. doi: 10.1007/BF03168425. [DOI] [PubMed] [Google Scholar]
- 16.Mathie AG, Strickland NH. Interpretation of CT scans with PACS image display in stack mode. Radiology. 1997;202:709–711. doi: 10.1148/radiology.203.1.9122394. [DOI] [PubMed] [Google Scholar]
- 17.Reiner BI, Siegel EL, Shastri K. The future of radiology reporting. In: Reiner BI, Siegel EL, Weiss DL, editors. Electronic Reporting in the Digital Medical Enterprise. Great Falls, VA: Society for Computer Applications in Radiology; 2003. pp. 83–104. [Google Scholar]
- 18.Reiner B, Siegel E. Psychological factors affecting the adoption of PACS. Appl Radiol. 2002;31:.–.. [Google Scholar]
- 19.Tourassi GD. Journey toward computer-aided diagnosis: role of texture analysis. Radiology. 1999;213:317–320. doi: 10.1148/radiology.213.2.r99nv49317. [DOI] [PubMed] [Google Scholar]
- 20.Berlin L. Malpractice issues in radiology: perceptual errors. AJR Am J Roentgenol. 1996;167:587–590. doi: 10.2214/ajr.167.3.8751657. [DOI] [PubMed] [Google Scholar]
- 21.Berlin L, Hendrix RW. Malpractice issues in radiology: perceptual errors and negligence. AJR Am J Roentgenol. 1998;170:863–867. doi: 10.2214/ajr.170.4.9530024. [DOI] [PubMed] [Google Scholar]
- 22.Berlin L. Errors in judgment. AJR Am J Roentgenol. 1996;166:1259–1261. doi: 10.2214/ajr.166.6.8633426. [DOI] [PubMed] [Google Scholar]


