Abstract
This paper queries the pharmaceutical industry’s concept of “ready-to-recruit” populations by examining its recruitment strategies for clinical trials and the types of human subjects who participate in these drug studies. The argument is that the pharmaceutical industry has profited from a system comprised of what can more aptly be characterized as ready-to-consent populations, meaning populations who do not have better alternatives than participation in clinical trials. Further, through qualitative research, this paper aims to highlight some of the limitations of current U.S. federal regulation and to show how these limits signal problems that are not normally discussed in the medical ethics literature about research on human subjects. It does this by examining the impotence of informed consent – both as a concept and as a practice – in light of recruitment strategies and the structural reasons motivating individuals to participate in clinical trials.
During the past two decades, human subjects research has developed into a full-fledged industry with a global presence. Human subjects are needed to test the safety and efficacy of new pharmaceutical products before those drugs or devices can be marketed to the general public. In response to the pharmaceutical industry’s demand for human bodies, companies have emerged specializing in finding the right bodies for clinical studies (Epstein, 2007; Fisher, 2005). These companies – contract research organizations (CROs) and central patient recruitment firms – promise increased efficiency in filling clinical trials in order for pharmaceutical companies to get their products to market faster.2
While the implications of these companies for the commercialization of science and for the ethics of human subjects research have begun to be discussed in academic scholarship (Mirowski & Van Horn, 2005; Petryna, 2006), there has not been a close examination of the adequacy of current U.S. federal regulation for safeguarding human subjects within this emergent industry.
This paper centers on one particular framing of human subjects – both in the U.S. and globally – as populations that are “ready to recruit” for clinical trials. This language mobilized by the pharmaceutical industry and ancillary clinical trial companies suggests a view of the public as comprised of potential human subjects who can be motivated to participate in clinical trials given the invitation to do so. Moreover, it signifies a strategy by the pharmaceutical industry to capitalize upon the political and economic conditions that disadvantage populations around the world. In short, the current clinical trials industry takes advantage of disenfranchised populations by offering these groups limited and problematic access to healthcare in exchange for their bodies as testing sites for new products (Fisher, 2005).
Discussions about populations being “ready to recruit” for clinical trials have emerged as part of a justification for a broader shift in the sites where the clinical development of pharmaceutical products takes place. Since 1990, the pharmaceutical industry has shifted the bulk of its clinical research away from academic medical centers in the United States to for- profit clinics around the world.3 This relocation of clinical trials to the private sector has been motivated by the industry’s desire to cut drug development costs and speed new products to market (Rainville, 2002). While the private sector may indeed be a cheaper, quicker place to conduct drug studies, the benefit of this new setting has been framed in terms of the availability of human subjects to participate in clinical research.4 The underlying logic of this approach has been to stop waiting for potential human subjects to come to clinical trials (i.e., to university hospitals) and instead to take the clinical trials directly to the appropriate patient populations (e.g., to private practices and local hospitals). Thus, the world – in this view – is made up of potential human subjects who, with the right marketing approach, are ready to be recruited into drug studies.
In order to underscore the importance of this rhetoric surrounding human subjects, this paper queries the concept of “ready-to-recruit” populations by examining not only recruitment strategies but also the types of human subjects participating in clinical trials. Specifically, I describe common advertising practices, including a lengthy discussion of a television advertisement designed to recruit potential subjects into an asthma study. Next, drawing upon extensive qualitative field research, I relate three case stories of individuals who participated in clinical trials for three very different reasons: the desire to find a cure for an intractable disease, a lack of health insurance, and a source of income.
By attending to the messages – both explicit and implicit – that are embedded in recruitment techniques and by illustrating which specific populations actually participate in drug studies, this paper argues that the pharmaceutical industry has profited from a system comprised of what can more aptly be characterized as ready-to-consent populations, meaning populations who do not have better alternatives than participation in clinical trials. My re-framing of the same populations is meant to call into question what operates within the industry as a euphemism for the exploitation of certain groups. Further, this paper aims to highlight some of the limitations of current U.S. federal regulation and to show how these limits signal problems that are not normally discussed in the medical ethics literature about research on human subjects. I do this by examining the impotence of informed consent – both as a concept and as a practice – in light of recruitment strategies and the structural reasons motivating individuals to participate in clinical trials.
Recruitment & Informed Consent
Informed consent as the key to decision-making for participation in medical research arose through U.S. federal regulation designed to protect the rights and welfare of human subjects. Emerging in 1981 after nearly a decade of Congressional hearings responding to public outcry over abuses of human subjects5, U.S. regulation aimed to eliminate the deception and coercion of Americans participating in research (Faden & Beauchamp, 1984).6 The panacea for correcting the problems of the past was symbolized by “informed consent” and the ethical principle of “respect for persons” (i.e., “autonomy”) upon which it is based. According to many ethicists, informed consent is the primary basis for determining that a research study is ethical (e.g., Caplan, 1998). Both the federal regulation and the ethical principle are premised on the assumption that individuals act as autonomous beings who make measured decisions about participating in research based on information given to them. While social scientists as well as feminist bioethicists have criticized this position by arguing that the ethics of human subjects research is much more complex than consent alone (e.g., Corrigan, 2003; Halpern, 2004; Sherwin, 1996; Wolpe, 1998), informed consent and the principle of “autonomy” have remained the foundations of ethical discourse and practice, especially in the policymaking context.
In fact, the U.S. federal regulation has changed very little in the past 25 years. Informed consent continues to be seen as sufficient protection for human subjects. Perspectives on informed consent, however, have not been entirely static. A recent recommendation from several advisory bodies to the government7 has been to re-envision informed consent not as a form to be signed but as a process (IOM, 2002). The clinical trials industry itself has internalized this new rhetoric surrounding consent and strongly advocates for informed consent to be an ongoing process, one that will aid in the recruitment and – equally importantly – the retention of human subjects (Anderson, 2004). In this industry view, informed consent should be strategically mobilized in such a way to persuade individuals to enroll in studies and to inform them of their responsibilities to pharmaceutical companies (Fisher, 2005).
Another model of informed consent that has been conceptualized by bioethicists envisions human subjects as collaborators in the research process. Robert Veatch (1987), who has significantly contributed to developing this position, advocates for patients and human subjects to be in partnership with physicians and researchers:
The patient as a partner needs to know all those things that a reasonable person would want to know in order to decide whether to participate in the partnership. Reasonable persons who are potential partners in a venture may want to know certain risks and potential benefits, but they may also want to know information that has no bearing whatsoever on potential risks. They may want to know something about the purposes of the study, maybe even something about the theory underlying the innovation. It is no longer a matter of benefits and harms – to either the subject or society – but rather what it takes to decide whether to becomes an active partner in an important enterprise. (Veatch, 1987, p. 9)
This position – as well as other instantiations of it developed by feminist bioethicists (e.g., Sherwin 1998) – is radical in that it attempts to take the ethical principle of autonomy a step beyond consent to encourage human subjects to engage actively in the research enterprise.
While a collaborative model of research can be highly successful in investigator-initiated studies where the researchers who have conceptualized the project are directly interacting with human subjects,8 pharmaceutical clinical trials prove more challenging because the physicians conducting the studies are rarely the ones who have designed them. In addition, pharmaceutical studies emphasize subjects’ passive compliance over active investment. Apart from these challenges to meaningful collaboration in pharmaceutical research, the partnership model requires that subjects will accept an active role in the research process if offered. This is seldom the case in practice.
Additionally, in spite of re-evaluations of the purpose and practice of informed consent, there is generally little recognition of when the process of informing as well as consenting begins. Policymakers and many ethicists assume that informed consent begins when prospective human subjects are directly given information about the research, usually the informed consent form. In other words, informed consent is generally thought to begin in clinical trials when individuals undergo what is called a “screening and consent visit” in the clinic. During this time, those individuals discuss the research with study staff and receive a lengthy informed consent form to sign and date.
What these views of informed consent do not take into account, however, is that most prospective human subjects have already decided to take part in clinical studies before receiving the informed consent forms (Fisher, 2005). This indicates that the process of consent actually begins before potential human subjects are informed about the purpose, risks, and benefits of any given study. Thus, the importance of recruitment cannot be underestimated given that potential human subjects are making decisions about participating in clinical trials before they know the details of the studies for which they will volunteer.
Recruitment methods for clinical trials vary from physician referrals to highly specific databases of patients to mass media advertising (Anderson, 2004). With the privatization of clinical trials, recruitment has increasingly been viewed as a science, and many niche-market companies have established themselves as experts in finding human subjects for clinical trials (Epstein, N.D.). Like direct-to-consumer advertising for marketed drugs, advertising for clinical trials has increased dramatically in the past decade and has consequently increased the visibility of these studies in the United States. In large cities around the country, clinical trials have become a part of everyday life through the public face that advertising for these studies has created. Advertisements appear across a range of venues and media from public transportation and newspapers to radio and television.
The proliferation of clinical trial advertising has reached the point where individuals’ understanding of and expectations about medical research is rooted in the messages infused in these advertisements (Fisher, 2005). This is of course no accident, and is in fact part of the process of privatization that clinical trials have been undergoing since the early 1990s. These ads can be said to be not only tools for recruiting human subjects into specific clinical trials but also for increasing the public’s awareness about participating in clinical trials more generally.9 This is particularly important to consider when examining the role of recruitment on informed consent.
Analysis of Advertisements
Advertising strategies as part of clinical trial recruitment serve to shape potential human subjects’ decisions to participate in pharmaceutical drug studies. Importantly, the most prevalent advertisements in the mass media for clinical trials depict common illnesses that tend to be chronic and rarely life threatening. Ads for depression, anxiety, insomnia, and arthritis studies appear with much more frequency than ads for cancer or HIV/AIDS clinical studies. Print ads emphasize that human subjects participating in clinical trials will receive medical evaluations and “study medications” or “investigational medications” at no cost. These ads tend not to communicate very much information but encourage interested parties to “call today!” or “give us a call” at local or toll-free numbers. In contrast, radio and television advertisements are often comprised of storylines in which characters inform each other about the possibility of participating in clinical trials. This genre of advertisement communicates on multiple levels about what can be gained and for whom by enrolling in a drug study.
The U.S. Food & Drug Administration (FDA) regulates the content of all advertisements used for recruitment into clinical trials, and it is the responsibility of local or centralized institutional review boards (IRBs) to review each proposed advertisement before it can be made public. In spite of this oversight, ads often (intentionally) undermine existing protections for human subjects through the information they do or do not supply. In fact, marketing techniques can be said to privilege a “ready-to-consent” orientation toward recruitment.
One television advertisement for an asthma study epitomizes how misleading information gets communicated about clinical trials. In this ad, two women – one African American and one White – run into each other in a grocery store and discuss an asthma clinical trial for their family members. The following is the text of the television commercial:10
[W1 = White woman, W2 = African American woman, VO = male voiceover]
W1: Hi, Nicki.
W2: Hey, girl, how’s things?
W1: Pretty good, except for my youngest Sherry.
W2: What’s the matter with Sherry?
W1: Oh, it’s her asthma. She can’t go anywhere without her inhaler, and it embarrasses her so much.
W2: My husband Anthony, he’s the same way, and he’s been using his inhaler since he was 12.
W1: Well, has he tried any other treatments?
W2: Honey, he’s tried all kinds of things!
W1: What are you going to do?
W2: You know, I convinced him to go into an asthma research study.
W1: You did what?!
W2: Well, I saw this tv ad. They said they were studying an investigational asthma medication, so I wrote down the 800 number, and I gave them a call.
W1: And?
VO: If you’re 12 or older and suffer from asthma, call 1-800-XXX-XXXX to enroll in a clinical research study. Participants receive free examination, study medicines, lab and breathing tests, and carfare. Have your medications with you when calling.
W1: Hey, can I get that number? Maybe I can get Sherry enrolled.
W2: I’ll call you with it as soon as I get home. VO: 1-800-XXX-XXXX.
The text of this advertisement alone cannot communicate the enthusiasm of the two women at having a potential solution for their ill family members’ problems. In addition, during the voice over, the text “free examination,” “free study medicines,” and “free lab and breathing tests” float over a backdrop of fresh produce. In each case, the word “free” is repeated on the screen and appears in a much larger font than the other words.
This ad is particularly interesting because the layered meanings that are communicated about clinical trials are infused with representations of gender, race, and class. What is immediately striking about this advertisement is that the women depicted do not have asthma and are not the population targeted for recruitment into the clinical trial. This is not the same as saying that they are not the target population for the advertisement itself. In fact, as wives and mothers, they are indeed the right demographic for the marketing message. The implied message is that it is up to women, who care about the health and well-being of their families, to “convince” those in their charge to enroll in clinical studies.
It is also not merely a coincidence that there is an African American woman depicted in this advertisement and that she is the woman who is informing the other about the study. This representation is meant to project to African American viewers that clinical trial participation is the right choice for them too.11 As for the meanings communicated about class, the television commercial implies that clinical trials are options for middle class Americans, not just the poor who sign up to be guinea pigs or the rich who are looking for an alternative cancer therapy. Overall, the implicit message of the ad is that participation in research studies is legitimate, even safe enough for children.
The maternal theme is important in that it underscores the ineffectualness of current asthma medications from both medical and psychosocial perspectives. More specifically, one woman’s daughter and the other’s husband cannot go anywhere without their inhalers, and this is embarrassing to them. The problem is two-fold: (1) the inhalers are not physiologically effective because they treat the symptoms rather than the disease and (2) the inhalers are not socially effective because they are embarrassing – or at least the symptoms of asthma are embarrassing and the inhaler represents these symptoms. This double failure of standard asthma treatment becomes the women’s responsibility for their loved ones.
Seen through the lens of the women seeking better asthma treatments for their families, the advertisement suggests that the “study medicine” will have better results, both physiologically and psychosocially. The implied promise is that the drug under investigation will be efficacious, safe, and better for asthma-sufferers. While this product may indeed be a better treatment for asthma,12 the television commercial is misleading because it implies a set of results that are the very purpose of the study itself.
The intent of this optimistic framing of the “study medicine” is for potential human subjects (or their loved ones) to assume that clinical trials – and this one in particular – do offer magic bullet cures. And, equally important in the ad copy, these results can be had at absolutely no cost to those who participate in the research study. What goes unmentioned in the advertisement – and others like it – are the use of placebo versus active drug, the potential risks to the human subjects, and the logistical burden of participating (both for the subjects themselves and for family members accompanying them to study visits).
The irony about clinical trial recruitment is that there are more disclaimers given to viewers as part of direct-to-consumer marketing of FDA approved drugs and their side effects than there are of investigational products, which may prove to be neither safe nor efficacious after clinical testing.13 Thus, from a regulatory perspective, the information communicated in advertisements for marketed drugs is required to be more balanced than the information about clinical trials. Given the American public’s general savviness about prescription drugs and general ignorance about drug development, the difference in advertising practices must be understood as problematic. This is particularly disturbing because the information contained in ads for clinical trials is much more digestable and straightforward than information in informed consent documents. As a result of these and other recruitment strategies, it should be no surprise that advertising can have a profound impact upon the decisions of potential human subjects (even after they have read informed consent forms). Yet an analysis of marketing to recruit human subjects is ungrounded without a discussion of the human subjects who do participate in clinical trials. To illustrate some limitations on informed consent, the next section will examine three cases of study volunteers’ decision-making about enrolling in three very different pharmaceutical clinical trials.
Participation & Informed Consent
The trends in the United States surrounding participation in pharmaceutical clinical studies can be mapped onto differences in gender, race, and class (Fisher, 2005). Early clinical testing of new products, called Phase I research, generally aims to determine the safety (read: toxicity) of investigational drugs in healthy humans and to establish appropriate dosage in humans for subsequent testing. These types of studies are overwhelmingly filled by low income, minority men who participate in clinical trials in exchange for money.14 In contrast, later clinical evaluation of pharmaceuticals (Phases II and III) aims to test the efficacy of these products.15 Enrollment in these studies tends to be comprised of individuals without health insurance and particularly White women.
In a very real sense, clinical trials have come to serve as a limited and problematic resource for disenfranchised groups. What this means in the context of the argument here is that structural variables are often much stronger determinants of participation in clinical trials than are the details of specific studies. What matters to most potential human subjects is that they will receive the monetary compensation or a form of access to healthcare; the risks of the study are usually of little interest to them, except in the extremely rare cases that informed consent forms are explicit about the possibility of death as a “side effect.” Many individuals who have participated as human subjects in drug studies report that what mattered to them much more than the risks of the study were the logistics (Fisher, 2005). When there are frequent study visits or long in-patient confinements, many individuals cannot make the clinical trial fit into their lives and must decline participation.
If potential human subjects are not particularly concerned about the details contained in informed consent forms and if most of their information comes from recruitment sources such as mass media advertisements, human subjects are making decisions to participate in studies based on their impressions of what benefits clinical trials will have for them. In order to explore this point further, I take three examples of human subjects who have participated in pharmaceutical clinical trials. Each case highlights a different type of motivation for participation in these studies: (1) patients with progressive diseases, (2) individuals without health insurance, and (3) healthy individuals seeking income. Together these cases illustrate that decision-making regarding participation in clinical trials is more complex than is modeled in the federal regulation, which assumes ideal “autonomous” individuals weighing the pros and cons of particular studies.
Case One: Progressive Diseases
During my fieldwork in the Southwest U.S. on the clinical trials industry, I had the opportunity to sit in on an informed consent visit for a study to test the safety of an experimental treatment for Alzheimer’s. The potential human subject was a 75-year old Latina woman, accompanied by her middle-age son. They had found out about the study through a print advertisement in a local newspaper. The ad had emphasized that human subjects could continue to take their prescribed Alzheimer’s medication while taking part in the study and receiving a “study medication.”
The tone of the informed consent visit was educational. The physician conducting the study spent an hour with the woman and her son to explain the disease itself and the history of the product being tested.16 The most important information given about the study was that the product had previously been tested in humans and had caused the development of encephalitis in many of the participants, leading to death in several cases. The current one-year study consisted of a retooled version of the drug, and the purpose was solely to test its safety. The mother and son were told that the study would not have any therapeutic value and that the primary motivation for participating should be altruism.
After the physician finished presenting the information, he asked whether either the son or the woman had any questions. What occurred during the subsequent conversation was revealing about the assumptions that potential human subjects (and their family members) have about medical research. The son began by telling the physician how important it was to him to find an effective treatment for his mother. While this would likely be true for any individuals watching their parents deteriorate from Alzheimer’s, the son had turned to clinical research because he had recently buried his father who had suffered for many years from the same disease. The possibility of losing his mother in the same slow way was unacceptable to him. His goal, in his explanation as to why he responded to the advertisement, was to find a treatment that would curb the progression of his mother’s Alzheimer’s disease.
In response to the son’s explanation, the physician carefully reiterated that participants would not receive any therapeutic benefit from the study. He explained that while the study included a rigorous evaluation, including an MRI at the outset to establish the diagnosis of Alzheimer’s disease, there would be no further tests during the course of the year to assess the amount of deterioration participants had experienced due to their illness. In spite of being assured that the study would do nothing to improve his mother’s condition, the son actively continued to search for a therapeutic benefit for his mother.17 For example, he hypothesized that his mother might experience an improvement in her illness if the treatment was later proved to be efficacious. He posited that even if the purpose of the study was not to help his mother, the drug could still work to that effect. The physician quickly told him that in order for the drug to have any effect, it would have to be administered regularly, and this study included only one dose and lengthy follow-up.
After much more exchange between the physician and the son, it appeared that the son had indeed accepted that his mother would not improve from participating in the clinical trial. Instead of using this opportunity to thank the physician and leave, the son settled on the diagnostic benefits of participating in the study as sufficient reason for his mother to enroll. His mother had only the most basic health coverage through Medicare, and he was attracted to the idea that she would be able to have a very expensive MRI performed. Even though he had responded to the ad because he hoped for a miracle cure for his mother, the son had his mother sign the consent form to enter a study that would have no therapeutic benefit and would have significant risks. It seemed that the son had made up his mind that his mother would participate in the study prior to hearing the details. What the informed consent visit achieved was to give him new reasons for justifying her participation.18
Case 2: Health Insurance Status
A White woman in her late forties volunteered for a clinical trial to test the efficacy of a product to treat a condition known as “overactive bladder.” When I interviewed her, she had been enrolled in the clinical trial for approximately six months, and she described these few months as life changing. Before seeing an advertisement about the study, she said that she was well aware that she had a medical condition that needed treatment. As someone who worked hourly jobs most of her life, she had not had any form of health insurance since becoming an adult. She described for me the embarrassment that overactive bladder had caused, leading her to pay out of pocket to see a physician and get a prescription for treatment. After filling the prescription for a brand name drug, she decided that she would use the treatment sparingly. Because it was so prohibitively expensive, she would not be able to fill it as often as she should. Over the next few months, she had several “accidents” at work, resulting in her losing her job and the little means she had to fill the prescription. She was out of work for several months when the first “miracle” happened.
She recalled hearing an advertisement on the radio that she felt described her perfectly. According to her, the ad stated that a clinic was seeking participants for a six-month evaluation of an overactive bladder drug for individuals currently not taking any medications for this condition. Not only would the study offer free medical evaluations and “medicines,” it also promised a stipend. Because she was no longer employed, the small income she would receive confirmed even further that the study was indeed “perfect” for her. She immediately called the toll-free number and was scheduled to screen for the study. In response to my questions, she told me that she could not recall much of what was discussed in the informed consent form, including any of the risks of the trial. What she remembered was feeling concerned that she might not get the treatment because some participants would receive a sugar pill. She went on to say that these worries were unfounded because she is sure that she got the drug; her symptoms cleared up entirely, and she experienced “dry mouth,” a common side effect of the drug.
As the trial elapsed, she began to worry about the end of the study. She dreaded losing access to the drug because of her continued inability to pay for any treatment herself. To make matters worse, she had been able to find a new job and feared losing it if she was no longer being “treated.” At the beginning of the sixth and what was to be the final month of the study, the second “miracle” happened. The study coordinator told her that the pharmaceutical company had decided to extend the study by an additional 12 months and asked her if she would be interested in continuing her participation. She described this news as immediately lifting an incredible burden. She said that the clinical trial had been life changing and its extension a godsend. In her estimation, clinical trials were the perfect option for people without health insurance suffering from medical problems. This case indicates that information about risks contained in the consent form did not matter compared to having limited access to a “treatment” that she otherwise could not afford.
Case 3: Healthy Human Studies
Generic advertisements appear daily in newspapers, on the radio, and in public transportation to recruit healthy individuals into clinical trials. In large cities where there are “clinics” specializing in drug studies of this type, the prevalence of these ads confers legitimacy on these studies, billed as “good, easy, fast money.”19 One of my interviewees who had participated in a healthy human study had an experience that sheds considerable light on the process of enrolling in drug studies to test new pharmaceutical products for safety.
I interviewed a Latina woman in her early thirties who described her interest in volunteering for a healthy human study as motivated by the desire for additional income. She was a single mother with a fairly low-paying job, and she thought that volunteering for a well- paying clinical trial would do a lot to provide additional money to see her through a few months. She called the toll-free number and was informed about several studies for which she pre- qualified – based on sex, age, etc. – and could select one for which to screen. She told me that the woman on the phone told her about a vaginal endometriosis study, and this study appealed to her because she had once been diagnosed with endometriosis and it was something she knew a little bit about. She also felt from her personal experience that women’s health problems are not as well understood as they should be, and that being in that study would not only benefit her economically but that it was something she could feel proud of participating in too.
When she arrived at the clinic to screen for the study, she was given a lengthy informed consent form to read and paperwork about her medical history to fill out. She also received a presentation with a group of other potential subjects by one of the staff. She told me what she could not understand was why the woman presenting the information kept talking about attention deficit disorder when she was there for an endometriosis study. She interrupted the staff person to clarify, and she was told that she was in fact in the process of screening for an attention deficit disorder study. When she told the woman that it was not the study she had signed up for, the woman assured her that she was equally qualified for the ADD study. She told me she hesitated only for a moment. She asked how much the ADD studied paid, and because it was the same amount ($2300), she signed the form. When I asked her, she said she didn’t know what the risks of the ADD study might have been and had no idea how those risks might have compared to any risks in an endometriosis study. She said that what was important about volunteering for a study was the original motive – the income she could earn – not any reasons associated with any particular study. While she indicated that she would have been more “proud” to have participated in the endometriosis study, those details were somewhat interchangeable compared to the bottom-line stipend amount that motivated her primary interest in participating in a clinical trial. Informed consent did not matter much in the face of financial need.
These three cases are meant to illustrate the disconnect between the reasons why individuals participate in clinical trials and U.S. federal regulation to protect human subjects. Holding autonomy and informed consent as the model for ethical practice, federal regulation places decision-making about study participation within a vacuum, stripping it of all social contexts (Corrigan, 2003; Fisher, 2006a). Qualitative approaches to evaluating why individuals enroll in clinical trials are critical for understanding how structural conditions shape those decisions.
A healthy critique of the ethical principle of “autonomy” does not, of course, imply that individuals cannot and do not exert agency in relation to the clinical trials industry. Individuals are clearly savvy about the choices that they make about whether to participate in studies. In fact, those who participate in Phase I studies are incredibly insightful about the exchange in which they are engaged with the pharmaceutical industry.20 Instead, what I am arguing is that the principle of autonomy – and the formal procedure of informed consent – is insufficient to protect individuals from research abuses.
Conclusion
This paper has introduced some of the ways in which current U.S. regulation fails to protect human subjects in pharmaceutical clinical trials. By highlighting recruitment strategies that confer both explicit and implicit meanings and expectations about study participation, I have argued that the information that potential human subjects receive about clinical trials is often misleading and that this initial information is more salient than anything contained in informed consent forms. The irony of the regulation (or lack thereof) surrounding recruitment for clinical trials is that marketers have more freedom in crafting messages about investigational drugs than do marketers in advertising FDA-approved prescription drugs to consumers. The second part of this paper drew upon field research to illustrate some reasons why individuals participate in clinical trials and how these motivations (i.e., intractable disease, lack of health insurance, economic need) appear vastly more important to subjects than information contained in informed consent forms.
Bioethicists and policymakers have proposed new models of informed consent for revitalizing the process and making consent more robust. Proposals have included more mainstream ideas, such as de-emphasizing consent forms and stressing on-going information and opportunities for consent, to more radical models, such as advocating for partnerships between researchers and subjects. Responding to the impotency of informed consent forms to communicate effectively to potential human subjects, these alternative models seek to engage subjects in more dialogue throughout the course of their involvement in clinical trials. A limitation of all these proposed models for consent is that they are unable to account for imbalances of power, not only between researchers and subjects but also among groups and institutions within society. By focusing on how subjects participate but ignoring why they participate, current informed consent models artificially circumscribe subjects’ decisions within a dyadic vacuum of clinical relationships. More importantly, this focus operates to hide the broader implications of pharmaceutical research and the insufficiency of informed consent as a mechanism to lessen the burden of research on disadvantaged groups.
What must become the focus of attention is that clinical trials have become a way for people to earn some income or have access to the medical establishment. Current federal regulation does not acknowledge these facts in its guidelines on “vulnerable populations” or in its rules for good clinical practice. While I am not arguing for a prohibition against recruiting the uninsured or the poor for clinical trials, I am calling for a re-evaluation of the structural conditions in the U.S. that make clinical trial participation necessary for these groups. In the Congressional investigations in the 1970s on the use of prisoners for medical research, for example, U.S. Senator Edward Kennedy coupled his call for human subjects protection with a call for prison reform. In his view, the avidness with which prisoners participated in studies (for money, for reduced sentences, for better food, etc.) signaled that something was wrong with the penal system (Hornblum, 1998). Likewise, today’s environment surrounding clinical trial participation signals gross problems with our healthcare system and with our distribution of economic and social opportunities for American citizens and others. These issues become more urgent as clinical trials are increasingly globalized and impact upon diverse groups. It should be a priority to ameliorate the conditions that have contributed to the creation of populations of disenfranchised individuals who are ready to consent to pharmaceutical clinical trials regardless of the risks.
Figure 1.
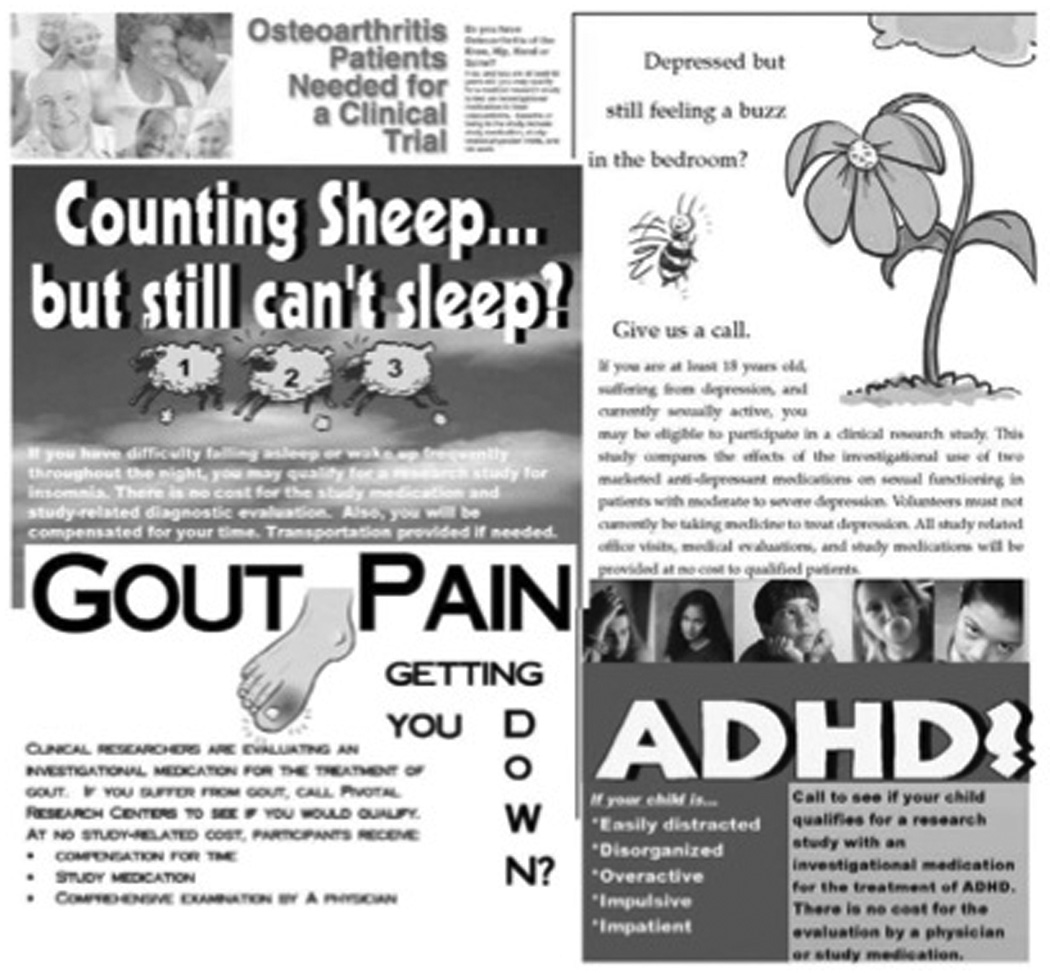
Sample of print media ads from the southwestern U.S.
Figure 2.

Still image from asthma ad
Footnotes
The research informing this paper was supported by the National Institutes of Health under Ruth L. Kirschstein National Research Service Award 5F31MH070222 from the National Institute of Mental Health. This project involved 12 months of qualitative fieldwork in the Southwest U.S., consisting of participant observation and 57 semi-structured interviews.
It could also be that the increased speed in filling clinical trials accelerates the process of finding out if a product under development is not going to be efficacious, thereby indicating to pharmaceutical companies to stop further clinical testing.
Specifically, before 1990, more than 80% of all pharmaceutical clinical trials were conducted at universities, today only 30% continue to be conducted in these settings (CenterWatch, 2005).
Within the global context of drug development, the pharmaceutical industry has also claimed that it is seeking “treatment naïve” human subjects in the developing world. According to this position, human subjects who have never received treatment for their illnesses are especially valuable test populations because they provide a more accurate assessment of the investigational product. Those analyzing the ethics of “treatment naïve” subjects (e.g., Petryna, 2006) must be cautious, however, not to buy into the pharmaceutical industry’s rhetoric and must instead be prepared to see this framing as “scientific” and “moral” justifications for enrolling vulnerable human subjects who have no other access to medical treatment.
Most notably, the cases of human subject abuse and research misconduct under inquiry by Congress were related to the U.S. Public Health Service’s Syphilis Study (Tuskegee) and widespread research on prisoners. For detailed discussions of these cases, see Jones (1981), Harkness (1996), Hornblum (1998), and Reverby (2000).
The explicit protection of Americans was indeed the intent and the effect of the regulation. Moreover, the regulation only covered – and continues to cover – human subjects research funded by or submitted to the U.S. government as evidence of product safety and efficacy. This means that research that is privately funded and is not submitted to the FDA is not subject to the regulation. For example, much of private-sector research on stem cells and human cloning is not regulated or overseen by the U.S. government.
These include the Institute of Medicine (IOM) and the Secretary’s Advisory Committee on Human Research Protections (SACHRP).
The model of research as collaboration may be particularly effective in social science or behavioral research. Participatory action research (PAR) has been hailed as a way to collect data on social problems while empowering human subjects who become participants in the research process. For a discussion of PAR, see Hall (1992) and Reason and Bradbury (2006).
These advertisements also serve to legitimate the pharmaceuticalization of many conditions. This seems to be particularly true in the domain of so-called lifestyle drugs like those targeting mood disorders. To extrapolate somewhat from David Healy (2006), advertisements for clinical trials that aim to recruit subjects for anxiety or depression studies further validate these psychological states as those that need pharmaceutical intervention regardless of whether individuals respond to the particular ad or ever volunteer for clinical trials.
This advertisement can be viewed online at http://www.trialbuilder.com/tv_friends_56.html. Last accessed on 11/16/06.
There has been some debate about the willingness of African Americans to participate in clinical trials. Some research has claimed that as a group, African Americans are suspicious of researchers due to past cases of exploitation (e.g., Corbie-Smith, Thomas, & St. George, 2002; Gamble, 2000). A smaller body of research has suggested that African Americans are no more or less suspicious of clinical research than are Whites, but that their lower level of participation is due to less access and knowledge of studies or due to the attitudes of African American physicians’ toward clinical trials (e.g., Brown & Topcu, 2003; Lynch, et al., 2001). I think both types of claims oversimplify past and present prejudices and structural reasons for African Americans’ participation or non-participation. I also find it problematic that the assumption of these types of studies about African Americans is often that participation in clinical trials is unequivocally in the best interest of this or any group. For discussions about the politics of inclusion of minorities in clinical studies, see King (2000) and Epstein (2004).
I should note that I am in no way making claims about the efficacy of the investigational drug that was being studied in this clinical trial. I am merely using this particular advertisement to illustrate implicit and explicit messages that are common in recruitment campaigns for clinical trials.
On direct-to-consumer advertising, see Fuqua (2002) and Ronald (2006).
Payment for participation in Phase I studies is determined by whether the study is in- or out-patient, the length of the study, the number of doses of the investigational drug, and the potential risks associated with the product. Advertisements for Phase I trials often announce that studies will “pay up to” $3500, and most studies pay over $1000. It is important to note that these studies, while generally safe, do have debilitating or fatal results, including a March 2006 Phase I study in London (Rosenthal, 2006) and a 2001 study at Johns Hopkins (Halpern, 2004).
Efficacy is determined in most industry-sponsored clinical trials by comparing the investigational drug to a placebo. This means that products under development have to be shown only to be better than nothing (i.e., a sugar pill) in order to receive approval by the FDA. In some cases of severe illness, it is impossible to randomize patients to a placebo arm of the study, but most pharmaceutical companies prefer placebo-controlled trials because they are considerably cheaper and because it is much easier to show efficacy (Fisher, 2005; Petryna, 2006).
It is quite unusual in the private sector for physicians to discuss informed consent with potential human subjects. This job is usually left to study staff, such as the research coordinator assigned to the study (Fisher, 2006b). In this case, the study was deemed sufficiently complex and risky, and the physician felt that he should conduct these interviews himself.
Belief in a therapeutic benefit to clinical studies when there is none is referred to as a “therapeutic misconception.” See Applebaum and Lidz (2006) for an important review of the literature and recommendations for minimizing these beliefs in human subjects. Elsewhere, I develop the concept of “procedural misconceptions” to highlight the ways in which clinical contexts can create false expectations about research in human subjects (Fisher, 2006a).
While my inclination is to problematize the paternalism that I witnessed in the relationship between the mother and son, it was impossible for me to determine the degree to which the woman had already been affected by Alzheimer’s disease. What is probably more worthy of discussion is the physician’s acceptance of the son’s role as decision-maker without evaluating the competency of the woman to make decisions for herself. For an interesting example of public controversy surrounding consenting on others’ behalf, see Chun and McEneaney (2006) who discuss the case of New York City orphans who were enrolled in HIV clinical trials with the consent of the city authorities.
These were the terms used to describe ongoing clinical trials in a recruitment call I received on my answering machine in January 2005.
One interviewee likened participation in Phase I studies to prostitution: “They’re paying a big amount of money to just use our bodies for that amount of time.”
References
- Anderson DL. A Guide to Patient Recruitment and Retention. Boston: Thomson CenterWatch; 2004. [Google Scholar]
- Applebaum PS, Lidz CW. The Therapeutic Misconception. In: Emanual EJ, et al., editors. The Oxford Textbook of Clinical Research Ethics. New York: Oxford University Press; 2006. [Google Scholar]
- Brown DR, Topcu M. Willingness to Participate in Clinical Treatment Research Among Older African Americans and Whites. The Gerontologist. 2003;43:62–72. doi: 10.1093/geront/43.1.62. [DOI] [PubMed] [Google Scholar]
- Caplan A. Due Consideration: Controversy in the Age of Medical Miracles. New York: John Wiley & Sons, Inc.; 1998. [Google Scholar]
- CenterWatch. An Industry in Evolution. 5th ed. Boston: Thomson CenterWatch; 2005. [Google Scholar]
- Chun M, McEneaney EH. Personhood and the Balance of Risk and Benefit: Analyzing the Participation of Foster Children in Clinical Trials. Paper presented at the American Sociological Association meetings in Montreal; Quebec, Canada. 2006. [Google Scholar]
- Corbie-Smith G, Thomas SB, St. George DMM. Distrust, Race, and Reasearch. Archives of Internal Medicine. 2001;162:2458–2463. doi: 10.1001/archinte.162.21.2458. [DOI] [PubMed] [Google Scholar]
- Corrigan OP. Empty Ethics: The Problem with Informed Consent. Sociology of Health and Illness. 2003;25:768–792. doi: 10.1046/j.1467-9566.2003.00369.x. [DOI] [PubMed] [Google Scholar]
- Epstein S. Bodily Differences and Collective Identities: The Politics of Gender and Race in Biomedical Research in the United States. Body & Society. 2004;10:183–203. [Google Scholar]
- Epstein S. Inclusion: The Politics of Difference in Medical Research. Chicago: University of Chicago Press; 2007. [Google Scholar]
- Epstein S. The Rise of “Recruitmentology”: Clinical Research, Racial Knowledge, and the Politics of Inclusion and Difference. Social Studies of Science. doi: 10.1177/0306312708091930. (N.D.) forthcoming. [DOI] [PubMed] [Google Scholar]
- Faden RR, Beauchamp TL. A History and Theory of Informed Consent. New York: Oxford University Press; 1986. [Google Scholar]
- Fisher JA. Ph.D. dissertation. Troy, NY: Rensselaer Polytechnic Institute; 2005. Pharmaceutical Paternalism and the Privatization of Clinical Trials. Unpublished. [Google Scholar]
- Fisher JA. Procedural Misconceptions and Informed Consent: Insights from Empirical Research on the Clinical Trials Industry. Kennedy Institute of Ethics Journal. 2006a;16(3):251–268. doi: 10.1353/ken.2006.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JA. Coordinating “Ethical” Clinical Trials: The Role of Research Coordinators in the Contract Research Industry. Sociology of Health and Illness. 2006b;28(6) doi: 10.1111/j.1467-9566.2006.00536.x. forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuqua JV. "Ask Your Doctor About…": Direct-to-Consumer Prescription Drug Advertising and the HIV/AIDS Medical Marketplace. Cultural Studies. 2002;16(5):650–672. [Google Scholar]
- Gamble VN. Under the Shadow of Tuskegee: African Americans and Healthcare. In: Reverby SM, editor. Tuskegee's Truths: Rethinking the Tuskegee Syphilis Study. Chapel Hill: University of North Carolina Press; 2000. pp. 431–442. [Google Scholar]
- Hall B. From Margins to Center? The Development and Purpose of Participatory Research. American Sociologist. 1992;22:15–28. [Google Scholar]
- Halpern SA. Lesser Harms: The Morality of Risk in Medical Research. Chicago: University of Chicago Press; 2004. [Google Scholar]
- Harkness JH. Ph.D. dissertation. Madison: University of Wisconsin; 1996. Research behind Bars: A History of Nontherapeutic Research on American Prisoners. Unpublished. [Google Scholar]
- Healy D. The New Medical Oikumene. In: Petryna A, Lakoff A, Kleinman A, editors. Global Pharmaceuticals: Ethics, Markets, Practices. Durham: Duke University Press; 2006. pp. 61–84. [Google Scholar]
- Hornblum AM. Acres of Skin: Human Experiments at Holmesburg Prison. New York: Routledge; 1998. [Google Scholar]
- Institute of Medicine. Responsible Research: A Systems Approach to Protecting Research Participants. Washington, D.C.: National Academies Press; 2002. [PubMed] [Google Scholar]
- Jones JH. Bad Blood: The Tuskegee Syphilis Experiment. New York: Free Press; 1981. [Google Scholar]
- King PA. The Dangers of Difference. In: Reverby SM, editor. Tuskegee's Truths: Rethinking the Tuskegee Syphilis Study. Chapel Hill: University of North Carolina Press; 2000. pp. 424–430. [Google Scholar]
- Lynch GF, Gorelick PB, Raman R, Leurgans S. A Pilot Survey of African-American Physician Perceptions about Clinical Trials. Journal of the National Medical Association. 2001;93(12):8S–13S. [PMC free article] [PubMed] [Google Scholar]
- Mirowski P, Van Horn R. The Contract Research Organization and the Commercialization of Scientific Research. Social Studies of Science. 2005;35(4):503–548. doi: 10.1177/0306312705052103. [DOI] [PubMed] [Google Scholar]
- Petryna A. Globalizing Human Subjects Research. In: Petryna A, Lakoff A, Kleinman A, editors. Global Pharmaceuticals: Ethics, Markets, Practices. Durham: Duke University Press; 2006. pp. 33–60. [Google Scholar]
- Rainville B. Strategic Outsourcing with Contract Research Organizations: Targeting Corporate Goals. Drug Information Journal. 2002;36(1):77–81. [Google Scholar]
- Reason P, Bradbury H, editors. Handbook of Action Research. Thousand Oaks: Sage; 2006. [Google Scholar]
- Reverby SM, editor. Tuskegee's Truths: Rethinking the Tuskegee Syphilis Study. Chapel Hill: University of North Carolina Press; 2000. [Google Scholar]
- Ronald L. Ph.D. dissertation. Troy, NY: Rensselaer Polytechnic Institute; 2006. Empowered to Consume: Direct-to-Consumer Advertising and Pharmaceutical Governance. Unpublished. [Google Scholar]
- Rosenthal E. British Rethinking Rules After Ill-Fated Drug Trial. New York Times. 2006 April 8; 2006. [PubMed] [Google Scholar]
- Sherwin S. Feminism and Bioethics. In: Wolf SM, editor. Feminism & Bioethics: Beyond Reproduction. New York: Oxford University Press; 1996. pp. 47–66. [Google Scholar]
- Sherwin S, editor. The Politics of Women's Health: Exploring Agency and Autonomy. Philadelphia: Temple University Press; 1998. [Google Scholar]
- Veatch RM. The Patient as Partner: A Theory of Human-Experimentation Ethics. Bloomington: Indiana University Press; 1987. [Google Scholar]
- Wolpe PR. The Triumph of Autonomy in American Bioethics: A Sociological Perspective. In: DeVries R, Subedi J, editors. Bioethics and Society: Constructing the Ethical Enterprise. Upper Saddle River, NJ: Prentice-Hall; 1998. pp. 38–59. [Google Scholar]


