Abstract
The current article discusses how momentary assessment may fundamentally contribute to identifying environmental risk factors and symptom patterns, as well as provide new opportunities for treatment. A new prototype device, the “PsyMate,” was specifically developed to implement momentary assessment in clinical practice. It was shown that self-monitoring of both positive and negative psychotic symptoms (a) is feasible, (b) provides a much more detailed and fine-grained picture of symptoms, and (c) reveals patterns of behavior that may be relevant for treatment. Furthermore, the PsyMate could be instrumental for real-time and real-world delivery of psychological interventions. With PsyMate, patients can become active partners in the therapeutic process, resulting in greater patient ownership and empowerment as well as understanding of their symptoms and the environment.
Keywords: psychosis, momentary assessment, environment, psychological intervention, CBT
Introduction
Psychotic symptoms are natural experiences emerging in the realm of normal daily life, often in interaction with contextual features. These contextual features, however, have mainly been identified through epidemiological research, resulting in general, global risk factors for psychosis,1–3 limiting the applicability for individualized intervention strategies. Momentary assessment approaches, on the other hand, using structured diary techniques, such as the Experience Sampling Method (ESM)4,5 or Ecological Momentary Assessment,6 have shown that both internal and external contextual features may influence the frequency and intensity of symptoms as they unfold in daily life.5 The current article will discuss how momentary assessment may fundamentally contribute to identifying these personal risk factors and symptom patterns as well as provide new opportunities for treatment.
The PsyMate: A Clinical Momentary Assessment Tool
Numerous methods and technologies have been employed to collect momentary assessment data in daily life including paper and pencil, notebooks, PDAs, mobile telephones, and online reporting.7 However, all of these methods suffer from limitations. Therefore, a new prototype device, the “PsyMate”, was specifically developed to implement momentary assessment in clinical practice (see figure 1). The PsyMate is designed to monitor experiences and behavior in daily life by signaling patients and recording and time-stamping their responses. It is small, lightweight, has a user-friendly interface and allows for easy and flexible programming, with the possibility to respond to the input of the subject. It is easily accessible for participants with limited familiarity with technological devices, thus overcoming some of the problems that have been reported with PDAs and mobile phones.7 The PsyMate is currently being used in 2 trials on depression.8 In the current article, we will focus on its applicability in psychosis.
Fig. 1.
The PsyMate Device: When Signaled, Patients Respond to Questions Regarding Thoughts, Mood, Symptoms as well as the Context, and Appraisals Thereof.
Can Patients With Psychosis Become Active Partners in Their Symptom Assessment?
Essential characteristics of psychotic phenomena include frequency of occurrence, variability over time, and the interplay with the context in which they are occurring. Despite the clinical relevance of these characteristics, very little of this information is available to the clinician or to the patient, for that matter. People are generally poor in providing accurate, global, retrospective reflections of real-life experiences, and behavior, and this appears to be especially problematic for patients with psychosis who experience a loss of reality testing and suffer from cognitive impairment. Furthermore, people are not always consciously aware of the patterns of behavior and the subtle interplay between experiences and environmental features.
Similar to advantages in somatic medicine of real-time monitoring of blood pressure9 or plasma glucose levels,10 real-time monitoring of psychiatric symptoms may considerably improve the understanding of the nature and expression of symptoms as well as actively engage patients in this assessment and monitoring process. Clinical studies are already underway for psychiatric disorders such as anxiety, eating disorders, or depression7,8,11; however, researchers and clinicians alike have yet to explore these opportunities in psychosis.
Positive Symptoms of Psychosis
The positive symptoms of psychosis, such as disturbances in the content of thought and in sensory perception, tend to be difficult for patients to accurately self-monitor. Patients are often unaware of the deviant nature of these experiences; however, items, such as “preoccupation with thoughts,” “feeling paranoid,” “feeling controlled,” or “feeling unreal,” capture aspects of mental state that are associated with delusions and that patients can accurately report. Similarly, patients can provide veridical self-report about the intensity of hallucinations, even when they are not aware of the origin of these experiences.
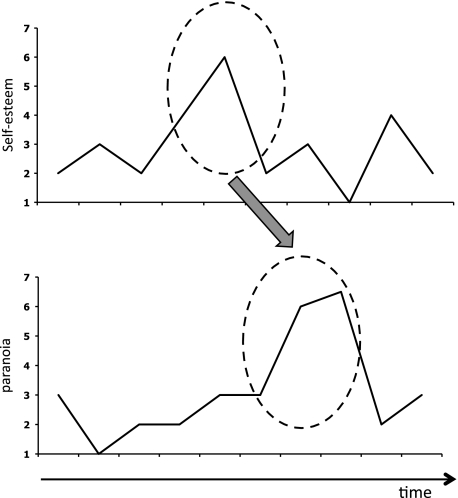
Studies using ESM have demonstrated that there is considerable variation in the intensity of both delusions12,13 and hallucinations14 over periods of minutes and hours. Furthermore, this variability in symptom intensity is driven both by internal and external factors. Increases in paranoia, eg, were precipitated by a decrease in self-esteem13 (see figure 2), an increase in anxiety,13,15 and increased feelings of subjective stress.16 External factors have also been implicated in the onset of positive symptoms including day-to-day urban exposure,17 social context,18 and cannabis use.19 Cannabis use, eg, immediately increased positive affect, whereas the increase in hallucinations occurred thereafter. This temporal dissociation between the acute rewarding effects and the subsequent toxic influences may explain the vicious circle of deleterious use in these patients.
Fig. 2.
The PsyMate May Be Used to Capture Temporal Associations Between Real-Time Variability in Internal States (eg, Self-esteem) and in Symptoms (eg, Paranoia).
Negative Symptoms of Psychosis
Negative symptoms of psychosis reflect deficits in cognitive functioning, experience of pleasure, and interest, motivation, and engagement in the world.20,21 These symptoms seem even less accessible to real-life self-monitoring because current assessment instruments rely solely on observer-rated behavior.20 However, the experiential and behavioral manifestations of negative symptoms can be self-monitored by patients in real life. It was shown, eg, that patients with a psychotic disorder show increased intensity and variability of negative emotions but a reduced intensity of positive emotions.22 This may reflect anhedonia, diminished capacity to experience pleasure, or rather result from living a less pleasant life. In a second study, it was shown that patients with a psychotic disorder were equally if not more able to experience pleasure when something pleasant was happening, only fewer pleasant events were reported (Oorschot M, Lataster T, Thewissen V, et al., unpublished data). It was also shown that patients reported similar levels of pleasure during activities as control participants but reported less anticipatory pleasure from future goal-directed activities.23
These results represent group comparisons rather than assessing individual risk profiles of patients. Yet, these data show that self-monitoring of both positive and negative psychotic symptoms (a) is feasible, (b) provides a much more detailed and fine-grained picture of symptoms, and (c) reveals patterns of behavior that may be relevant for treatment. Thus, patients with psychosis, even during acute phases of the illness, can become active partners in the assessment of their symptoms. Furthermore, the fine-grained assessment of symptoms and behavior may accelerate and fundamentally broaden the assessment of treatment efficacy, both at the individual level as well as in clinical trials.
From Assessment to Treatment in Real Life
In addition to real-time assessment of symptoms, the PsyMate could be instrumental for real-time and real-world delivery of psychological interventions. This procedure, referred to as Ecological Momentary Intervention,7 can extend therapeutic interventions for patients with psychosis beyond the clinical setting. The integration of assessment and treatment in the PsyMate allows for an individual-tailored intervention with the possibility of delivering feedback that is directly related to symptom intensity or environmental risks. Ecological Momentary Intervention for psychiatric problems has primarily been used to supplement other psychological treatments such as Cognitive Behavioral Therapy.7 However, it could also be used as a treatment in and of itself. So far, almost no real-time applications have been developed for treatment of psychosis. We will outline some of the possibilities below.
Paranoia
As previously outlined, there is an evidence that the experience and expression of paranoia are strongly driven by increased anxiety and decreased self-esteem and is exacerbated/triggered by environmental cues. At a metacognitive level, the PsyMate could be used to increase awareness of this pattern, eg, through giving patients feedback on these processes at the end of the assessment period. Similarly, feedback in real time may aid in inducing behavioral changes; for example, when patients become more anxious, real-time feedback could be provided helping patients to actively reduce the anxiety, thus reducing the risk that paranoia intensity would increase. The PsyMate may also be instrumental in conducting individualized behavioral experiments in the context of cognitive behavioral therapy (CBT). Paranoia, eg, often leads to safety behaviors to mitigate the perceived threat (eg, avoiding potentially “dangerous” situations), thus missing the opportunity to gather disconfirming evidence.24 The PsyMate could be used to (a) set up the exercise and to gather real-time information about the behavioral experiments and (b) provide detailed information on the real-life outcomes of these tests.
Hallucinations
The PsyMate could be used in the treatment of hallucinations as well.25 One recent article describes an ongoing trial in schizophrenia using mobile technology to provide a brief intervention for hallucinations that involves cognitive (eg, “but you mentioned in the past that voices are just sounds and can’t really hurt you”) and behavioral (eg, “try not responding to see what happens … ”) interventions through text exchange 3 times a day.24 With the PsyMate, a more frequent (up to 10 times a day) and more detailed assessment of symptom intensity as well as contextual risk profile could be achieved. More importantly, however, the PsyMate could be used to provide individual-tailored feedback rather than generic interventions, related to the real-time presence of the hallucinations, helping patients to challenge for example, beliefs about voices’ power and intent25 as they occur in real life.
Negative Symptoms
Very few treatments, if any, have proven to be successful for negative symptoms.20 One of the central problems underlying negative symptoms seems to be a divide between the experience of pleasure and motivation.26 Patients with psychosis report an equal capacity to experience pleasure compared with controls. However, experienced pleasantness does not result in increased motivation for this activity, resulting in the paradoxical situation that patients do not often engage in activities that they actually enjoy. Feedback on this process through real-time monitoring of the patterns of behavior may increase insight in and awareness of this divide. PsyMate data may also aid in discovering which activities or situations result in increased feelings of pleasure. Real-life monitoring may also be used to induce behavioral changes. For example, patients could receive real-time support to undertake activities that were previously been identified as pleasant.
In conclusion, the PsyMate offers a device that is not only instrumental in the assessment of psychosis but may also provide treatment interventions in real-world settings as well as monitor the efficacy of these interventions. With PsyMate, patients can become active partners in the therapeutic process, resulting in greater patient ownership and empowerment as well as understanding of their symptoms and the environment. This would be entirely congruent with the proposed “next generation” of CBT for psychosis where it is argued that more focus is required on the interaction of emotions, context, and delusions as well as on the safety behaviors that support threat beliefs about persecutors27: PsyMate is ideal to move therapy out of the office and into the patient’s day-to-day experience.
Funding
National Alliance for Research on Schizophrenia and Depression Young Investigator Award 2006; Dutch Medical Research Council, VIDI grant (grant number 917.76.341 to I.M.-G.).
Acknowledgments
The Authors have declared that there are no conflicts of interest in relation to the subject of this study. PsyMate is developed under the auspices of the Maastricht University technology transfer office; none of the authors will benefit financially.
References
- 1.Henquet C, Murray R, Linszen D, van Os J. The environment and schizophrenia: the role of cannabis use. Schizophr Bull. 2005;31:608–612. doi: 10.1093/schbul/sbi027. [DOI] [PubMed] [Google Scholar]
- 2.Krabbendam L, van Os J. Schizophrenia and urbanicity: a major environmental influence—conditional on genetic risk. Schizophr Bull. 2005;31:795–799. doi: 10.1093/schbul/sbi060. [DOI] [PubMed] [Google Scholar]
- 3.van Os J, Krabbendam L, Myin-Germeys I, Delespaul P. The schizophrenia envirome. Curr Opin Psychiatry. 2005;18(2):141–145. doi: 10.1097/00001504-200503000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Hektner JM, Schmidt JA, Csikszentmihalyi M. Experience Sampling Method: Measuring the Quality of Everyday Life. London, UK: Sage Publications; 2007. [Google Scholar]
- 5.Myin-Germeys I, Oorschot M, Collip D, Lataster J, Delespaul P, van Os J. Experience sampling research in psychopathology: opening the black box of daily life. Psychol Med. 2009;39:1533–1547. doi: 10.1017/S0033291708004947. [DOI] [PubMed] [Google Scholar]
- 6.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu rev clin psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- 7.Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol. 2010;15(Pt 1):1–39. doi: 10.1348/135910709X466063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wichers MC, Simons C, Kramer I, et al. Helping depressed patients help themselves: a momentary assessment device to diagnose and remedy emotional dynamics in daily life. Acta Psychiatrica Scandinavica. In press. [Google Scholar]
- 9.Parati G, Omboni S, Bilo G. Why is out-of-office blood pressure measurement needed? Home blood pressure measurements will increasingly replace ambulatory blood pressure monitoring in the diagnosis and management of hypertension. Hypertension. In press. [Google Scholar]
- 10.Nardacci EA, Bode BW, Hirsch IB. Individualizing care for the many: the evolving role of professional continuous glucose monitoring systems in clinical practice. Diabetes Educ. 2010;36(suppl 1):4S–19S. doi: 10.1177/0145721710362798. quiz 20S–21S. [DOI] [PubMed] [Google Scholar]
- 11.Lenderking WR, Hu M, Tennen H, Cappelleri JC, Petrie CD, Rush AJ. Daily process methodology for measuring earlier antidepressant response. Contemp Clin Trials. 2008;29:867–877. doi: 10.1016/j.cct.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 12.Myin-Germeys I, Nicolson NA, Delespaul PA. The context of delusional experiences in the daily life of patients with schizophrenia. Psychol Med. 2001;31:489–498. doi: 10.1017/s0033291701003646. [DOI] [PubMed] [Google Scholar]
- 13.Thewissen V, Bentall RP, Lecomte T, van Os J, Myin-Germeys I. Fluctuations in self-esteem and paranoia in the context of daily life. J Abnorm Psychol. 2008;117(1):143–153. doi: 10.1037/0021-843X.117.1.143. [DOI] [PubMed] [Google Scholar]
- 14.Delespaul P, deVries M, van Os J. Determinants of occurrence and recovery from hallucinations in daily life. Soc Psychiatry Psychiatr Epidemiol. 2002;37(3):97–104. doi: 10.1007/s001270200000. [DOI] [PubMed] [Google Scholar]
- 15.Thewissen V, Bentall RP, Oorschot M, et al. Emotions, self-esteem, and paranoid episodes: an experience sampling study. Br J Clin Psychol. doi: 10.1348/014466510X508677. In press. [DOI] [PubMed] [Google Scholar]
- 16.Myin-Germeys I, Delespaul P, van Os J. Behavioural sensitization to daily life stress in psychosis. Psychol Med. 2005;35:733–741. doi: 10.1017/s0033291704004179. [DOI] [PubMed] [Google Scholar]
- 17.Ellett L, Freeman D, Garety PA. The psychological effect of an urban environment on individuals with persecutory delusions: the Camberwell walk study. Schizophr Res. 2008;99(1–3):77–84. doi: 10.1016/j.schres.2007.10.027. [DOI] [PubMed] [Google Scholar]
- 18.Collip D, Oorschot M, Thewissen V, Van Os J, Bentall R, Myin-Germeys I. Social world interactions: how company connects to paranoia. Psychol Med. doi: 10.1017/S0033291710001558. In press. [DOI] [PubMed] [Google Scholar]
- 19.Henquet C, van Os J, Kuepper R. Psychosis reactivity to cannabis use in daily life: an experience sampling study. Br J Psychiatry. 2010;196:447–453. doi: 10.1192/bjp.bp.109.072249. [DOI] [PubMed] [Google Scholar]
- 20.Blanchard JJ, Kring AM, Horan WP, Gur R. Toward the next generation of negative symptom assessments: the collaboration to advance negative symptom assessment in schizophrenia. Schizophr Bull. September 22, 2010 doi: 10.1093/schbul/sbq104. doi: 10.1093/schbul/sbq104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Messinger JW, Tremeau F, Antonius D, et al. Avolition and expressive deficits capture negative symptom phenomenology: implications for DSM-5 and schizophrenia research. Clin Psychol Rev. 2011;31:161–168. doi: 10.1016/j.cpr.2010.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myin-Germeys I, Delespaul PA, deVries MW, et al. Schizophrenia patients are more emotionally active than is assumed based on their behavior. Schizophr Bull. 2000;26:847–854. doi: 10.1093/oxfordjournals.schbul.a033499. [DOI] [PubMed] [Google Scholar]
- 23.Gard DE, Kring AM, Gard MG, Horan WP, Green MF. Anhedonia in schizophrenia: distinctions between anticipatory and consummatory pleasure. Schizophr Res. 2007;93:253–260. doi: 10.1016/j.schres.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Depp CA, Mausbach B, Granholm E, et al. Mobile interventions for severe mental illness: design and preliminary data from three approaches. J Nerv Ment Dis. 2010;198:715–721. doi: 10.1097/NMD.0b013e3181f49ea3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Trower P, Birchwood M, Meaden A, Byrne S, Nelson A, Ross K. Cognitive therapy for command hallucinations: randomised controlled trial. Br J Psychiatry. 2004;184:312–320. doi: 10.1192/bjp.184.4.312. [DOI] [PubMed] [Google Scholar]
- 26.Tremeau F, Antonius D, Cacioppo JT. Anticipated, on-line and remembered positive experience in schizophrenia. Schizophr Res. 2010;122:199–205. doi: 10.1016/j.schres.2009.10.019. [DOI] [PubMed] [Google Scholar]
- 27.Birchwood M, Trower P. The future of cognitive-behavioural therapy for psychosis: not a quasi-neuroleptic. Br J Psychiatry. 2006;188:107–108. doi: 10.1192/bjp.bp.105.014985. [DOI] [PubMed] [Google Scholar]