Abstract
Objective
To examine the effectiveness of the health system response to the challenge of diabetes across different settings and explore the inequalities in diabetes care that are attributable to socioeconomic factors.
Methods
We used nationally representative health examination surveys from Colombia, England, the Islamic Republic of Iran, Mexico, Scotland, Thailand and the United States of America to obtain data on diagnosis, treatment and control of hyperglycaemia, arterial hypertension and hypercholesterolaemia among individuals with diabetes. Using logistic regression, we explored the socioeconomic determinants of diagnosis and effective case management.
Findings
A substantial proportion of individuals with diabetes remain undiagnosed and untreated, both in developed and developing countries. The figures range from 24% of the women in Scotland and the USA to 62% of the men in Thailand. The proportion of individuals with diabetes reaching treatment targets for blood glucose, arterial blood pressure and serum cholesterol was very low, ranging from 1% of male patients in Mexico to about 12% in the United States. Income and education were not found to be significantly related to the rates of diagnosis and treatment anywhere except in Thailand, but in the three countries with available data insurance status was a strong predictor of diagnosis and effective management, especially in the United States.
Conclusion
There are many missed opportunities to reduce the burden of diabetes through improved control of blood glucose levels and improved diagnosis and treatment of arterial hypertension and hypercholesterolaemia. While no large socioeconomic inequalities were noted in the management of individuals with diabetes, financial access to care was a strong predictor of diagnosis and management.
Résumé
Objectif
Étudier l'efficacité de la réponse du système de santé au problème du diabète sur différents paramètres et explorer les inégalités dans la prise en charge du diabète, attribuables à des facteurs socio-économiques.
Méthodes
Nous avons utilisé des enquêtes de santé par examen représentatives au plan national pour la Colombie, l'Angleterre, la République islamique d'Iran, le Mexique, l'Écosse, la Thaïlande et les États-Unis d'Amérique. Les données exploitées portent sur le diagnostic, le traitement et le contrôle de l'hyperglycémie, de l'hypertension artérielle et de l’hypercholestérolémie chez les diabétiques. Nous avons utilisé la régression logistique pour explorer les déterminants socioéconomiques du diagnostic et de la bonne gestion thérapeutique.
Résultats
Une proportion substantielle des diabétiques n’a pas fait l’objet d’un diagnostic et ne reçoit par conséquent aucun traitement et ce, à la fois dans les pays développés et dans les pays en voie de développement. Les chiffres vont de 24% des femmes en Écosse et aux États-Unis d’Amérique à 62% des hommes en Thaïlande. La proportion de diabétiques atteignant les cibles de traitement pour la glycémie, la tension artérielle et le cholestérol sérique était très faible: de 1% des patients masculins au Mexique jusqu'à environ 12% aux États-Unis. Il n’a pas été constaté que le revenu et l'éducation aient un lien significatif avec les taux de diagnostic et de traitement sauf en Thaïlande. Toutefois, pour les trois pays pour lesquels nous disposions de données, la couverture sociale était un puissant indicateur de diagnostic et de traitement efficace, particulièrement aux États-Unis.
Conclusion
Il existe de nombreuses occasions manquées de réduction du fardeau du diabète au moyen d'un contrôle renforcé des taux de glycémie et d'un diagnostic et d'un traitement meilleurs de l'hypertension artérielle et de l'hypercholestérolémie. Alors qu'aucune inégalité socioéconomique importante n'a été relevée dans le traitement des diabétiques, le coût de l'accès aux soins s'est révélé être un puissant indicateur de diagnostic et de traitement.
Resumen
Objetivo
Examinar la efectividad de la respuesta del sistema sanitario ante el reto de la diabetes en diversos entornos y observar las desigualdades atribuibles a factores socioeconómicos en el tratamiento de la diabetes.
Métodos
Hemos empleado las encuestas representativas a nivel nacional de los exámenes médicos de Colombia, Escocia, Estados Unidos, Inglaterra, México, la República Islámica de Irán y Tailandia para obtener datos sobre el diagnóstico, el tratamiento y el control de la hiperglucemia, la hipertensión arterial y la hipercolesterolemia en pacientes con diabetes. Empleando una regresión logística, hemos analizado los determinantes socioeconómicos del diagnóstico y de un tratamiento efectivo de cada caso.
Resultados
Un proporción considerable de pacientes con diabetes permanecen sin diagnosticar y sin tratar, tanto en los países desarrollados como en aquellos en vías de desarrollo. Las cifras oscilan desde un 24% de las mujeres en Escocia y Estados Unidos hasta un 62% de los hombres en Tailandia. Solo una proporción muy reducida de personas con diabetes (oscilando entre el 1% de los pacientes hombres en México y alrededor del 12% en Estados Unidos) alcanzó los objetivos de su tratamiento para sus problemas de glucosa en sangre, presión arterial y nivel sérico de colesterol. En ninguna de las regiones (excepto Tailandia) se observó que los porcentajes de diagnóstico y tratamiento estuvieran relacionados con los ingresos y la educación, si bien en tres países con datos disponibles contar con un seguro representó un factor importante de previsibilidad para el diagnóstico y tratamiento efectivo de la diabetes, especialmente en el caso de Estados Unidos.
Conclusión
Se han dejado pasar muchas oportunidades para reducir la carga de la diabetes a través de un mejor control de los niveles de glucosa en sangre y de un mejor diagnóstico y tratamiento de la hipertensión arterial y de la hipercolesterolemia. Si bien no se observaron grandes desigualdades socioeconómicas en el tratamiento de los pacientes con diabetes, el acceso económico al tratamiento fue un factor importante de previsibilidad para el diagnóstico y el tratamiento de esta enfermedad.
ملخص
الغرض: فحص فعالية تصدي النظام الصحي لتحدي السكري في مواقع مختلفة واستكشاف عدم المساواة في رعاية السكري التي تُعزَى إلى عوامل اجتماعية واقتصادية.
الطريقة: استخدم الباحثون مسوحات وطنية لفحص الصحة من كل من كمبوديا، وانكلترا، وجمهورية إيران الإسلامية، والمكسيك، وسكوتلاندا، وتايلاند، والولايات المتحدة الأمريكية لجمع معطيات تشخيص، ومعالجة، وتضبيط فرط سكر الدم، وفرط الضغط الشرياني، وفرط كوليستيرول الدم بين المصابين بالسكري. واستكشف الباحثون، باستخدام التحوّف اللوجستي، المحددات الاجتماعية-الاقتصادية للتشخيص والتدبير العلاجي الفعّال للحالات.
النتائج: لم تُشخَّص ولم تعالج نسبة كبيرة من المصابين بالسكري، في كل من البلدان المتقدمة والنامية. وتراوحت هذه النسبة من24% بين النساء في سكوتلاندا والولايات المتحدة الأمريكية إلى% 62 بين الرجال في تايلاند. وكانت نسبة المصابين بالسكري الذين بلغوا مرامي معالجة غلوكوز الدم، وضغط الدم الشرياني، والكوليستيرول المصلي نسبة منخفضة للغاية، تراوحت بين% 1 من الذكور في المكسيك إلى % 12 في الولايات المتحدة. لم يُلاحَظ للدخل والتعليم علاقة يعتد بها إحصائياً مع معدلات التشخيص والمعالجة في أي مكان ماعدا تايلاند، وكانت حالة التأمين، في ثلاثة بلدان توفرت فيها المعطيات، منبئاً قوياً على التشخيص وفعالية التدبير العلاجي، ولاسيما في الولايات المتحدة.
الاستنتاج: كثير من الفرص المفقودة يمكن الاستفادة منها للحد من عبء السكري عن طريق تحسين تضبيط مستويات غلوكوز الدم، وتحسين تشخيص ومعالجة فرط الضغط الشرياني وفرط كوليستيرول الدم. ومع أنه لم يُلاحَظ في التدبير العلاجي للمصابين بالسكري قدر كبير من عدم المساواة الاقتصادية والاجتماعية، إلا أن القدرة المالية على الوصول إلى خدمات الرعاية كانت منبئاً قوياً على التشخيص والتدبير العلاجي.
Резюме
Цель
Рассмотреть эффективность реакции системы здравоохранения на проблему диабета в различных условиях и исследовать неравенство в области медико-санитарной помощи при диабете, обусловленное социально-экономическими факторами.
Методы
Для получения данных о диагностике, лечении и контроле гипергликемии, артериальной гипертензии и повышенного уровня холестерина среди больных диабетом мы использовали данные национально-репрезентативных опросов по изучению состояния здоровья, проводившихся в Англии, Исламской Республике Иран, Колумбии, Мексике, Соединенных Штатах Америки, Таиланде и Шотландии. Используя логистическую регрессию, мы исследовали социально-экономические детерминанты диагностики и эффективного лечения больных.
Результаты
Как в развитых, так и в развивающихся странах у значительной доли больных диабет не диагностируется, и они не получают лечения. Цифры варьируют от 24% женщин в Шотландии до 62% мужчин в Таиланде. Доля больных диабетом, достигающих целей лечения в отношении содержания глюкозы в крови, артериального кровяного давления и сывороточного холестерина, была очень низкой и ранжировала от 1% пациентов-мужчин в Мексике до примерно 12% в США. Нигде, за исключением Таиланда, не было выявлено существенной корреляции между доходом, образованием и показателями диагностирования и лечения. Однако в трех странах, данные по которым были доступны, особенно в США, сильным предиктором диагностирования и эффективного ведения диабета являлся страховой статус.
Вывод
Существует много неиспользованных возможностей для снижения бремени заболеваемости диабетом путем улучшения контроля над уровнем содержания глюкозы в крови, а также совершенствования диагностики и лечения артериальной гипертензии и повышенного уровня холестерина. Хотя значительного социально-экономического неравенства в ведении больных диабетом отмечено не было, финансовая доступность медико-санитарной помощи являлась сильным предиктором диагностики и эффективного лечения болезни.
摘要
目的
旨在考察不同环境下的医疗体系应对糖尿病挑战的有效性,并探讨因社会经济因素引起的糖尿病护理中的不平等现象。
方法
我们运用哥伦比亚、英格兰、伊朗、墨西哥、苏格兰、泰国和美国的全国代表性体检调查结果,从中获得糖尿病患者在诊断、治疗和高血糖、动脉高血压和高胆固醇血症的控制方面的数据。使用逻辑回归分析探讨了诊断和病例有效管理的社会经济因素。
结果
无论是在发达国家还是在发展中国家,有相当比例的糖尿病患者仍然未经诊断和治疗。这方面数字在24%(苏格兰和美国女性)到62%(泰国男性)之间变化。实现血糖、动脉血压和胆固醇治疗目标的糖尿病患者的比例非常低,仅占1%(墨西哥男性)到约12%(美国)。除泰国外,未发现收入和教育程度与诊断和治疗比例显著相关。然而,在有可用数据的三个国家,特别是在美国,保险状况是实现糖尿病诊断和有效管理的一个强大的预警器。
结论
人们错过了很多通过更好地控制血糖水平、更早地诊断和治疗动脉高血压和高胆固醇血症来减轻糖尿病负担的机会。尽管在糖尿病患者的管理中并未发现重大经济社会不公现象,但是,具备享受医疗服务的经济能力仍是实现糖尿病诊断和有效管理的一个强大预警器。
Introduction
The estimated global prevalence of diabetes is around 6.4% and more than 280 million people in the world have diabetes. Of those affected, the majority live in the developing world.1 Projections for 2010 were that diabetes would account for almost 4 million deaths worldwide.2 The burden of diabetes will only continue to grow, since the number of adults with diabetes in developing countries is projected to rise by more than two-thirds between 2010 and 2030.1 Previous studies have documented significant deficits in the management of individuals with diabetes.3–8
Five strategies can help reduce the burden of diabetes at the population level: (i) case prevention through reductions in modifiable risk factors such as obesity; (ii) screening coupled with pharmacological or lifestyle interventions targeting individuals with pre-diabetes;9,10 (iii) improved diagnosis and control of blood glucose among individuals with diabetes;11–13 (iv) improved management of microvascular complications, including renal disease, retinopathy, diabetic foot and other neuropathies;14,15 and (v) improved management of associated cardiovascular risks.13,16 It is essential to understand how well health systems are performing in terms of these five strategies and the role of health system and individual attributes such as physical access, financial access, provider quality and patient education and motivation.
While diabetes care under specific providers is extensively examined in the literature,17–19 there is only one previous comparative analysis of how health systems overall are responding to diabetes.7 In this paper we expand the range of comparisons by analysing in a consistent way surveys conducted in three developed and four developing settings. We focus the analysis on the two strategies for which data are available: (i) diagnosis and control of blood glucose, and (ii) the management of arterial blood pressure and serum cholesterol in individuals with diabetes. We explore the relationship between socioeconomic status, financial access to diabetes care and place of residence with effective management of diabetes.
Methods
Our selection of countries was opportunistic. We searched extensively for nationally representative health examination surveys that included measurements of fasting plasma glucose or glycosylated haemoglobin or haemoglobin A1c (HbA1c) as well as arterial blood pressure and serum cholesterol. We downloaded publicly available data sets from England, Scotland and the United States of America. For other countries we requested data and collaboration on this project from the institution that conducted the survey and were able to include surveys from Colombia, the Islamic Republic of Iran, Mexico and Thailand. Table 1 presents the characteristics of each survey. For all surveys except the one conducted in the Islamic Republic of Iran, sampling weights were available and were taken into account in the analysis.
Table 1. Sample information for nationally representative surveys used to study the management of diabetes and associated cardiovascular risk factors in seven countries.
| Sample characteristic | Colombia20 | England21 | Islamic Republic of Iran22 | Mexico23 | Scotland24 | Thailand3 | United States25 |
|---|---|---|---|---|---|---|---|
| Survey year(s) | 2007 | 2003 | 2004 | 2006 | 2003 | 2004 | 2003–06 |
| Overall sample size | 41 833 | 18 553 | 89 400 | 45 446 | 8148 | 39 290 | 20 470 |
| Ages (in years) included in analysis | 35–64 | 35+ | 35–64 | 35+ | 35+ | 35+ | 35+ |
| Method used to diagnose diabetes | FPG | HbA1c | FPG | FPG | HbA1c | FPG | HbA1c |
| No. in sample within age group of analysis | 7284 | 10 890 | 49 695 | 30 602 | 4438 | 33 058 | 7142 |
| No. in sample with some physical measurement | 7035 | 6434 | 37 784 | 3856 | 3397 | 31 203 | 6460 |
| No. of individuals with diabetes | 349 | 363 | 4068 | 720 | 186 | 4145 | 1018 |
| Diabetic individuals with measured arterial blood pressure | 322 | 305 | 4050 | 699 | 158 | 4131 | 911 |
| Diabetic individuals with measured serum cholesterol | 345 | 242 | 4011 | 648 | 125 | 4123 | 785 |
| Diabetic individuals with measured blood glucose, blood pressure and serum cholesterol | 319 | 208 | 3993 | 630 | 103 | 4109 | 716 |
FPG, fasting plasma glucose; HbA1c, glycosylated haemoglobin.
Table 2 summarizes the definitions, diagnostic parameters and treatment targets for all the conditions under study. We followed the International Diabetes Federation (IDF) guidelines26 for diagnosis and treatment values in all cases except for serum cholesterol, for which we used the guidelines of the National Institute for Health and Clinical Excellence (NICE).27 Individuals with diabetes were categorized into four mutually exclusive groups: (i) undiagnosed, (ii) diagnosed but untreated, (iii) treated but not controlled (not meeting treatment targets), and (iv) treated and controlled (meeting treatment targets) for blood glucose, blood pressure and serum cholesterol. Our analysis was limited to medical treatment as lifestyle interventions, such as dietary changes, are not measured consistently in the household surveys.
Table 2. Definitions of categories used in the analysis in seven-country study of the management of diabetes and associated cardiovascular risk factors.
| Condition | Status | Definition |
|---|---|---|
| Diabetes (self-reported diagnosis or HbA1c ≥ 6.5% or FPG ≥ 126 mg/dl) | Undiagnosed | No self-reported diagnosis of diabetes and HbA1c ≥ 6.5% (FPG ≥ 126 mg/dl) |
| Diagnosed and untreated | Self-reported diagnosis of diabetes and no self-reported current use of medication for diabetes and HbA1c ≥ 6.5% (FPG ≥ 126 mg/dl) | |
| Diagnosed, treated, uncontrolled | Self-reported diagnosis of diabetes and self-reported current use of medication for diabetes and HbA1c ≥ 6.5% (FPG ≥ 126 mg/dl) | |
| Diagnosed, treated, controlled | Self-reported diagnosis of diabetes and self-reported current use of medication for diabetes and HbA1c < 6.5% (FPG < 126 mg/dl) | |
| Hypertension (Self-reported diagnosis or SBP ≥ 130 mmHg) | Undiagnosed | No self-reported diagnosis of hypertension and systolic blood pressure ≥ 130 mmHg |
| Diagnosed and untreated | Self-reported diagnosis of hypertension and no self-reported current use of medication for hypertension and systolic blood pressure ≥ 130 mmHg | |
| Diagnosed, treated, uncontrolled | Self-reported diagnosis of hypertension and self-reported current use of medication for hypertension and systolic blood pressure ≥ 130 mmHg | |
| Diagnosed, treated, controlled | Self-reported diagnosis of hypertension and self-reported current use of medication for hypertension and systolic blood pressure < 130 mmHg | |
| Serum cholesterol (self-reported diagnosis or total cholesterol ≥ 5.0 mmol/l) | Undiagnosed | No self-reported diagnosis of hypercholesterolaemia and total serum cholesterol ≥ 5.0 mmol/l |
| Diagnosed and untreated | Self-reported diagnosis of hypercholesterolaemia and no self-reported current use of medication for hypercholesterolaemia and total serum cholesterol ≥ 5.0 mmol/l | |
| Diagnosed, treated, uncontrolled | Self-reported diagnosis of hypercholesterolaemia and self-reported current use of medication for hypercholesterolaemia and total serum cholesterol ≥ 5.0 mmol/l | |
| Diagnosed, treated, controlled | Self-reported diagnosis of hypercholesterolaemia and self-reported current use of medication for hypercholesterolaemia and total serum cholesterol < 5.0 mmol/l | |
| Diagnosed, uncontrolleda | Self-reported diagnosis of hypercholesterolaemia and total serum cholesterol ≥ 5.0 mmol/l; medication use unknown | |
| Diagnosed, controlleda | Self-reported diagnosis of hypercholesterolaemia and total serum cholesterol < 5.0 mmol/l; medication use unknown | |
| Management status unknownb | Total serum cholesterol ≥ 5.0 mmol/l; diagnosis status and medication use unknown | |
| Comprehensive management | Undiagnosed or untreated for one or more conditions | Individual has diabetes and is either “undiagnosed” or “diagnosed and untreated” for diabetes, hypercholesterolaemia, or hypertension |
| Ineffective management of one or more conditions | Individual has diabetes and is currently taking all necessary medication, but “diagnosed, treated, and uncontrolled” for one or more condition | |
| Effective management of all conditions | Individual has diabetes and is “diagnosed, treated and controlled” for all existing conditions |
FPG, fasting plasma glucose; HbA1c, glycosylated haemoglobin; mg/dl, milligrams per decilitre; mmHg, millilitres of mercury; mmol/l, millimoles per litre; SBP, systolic blood pressure.
a Colombia only.
b Islamic Republic of Iran only.
Analysis of determinants
We used logistic regression to explore the determinants of being diagnosed, treated and controlled among individuals with diabetes, separately for each survey. We examined the determinants of having been previously diagnosed by a physician and, among those previously diagnosed, we explored the determinants of having been effectively treated for all identified conditions. We also performed a regression to identify the determinants of meeting treatment targets for blood glucose (Appendix A, available at: http://www.healthmetricsandevaluation.org/files/2010/diabetes_comparative_analysis/Webappendix_1.pdf). We controlled for the following determinants: age and sex of the respondent, urban or rural residence, income or wealth quintile, insurance status, and educational level. For Colombia and Mexico we created a household wealth index and divided households into quintiles. For Thailand and the United States, the surveys included information on self-reported income and we divided individuals into income quintiles. In the Islamic Republic of Iran, the survey questionnaire did not include information on income or assets.
In the United States, the survey enquired whether the respondent had or did not have insurance. For Mexico we used three insurance status categories: (i) uninsured, (ii) insured through the informal sector (Seguro Popular), and (iii) insured through the formal or private sector. For Colombia we used three categories: (i) uninsured, (ii) insured through the informal sector (régimen subsidiado), and (iii) insured through the formal sector (régimen contributivo) or through a special social security fund for the military, the police, teachers and public oil company employees (régimen especial). Insurance status was not available in the Islamic Republic of Iran or Thailand.
All analyses were run using STATA version 11 (StataCorp. LP, College Station, USA).
Results
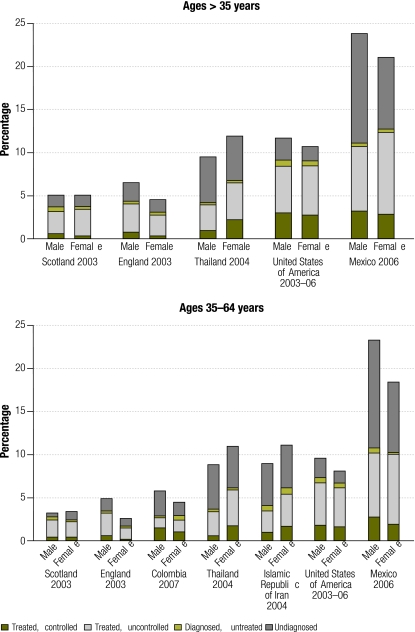
Fig. 1 shows the age-standardized prevalence and rates of diagnosis of diabetes and the rates of treatment and effective control of blood glucose. Mexico stands out for its high prevalence of the disease, with 24% of males and 21% of females over the age of 35 years having diabetes.23 England and Scotland appear to have the lowest prevalence rates. Prevalence is higher among males in Colombia, England, Mexico and the United States, and among women in the Islamic Republic of Iran and Thailand (Appendix B, available at: http://www.healthmetricsandevaluation.org/files/2010/diabetes_comparative_analysis/Webappendix_1.pdf).
Fig. 1.
Prevalence, diagnosis and treatment rates for diabetesa among adults in seven-country study of the management of diabetes and associated cardiovascular risk factors
a Individuals with diabetes are assigned to one of four groups: (i) undiagnosed, (ii) diagnosed but not on treatment, (iii) diagnosed, on treatment but not meeting treatment targets, and (iv) diagnosed, on treatment and meeting treatment targets. The overall height of the bars represents the diabetes prevalence in that population.
Fig. 1 also shows the proportion of individuals who had diabetes but remained undiagnosed at the time of the survey. Diagnosis rates were higher for women than men, with the largest sex differential seen in Colombia. Appendix C (available at: http://www.healthmetricsandevaluation.org/files/2010/diabetes_comparative_analysis/Webappendix_1.pdf) shows the same results expressed in terms of the proportion of individuals with diabetes. Coverage of treatment with medication for control of blood glucose is higher in developed countries, but low overall, especially in younger people (Fig. 1). The highest treatment rates were found in the United States. In Colombia, the Islamic Republic of Iran and Thailand the majority of individuals with diabetes were not using medication for blood glucose control. The highest proportion of diagnosed but untreated individuals was found among Colombian women, at 12%.
In all surveys only a small fraction of individuals with diabetes met treatment targets. The United States was the best performer, with about 26% of individuals with diabetes meeting treatment targets. In Colombia, 27% of men and 24% of women were meeting the targets, while England and Scotland were among the worst performers. While the proportion of diabetic individuals who were on treatment was low in Colombia, that country appeared to be more effective than others at reaching treatment targets.
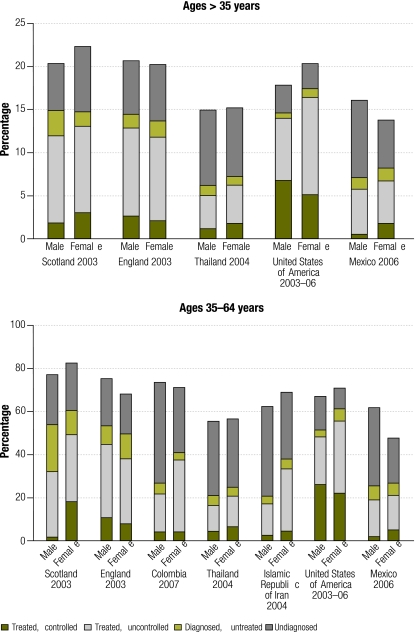
Fig. 2 shows the prevalence of arterial hypertension and the rates of diagnosis, treatment and control among individuals with diabetes. The prevalence of arterial hypertension was high in all surveys but was highest among Scottish women and lowest among Mexican women. The rate of diagnosis was distinctly higher in England, Scotland and the United States than in Colombia, the Islamic Republic of Iran, Thailand or Mexico, countries where more than half of men with diabetes and arterial hypertension had never been diagnosed.
Fig. 2.
Prevalence, diagnosis and treatment rates for arterial hypertensiona among adults in seven-country study of the management of diabetes and associated cardiovascular risk factors
a Individuals with arterial hypertension are assigned to one of four groups: (i) undiagnosed, (ii) diagnosed but not on treatment, (iii) diagnosed, on treatment but not meeting treatment targets, and (iv) diagnosed, on treatment and meeting treatment targets. The total height of the bars represents the prevalence of arterial hypertension in individuals with diabetes.
Treatment rates for arterial hypertension followed a similar pattern and were higher in the more developed countries. The highest proportion of individuals with diabetes and hypertension who were meeting treatment targets for hypertension was seen in the United States (38% for men and 25% for women), while in all other surveys fewer than 15% of individuals with diabetes were meeting treatment targets for blood pressure.
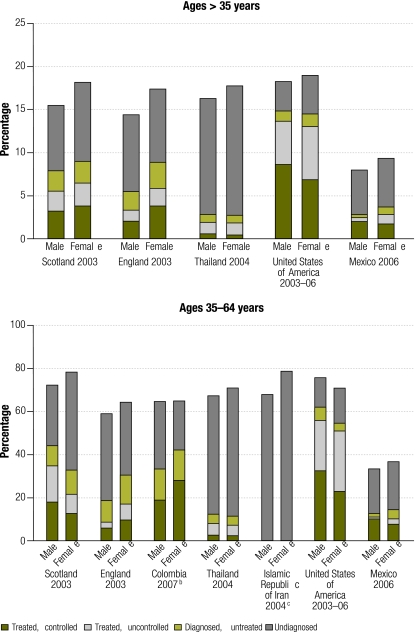
The prevalence of hypercholesterolaemia among individuals with diabetes was similarly high; it was above 55% in all surveys except in Mexico, where it was only about 35% (Fig. 3). Rates of diagnosis are very low in all surveys except the one in the United States. Diagnostic rates in Thailand were below one-fourth the rate observed in the United States, even though both countries had a similar prevalence of diabetes. Countries had a lower proportion of diabetic individuals on treatment for the control of serum cholesterol than for blood pressure or blood glucose control, but of those receiving treatment for hypercholesterolaemia, higher proportions were meeting treatment targets when compared to those on treatment for hyperglycaemia or hypertension.
Fig. 3.
Prevalence, diagnosis and treatment rates for hypercholesterolaemiaa among adults in seven-country study of the management of diabetes and associated cardiovascular risk factors
a Individuals with hypercholesterolaemia are assigned to one of four groups: (i) undiagnosed, (ii) diagnosed but not on treatment, (iii) diagnosed and on treatment but not meeting treatment targets, and (iv) diagnosed, on treatment and meeting treatment targets. The total height of the bars represents the prevalence of hypercholesterolaemia in individuals with diabetes.
b No information on current use of cholesterol-lowering medication was available for Colombia. The bars reflect whether individuals are diagnosed and whether they are meeting treatment targets.
c No information on previous diagnosis or current use of cholesterol-lowering medication was available for the Islamic Republic of Iran. The height of the bar represents the prevalence of hypercholesterolaemia among individuals with diabetes.
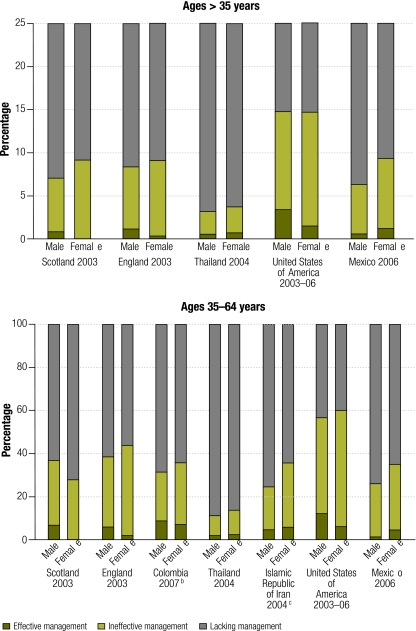
Fig. 4 depicts how well countries perform overall in managing individuals with diabetes. Effective management was defined in terms of the proportion of individuals with diabetes who were receiving the treatment they required and who were meeting treatment targets for blood glucose, blood pressure and serum cholesterol. Across all surveys, only a small proportion of individuals with diabetes had achieved treatment targets for all three conditions. Within this set of surveys, the United States had the highest rates of effective management, at 13% for men and 6% for women. Ineffective management was assessed in terms of the proportion of individuals who were receiving required treatment for all the conditions they had but who were not meeting treatment targets. A striking finding, shown in Fig. 4, was the enormous proportion of individuals with diabetes who were undiagnosed or who had been diagnosed but were not being treated for hyperglycaemia, arterial hypertension or hypercholesterolaemia, individually or in combination. It was highest in Thailand, where 88% of men and 85% of women were lacking management, largely on account of the low rates of diagnosis of hypercholesterolaemia. The United States had the lowest proportion of individuals who were not being managed, but even there more than 40% of men and women with diabetes were undiagnosed or had been diagnosed but were not being treated for one or more conditions. There is substantial room for improvement in the management of diabetes and its associated cardiovascular risks.
Fig. 4.
Comprehensive managementa of blood glucose, arterial hypertension and hypercholesterolaemia among adults with diabetes in seven-country study of the management of diabetes and associated cardiovascular risk factors
a Effective management refers to individuals with diabetes who are diagnosed, treated and controlled for all existing conditions. Ineffective management of one or more conditions refers to individuals with diabetes who are currently taking all necessary medication but are not meeting treatment targets for one or more condition. Lacking management refers to individuals with diabetes who are either undiagnosed or diagnosed but untreated for diabetes, arterial hypertension or hypercholesterolaemia.
b No information on current use of cholesterol-lowering medication was available for Colombia. Comprehensive management has been estimated for blood glucose and blood pressure only.
c No information on previous diagnosis or current use of cholesterol-lowering medication was available for the Islamic Republic of Iran. Comprehensive management has been estimated for blood glucose and blood pressure only.
Surprisingly, wealth was not significantly associated with the probability of being diagnosed with diabetes (Table 3) anywhere except in Thailand, where the poorest quintile had significantly lower odds of being diagnosed than the richest quintile. In Thailand, individuals with a higher educational level also had significantly higher odds of being diagnosed. In the Islamic Republic of Iran and Thailand, living in an urban location was associated with significantly higher odds of being diagnosed than living in a rural location, but it was not a significant determinant in other surveys. In Colombia, Mexico and the United States, where data were available, insurance status was a strong and significant predictor of diagnosis.
Table 3. Probability of (i) being diagnosed with diabetes if diabetic, and of (ii) being treated and meeting treatment targets for blood glucose, blood pressure and serum cholesterol if previously diagnosed as diabetic in seven-country study of the management of diabetes and associated cardiovascular risk factors.
| Determinant | Colombia |
England |
Islamic Republic of Iran |
Mexico |
Scotland |
Thailand |
United States |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | P | OR | P | OR | P | OR | P | OR | P | OR | P | OR | P | |||||||
| Probability of being diagnosed | ||||||||||||||||||||
| Age group (years) | ||||||||||||||||||||
| 35–44 | 0.29 | 0.000 | 0.80 | 0.627 | 0.55 | 0.000 | 0.36 | 0.000 | 3.00 | 0.344 | 0.35 | 0.000 | 0.73 | 0.328 | ||||||
| 45–54 | 0.86 | 0.631 | 0.99 | 0.981 | 0.82 | 0.007 | 0.75 | 0.178 | 1.04 | 0.954 | 0.63 | 0.000 | 0.78 | 0.344 | ||||||
| 55–64 | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | ||||||
| 65+ | – | – | 0.70 | 0.331 | – | – | 0.96 | 0.867 | 0.98 | 0.957 | 1.09 | 0.268 | 0.95 | 0.820 | ||||||
| Sex | ||||||||||||||||||||
| Male | 0.76 | 0.296 | 0.62 | 0.092 | 0.70 | 0.000 | 0.82 | 0.220 | 0.80 | 0.588 | 0.63 | 0.000 | 0.82 | 0.268 | ||||||
| Female | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | ||||||
| Residence | ||||||||||||||||||||
| Urban | 1.30 | 0.430 | 1.31 | 0.356 | 1.60 | 0.000 | 0.88 | 0.551 | 0.68 | 0.366 | 1.30 | 0.000 | – | – | ||||||
| Rural | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | – | – | ||||||
| Wealth quintile | ||||||||||||||||||||
| Poorest | 1.19 | 0.746 | 1.10 | 0.858 | – | – | 0.86 | 0.613 | 1.74 | 0.546 | 0.61 | 0.008 | 1.38 | 0.289 | ||||||
| Quintile 2 | 1.62 | 0.298 | 1.54 | 0.412 | – | – | 1.57 | 0.115 | 1.51 | 0.629 | 0.80 | 0.075 | 1.45 | 0.243 | ||||||
| Quintile 3 | 1.00 | 0.992 | 1.45 | 0.475 | – | – | 1.20 | 0.489 | 3.38 | 0.199 | 1.08 | 0.527 | 1.21 | 0.537 | ||||||
| Quintile 4 | 1.79 | 0.195 | 1.19 | 0.730 | – | – | 1.53 | 0.094 | 0.68 | 0.664 | 0.96 | 0.733 | 1.35 | 0.340 | ||||||
| Richest | 1.00 | – | 1.00 | – | – | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | ||||||
| Insurance statusa | ||||||||||||||||||||
| Insured A | 3.31 | 0.005 | – | – | – | – | 1.47 | 0.029 | – | – | – | – | 2.23 | 0.002 | ||||||
| Insured B | 1.62 | 0.232 | – | – | – | – | 1.74 | 0.027 | – | – | – | – | – | – | ||||||
| Uninsured | 1.00 | – | – | – | – | – | 1.00 | – | – | – | – | – | 1.00 | – | ||||||
| Educationb | ||||||||||||||||||||
| No education | 1.00 | – | – | – | 1.00 | – | 1.00 | – | – | – | 1.00 | – | – | – | ||||||
| Complete primary | 1.06 | 0.858 | 1.00 | – | 1.09 | 0.292 | 0.71 | 0.123 | 1.00 | – | 1.23 | 0.075 | 1.00 | – | ||||||
| Complete secondary | 0.99 | 0.987 | 1.37 | 0.428 | 0.94 | 0.597 | 0.52 | 0.018 | 0.66 | 0.390 | 1.39 | 0.039 | 0.82 | 0.391 | ||||||
| University | – | – | 1.41 | 0.546 | 0.75 | 0.012 | – | – | 4.18 | 0.119 | 1.51 | 0.028 | 0.76 | 0.204 | ||||||
|
Sample size |
297 |
283 |
4063 |
717 |
156 |
3706 |
988 |
|||||||||||||
| Probability of being effectively managed | ||||||||||||||||||||
| Age group (years) | ||||||||||||||||||||
| 35–44 | 0.68 | 0.471 | 0.62 | 0.429 | 0.86 | 0.311 | 2.09 | 0.073 | 0.40 | 0.364 | 0.80 | 0.345 | 1.66 | 0.212 | ||||||
| 45–54 | 0.96 | 0.914 | 0.61 | 0.428 | 0.85 | 0.112 | 0.99 | 0.986 | 0.06 | 0.043 | 0.72 | 0.049 | 1.13 | 0.691 | ||||||
| 55–64 | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | ||||||
| 65+ | – | – | 0.65 | 0.383 | – | – | 1.19 | 0.565 | 0.44 | 0.226 | 1.11 | 0.321 | 0.89 | 0.608 | ||||||
| Sex | ||||||||||||||||||||
| Male | 0.76 | 0.465 | 0.83 | 0.636 | 0.63 | 0.000 | 0.59 | 0.035 | 1.84 | 0.312 | 1.27 | 0.020 | 1.25 | 0.230 | ||||||
| Female | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | ||||||
| Residence type | ||||||||||||||||||||
| Urban | 0.73 | 0.509 | 1.27 | 0.579 | 0.93 | 0.487 | 1.42 | 0.263 | 1.08 | 0.899 | 1.03 | 0.775 | – | – | ||||||
| Rural | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | – | – | ||||||
| Wealth quintile | ||||||||||||||||||||
| Poorest | 1.28 | 0.741 | 0.53 | 0.381 | – | – | 1.42 | 0.448 | 4.27 | 0.339 | 0.56 | 0.047 | 1.79 | 0.066 | ||||||
| Quintile 2 | 0.61 | 0.460 | 1.13 | 0.855 | – | – | 0.93 | 0.860 | 0.63 | 0.743 | 0.65 | 0.011 | 1.11 | 0.745 | ||||||
| Quintile 3 | 0.81 | 0.728 | 0.72 | 0.632 | – | – | 0.85 | 0.696 | 0.98 | 0.991 | 0.72 | 0.055 | 1.52 | 0.186 | ||||||
| Quintile 4 | 0.75 | 0.603 | 1.12 | 0.868 | – | – | 1.32 | 0.497 | 0.10 | 0.175 | 0.86 | 0.371 | 1.09 | 0.793 | ||||||
| Richest | 1.00 | – | 1.00 | – | – | – | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – | ||||||
| Insurance statusa | ||||||||||||||||||||
| Insured A | 0.81 | 0.750 | – | – | – | – | 0.87 | 0.612 | – | – | – | – | 1.98 | 0.039 | ||||||
| Insured B | 0.90 | 0.868 | – | – | – | – | 0.70 | 0.311 | – | – | – | – | – | – | ||||||
| Uninsured | 1.00 | – | – | – | – | – | 1.00 | – | – | – | – | – | 1.00 | – | ||||||
| Educationb | ||||||||||||||||||||
| No education | 1.00 | – | – | – | 1.00 | – | 1.00 | – | – | – | 1.00 | – | – | – | ||||||
| Complete primary | 0.80 | 0.628 | 1.00 | – | 1.05 | 0.625 | 0.86 | 0.624 | 1.00 | – | 1.24 | 0.210 | 1.00 | – | ||||||
| Complete secondary | 4.48 | 0.011 | 0.60 | 0.322 | 0.92 | 0.647 | 1.46 | 0.386 | 0.69 | 0.601 | 1.06 | 0.810 | 1.10 | 0.700 | ||||||
| University | – | – | 1.05 | 0.945 | 1.08 | 0.663 | – | – | 0.14 | 0.135 | 1.24 | 0.413 | 1.07 | 0.764 | ||||||
| Sample size | 156 | 131 | 2107 | 318 | 73 | 2097 | 603 | |||||||||||||
OR, odds ratio.
a Insured A includes those insured in the United States and insured through the formal sector in Colombia and Mexico. Insured B includes those insured through the informal sector in Colombia and Mexico.
b For Colombia and Mexico, complete secondary includes individuals with a university education.
Finally, Table 3 explores the determinants of being on treatment and meeting treatment targets for all existing cardiovascular risks. Once diagnosed, males were less likely to be effectively managed than females in the Islamic Republic of Iran and Mexico, but in Thailand they were more likely to be. In Thailand, the two lowest income quintiles were less likely to be effectively managed, but surprisingly, in other surveys income was not a significant determinant of effective management. Similarly, a higher educational level was associated with a higher probability of meeting treatment targets in Colombia but not in other countries. Finally, insured individuals in the United States were almost twice (P < 0.05) as likely to be effectively managed as those without insurance, but insurance status was not associated with effective management in Colombia or Mexico. It is also important to note that in England and Scotland none of the socio-economic determinants were significantly associated with higher rates of diagnosis or effective treatment.
Discussion
In this paper we present a unique comparative picture of diabetes mellitus management based on an analysis of nationally representative surveys from seven countries, three of them developed and four in development. The overall finding was that a substantial proportion of individuals with diabetes remain undiagnosed and untreated and, perhaps more worryingly, that the percentage of individuals reaching International Diabetes Federation treatment goals for blood glucose, blood pressure and serum cholesterol is very low, ranging from 1% to 12%. These low rates of diagnosis, treatment and control reflect many lost opportunities for reducing the growing global burden of diabetes.
Once individuals are diagnosed, they are highly likely to be treated with medication, both in developed and in developing countries. Information on the management of hyperglycaemia with lifestyle interventions such as diet is not available. Nevertheless, in all countries more than 70% of individuals with diabetes were not reaching the blood glucose treatment targets set by the International Diabetes Federation and there was considerable variation across the seven surveys. While diagnostic criteria were largely consistent across national guidelines, there was less agreement on the treatment targets for blood glucose (Table 4), which may partly explain the wide variation in control rates. More recent evidence on the most appropriate treatment targets for blood glucose control34 further complicates the process of arriving at national and international treatment guidelines that are consistent, acceptable and implemented by national health-care providers and individuals with diabetes. Successful blood glucose management is clearly the result of a complex interplay between physician behaviour and patient adherence to treatment.
Table 4. Comparison of diagnostic thresholds for diabetes and treatment targets for blood glucose, systolic blood pressure (BP) and serum cholesterol across national guidelines in seven-country study of the management of diabetes and associated cardiovascular risk factors.
| National guideline (country, issuing body, year of publication) | Diagnostic threshold, FPG (mg/dl) | Treatment target |
||
|---|---|---|---|---|
| Blood glucose (HbA1c or FPG) | Systolic BP (mmHg) | Serum lipids (mmol/l) | ||
| Colombia, Ministry of Social Protection,28 2007 | ≥ 126 | < 7.0% HbA1c | < 140 | LDL < 2.6 |
| England and Scotland, National Institute for Clinical Excellence,29 2008 | NA | < 6.5–7.5% HbA1c | < 140 | LDL < 3.0 |
| TC < 5.0 | ||||
| TG < 2.3 | ||||
| Islamic Republic of Iran, Ministry of Health,30 2004 | ≥ 126 | < 140 mg/dl FPG | < 130 | LDL < 3.4 |
| TC < 6.2 | ||||
| TG < 2.3 | ||||
| Mexico, Ministry of Health,31 1994 | ≥ 126 | < 140 mg/dl FPG | < 130 | TC < 6.2 |
| TG < 2.3 | ||||
| HDL > 0.9 | ||||
| Thailand, National Health Security Office,32 2008 | ≥ 126 | < 6.5% HbA1c; 70–110 mg/dl FPG | < 130 | LDL < 2.6 |
| TC 3.4–4.4 | ||||
| TG < 1.7 | ||||
| HDL ≥ 1.0 | ||||
| United States, American Diabetes Association,33 2009 | ≥ 126 | < 7.0% HbA1c | < 130 | LDL < 2.6 |
| TG < 1.7 | ||||
| HDL > 1.0 | ||||
| World, International Diabetes Federation,26 2005 | ≥ 126 | < 6.5% HbA1c; < 110 mg/dl FPG | < 130 | LDL < 2.5 |
| TG < 2.3 | ||||
| HDL > 1.0 | ||||
FPG, fasting plasma glucose; HbA1c, glycosylated haemoglobin; HDL, high-density lipoprotein; LDL, low-density lipoprotein; mg/dl, milligrams per decilitre; mmHg, millimetres of mercury; mmol/l, millimoles per litre; NA, not available; TC, total cholesterol; TG, triglycerides.
One of the keys to the effective management of individuals with diabetes is the treatment of associated cardiovascular risks.13,16 Our analysis showed that 28–78% of individuals with diabetes who were also hypertensive were being treated or had attained therapeutic control targets. Much greater variation was seen in the treatment of hypercholesterolaemia, with especially low rates of diagnosis and treatment in Thailand. Control rates for blood pressure and serum cholesterol were much higher than for blood glucose, perhaps because of the high efficacy and minimal side-effects of the drugs used to lower blood pressure and serum cholesterol. Some of the variation seen across countries may be related to differential treatment guidelines. For both arterial hypertension and hypercholesterolaemia, low treatment rates coupled with high control rates among treated individuals suggest that there is a huge potential for reducing the burden of diabetes, particularly in developing countries.
The rates of effective management of cardiovascular risk factors in individuals with diabetes vary considerably. In all countries except Thailand, a large fraction of individuals with diabetes – about 35% in England and Scotland and close to 50% in the United States – take medication to lower blood glucose, blood pressure and serum cholesterol, but without meeting treatment targets. This suggests that the burden of diabetes in high-income countries could be reduced through improved patient management. It should be noted that the rates of effective management of cardiovascular risk factors for England and Scotland may have changed since 2004 as a result of the National Health Service’s experiment for improving the quality of care, but more recent data are not available.7,35
At least three strategies can be employed to improve the management of diabetes in the short term. First, efforts to standardize and track the care of patients with diabetes do not appear to have had a major impact to date. Hence, greater effort in this area and clear targets for physicians and patients are needed. Second, offering incentives to providers and patients is a new but promising approach, although it calls for further experimentation and evaluation. These incentives should ideally be related to blood glucose outcomes rather than process measures. The experience of the United Kingdom of Great Britain and Northern Ireland with providing incentives to physicians to improve the quality of care and disease management will be a source of useful lessons for other countries. Third, there appears to be an urgent need for technological innovation in the care of diabetes. The poor performance noted, for example, in meeting blood glucose control targets may be strongly related to the narrow window between ideal and excessively low blood glucose levels. Innovations in blood glucose monitoring and drug delivery could increase the proportion of diabetic individuals who remain within an optimal blood glucose range. Clearly, diabetes management has not been successful at the population level and both policy and research need to be strengthened in the future.
In most countries, income, wealth and education were not significantly associated with diagnosis, treatment and control rates. This is an encouraging finding, especially given the large socioeconomic inequalities seen in many health outcomes. In Thailand, however, low income and low educational level were significantly associated with lower rates of diabetes diagnosis and effective management, and with the diagnosis and treatment of arterial hypertension and hypercholesterolaemia.36 These findings suggest a clear need for better strategies targeting the poor in Thailand.
More intriguing still is the finding that health insurance status is an important predictor of diagnosis and treatment. This underscores the fact that for those who require diagnosis and chronic management, financial access to care is a critical concern. This is particularly evident in the United States. The fact that Mexico has succeeded in expanding financial access to services through a public insurance scheme highlights the interplay between financial access and disease management. Even though Seguro Popular had only existed for two years when the Mexican survey was conducted, individuals with diabetes who were covered by Seguro Popular had been diagnosed at significantly higher rates than those who were uninsured, and at rates comparable to those observed among individuals who were insured through the formal sector. This is very different from what we found in Colombia, where in 2007 individuals insured through the informal sector (subsidized scheme) had the same rates of treatment as the uninsured and significantly lower rates of treatment than those insured through the formal sector (contributory scheme). This may be attributable to the fact that at the time of the survey the two insurance schemes were offering substantially different benefits packages. Provisions for diabetes treatment under both packages were made identical in 2008, and since the survey was conducted insurance coverage has expanded almost the entire population. Therefore, the role of insurance in the diagnosis and management of individuals with diabetes in Colombia may become less important in the future.
Our study has several limitations. First, while the data we used are the latest available, they are not very recent. Changes in diagnosis and treatment guidelines have subsequently occurred in several countries. The most recent survey from England and Scotland was conducted in 2003, before the 2004 NICE experiment for improving quality. More recent studies have shown that prescription rates for oral hypoglycaemic agents have increased in the United Kingdom since 2000,37 so our results have probably underestimated the performance of the National Health Service in effectively controlling cardiovascular risks in individuals with diabetes. Second, there is debate as to whether there are differences when diabetes is diagnosed based on fasting plasma glucose versus HbA1c, and as to whether the method used to measure HbA1c is the same across surveys or not. In four of the surveys used in this analysis, fasting plasma glucose was measured, while HbA1c was measured in the other three. Recent literature, however, provides strong evidence that an HbA1c level of 6.5% is equivalent to a fasting plasma glucose level of 126 milligrams (mg) per decilitre (dl).38 Third, individuals in the sample for whom all three physical examination measures were available were fewer than those for which blood glucose levels were available, and the difference between the two groups varied across countries. Thus, our estimates may have been subject to selection bias. Fourth, much of this analysis relied on self-reported diagnosis and treatment obtained from population surveys, and the limitations of self-reported data are known. It is also impossible to ascertain the reasons for not being on medication or for not reaching treatment targets, and it is possible that poor patience adherence is playing a part. Fifth, the number of individuals with diabetes in the surveys conducted in Colombia, England and Scotland is very small, as a result of which greater uncertainty surrounds the estimates from these countries. Finally, our analysis of treatment is limited to pharmacological treatment only. Lifestyle intervention programmes, especially those that rely on dietary changes and increased physical activity, play an important role in diabetes management. However, household health surveys are inconsistent in enquiring about diet and physical activity, and this limited our ability to monitor the uptake of these interventions at the population level.
Based on this comparison of how well seven countries are performing in terms of population-level management of diabetes, hypertension and hypercholesterolaemia we make several recommendations. First, since the prevalence of diabetes is increasing worldwide and particularly in developing countries, it is critical to track diabetes care at the population level and to focus on actual outcomes, rather than on the process of care. It is also critical to study other countries with larger numbers of individuals with diabetes, such as China and India, for which nationally representative studies are not readily available. Second, it is important to prioritize the development and implementation of national guidelines and the use of new incentive programmes for the management of hypertension and hypercholesterolaemia among individuals with diabetes in developing countries. Our findings suggest that such progress may be more feasible and more likely to have a larger population health impact than blood glucose control. Third, there are opportunities for innovation in providing incentives, in the technology of diabetes management and in improving financial access to care. Real progress at the population level in the management of diabetes will likely require all three: monitoring performance in meeting treatment targets, expanding management of hypertension and hypercholesterolemia in individuals with diabetes, and innovations in the delivery of and access to care.
Acknowledgements
The authors thank Majid Ezzati and John Lin (Harvard School of Public Health) and Greg Roth and Mohammad Forouzanfar (Institute for Health Metrics and Evaluation) for their technical assistance. Thanks also to Brent Anderson and Kelsey Moore (Institute for Health Metrics and Evaluation) for help with the editing.
Funding:
EG, LM, MN, SL, RL and CJLM received research support from the Bill & Melinda Gates Foundation. RG received research support from the CARSO Institute and the Health Observatory of Latin America and the Caribbean. The funding sources had no role in the study design, data collection, data analysis, data interpretation, or writing of this paper. The corresponding author had full access to all data in the study and had final responsibility for the decision to submit the paper for publication.
Competing interests:
None declared.
References
- 1.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 2.Roglic G, Unwin N. Mortality attributable to diabetes: estimates for the year 2010. Diabetes Res Clin Pract. 2010;87:15–9. doi: 10.1016/j.diabres.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 3.Aekplakorn W, Abbott-Klafter J, Premgamone A, Dhanamun B, Chaikittiporn C, Chongsuvivatwong V, et al. Prevalence and management of diabetes and associated risk factors by regions of Thailand: Third National Health Examination Survey 2004. Diabetes Care. 2007;30:2007–12. doi: 10.2337/dc06-2319. [DOI] [PubMed] [Google Scholar]
- 4.Cowie CC, Rust KF, Byrd-Holt DD, Eberhardt MS, Flegal KM, Engelgau MM, et al. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999–2002. Diabetes Care. 2006;29:1263–8. doi: 10.2337/dc06-0062. [DOI] [PubMed] [Google Scholar]
- 5.Gu D, Reynolds K, Duan X, Xin X, Chen J, Wu X, et al. InterASIA Collaborative Group Prevalence of diabetes and impaired fasting glucose in the Chinese adult population: International Collaborative Study of Cardiovascular Disease in Asia (InterASIA). Diabetologia. 2003;46:1190–8. doi: 10.1007/s00125-003-1167-8. [DOI] [PubMed] [Google Scholar]
- 6.Kim SM, Lee JS, Lee J, Na JK, Han JH, Yoon DK, et al. Prevalence of diabetes and impaired fasting glucose in Korea: Korean National Health and Nutrition Survey 2001. Diabetes Care. 2006;29:226–31. doi: 10.2337/diacare.29.02.06.dc05-0481. [DOI] [PubMed] [Google Scholar]
- 7.Mainous AG, 3rd, Diaz VA, Saxena S, Baker R, Everett CJ, Koopman RJ, et al. Diabetes management in the USA and England: comparative analysis of national surveys. J R Soc Med. 2006;99:463–9. doi: 10.1258/jrsm.99.9.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rull JA, Aguilar-Salinas CA, Rojas R, Rios-Torres JM, Gómez-Pérez FJ, Olaiz G. Epidemiology of type 2 diabetes in Mexico. Arch Med Res. 2005;36:188–96. doi: 10.1016/j.arcmed.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 9.Gillies CL, Abrams KR, Lambert PC, Cooper NJ, Sutton AJ, Hsu RT, et al. Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. BMJ. 2007;334:299. doi: 10.1136/bmj.39063.689375.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bertram MY, Lim SS, Barendregt JJ, Vos T. Assessing the cost-effectiveness of drug and lifestyle intervention following opportunistic screening for pre-diabetes in primary care. Diabetologia. 2010;53:875–81. doi: 10.1007/s00125-010-1661-8. [DOI] [PubMed] [Google Scholar]
- 11.Hamnvik OP, McMahon GT. Glycemic targets for patients with type 2 diabetes mellitus. Mt Sinai J Med. 2009;76:227–33. doi: 10.1002/msj.20117. [DOI] [PubMed] [Google Scholar]
- 12.Ray KK, Seshasai SR, Wijesuriya S, Sivakumaran R, Nethercott S, Preiss D, et al. Effect of intensive control of glucose on cardiovascular outcomes and death in patients with diabetes mellitus: a meta-analysis of randomised controlled trials. Lancet. 2009;373:1765–72. doi: 10.1016/S0140-6736(09)60697-8. [DOI] [PubMed] [Google Scholar]
- 13.Zarich SW. Antidiabetic agents and cardiovascular risk in type 2 diabetes. Nat Rev Endocrinol. 2009;5:500–6. doi: 10.1038/nrendo.2009.150. [DOI] [PubMed] [Google Scholar]
- 14.Clark CM, Jr, Lee DA. Prevention and treatment of the complications of diabetes mellitus. N Engl J Med. 1995;332:1210–7. doi: 10.1056/NEJM199505043321807. [DOI] [PubMed] [Google Scholar]
- 15.Nathan DM. Clinical practice. Initial management of glycemia in type 2 diabetes mellitus. N Engl J Med. 2002;347:1342–9. doi: 10.1056/NEJMcp021106. [DOI] [PubMed] [Google Scholar]
- 16.Mourad JJ, Le Jeune S. Blood pressure control, risk factors and cardiovascular prognosis in patients with diabetes: 30 years of progress. J Hypertens Suppl. 2008;26:S7–13. [PubMed] [Google Scholar]
- 17.Bellary S, O’Hare JP, Raymond NT, Gumber A, Mughal S, Szczepura A, et al. UKADS Study Group Enhanced diabetes care to patients of south Asian ethnic origin (the United Kingdom Asian Diabetes Study): a cluster randomised controlled trial. Lancet. 2008;371:1769–76. doi: 10.1016/S0140-6736(08)60764-3. [DOI] [PubMed] [Google Scholar]
- 18.Foley RN, Collins AJ. The growing economic burden of diabetic kidney disease. Curr Diab Rep. 2009;9:460–5. doi: 10.1007/s11892-009-0075-9. [DOI] [PubMed] [Google Scholar]
- 19.Sosa-Rubí SG, Galárraga O, López-Ridaura R. Diabetes treatment and control: the effect of public health insurance for the poor in Mexico. Bull World Health Organ. 2009;87:512–9. doi: 10.2471/BLT.08.053256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rodríguez J, Ruiz F, Peñaloza E, Eslava J, Gómez LC, Sánchez H, et al. Encuesta Nacional de Salud 2007: resultados nacionales. Bogota: Ministry of Health and Social Protection; 2009. [Google Scholar]
- 21.Health survey for England 2003: summary of key findings. London: National Centre for Social Research, Department of Epidemiology and Public Health; 2004. Available from: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsStatistics/DH_4098712 [accessed 6 November 2010].
- 22.Asgari F, Aghajani H, Haghazali M, Heidarian H. Non-communicable diseases risk factors surveillance in Islamic Republic of Iran. Iran J Public Health. 2009;38(Suppl 1):119–22. [Google Scholar]
- 23.Villalpando S, de la Cruz V, Rojas R, Shamah-Levy T, Avila MA, Gaona B, et al. Prevalence and distribution of type 2 diabetes mellitus in Mexican adult population: a probabilistic survey. Salud Publica Mex. 2010;52(Suppl 1):S19–26. doi: 10.1590/s0036-36342010000700005. [DOI] [PubMed] [Google Scholar]
- 24.The Scottish Health Survey 2003: summary of key findings. Edinburgh: The Scottish Executive Health Department; 2005. Available from: http://www.scotland.gov.uk/Resource/Doc/924/0021055.pdf [accessed 6 November 2010].
- 25.National Health and Nutrition Examination Survey 2003–2006. Hyattsville: National Center for Health Statistics. Available from: http://www.cdc.gov/nchs/nhanes.htm [accessed 6 November 2010].
- 26.Global guideline for type 2 diabetes Brussels: International Diabetes Federation; 2005.
- 27.Type 2 diabetes: national clinical guideline for management in primary and secondary care (update) London: National Collaborating Centre for Chronic Conditions (Great Britain), Royal College of Physicians; 2008. [PubMed] [Google Scholar]
- 28.Guide 17: guide for care of diabetes mellitus type 2. In: Guidelines for health promotion and disease prevention in public health, volume II. Bogota: Ministry of Social Protection; 2007.
- 29.Type 2 diabetes: national clinical guideline for management in primary and secondary care (update) London: National Institute for Clinical Excellence; 2008. [PubMed]
- 30.Delavari A, Mahdavihazaveh A, Norozinejad A, Yahramadi S. National health programme for control and prevention of diabetes for Behvarzes Tehran: Center for Disease Control, Ministry of Health and Medical Education; 2004. [Google Scholar]
- 31.Mexican official standard for the prevention, treatment, and control of diabetes (NOM-015-SSA2–1994). Mexico City: Secretaría de Salud; 1994. Spanish.
- 32.Clinical practice guideline for management of diabetes 2008 Bangkok: Diabetes Association of Thailand, Endocrine Society of Thailand & National Health Security Office; 2008.
- 33.American Diabetes Association Standards of medical care in diabetes - 2009. Diabetes Care. 2009;32:S13–61. doi: 10.2337/dc09-S013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Currie CJ, Peters JR, Tynan A, Evans M, Heine RJ, Bracco OL, et al. Survival as a function of HbA(1c) in people with type 2 diabetes: a retrospective cohort study. Lancet. 2010;375:481–9. doi: 10.1016/S0140-6736(09)61969-3. [DOI] [PubMed] [Google Scholar]
- 35.Roland M. Linking physicians’ pay to the quality of care – a major experiment in the United Kingdom. N Engl J Med. 2004;351:1448–54. doi: 10.1056/NEJMhpr041294. [DOI] [PubMed] [Google Scholar]
- 36.Khonputsa P, Veerman JL, Vos ET, Aekplakorn W, Bertram M, Abbott-Klafter J, et al. Joint prevalence and control of hypercholesterolemia and hypertension in Thailand: third National Health Examination Survey. Asia Pc J Public Health Epub 2010 Aug 3. [DOI] [PubMed]
- 37.Filion KB, Joseph L, Boivin JF, Suissa S, Brophy JM. Trends in the prescription of anti-diabetic medications in the United Kingdom: a population-based analysis. Pharmacoepidemiol Drug Saf. 2009;18:973–6. doi: 10.1002/pds.1802. [DOI] [PubMed] [Google Scholar]
- 38.Saudek CD, Herman WH, Sacks DB, Bergenstal RM, Edelman D, Davidson MB. A new look at screening and diagnosing diabetes mellitus. J Clin Endocrinol Metab. 2008;93:2447–53. doi: 10.1210/jc.2007-2174. [DOI] [PubMed] [Google Scholar]