SUMMARY
Objectives
Depression, loss, and physical illness are associated with suicide in the elderly. However, the nature of individual vulnerability remains poorly understood. Poor problem solving has been suggested as a risk factor for suicide in younger adults. Unresolved problems may create an accumulation of stressors. Thus, those with perceived deficits in problem-solving ability may be predisposed to suicidal behavior. To test this hypothesis, we investigated whether elderly suicide attempters perceived their problem solving as deficient.
Methods
Sixty-four individuals aged 60 and older participated in the study including depressed suicide attempters, depressed non-attempters, and non-depressed controls. The social problem solving inventory-revised: short-version was used to measure participants' perceived social problem solving, assessing both adaptive problem-solving dimensions (positive problem orientation and rational problem solving) and dysfunctional dimensions (negative problem orientation, impulsivity/carelessness, and avoidance).
Results
Depressed elderly who had attempted suicide perceived their overall problem solving as deficient, compared to non-suicidal depressed and non-depressed elderly. Suicide attempters perceived their problems more negatively and approached them in a more impulsive manner. On rational problem solving and avoidant style sub-scales, suicide attempters did not differ from non-suicidal depressed. However, both depressed groups reported lower rational problem solving and higher avoidance compared to non-depressed controls.
Conclusions
A perception of life problems as threatening and unsolvable and an impulsive approach to problem solving appear to predispose vulnerable elderly to suicide attempts.
Keywords: social problem solving, elderly, suicide attempt, depression
INTRODUCTION
Suicide accounted for almost 32 000 deaths in the United States in 2004 (CDC, 2005). The elderly make up a disproportionately high number of these suicide deaths and are more likely to succeed in their suicide attempts (Goldsmith et al., 2002). Depression is the most important established risk factor for suicide in late life (Conwell et al., 1996; Skoog et al., 1996; Turvey et al., 2002; Sokero et al., 2003; and Waern et al., 2002), however, most depressed elderly do not become suicidal. Thus, it is important to identify characteristics that distinguish suicidal elderly from other people with depression and that are potentially modifiable by targeted interventions.
It is believed that unresolved problems create an accumulation of stressors (Nezu and Ronan, 1988), and those with deficits in problem-solving ability are likely predisposed to hopelessness and suicidal behavior (Schotte and Clum, 1982, 1987; Evans et al., 1992; Priester and Clum 1993; and Rudd et al., 1994). Indeed, studies of young and mid-age suicide attempters (Evans et al., 1992; Levenson and Neuringer, 1971; Schotte and Clum, 1982, Linehan et al., 1987 and Pollock and Williams, 2004) and of adults with suicidal ideation (Linehan et al., 1987 and Schotte and Clum, 1987) find that suicidal individuals are poorer problem solvers, generating fewer solution options than do depressed non-suicidal individuals and healthy controls. A diathesis–stress–hopelessness model of suicidal behavior has been proposed by Schotte and Clum (1982, 1987) where problem-solving deficits contribute to hopelessness and depression, which, in turn, increase suicidal risk. In this model, the relationships among these constructs, rather than a single construct, are central to suicidal predisposition (Reinecke et al., 2001).
One's perception of his/her problem-solving ability may be particularly germane to suicidal behavior: in a mid-life suicidal psychiatric sample, deficits in perceived problem solving accounted for 55.4% of the variance in suicidal risk (D'Zurilla et al., 2004). Suicidal individuals tended to view problems as significant threats to their well-being and exhibited increased self-blame while doubting their ability to solve problems successfully. Ultimately, when they did attempt to solve problems, these individuals were prone to making attempts that tended to be narrowed, impulsive, careless, and incomplete (D'Zurilla et al., 1998).
Much research in the area of social problem-solving has been done in adolescents and young adults (Chang et al., 2007). While the elderly face the often intractable problems of loss and increasing dependence on caregivers, we are aware of only one study examining the relationship of problem solving and suicide in old age (Howat and Davidson, 2002). The authors found no differences on most measures of problem solving outcomes between suicide attempters, depressed elderly, and community controls. However, elderly suicide attempters were poorer at generating relevant means of reaching given outcomes to interpersonal problems than community controls. We believe that Howat and Davidson's mixed findings may be explained by the choice of the means-ends problem-solving procedure (MEPS), which assesses the outcomes of problem-solving, rather than one's self-perception of problem-solving ability: depressed elderly who perceive themselves as unable to solve problem may be primarily at risk for suicide. The inclusion of a few past suicide attempters in the comparison groups may have also diminished the study's ability to detect group differences.
To understand whether perceived deficits in problem solving were associated with suicidal behavior in late-life depression, we assessed self-perceptions of problem solving in a carefully clinically characterized group of 64 elderly with and without suicide attempts and depression. We hypothesized that depressed elderly with past suicide attempts would demonstrate poorer self-reported social problem-solving compared to never-suicidal depressed elderly and to non-depressed elderly controls.
METHODS
Participants
Sixty-four individuals, aged 60 and older, with a score of at least 18 on the mini-mental state exam (Folstein et al., 1975) participated in the study. All participants provided written informed consent as required by the University of Pittsburgh Institutional Review Board. Clinical and demographic characteristics of the three groups are given in Table 1. We compared depressed elderly attempters to (1) non-suicidal depressed elders and (2) non-depressed controls in order to assess the effect of depression and suicidality on perceived problem-solving abilities.
Table 1.
Demographic and clinical characteristics (standard deviations in parentheses)
| Depressed attempter (A) n = 18 |
Non-suicidal depressed (D) n = 27 |
Non-depressed control (C) n = 19 |
p | Post-hoc | |
|---|---|---|---|---|---|
| Age | 67.9 (7.5) | 74.0 (8.9) | 69.2 (8.6) | .043 | |
| Men (%) | 50 | 41 | 68 | .18 | |
| White (%) | 78 | 81 | 89 | .62 | |
| Married (%) | 33 | 41 | 63 | .16 | |
| Education in years | 13.2 (3.5) | 14.3 (2.9) | 15.5 (2.8) | .054 | |
| Burden of physical illness (CIRS-Ga total) | 8.8 (3.6) | 9.6 (3.5) | 8.2 (3.0) | .67 | |
| HRSD-16b | 22.5 (5.8) | 19.0 (4.1) | 2.8 (2.0) | .0001 | A,D > C |
| MMSEc | 27.7 (2.2) | 27.6 (2.9) | 27.6 (1.8) | .95 | |
| Hopelessness (BHSd) | 8.7 (5.2) | 5.4 (5.7) | 1.8 (1.7) | .0002 | A,D > C |
| DRSe raw score | 132.0 (4.4) | 133.7 (6.6) | 134 (6.1) | .68 | |
| DRS scaled | 7.3 (2.0) | 8.8 (2.3) | 8.3 (1.7) | .099 |
CIRS-G—cumulative illness rating scale adapted for geriatrics.
Hamilton depression rating scale score minus the suicide item score.
MMSE—mini-mental status examination.
BHS—Beck hopelessness scale.
DRS—dementia rating scale.
Non-suicidal depressed participants and depressed suicide attempters met criteria for major depressive disorder or depressive disorder NOS as diagnosed by Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (SCID/DSM-IV), and they were recruited from the inpatient psychogeriatric unit and from the late-life depression research clinic at the University of Pittsburgh. Depressed participants were assessed at the beginning of treatment for the index depressive episode. Patients were excluded from the study if they had bipolar disorder, schizophrenia, schizoaffective disorder, or sensory disorders that precluded cognitive testing.
Depressed Suicide Attempters
Eighteen elderly participants who either (1) attempted suicide during the index episode or (2) had a previous suicide attempt and severe suicidal ideation in the current episode, requiring an inpatient admission or an increase in the level of care.
Non-Suicidal Depressed Participants
Twenty-seven comparison participants with no lifetime history of suicide attempts and no current suicidal ideation as defined by scores of 0 on the Beck's scale for suicidal ideation (Beck et al., 1999).
Non-depressed Controls
Nineteen elderly with no lifetime diagnosis of any SCID/DSM-IV Axis I disorder were recruited from university and community primary care practices. Care was taken to equate physical illness burden with those in the other two study groups. As with the non-suicidal depressed participants, they were required to have no lifetime history of suicide attempts and no current suicidal ideation as defined by scores on the Beck's scale for suicidal ideation.
Problem solving measures
The Social Problem Solving Inventory-revised Short-version (SPSI-R:S)
SPSI-R:S was used to measure participants' perceptions of their social problem-solving ability. This 25-item, self-report instrument assesses both constructive/adaptive problem-solving dimensions (positive problem orientation and rational problem solving) and three dysfunctional dimensions (negative problem orientation, impulsivity/carelessness, and avoidance). Positive problem-solving orientation captures a sense of one's constructive, cognitive schema: challenge, self-efficacy, and optimism. Negative problem-solving orientation assesses inhibitive cognitions and emotions: threat, self-blame, self-inefficacy, pessimism, and anger. Rational problem solving includes the systematic utilization of effective problem-solving principles and techniques: problem definition and formulation, generation of alternative solutions. The impulsive/careless style is described as narrow, hurried, and inadequate, and avoidance is characterized by procrastination, passivity/inactivity, and dependency on others to solve one's problems (D'Zurilla et al., 1998, 2002, 2004). High scores on positive problem-solving orientation and rational problem-solving and low scores on negative problem-solving orientation, impulsivity/carelessness, and avoidance indicate of positive evaluations of social problem solving ability. Normative data for the SPSI-R come from over 2350 individuals, including healthy elderly, depressed adults, and suicidal adults. Plotted raw scores are converted to standard scores. Previous psychometric evaluation of SPSI-R among a variety of patient populations suggests strong internal consistency (Cronbach's a α > 0.9) that is stable over time (D'Zurilla et al., 2002).
Clinical characterization
The 17-item Hamilton Depression Rating Scale (HAM-D)
HAM-D was used to assess presence and severity of current depressive symptoms (Hamilton, 1967). In analyses, we omitted the HAM-D item assessing suicidality in order to reduce potential co-linearity with group status.
Beck Hopelessness Scale (BHS)
BHS was used to measure participants' hopelessness. The instrument consists of 20 statements that describe positive and negative thoughts about the future (Beck et al., 1993).
Beck's Scale for Suicidal Ideation (SSI)
SSI was used to measure suicidal ideation. This 19-item, interviewer-rated measure of suicidal ideation was shown to predict eventual suicide (Beck et al., 1999), and has been validated in older depressed patients (Bruce et al., 2004).
Suicidal Intent Scale (SIS)
SIS was used to assess the severity of suicidal intent associated with the suicide attempts (Beck et al., 1974). This 15-item questionnaire yields a total score of 0–30, where higher scores indicate high intent.
Beck Suicide Lethality Scale (LS)
LS was used to assess medical lethality of suicide attempts (Beck et al., 1974).
Cumulative Illness Rating Scale adapted for Geriatrics (CIRS-G)
CIRS-G was used to assess illness burden in each of 13 different organ systems (Miller et al., 1992). CIRS-G data were gathered from participants' electronic health records and verified by personal interviews.
Mini-mental status examination (MMSE) (Folstein et al., 1975), and the Mattis dementia rating scale (DRS) were used to assess global cognition (Mattis, 1988).
Intra-class correlation coefficients measuring inter-rater reliability among our assessors in 2007 were: 0.95 for Hamilton rating scale of depression, 0.94 for cumulative illness rating scale for geriatrics, 0.98 for MMSE, 0.997 for DRS. SCID diagnoses were reviewed at consensus case conferences attended by at least two board-certified psychiatrists.
Statistical analysis
Data analysis was performed using SAS software v 9.2 (SAS Institute, Cary, NC). We compared groups on demographic and clinical characteristics using analysis of variance (ANOVA) for continuous measures and χ2 test for categorical measures. Correlations between SPSI-R subscores were calculated and, subsequently, factor analysis was performed using promax rotation since all factors were from same the instrument. Analysis of covariance (ANCOVA) was used to compare SPSI-R and subscale scores between the three groups controlling for education. Square root transformation was made on scores measuring avoidant and impulsive/careless problem solving prior to statistical comparison. Age was not used as a covariate as raw scores on the SPSI-R were converted to age-specific scores using previously validated conversions for this instrument (found in D'Zurilla et al., 2002). Tukey post-hoc tests are reported on significant results.
RESULTS
Group characteristics
There were no significant differences between groups in sex, race, or marital status (Table 1). As at post-hoc comparison there was a significant difference between groups with respect to age and there was a trend for education being different among groups, we used education as a covariate in the analyses of SPSI-R scores, as age is taken into account when converting from raw to scaled scores.
The groups did not differ in the burden of physical illness (CIRS-G) and general cognitive functioning (MMSE and DRS). The two depressed groups were not different in the severity of depression measured by the HAM-D (excluding the suicide item) nor in level of hopelessness, measured by BHS. With regard to comorbidities, 7/18 (39%) suicide attempters and 3/27 (11%) non-suicidal depressed had a lifetime diagnosis of substance use disorder (χ2=4.82, df=1, p=.028), while 5/18 (28%) suicide attempters and 12/27 (44%) non-suicidal depressed had a lifetime diagnosis of anxiety disorder (χ2=1.28, df=1, p=.26).
Suicide attempters were characterized by high lethality of suicide attempts (mean[SD]=3.7[2.0]), with 8/16 scoring 4 or higher (0=minimal damage, 3 or higher=hospitalization, 8=death). The attempts were also characterized by strong suicidal intent (mean[SD]=16.8[5.1]), median of 17. Current suicidal ideation among attempters was also high (mean[SD]=22.2[7.7]).
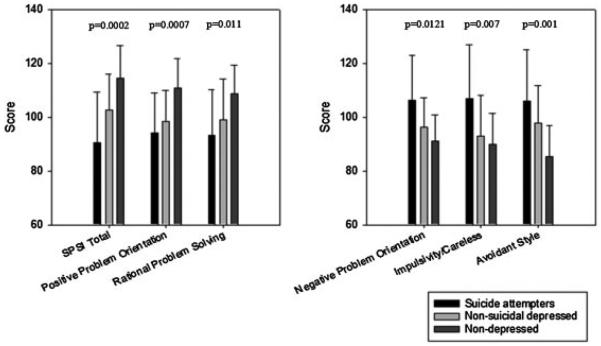
Problem solving and suicidal behavior
Self-reported aggregate perceptions of problem-solving ability were poorer in suicide attempters than in non-suicidal depressed and highest in non-depressed controls (Figure 1). Suicide attempters (A) did not differ from non-suicidal depressed elderly (D) in positive problem orientation, but both depressed groups exhibited lower scores than non-depressed controls (C) (A : mean[SD]=94.2[14.9], D: 98.4[11.4], C : 110.9[10.9], F[2,60]=8.16, p=0.0007). Suicide attempters reported higher negative problem solving orientation than either depressed or non-depressed controls (A : 106.2 [16.7], D : 96.1[11.2], C : 91.1[9.8], F[2,60] = 4.75 p=0.012). Suicide attempters perceived themselves as more impulsive/careless than non-suicidal depressed and non-depressed participants (A=107.7[19.9], D: 93.0[15.0], C: 89.8[11.5], F[2,60]=5.39, p=0.007).
Figure 1.
Problem-solving and suicidal behavior: social problem solving inventory scores and subscores with SD and p-values. Left illustrates SPSI total, positive problem orientation, and rationale problem solving (higher scores indicate adaptive problem solving). Right illustrates negative problem orientation, impulsive/careless, and avoidant style (lower scores indicate adaptive problem solving).
On rational problem solving and avoidant style sub-scales, suicide attempters did not differ from non-suicidal depressed. However, attempters reported lower rational problem solving and higher avoidant style compared to non-depressed controls (rational problem solving, A : 93.2[16.9], D: 99.1[15.0], C: 108.6[10.7], F[1,60] = 4.85, p=0.011; avoidant style, A: 106.1[19.1], D: 97.7[14.1], C: 85.4[11.4], F[2,60] = 7.73, p = 0.001).
Effect sizes for differences between suicide attempters and non-suicidal depressed proved to be large for SPSI total (Cohen's d=−0.76), impulsivity/carelessness (0.86), and negative problem orientation (0.74). Small to medium effect sizes were found for the statistically insignificant differences in rational problem-solving (−0.37), positive problem orientation (−0.33), and avoidance (0.52).
Data reduction: dysfunctional and adaptive problem solving factors
To account for high inter-correlations between subscales of (1) negative orientation, impulsivity, and avoidance and (2) positive orientation and rational problem solving (data not shown) and to control type I error, we further reduced the data with an exploratory factor analysis. The scree plot and the eigen criteria suggested that a two factor model should be retained. Mirroring our findings with single subscale scores, suicide attempters scored higher on the ‘dysfunctional problem-solving factor’ (negative problem orientation, impulsivity/carelessness, and avoidance; accounted for 41% of variance before rotation) than either non-suicidal depressed or non-depressed elderly (F[2,61]=8.93, p=0.0004). In contrast, both depressed groups scored lower on the ‘adaptive problem-solving factor’ (positive problem-solving orientation, rational problem-solving; accounted for 29% of variance) than non-depressed elderly (F[2,61]=7.93, p=0.0009).
Substance use disorders, anxiety, and problem solving
Sensitivity analyses examining lifetime diagnoses of substance use or anxiety disorders as covariates did not qualitatively change any of the results for total problem solving or subscale scores. Specifically, the lifetime diagnosis of a substance use disorder predicted lower total problem solving scores and higher negative problem orientation, impulsivity, and avoidance scores. However, the inclusion of substance use disorders in the model did not change the relationship between suicidal behavior and measures of problem solving. Lifetime anxiety disorders were not significantly related to any of the problem solving measures (data not shown).
DISCUSSION
Depressed elderly who had attempted suicide perceived their overall problem-solving as dysfunctional, compared to non-suicidal depressed and non-depressed elderly. Suicide attempters perceived their problems more negatively and approached them in a more impulsive manner. These results parallel those seen in younger populations (Dixon et al., 1991; Rudd et al., 1994; and Schotte and Clum, 1987), suggesting that perceived problem-solving deficits are an important correlate of attempted suicide in the elderly.
In our study, only negative problem orientation and impulsive/careless style distinguished between attempters and non-suicidal depressed. Similar results were found by Reinecke et al., (2001) in adolescents, where negative problem orientation, avoidance, and impulsiveness were related to suicidal behavior. Thus, negative problem orientation is consistently associated with attempted suicide. It is worth remembering that problem-orientation reflects perceived control and ability to handle and cope with a problem. As described by D'Zurilla et al. (2004), those with a negative problem orientation are more likely to view a problem as a threat to their well-being, have self-doubt in their problem-solving abilities, and more quickly become distressed when faced with a problem. Therefore, it is not surprising that negative problem orientation is associated with attempted suicide in depressed elderly, who face loss, illness, disability, and dependence. Our findings parallel Williams's notion of ‘entrapment’, where perceived inability to get away from an aversive environment is theorized to set off escape motivations that lead to suicide attempts (Williams et al., 2005).
In finding that elderly suicide attempters approach their problems more impulsively than non-suicidal depressed elderly, our study is perhaps the first to contradict the common clinical view of late-life suicide attempters and those who die by suicide as being non-impulsive. It is remarkable that this difference persisted even after accounting for comorbid substance use disorders. Plausibly, impulsiveness can both lead to an accumulation of stressors and facilitate suicidal behavior as a dysfunctional solution. On the other hand, a careless approach to problems represents only one facet of impulsivity. The complex nature of this phenomenon and varying ways of assessing it have given rise to conflicting findings in younger adults and adolescents, where some studies point to an association with suicidal behavior (Mann et al., 1999), while others fail to find it (Oquendo et al., 2004; Renaud et al., 2008; Soloff et al., 2005; and Witte et al., 2008). One explanation that may account for some of the discrepancies is that in vulnerable individuals impulsivity is accentuated in a suicidal crisis, while at other times it may not be as apparent. Since we assessed our participants during a depressive episode with intense suicidal ideation, our approach may be more sensitive to state-modulated differences in impulsivity.
In our study, suicide attempters and non-suicidal depressed patients did not differ in rational problem solving. This finding is consistent with past research (D'Zurilla et al., 1998 and Reinecke et al., 2001) and, if not due to low power, could suggest that deficiencies in potential solution generation and problem definition may not contribute to one's ultimate decision to attempt suicide as much as negative orientation to problems and the tendency to be more impulsive. This becomes important when one considers that many therapies aimed at treating depression and preventing suicide place an emphasis on improving patients' rational problem-solving abilities (Reinecke et al., 2001).
There are several strengths of the current study. The use of the SPSI-R allowed us to examine the process of problem solving as perceived by elderly suicide attempters. Assessing the process of problem-solving is important for assessing deficits, planning an individualized training program and its progress, and making predictions about adaptational outcomes (D'Zurilla and Nezu, 1990). An outcome measure like the MEPS does provide one with an overall sense of the quality of patients' solutions, but does not offer specific information about the components of social problem-solving ability (D'Zurilla and MaydeuOlivares, 1995; D'Zurilla et al., 2004). Also, as pointed out by Linehan et al. (1987), the standard MEPS test is not sensitive enough to discern between passive and active responses which is important in determining if the individual is taking an active role in solving his/her problems versus relying on others or time to solve the problems. Additional strengths of the study include its extensive clinical and cognitive characterization of study participants and inclusion of actual suicide attempters instead of ideators, increasing the clinical relevance of our findings.
Limitations to the current study should be noted as well. The first relates to the self-report nature of the SPSI-R. Though past studies in non-elderly samples suggest that self-report measures of perceived problem-solving ability parallel observer-rated problem-solving effectiveness (Nezu and Ronan, 1988 and MacLeod et al., 1992), external ratings of problem-solving abilities or behavioral observations of social problem-solving would improve validation of the current findings. An optimal design would measure the perception, the process, as well as the outcome of problem solving. Second, the cross-sectional nature of our study precludes definitive causal inferences. For instance, whether one's responses on the SPSI-R were indicative of their pre-attempt problem solving ability or were in some way affected by their suicide attempt is not entirely clear. A more prospective approach, though potentially difficult when exploring correlates of suicidal behavior, would certainly allow for cause and effect to be more clearly delineated. Third, in order to better identify if problem solving deficits are uniquely associated with suicidal behavior or these deficits are common in other depressed older adults with suicidal ideation, inclusion of a group of suicidal ideators (with no history of suicide attempt) would be necessary. Inclusion of such a group in a future prospective study could better separate ideators and attempters. Fourth, our sample, though large enough to allow important differences to be detected between attempters and depressed non-attempters in areas of orientation and impulsivity, may have been too small to detect differences in rational problem solving skills among the depressed groups. Last, though care was taken to match demographic differences between groups, suicide attempters tended to be less educated, as seen in psychological autopsy studies (Pompili et al., 2008). It is possible that increased education may confound problem-solving's actual role in suicidal risk even though we controlled for education in our analyses.
Clinical implications
Treatments for vulnerable depressed elderly that target negative and impulsive approaches to problems may help them break the cycle of accumulating stressors, hopelessness, and suicidal behavior. One such treatment shown to improve depressive symptoms (Alexopoulos et al., 2003), reduce feelings of hopelessness, and increase one's ability to cope with problems (MacLeod et al., 1992 and Williams and Pollock, 1993) is problem solving therapy (PST). In the supplemental material, we present a case of an older man with depression and past suicide attempts, who received PST in our clinic. The case illustrates how PST builds on the stress-diathesis model, enabling individuals to cope with problems more effectively thereby preventing or lessening depressive symptoms and hopelessness when one faces stress (Nezu and Ronan, 1988). It also shows that psychotherapy for suicidal elderly has to not only improve rational problem solving skills, but also help them overcome the negative problem orientation and impulsive approach to problems (refer to Case Vignette in Supplementary data).
Further, our study suggests the importance, of not only actual, but perceived aspects of problem solving. Cognitive therapy (Beck, 1979) explicitly addresses individuals' perceptions of their own functioning, helping them to understand the extent to which their negative views of themselves may be inaccurate and unhelpful. Brown and colleagues showed that a cognitive intervention designed to help individuals develop adaptive ways of coping with stressors decreased severity of self-reported depression and feelings of hopelessness in younger adults with recent suicide attempts. Participants receiving cognitive therapy were approximately 50% less likely to attempt suicide during the study's 18-month follow-up period (Brown et al., 2005). While our findings support the use of cognitive therapy in elderly at risk for suicide, its relative complexity may pose a challenge for these patients, who demonstrate significant cognitive impairment (Dombrovski et al., 2008). Thus, adaptations, similar to those undertaken by Alexopoulos et al. for PST (Alexopoulos et al., 2003) may be needed.
In summary, our findings of a negative and impulsive approach to problems in elderly suicide attempters point to a need for treatments that would remediate these deficits. While both problem-solving therapy and cognitive therapy provide potentially useful approaches, either therapy would require modifications to target the suicide diathesis in late life.
ACKNOWLEDGEMENTS
This research is supported by grant NIMH K23 MH070471 and an American Foundation of Suicide Prevention Mentored Junior Investigator Award to Katalin Szanto, and by the John A. Hartford Foundation for Alexandre Y. Dombrovski.
Footnotes
CONFLICT OF INTEREST
None declared.
SUPPORTING INFORMATION
Supporting information may be found in the online version of this article.
REFERENCES
- Alexopoulos GS, Raue P, Arean P. Problem-solving therapy versus supportive therapy in geriatric major depression with executive dysfunction. Am J Geratr Psychiatry. 2003;11(1):46–52. [PubMed] [Google Scholar]
- Beck AT. Cognitive Therapy of Depression. Guilford Press; New York: 1979. [Google Scholar]
- Beck AT, Schuyler D, Herman I. Development of suicidal intent scales. In: Beck AT, Resnick HCP, Lettieri, editors. The Prediction of Suicide. Charles Press; Bowie: 1974. [Google Scholar]
- Beck AT, Brown GK, Steer RA, Dahlsgaard KK, Grisham JR. Suicide ideation at its worst point: a predictor of eventual suicide in psychiatric outpatients. Suicide Life Threat Behav. 1999;29(1):1–9. [PubMed] [Google Scholar]
- Beck AT, Steer RA, Beck JS, Newman CF. Hopelessness, depression, suicidal ideation, and Clinical diagnosis of depression. Suicide Life Threat Behav. 1993;23(2):139–145. [PubMed] [Google Scholar]
- Brown GK, Ten Have T, Henriques GR, et al. Cognitive therapy for the prevention of suicide attempts. JAMA. 2005;294(5):563–570. doi: 10.1001/jama.294.5.563. [DOI] [PubMed] [Google Scholar]
- Bruce ML, Ten Have TR, Reynolds CF, 3rd, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Web-based Injury Statistics Query and Reporting System (WISQARS) [Online] National Center for Injury Prevention and Control, CDC (producer) 2005 Available from URL: www.cdc.gov/ncipc/wisqars/default.htm. [Google Scholar]
- Chang EC, D'Zurilla TJ, Sanna LJ. Social problem solving as a mediator of the link between stress and psychological well-being in middle-adulthood. Cognitive Therapy and Research. 2007 e-publication. http://online5.hsls.pitt.edu:2073/content/gx948135834 wx6t6/fulltext.html (accessed 15 June 2008) [Google Scholar]
- Conwell Y, Duberstein PR, Cox C, et al. Relationships of age and axis I diagnosis in victims of completed suicide: a psychological autopsy study. Am J Psychiatry. 1996;153(8):1001–1008. doi: 10.1176/ajp.153.8.1001. [DOI] [PubMed] [Google Scholar]
- D'Zurilla TJ, Chang EC, Nottingham EJI, et al. Social problem-solving deficits and hopelessness, depression, and suicidal risk in college students and psychiatric inpatients. J Clin Psychol. 1998;54(8):1091–1107. doi: 10.1002/(sici)1097-4679(199812)54:8<1091::aid-jclp9>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- D'Zurilla TJ, Maydeu-Olivares A. Conceptual and methodological issues in social problem-solving assessment. Behav Ther. 1995;26(3):409–432. [Google Scholar]
- D'Zurilla TJ, Nezu AM. Development and preliminary evaluation of the Social Problem-Solving Inventory. Psychol Asses: A J Consult Clin Psychol. 1990;2(2):156–163. [Google Scholar]
- D'Zurilla T, Nezu AM, Maydeu-Olivares A. Social Problem Solving Inventory-revised (SPSI-R) Multi-health Systems Inc; North Tonawanda NY: 2002. [Google Scholar]
- D'Zurilla TJ, Nezu AM, Maydeu-Olivares A. Social problem solving: theory, research, and assessment. In: Chang EC, D'Zurilla TJ, Sanna LJ, editors. Social Problem-Solving: Theory, Research, and Training. American Psychological Association; Washington, DC: 2004. pp. 11–27. [Google Scholar]
- Dixon WA, Heppner PP, Anderson WP. Problem-solving appraisal, stress, hopelessness, and suicide ideation in a college population. J Counsel Psychol. 1991;38(1):51–56. [Google Scholar]
- Dombrovski AY, Butters MA, Reynolds CF, et al. Cognitive performance in suicidal depressed elderly: preliminary report. Am J Geriatr Psychiatry. 2008;16:109–115. doi: 10.1097/JGP.0b013e3180f6338d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans J, Williams JMG, O'Loughlin S, Howells K. Autobiographical memory and problem-solving strategies of parasuicide patients. Psychol Med. 1992;22:399–405. doi: 10.1017/s0033291700030348. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state,” a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE, editors. Reducing Suicide: A National Imperative. National Academy Press; Washington, DC: 2002. [PubMed] [Google Scholar]
- Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- Howat S, Davidson K. Parasuicideal behaviour and interpersonal problem solving performance in older adults. Br J Clin Psychol. 2002;41:375–386. doi: 10.1348/014466502760387498. [DOI] [PubMed] [Google Scholar]
- Levenson M, Neuringer C. Problem solving behavior in suicidal adolescents. J Consult Clin Psychol. 1971;37:433–436. doi: 10.1037/h0031985. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Camper P, Chiles JA, Strosahl K, Shearin E. Interpersonal problem solving and parasuicide. Cognit Ther Res. 1987;11(1):1–12. [Google Scholar]
- MacLeod AK, Williams JMG, Linehan MM. New developments in the understanding and treatment of suicidal behaviour. Behav Psycother. 1992;20(3):193–218. [Google Scholar]
- Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156(2):181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- Mattis S. Psychological Assessment Resources. Odessa, FL: 1988. Dementia rating scale (DRS) [Google Scholar]
- Miller MD, Paradis CF, Houck PR, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the cumulative illness rating scale. Psych Res. 1992;41(3):237–248. doi: 10.1016/0165-1781(92)90005-n. [DOI] [PubMed] [Google Scholar]
- Nezu AM, Ronan GF. Social problem solving as a moderator of stress-related depressive symptoms: a prospective analysis. J Couns Psychol. 1988;35(2):134–138. [Google Scholar]
- Oquendo MA, Galfalvy H, Russo S, et al. Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. Am J Psychiatry. 2004;161(8):1433–1441. doi: 10.1176/appi.ajp.161.8.1433. [DOI] [PubMed] [Google Scholar]
- Pollock LR, Williams JMG. Problem-solving in suicide attempters. Psychol Med. 2004;34:163–167. doi: 10.1017/s0033291703008092. [DOI] [PubMed] [Google Scholar]
- Pompili M, Innamorati M, Masotti V, et al. Suicide in the elderly: a psychological autopsy study in a north Italy area (1994–2004) Am J Geriatr Psychiatry. 2008;16:727–735. doi: 10.1097/JGP.0b013e318170a6e5. [DOI] [PubMed] [Google Scholar]
- Priester MJ, Clum GA. Perceived problem-solving ability as a predictor of depression, hopelessness, and suicide ideation in a college population. J Counsel Psychol. 1993;40:79–95. [Google Scholar]
- Reinecke MA, DuBois DL, Schultz TM. Social problem solving, mood, and suicidality among inpatient adolescents. Cognit Ther Res. 2001;25(6):743–756. [Google Scholar]
- Renaud J, Berlim MT, McGirr A, Tousignant M, Turecki G. Current psychiatric morbidity, aggression/impulsivity, and personality dimensions in child and adolescent suicide: a case-control study. J Affect Disord. 2008;105(1–3):221–228. doi: 10.1016/j.jad.2007.05.013. [DOI] [PubMed] [Google Scholar]
- Rudd MD, Rajab MH, Dahm PF. Problem-solving appraisal. in suicide ideators and attempters. Am J Orthopsychiatry. 1994;64(1):136–149. doi: 10.1037/h0079492. [DOI] [PubMed] [Google Scholar]
- Schotte DE, Clum GA. Suicide ideation in a college population: a test of a model. J Consult Clin Psychol. 1982;50:690–696. doi: 10.1037//0022-006x.50.5.690. [DOI] [PubMed] [Google Scholar]
- Schotte DE, Clum GA. Problem-solving skills in suicidal psychiatric patients. J Consult Clin Psychol. 1987;55(1):49–54. doi: 10.1037//0022-006x.55.1.49. [DOI] [PubMed] [Google Scholar]
- Skoog I, Aevarsson O, Beskow J, et al. Suicidal feelings in a population sample of nondemented 85-year-olds. Am J Psychiatry. 1996;153(8):1015–1020. doi: 10.1176/ajp.153.8.1015. [DOI] [PubMed] [Google Scholar]
- Sokero TP, Melartin TK, Rytsala HJ, et al. Suicidal ideation and attempts among psychiatric patients with major depressive disorder. J Clin Psychiatry. 2003;64(9):1094–1100. doi: 10.4088/jcp.v64n0916. [DOI] [PubMed] [Google Scholar]
- Soloff PH, Fabio A, Kelly TM, Malone KM, Mann JJ. High-lethality status in patients with borderline personality disorder. J Pers Disord. 2005;19(4):386–399. doi: 10.1521/pedi.2005.19.4.386. [DOI] [PubMed] [Google Scholar]
- Turvey CL, Conwell Y, Jones MP, et al. Risk factors for late-life suicide: a prospective, community-based study. Am J Geriatr Psychiatry. 2002;10(4):398–406. [PubMed] [Google Scholar]
- Waern M, Runeson BS, Allebeck P, et al. Mental disorder in elderly suicides: a case-control study. Am J Psychiatry. 2002;159(3):450–455. doi: 10.1176/appi.ajp.159.3.450. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Pollock LR. Factors mediating suicidal behavior: their utility in primary and secondary prevention. J Ment Health. 1993;2(1):3–26. [Google Scholar]
- Williams JMG, Crane C, Barnhofer T, Duggan D. Psychology and suicidal behaviour: elaborating the entrapment model. In: Hawton K, Van Herringen K, editors. Understanding Suicidal Behavior: The Suicidal Process Approach to Research, Treatment and Prevention. 2nd edn Wiley; Chichester: 2005. pp. 71–89. [Google Scholar]
- Witte TK, Merrill KA, Stellrecht NE, et al. “Impulsive” youth suicide attempters are not necessarily all that impulsive. J Affect Disord. 2008;107(1–3):107–116. doi: 10.1016/j.jad.2007.08.010. [DOI] [PubMed] [Google Scholar]