Abstract
Objective
Models that explain preventive behaviors, such as colorectal cancer (CRC) screening, do not account for social and cultural factors relevant to African Americans. This exploratory study examined the relationship between socio-cultural factors (e.g., traditional acculturative strategy, group-based medical mistrust, physician ethnicity, and group-level perceptions of susceptibility) and perceived benefits, perceived barriers, and CRC screening intentions among African Americans (N = 198; Age: M = 59.7, SD = 9.9; 65% female; 44% household income $50,000+).
Design
Hierarchical multiple regression was used to test the following models: Traditional Acculturative Strategy × Medical Mistrust; b) Physician’s Ethnicity × Medical Mistrust; c) Group Susceptibility × Medical Mistrust; and d) Group Susceptibility × Traditional Acculturative Strategy.
Results
Results revealed that perceiving high group susceptibility while being both more culturally traditional and less mistrustful was associated with more perception of screening benefits. Greater intention to be screened was associated with perceiving high group susceptibility while being more traditional and with low levels of mistrust in those with African American physicians.
Conclusion
These results suggest that it may be beneficial to include social and cultural factors in behavioral interventions to increase CRC screening among African Americans.
Keywords: Colorectal cancer, screening, African American, culture
Introduction
Colorectal cancer (CRC) is the third leading type of cancer and the third leading cause of cancer deaths among African Americans, and African Americans are 40% more likely than Whites to die of the disease (American Cancer Society, 2005). CRC incidence rates also are higher for African Americans compared to Whites (American Cancer Society 2007b). More than half of the excess CRC mortality among African Americans is attributable to advanced stage disease, and 5-year survival rates are worse for African Americans than for Whites (Bradley et al. 2001, Ghafoor et al. 2002, American Cancer Society 2005, American Cancer Society 2007b). In addition, only 38.9% of African Americans aged 50+ years have had CRC screening within recommended guidelines compared to 44.2% of Whites (American Cancer Society 2007a). Because of the increased risk of CRC among African Americans, it has been recently suggested that this population begin CRC screening at age 45 (Agrawal et al. 2005).
Although several theoretical frameworks have been proposed to understand CRC screening behavior, most studies have not included social and cultural variables relevant in this specific minority population (Becker 1974, Janz and Becker 1984, Myers et al. 1994). Studies that accurately reflect this within-group variability while accounting for broad cultural commonalities offer the opportunity to identify salient social and cultural factors that either facilitate or impede the adoption of preventive health behaviors, like CRC screening.
Theorists and researchers have consistently noted that traditional African American cultural values and assumptions emphasize a collectivist cultural orientation as well as an adaptive mistrust of mainstream institutions (i.e., cultural mistrust) that is based upon a history of racial discrimination (Terrell and Terrell 1981, Myers 1993, Parham et al. 1999). The collectivist outlook characteristic of traditional African American cultural orientation and a history of discrimination may result in an increased emphasis on threats to the group, including health threats such as cancer. It is possible that this perception of group-level susceptibility may influence attitudes towards preventive health behaviors and may motivate African Americans to complete CRC screening (Ashing-Giwa 1999). Prevailing cultural patterns notwithstanding, it is important to account for the considerable variability in African American models of cultural expression. One way of addressing this within-group diversity is by examining African American acculturation, which attempts to identify individuals who have maintained a traditional African American cultural orientation versus embracing mainstream cultural values (Landrine and Klonoff 1996, Snowden and Hines 1999, Obasi 2004). Studies have shown a significant relationship between acculturation and health behaviors, including cancer screening in Asian American, Native American and Hispanic populations (Risendal et al. 1999, Tang et al. 1999, Maxwell et al. 2000, Tang et al. 2001, Honda 2004, Abraido-Lanza et al. 2005, Honda and Gorin 2005, Shah et al. 2006), and more recently among African Americans (Landrine et al. 1996, Snowden and Hines, 1998, Ard et al. 2005). In general, individuals with a more traditional, or less acculturated, cultural orientation have been screened at lower rates.
Patient trust of physicians is one of the strongest correlates of adherence to medical recommendations and treatments (Safran et al. 1998, Thom et al. 1999, O’Malley et al. 2004) and good provider-patient communication has been associated with completing CRC screening within recommended guidelines (Katz et al. 2004). Due to experiences of discrimination, African Americans may be more mistrustful of physicians and more dissatisfied with health care than Whites (LaVeist et al. 2000). Examining the construct of group-based medical mistrust (i.e., suspicion of the treatment provided to an individual’s racial or ethnic group by mainstream health care systems and health professionals) investigators have reported that medical mistrust is associated with poorer adherence to breast cancer screening recommendations (Thompson et al. 2004). However, African Americans with physicians of the same race are more likely to rate their physician as excellent and to report receiving preventive care (Saha et al. 1999). This finding suggests that mistrust may be attenuated and the quality of care enhanced by having a physician of the same race. However, there are very few rigorous studies examining the impact of race concordance on patient mistrust and patient care.
This exploratory study examined the relationship between social and cultural factors (i.e., group-level perceptions of susceptibility to colorectal cancer, African American acculturation, physician ethnicity, and group-based medical mistrust) and perceived benefits, perceived barriers, and intention to be screened for colorectal cancer. In related work, we have established that these factors are related to CRC screening attitudes and intentions (Purnell and Andersen 2007). In this study we were interested in whether these variables interacted with one another in influencing screening benefits, barriers, and intentions.
Methods
Recruitment and Characteristics of Participants
This cross-sectional survey study was approved by the Institutional Review Board at The Ohio State University. In order to ensure the broadest possible representation with respect to socioeconomic and other characteristics, organizations comprising a sizeable proportion of African Americans were identified and consulted in two large Midwestern cities. Among these were a large organization of African American clergy, several large social and fraternal organizations, and several places of employment.
A total of 12 entities were contacted and a letter was sent to the leaders of these organizations. The letter explained the purpose of the study and asked the leader to designate a contact person. Of the 12 organizations, 10 designated a contact person for the study, including 4 churches, 3 social/fraternal groups, and 3 work sites. Repeated attempts to reach the contact person at one church were unsuccessful, leaving 9 groups (3 of each type) participating in the study. The contact person at each site aided in coordinating the date, time, and space (e.g., church sanctuary, meeting rooms, etc.) for the assessment and assisted in the recruitment process. Announcements about the study appeared in church bulletins and in organization newsletters.
On the day of the study at each location, trained research assistants briefly explained the purpose of the study to participants and reviewed instructions for completing the self-administered questionnaire. Participants completed the questionnaire in a group setting and were provided with $15 in appreciation of their time. When the questionnaire had been completed each participant was provided with information about CRC screening and prevention.
The study was limited to those aged 45 and older. Individuals with a personal history of cancer at any site, chronic colorectal disease (e.g., Crohn’s disease or ulcerative colitis), or currently being treated for a life-threatening disease or severe mental disorder (e.g., schizophrenia, dementia, Alzheimer’s disease), and pregnant women were excluded. A total of 203 African American adults were accrued to the study. Four individuals were excluded from the study due to a personal history of chronic colorectal disease, and one individual was excluded because of the age requirements of the study.
The participants (N = 198) were mostly female (65%) with a mean age of 59.7 years (SD = 9.9 years). The majority of participants (83%) had completed at least some post-secondary education, and 25% had a household income of less than $30,000. Specifically related to colorectal disease, 11% of the participants reported a personal history of colorectal polyps. Twenty percent of the participants had a family member (i.e., grandparents, parents, siblings) diagnosed with CRC, 12% had family members diagnosed with colorectal polyps, and 8% had family members diagnosed with irritable bowel disease or other colorectal disease (e.g., ulcerative colitis or Crohn’s disease). With respect to American Cancer Society recommendations for screening, 64% of those 50+ reported having had a colonoscopy in the past 10 years, 16% had sigmoidoscopy in the past 5 years, 11% had a fecal occult blood test within the past year, and 26% had a barium enema in the past 5 years.
Measures
Group susceptibility
Three items from the Colorectal Cancer Screening Questionnaire (CCSQ; Vernon et al. 1997) assess perceptions of the probability of developing colorectal polyps and cancer. These items were modified for this study to assess group-level perceptions (e.g., “I believe African Americans are very likely to develop colorectal cancer or polyps”). Items are rated on a 4-point Likert scale from 1= strongly agree to 4 = strongly disagree, and coefficient alpha was .94.
Traditional Acculturation
The Traditional subscale of the Measurement of Acculturation Strategies for People of African Descent (MASPAD; Obasi 2004) assesses adoption of traditional modes of cultural expression. Twenty-two items are rated on a 6-point Likert scale from 1= strongly disagree to 6 = strongly agree, and coefficient alpha was .86. A sample item is, “It is vital for me to be actively involved in the Black community.”
Physician ethnicity
Study participants who indicated that they had a regular health care provider subsequently were asked to identify the race/ethnicity of that individual. For the purposes of this study, responses were coded as African American or not African American.
Medical mistrust
The Group-Based Medical Mistrust Scale (GBMMS; Thompson et al. 2004) measures suspicion of mainstream health care systems, treatment, and professionals. Twelve items are rated on a 5-point Likert scale from 1 = strongly disagree to 5 = strongly agree. Scores range from 12 to 60. A sample item is: “Doctors and health care workers treat people of my ethnic group like ‘guinea pigs.’” Coefficient alpha was .88 for the total scale.
Perceived benefits, perceived barriers, and intentions
The Colorectal Cancer Screening Questionnaire (CCSQ; Vernon et al. 1997) consists of a set of scales to measure factors related to general colorectal cancer screening adherence based on the Health Belief Model and Social Cognitive Theory. The present study uses scales assessing barriers (worries), benefits (salience and coherence), intention to be screened. Responses are rated on a 4-point Likert scale from 1 = strongly agree to 4 = strongly disagree. Coefficient alpha for perceived the benefits scale was .88. The perceived barriers and intention scales are both two-item scales, and therefore estimating coefficient alpha is not possible.
Sociodemographics and health background
Participants were asked to provide information on the following sociodemographic indicators: age, gender, education, marital/partner status, individual and household income, occupation, and employment status. They also provided information regarding health insurance coverage, personal and family colorectal disease history, and CRC screening history.
Data Analysis
Exploratory hierarchical multiple regression analyses were performed to test for potential interactions between socio-cultural variables in their associations with colorectal cancer screening perceived benefits, perceived barriers, and intention. The following interactions were tested: a) Traditional Acculturative Strategy × Medical Mistrust; b) Physician’s Ethnicity × Medical Mistrust; c) Group Susceptibility × Medical Mistrust; and d) Group Susceptibility × Traditional Acculturative Strategy. Each interaction was the final step in regression analyses with perceived benefits of screening, perceived barriers to screening, and general intention to be screened as the dependent variables. A total of 12 regression analyses were performed. Sociodemographic and access to health care variables significantly correlated with the dependent variables (p < .05) were entered as controls. Table 1 summarizes the regression analyses in which the interaction term was significant.
Table 1.
Hierarchical Multiple Regressions of Interactions Associated with Perceived Benefits and Intention
| Step and Predictor | Statistics by Step | Statistics by Predictor | ||
|---|---|---|---|---|
| TR2 | R2 Change | β | t | |
| Outcome: General Benefits (N = 169) | ||||
| 1. Education | .09 | .09** | .11 | 1.16 |
| Household income | .19 | 2.26* | ||
| Occupation | .02 | .17 | ||
| 2. Regular physician | .12 | .03 | .04 | .60 |
| Physician recommendation | .15 | 1.93 | ||
| 3. Group susceptibility | .15 | .03* | .09 | 1.20 |
| 4. Traditional acculturative strategy | .19 | .04** | .23 | 3.14** |
| 5. Group Susceptibility × Traditional | .22 | .03* | .19 | 2.56* |
| Outcome: General Benefits (N = 165) | ||||
| 1. Education | .11 | .11** | .11 | 1.26 |
| Household income | .20 | 2.53* | ||
| Occupation | −.01 | −.14 | ||
| 2. Regular physician | .13 | .02 | .03 | .47 |
| Physician recommendation | .06 | .88 | ||
| 3. Group susceptibility | .18 | .05** | .29 | 4.28** |
| 4. Medical mistrust | .23 | .05** | −.28 | −3.92** |
| 5. Group Susceptibility × Medical Mistrust | .27 | .04** | .20 | 3.04** |
| Outcome: General Intention (N = 176) | ||||
| 1. Age | .02 | .02 | .11 | 1.43 |
| 2. Education | .08 | .07** | .16 | 1.60 |
| Household income | .17 | 1.82 | ||
| Occupation | −.03 | −.33 | ||
| 3. Insurance | .10 | .01 | .03 | .33 |
| Regular physician | −.03 | −.39 | ||
| Physician recommendation | .09 | 1.20 | ||
| 4. Physician ethnicity | .11 | .01 | .10 | 1.31 |
| 5. Medial mistrust | .11 | .00 | −.02 | −.23 |
| 6. Physician ethnicity × Medical Mistrust | .13 | .03* | .17 | 2.32* |
| Outcome: General Intention (N = 165) | ||||
| 1. Age | .06 | .06** | .12 | 1.53 |
| 2. Education | .11 | .05* | .12 | 1.34 |
| Household income | .11 | 1.32 | ||
| Occupation | −.02 | −.23 | ||
| 3. Insurance | .14 | .03 | .12 | 1.60 |
| Regular physician | .07 | .95 | ||
| Physician recommendation | .13 | 1.74 | ||
| 4. Group susceptibility | .14 | .00 | −.06 | −.78 |
| 5. Traditional acculturative strategy | .21 | .07** | .34 | 4.72** |
| 6. Group Susceptibility × Traditional | .30 | .09** | ..33 | 4.49** |
Note:
p < .05
p < .01; reduced N’s due to missing data.
Results
General benefits
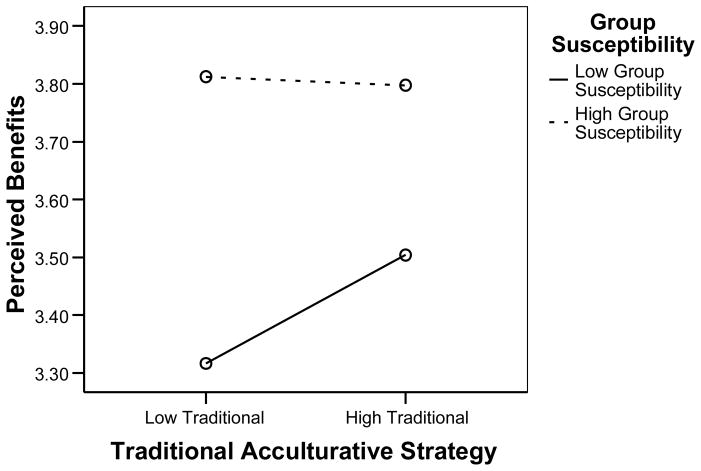
For all perceived benefits models, variables were entered in the following order: step 1) education, household income, and occupation; step 2) regular physician and physician recommendation; step 3) predictor A; step 4) predictor B; step 5) A × B interaction. The model testing the Group Susceptibility × Traditional Acculturative Strategy interaction was significant F(8, 168) = 5.66, p < .001, and accounted for 22% of the variance (total adjusted R2 = .18) in perceived benefits of screening. The interaction step was significant (p < .05), accounting for 3% of the variance (Cohen’s f2 = .04). Figure 1 presents the interaction graphically and reveals that those who perceive high group susceptibility also perceive greater benefits in screening. However, for those who perceive low group susceptibility, individuals who are also more traditional perceive greater benefits than individuals who are less traditional. In other words, individuals who perceive less group susceptibility and are also less traditional perceive the least benefit of screening.
Figure 1.
Estimated perceived benefits (CCSQ) scores as a function of group susceptibility and traditional acculturative strategy.
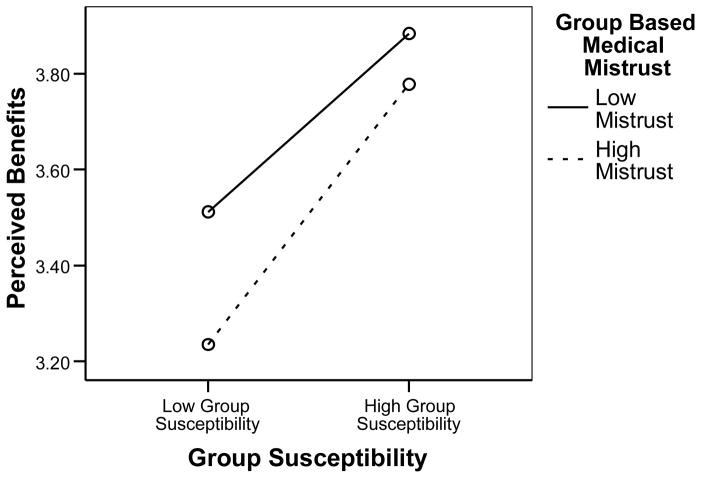
The benefits model testing the Group Susceptibility × Medical Mistrust interaction was also significant F(8, 182) = 8.00, p < .001, and accounted for 27% of variance in perceived benefits. The interaction step was significant (p < .01), accounting for 4% of the variance (Cohen’s f2 = .05). Figure 2 presents this interaction graphically. It shows that those with low levels of mistrust are more likely to perceive benefits than those with high levels of mistrust, but that perception of high group susceptibility makes both groups more likely to perceive benefits. Individuals high in mistrust and low in their perception of group susceptibility perceive the least benefit of screening.
Figure 2.
Estimated perceived benefits (CCSQ) scores as a function of group susceptibility and medical mistrust.
General barriers
The order for general barriers was: step 1) education and occupation; step 2) regular physician and physician recommendation; step 3) predictor A; step 4) predictor B; step 5) A × B interaction. None of the perceived barriers models testing interactions were significant (all ps > .05; data not presented).
General intention
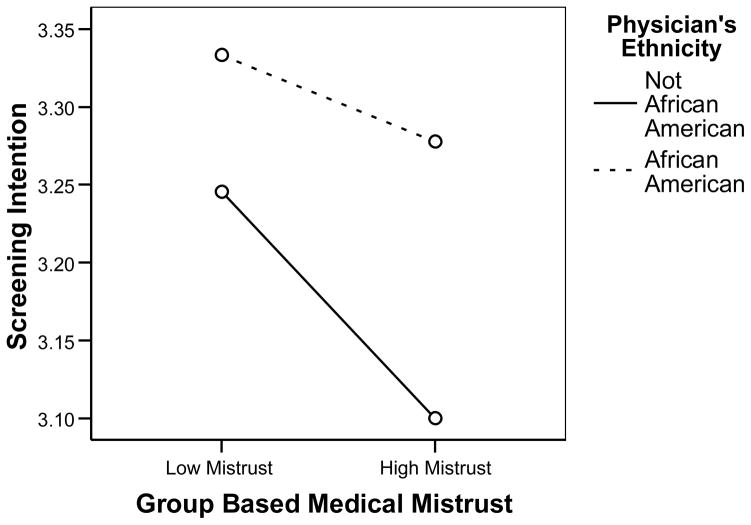
Variables were entered in the following order for all screening intention models: step 1) age; step 2) education, occupation, and household income; step 3) health insurance, regular physician, and physician recommendation; step 4) predictor A; step 5) predictor B; step 6) A × B interaction. The intention model testing the Physician Ethnicity × Medical Mistrust interaction was significant F(10, 175) = 2.55, p < .01, and accounted for 13% of the variance (total adjusted R2 = .08) in screening intention. The interaction step was significant (p < .05), accounting for 3% of the variance (Cohen’s f2 = .03). Figure 3 presents the interaction, showing that overall individuals with an African American physician express greater intent to be screened relative to individuals with physicians who are not African American. Though it shows some decline, this intent remains fairly stable even in the face of high levels of medical mistrust. However, for individuals with non-African American physicians, high levels of mistrust are associated with less intent to be screened. In fact, these individuals expressed the least intent to be screened.
Figure 3.
Estimated screening intention (CCSQ) scores as a function of physician ethnicity and medical mistrust.
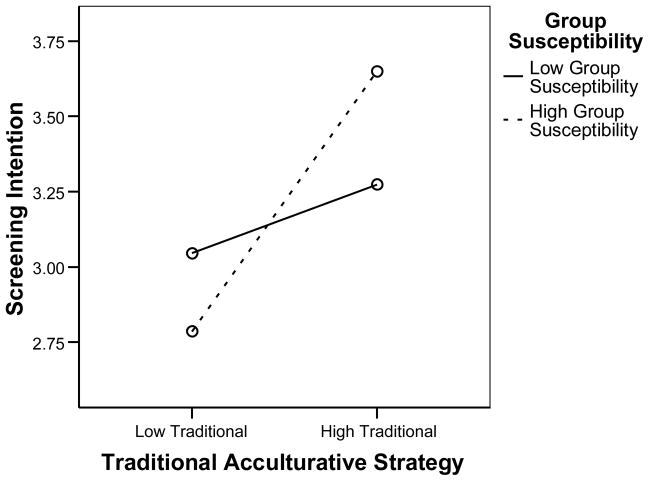
Finally, the intention model testing the Group Susceptibility × Traditional Acculturative Strategy interaction was significant F(10, 164) = 6.69, p < .001, and accounted for 30% of the variance (total adjusted R2 = .26) in screening intention. The interaction step was significant (p < .001), accounting for 9% of the variance (Cohen’s f2 = .13). Figure 4 presents this interaction. While individuals who perceived low levels of group susceptibility expressed slightly more intent to be screened at high levels of traditionalism, individuals who perceived high levels of group susceptibility expressed considerably more intent at high levels of traditionalism.
Figure 4.
Estimated screening intention (CCSQ) scores as a function of group susceptibility and traditional acculturative strategy.
Discussion
In light of the higher CRC mortality rates among African Americans, early detection by screening within recommended guidelines is vital for this vulnerable population. In this study, we found greater perception of CRC screening benefits among individuals who perceived high group susceptibility to CRC, regardless of the level of traditional cultural orientation or medical mistrust. Among individuals who perceived low group susceptibility to CRC, however, perceptions of the benefits of CRC screening were increased if they had a high versus a low traditional cultural orientation. Perception of benefits also increased if low perceivers of group susceptibility had low medical mistrust compared to those with high medical mistrust. Increased expressed intention to complete CRC screening was associated with perceiving high group CRC susceptibility while being more culturally traditional, and increased CRC screening intention was also associated with having an African American physician and low medical mistrust. These findings suggest that perceived benefit and intent to complete CRC screening is best among African Americans with high group susceptibility, high traditional cultural orientation, less mistrust of the medical system, and who report that their primary healthcare provider is an African American physician.
The results of this study suggest that African Americans who identify with a traditional cultural orientation only have lower perceived benefits to CRC screening if they have low perceived group susceptibility. Individuals with a more traditional cultural orientation have increased perceived benefit to CRC screening if they perceive high group susceptibility for CRC. Since many of the MASPAD items address fidelity to one’s racial/ethnic identity as a person of African descent and adherence to cultural norms, it is possible that the traditional acculturative strategy was a proxy for a positive racial identity in this study. This may explain why results from this study differ from studies that report a negative association between traditional cultural orientation (e.g., low acculturation) and colorectal cancer screening in other ethnic groups (Maxwell et al. 2000, Tang et al. 2001, Honda 2004, Honda et al. 2005, Shah et al. 2006,). There is some evidence that the protective nature of positive racial identity leads to less risky health behaviors (Caldwell et al. 2002, Beadnell et al. 2003, Caldwell et al. 2004). This implies that behavioral interventions seeking to increase screening among this population might successfully incorporate traditional African American values (e.g., group solidarity, striving despite obstacles, and reliance on others within the group) and risk messages focused at the level of the African American community rather than exclusively at the individual level. Interventions that use existing social networks (e.g., churches, social and fraternal organizations, extended families) as motivational and venues for message delivery may prove especially effective at increasing CRC screening rates.
In contrast to individuals with high traditional cultural orientation and perceived high group susceptibility, study participants who perceived low group susceptibility and who were also highly mistrustful of healthcare professionals and the healthcare system perceived fewer benefits of CRC screening. The relationship of mistrust with less perception of benefits is consistent with previous research in which African Americans are more likely to express mistrust of the medical system and concerns about quality of care when contemplating CRC screening (Holmes-Rovner et al. 2002, Greiner et al. 2005). However, the concept of group susceptibility has not received as much attention in the literature. It is possible that one way to overcome CRC screening barriers associated with medical mistrust is to focus cancer prevention and control communications at both the individual and group levels. There is evidence from previous research that African Americans are interested in receiving information regarding their racial group, as long as group-level risk information is closely paired with concrete behavioral recommendations for cancer screening (Sanders Thompson et al. 2007).
Having an African American physician appeared to have buffered the impact of mistrust on intention to be screened. While several studies have noted the impact of racial concordance on health care utilization and perceptions of quality of care (LaVeist and Nuru-Jeter 2002, Cooper et al. 2003, LaVeist et al. 2003), more information is needed about the effect of having a same-race physician on CRC screening completion. African American physicians and other health providers may be particularly important as spokespersons to communicate CRC risk and prevention messages to African Americans.
While we believe that this study offers important new information that could improve behavioral interventions aimed at increasing CRC among African Americans, there are several limitations that must be noted. First, this study was exploratory in nature and therefore did not proceed from a priori hypotheses regarding the relationships under study. The participants in this study were a convenience sample of African Americans from two large Midwestern cities, who may differ from African Americans in other communities. The participants included in this study also had a relatively high socioeconomic status, and rates of physician recommendation for CRC screening and CRC screening completion were above the rates reported nationally. Also while gender was not a significant correlate of the outcomes addressed in this study, a majority of study participants was female and more information may be necessary before drawing conclusions regarding African American men.
In conclusion, the results of this study suggest that among African Americans, traditional cultural orientation, group susceptibility of CRC, medical mistrust, and physician ethnicity play a significant role in perceived benefits to CRC screening and intention to complete CRC screening. These factors should be considered when developing new behavioral interventions to increase CRC screening among African Americans. The development of new prevention and control strategies will potentially reduce the disparities associated with CRC and race.
Contributor Information
Jason Q. Purnell, University of Rochester School of Medicine & Dentistry
Mira L. Katz, Ohio State University
Barbara L. Andersen, Ohio State University
Nancy Bennett, University of Rochester School of Medicine & Dentistry.
References
- Abraido-Lanza AF, Chao MT, Gates CY. Acculturation and cancer screening among Latinas: Results from the National Health Interview Survey. Annals of Behavioral Medicine. 2005;29 (1):22–28. doi: 10.1207/s15324796abm2901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal S, et al. Colorectal cancer in African Americans. American Journal of Gastroenterology. 2005;100 (3):515–523. doi: 10.1111/j.1572-0241.2005.41829.x. [DOI] [PubMed] [Google Scholar]
- American Cancer Society. Colorectal Cancer Facts & Figures - Special Edition 2005. Atlanta, GA: American Cancer Society; 2005. [Google Scholar]
- American Cancer Society. Cancer Prevention & Early Detection Facts & Figures 2007. Atlanta, GA: American Cancer Society; 2007a. [Google Scholar]
- American Cancer Society. Cancer Facts & Figures for African Americans 2007–2008. Atlanta, GA: American Cancer Society; 2007b. [Google Scholar]
- Ard JD, et al. Informing cancer prevention strategies for African Americans: The relationship of African American acculturation to fruit, vegetable, and fat intake. Journal of Behavioral Medicine. 2005;28 (3):239–247. doi: 10.1007/s10865-005-4660-3. [DOI] [PubMed] [Google Scholar]
- Ashing-Giwa K. Health behavior change models and their socio-cultural relevance for breast cancer screening in African American women. Women & Health. 1999;28 (4):53–71. doi: 10.1300/J013v28n04_04. [DOI] [PubMed] [Google Scholar]
- Beadnell B, et al. Ethnic identity and sexual risk-taking among African-American women enrolled in an HIV/STD prevention intervention. Psychology, Health & Medicine. 2003;8 (2):187–198. [Google Scholar]
- Becker MH. The Health Belief Model and personal health behavior. Health Education Monographs. 1974:2. [Google Scholar]
- Bradley CJ, Given CW, Roberts C. Disparities in cancer diagnosis and survival. Cancer. 2001;91 (1):178–188. doi: 10.1002/1097-0142(20010101)91:1<178::aid-cncr23>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- Caldwell CH, et al. Racial identity, maternal support, and psychological distress among African American adolescents. Child Development. 2002;73 (4):1322–1336. doi: 10.1111/1467-8624.00474. [DOI] [PubMed] [Google Scholar]
- Caldwell CH, et al. Racial identity, parental support, and alcohol use in a sample of academically at-risk African American high school students. American Journal of Community Psychology. 2004;34 (4):71–82. doi: 10.1023/b:ajcp.0000040147.69287.f7. [DOI] [PubMed] [Google Scholar]
- Cooper LA, et al. Patient-centered communication, ratings of care, and concordance of patient and physician race. Annals of Internal Medicine. 2003;139 (11):907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- Ghafoor A, et al. Cancer statistics for African Americans. CA: A Cancer Journal for Clinicians. 2002;52 (6):326–341. doi: 10.3322/canjclin.52.6.326. [DOI] [PubMed] [Google Scholar]
- Greiner KA, et al. Knowledge and perceptions of colorectal cancer screening among urban African Americans. Journal of General Internal Medicine. 2005;20 (11):977–983. doi: 10.1111/j.1525-1497.2005.00165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes-Rovner M, et al. Colorectal cancer screening barriers in persons with low income. Cancer Practice. 2002;10 (5):240–247. doi: 10.1046/j.1523-5394.2002.105003.x. [DOI] [PubMed] [Google Scholar]
- Honda K. Factors associated with colorectal cancer screening among the US urban Japanese population. American Journal of Public Health. 2004;94 (5):815–822. doi: 10.2105/ajph.94.5.815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honda K, Gorin SS. Modeling pathways to affective barriers on colorectal cancer screening among Japanese Americans. Journal of Behavioral Medicine. 2005;28 (2):115–124. doi: 10.1007/s10865-005-3661-6. [DOI] [PubMed] [Google Scholar]
- Janz NK, Becker MH. The Health Belief Model: A decade later. Health Education Quarterly. 1984;11 (1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Katz ML, et al. Colorectal cancer screening among African American church members: A qualitative and quantitative study of patient-provider communication. BMC Public Health. 2004;4:62. doi: 10.1186/1471-2458-4-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landrine H, Klonoff EA. African American acculturation: Deconstructing race and reviving culture. Thousand Oaks, CA: Sage; 1996. [Google Scholar]
- LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Medical Care Research and Review. 2000;57 (Suppl 1):146–161. doi: 10.1177/1077558700057001S07. [DOI] [PubMed] [Google Scholar]
- LaVeist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? Journal of Health and Social Behavior. 2002;43 (3):296–306. [PubMed] [Google Scholar]
- LaVeist TA, Nuru-Jeter A, Jones KE. The association of doctor-patient race concordance with health services utilization. Journal of Public Health Policy. 2003;24 (3–4):312–323. [PubMed] [Google Scholar]
- Maxwell AE, Bastani R, Warda US. Demographic predictors of cancer screening among Filipino and Korean immigrants in the United States. American Journal of Preventive Medicine. 2000;18 (1):62–68. doi: 10.1016/s0749-3797(99)00110-5. [DOI] [PubMed] [Google Scholar]
- Myers LJ. Understanding an Afrocentric world view: Introduction to an optimal psychology. Dubuque, IA: Kendall/Hunt; 1993. [Google Scholar]
- Myers RE, et al. Modeling adherence to colorectal cancer screening. Preventive Medicine. 1994;23 (2):142–151. doi: 10.1006/pmed.1994.1020. [DOI] [PubMed] [Google Scholar]
- O’Malley AS, et al. The role of trust in use of preventive services among low-income African-American women. Preventive Medicine. 2004;38 (6):777–785. doi: 10.1016/j.ypmed.2004.01.018. [DOI] [PubMed] [Google Scholar]
- Obasi EM. Dissertation (PhD) The Ohio State University; 2004. Measurement of acculturation strategies for people of African descent (MASPAD): An emic conceptualization of acculturation as a moderating factor between psychological and mental health seeking attitudes. [Google Scholar]
- Parham TA, White JL, Ajamu A. The psychology of Blacks: An African-centered perspective. Upper Saddle River, NJ: Prentice Hall; 1999. [Google Scholar]
- Purnell JQ, Andersen BL. Testing a sociocultural model of colorectal cancer screening among African Americans. Annals of Behavioral Medicine. 2007;33:S084. [Google Scholar]
- Risendal B, et al. Influence of health care, cost, and culture on breast cancer screening: Issues facing urban American Indian women. Preventive Medicine. 1999;29 (6):501–509. doi: 10.1006/pmed.1999.0564. [DOI] [PubMed] [Google Scholar]
- Safran DG, et al. Linking primary care performance to outcomes of care. The Journal of Family Practice. 1998;47 (3):213–220. [PubMed] [Google Scholar]
- Saha S, et al. Patient-physician racial concordance and the perceived quality and use of health care. Archives of Internal Medicine. 1999;159 (9):997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- Sanders Thompson VL, et al. Evidential preferences: Cultural appropriateness strategies in health communications. Health Education Research. 2007 doi: 10.1093/her/cym029. Advance Access published on July 13, 2007. [DOI] [PubMed] [Google Scholar]
- Shah M, Zhu KM, Potter J. Hispanic acculturation and utilization of colorectal cancer screening in the United States. Cancer Detection and Prevention. 2006;30 (3):306–312. doi: 10.1016/j.cdp.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Snowden LR, Hines AM. Acculturation, alcohol consumption, and AIDS-related risky sexual behavior among African American men. Journal of Community Psychology. 1998;26 (4):345–359. doi: 10.1300/J013v27n03_02. [DOI] [PubMed] [Google Scholar]
- Snowden LR, Hines AM. A scale to access African American acculturation. Journal of Black Psychology. 1999;25 (1):36–47. [Google Scholar]
- Tang TS, Solomon LJ, McCracken LM. Barriers to fecal occult blood testing and sigmoidoscopy among older Chinese-American women. Cancer Practice. 2001;9 (6):277–282. doi: 10.1046/j.1523-5394.2001.96008.x. [DOI] [PubMed] [Google Scholar]
- Tang TS, et al. The role of cultural variables in breast self-examination and cervical cancer screening behavior in young Asian women living in the United States. Journal of Behavioral Medicine. 1999;22 (5):419–436. doi: 10.1023/a:1018653306776. [DOI] [PubMed] [Google Scholar]
- Terrell F, Terrell SL. An inventory to measure cultural mistrust among Blacks. Western Journal of Black Studies. 1981;5 (3):180–184. [Google Scholar]
- Thom DH, et al. Further validation and reliability testing of the Trust in Physician Scale. The Stanford Trust Study Physicians. Medical Care. 1999;37 (5):510–517. doi: 10.1097/00005650-199905000-00010. [DOI] [PubMed] [Google Scholar]
- Thompson HS, et al. The Group-Based Medical Mistrust Scale: psychometric properties and association with breast cancer screening. Preventive Medicine. 2004;38 (2):209–218. doi: 10.1016/j.ypmed.2003.09.041. [DOI] [PubMed] [Google Scholar]
- Vernon SW, Myers RE, Tilley BC. Development and validation of an instrument to measure factors related to colorectal cancer screening adherence. Cancer Epidemiology, Biomarkers & Prevention. 1997;6 (10):825–832. [PubMed] [Google Scholar]