Abstract
Background
Prior administration of a small dose of lipopolysaccharide confers a cardiac protection against ischemia-reperfusion injury. However, the signaling mechanisms that control the protection are incompletely understood. We tested the hypothesis that TLR4 mediates the ability of lipopolysaccharide to protect against cardiac ischemia-reperfusion injury through distinct intracellular pathways involving myeloid differentiation factor 88 (MyD88), TIR-domain-containing adaptor protein inducing interferon-β–mediated transcription-factor (Trif), inducible nitric-oxide synthase (iNOS), and soluble guanylate cyclase (sGC).
Methods
Wild-type mice and the genetically modified mice, i.e., TLR4-deficient (TLR4-def), TLR2 knockout (TLR2−/−), MyD88−/−, Trif−/−, iNOS−/−, and sGCα1−/−, were treated with normal saline or 0.1 mg/kg of lipopolysaccharide, intraperitoneally. Twenty-four hours later, isolated hearts were perfused in a Langendorff apparatus and subsequently subjected to 30 min of global ischemia and reperfusion for up to 60 min. Left ventricular function and myocardial infarction sizes were examined.
Results
Compared to saline-treated mice, lipopolysaccharide-treated mice had markedly improved left ventricular developed pressure and dP/dtmax (P < 0.01) and reduced MI sizes (37.2 ± 3.4% vs. 19.8 ± 4.9%, P < 0.01) after ischemia-reperfusion. The cardiac protective effect of lipopolysaccharide was abolished in the TLR4-def and MyD88−/− mice, but remained intact in TLR2−/− or Trif−/− mice. iNOS−/− mice or wild-type mice treated with the iNOS inhibitor 1400W failed to respond to the TLR4-induced nitric oxide production and were not protected by the lipopolysaccharide preconditioning. While sGC 1−/− mice had robust nitric oxide production in response to lipopolysaccharide, they were not protected by the TLR4-elicited cardiac protection.
Conclusions
TLR4 activation confers a potent cardiac protection against ischemia-reperfusion injury via a MyD88-dependent, but Trif-independent mechanism. iNOS/sGC are essential for the TLR4-induced cardiac protection.
INTRODUCTION
Toll-like receptors (TLRs) represent the first line of host defense against microbial infection and play a pivotal role in both innate and adaptive immunity 1. TLRs recognize invading pathogens through the “molecular pattern-recognition”, transduce the signals via distinct intracellular pathways involving a unique set of adaptor proteins and kinases, and ultimately lead to activation of transcription factors and inflammatory responses 2,3. All TLRs, except TLR3, signal through the common MyD88-dependent pathway. TLR3 signals exclusively, and TLR4 partly via MyD88-independent but Trif-dependent pathway 4,5. Animal studies have indicated that these receptors are in part responsible for cardiac dysfunction in certain pathological conditions characterized in either Gram-negative or Gram-positive bacterial infection, such as endotoxemia 6,7, peptidoglycan-associated lipoprotein 8, staphylococcus aureus 9, and in polymicrobial peritonitis 10.
In addition to their role in mediating cardiac dysfunction in septic conditions, emerging evidence indicate that TLRs may also play an important role in noninfectious tissue injury in various organs including the heart and liver 5,11. In the heart, for example, systemic deficiency of TLR2, TLR4, or MyD88 leads to attenuated myocardial inflammation, smaller infarction size, and better preserved ventricular function after transient ischemic injury 12–17. These loss-of-function studies suggest that the intrinsic TLR signaling may contribute to myocardial inflammation and injury during ischemia-reperfusion (I/R).
Intriguingly, a large body of evidence in several animal models demonstrates that prior administration of sub-lethal dose of lipopolysaccharide confers a “preconditioning-like” effect [Review: Ref. 5], similar to the well-characterized ischemic preconditioning 18 or anesthetic preconditioning 19, protecting the heart against subsequent lethal I/R injury. The cardioprotective effect of lipopolysaccharide usually occurs between 12 – 24 h after administration of lipopolysaccharide and is abolished by cycloheximide, a protein synthesis inhibitor that blocks translation elongation, suggesting a mechanism involving de novo synthesis of cardioprotective proteins 20. Lipopolysaccharide is known to enhance production of inducible nitric-oxide synthase (iNOS) in the heart, a process mediated via TLR4 7,21. We have previously demonstrated, in an in vitro system, that TLR4 activation by lipopolysaccharide leads to a survival benefit in isolated cardiomyocytes through MyD88- and iNOS-dependent mechanisms 21,22. iNOS has also been proposed to be the trigger for the lipopolysaccharide-induced preconditioning 23. However, given the multiple systemic reactions in response to in vivo administration of lipopolysaccharide in these animal studies, it is unclear whether the observed cardiac benefits are the direct results of TLR4 stimulation or due to other events secondary to systemic TLR4 activation. Therefore, the critical role of TLR4 and its downstream signaling events in the cardiac protection in vivo remains unclear.
Here, we tested the hypothesis that TLR4 specifically mediates the lipopolysaccharide-elicited cardiac protection against I/R injury through distinct intracellular pathways involving MyD88, Trif, iNOS, and sGC. Using genetically modified mice and an ex-vivo model of I/R injury, we demonstrate that TLR4-MyD88 signaling confers a potent cardiac protection against I/R injury via iNOS- and sGC-dependent mechanisms.
MATERIALS AND METHODS
Animals
C57BL/6J, C57BL/10ScSn, iNOS−/−/C57BL/6J, and TLR4-def mice (C57BL/10ScCr) were purchased from The Jackson Laboratory (Bar Harbor, ME). C57BL/10ScCr is also referred to as C57BL/10ScNJ (Stock No. 003752) with wild-type (WT) Il12rb2 allele. C57BL/10ScCr mice have a deletion of the Tlr4 gene that results in absence of both mRNA and protein and thus in defective response to lipopolysaccharide stimulation. Tlr4lps-del differs from the Tlr4Lps-d mutation of C3H/HeJ mice, a point mutation of Tlr4 gene that causes an amino acid substitution 24. C57BL/10ScSn mice were used as the appropriate WT controls for the TLR4-def mice. TLR2−/− mice were generated by Takeuchi et al 25. MyD88−/− mice were generated by Kawai and colleagues 26 and had been backcrossed > 10 generations into the C57BL/6J strain. Trif−/− mice were generated by Yamamoto, et al. 27. sGCα1−/− mice were generated on the 129S6 background (sGCα1−/−S6) and were backcrossed at least eight generations into a C57BL/6J background (sGCα1−/−B6) 28. sGCα1−/− mice carry a targeted deletion of the sixth exon of the gene encoding of a mutant, catalytically inactive protein. All mice used in the sGC 1, resulting in the expression study were 8–12 week-old, male (except sGCα1−/−B6 mice), and weighed between 20–30 g. Mice were fed with the same bacteria-free diet (Prolab Isopro RMH 3000) and water, and housed in accordance with guidelines from the American Association for Laboratory Animal Science (Memphis, TN). All animal protocols used in the study were approved by the Subcommittee on Research Animal Care of the Massachusetts General Hospital (Boston, Massachusetts).
Lipopolysaccharide treatment
WT and the genetically modified mice were treated with normal saline or lipopolysaccharide (Escherichia coli 0111:B4, Sigma, St Louis, MO) at the dose of 0.1mg/kg by intraperitoneal injection 24 h prior to the I/R protocol. Lipopolysaccharide was dissolved in normal saline and diluted to a final concentration of 0.02 mg/ml for intraperitoneal injection. Baseline left ventricular (LV) function was examined with echocardiography and catheter-based LV pressure measurement in both normal saline- and lipopolysaccharide-treated mice prior to the ex-vivo I/R protocol. To test the effect of iNOS inhibition, WT C57BL/6J mice were injected with 1400W (20 mg/kg) (Enzo Life Sciences International, Plymouth Meeting, PA), intraperitoneally, 2 hours before lipopolysaccharide treatment. 1400W or N-(3-(Aminomethyl)benzyl)acetamidine is a slow, tight binding, and highly selective inhibitor of iNOS 29. It is at least 5,000- and 1,000-folds selective for iNOS versus endothelial NOS (eNOS) in vitro assay and in isolated rat aortic rings, respectively. Inhibition of neuronal NOS (nNOS) and eNOS by 1400W was weaker and rapidly reversible. In the original in vivo study, 1400W at 5 mg/kg inhibited lipopolysaccharide-induced vascular leakage by 94% 29.
Echocardiographic measurements
Twenty-four hours after lipopolysaccharide administration, mice were lightly anesthetized with ketamine (20 mg/kg). Transthoracic echocardiographic images were obtained and interpreted by an echocardiographer blinded to the experimental design using a 13.0-MHz linear probe (Vivid 7; GE Medical System, Milwaukee, WI) as described previously 10,16. M-mode images were obtained from a parasternal short-axis view at mid-ventricular level with a clear view of papillary muscle. LV end-diastolic internal diameter (LVIDED) and LV end-systolic internal diameter (LVIDES) were measured. Fractional shortening (FS) was defined as [(LVIDED – LVIDES)/LVIDED] × %. Ejection fraction (EF) was calculated by the formula (EDV-ESV)/EDV × %, in which EDV was defined as 7 × LVIDED3/(2.4+ LVIDED) or area-length method in 2-D long axis view, ESV was defined as 7 × LVIDES3/(2.4+ LVIDES) or area-length method in 2-D long axis view. The values of three consecutive cardiac cycles were averaged.
Ex vivo model of myocardial ischemia/reperfusion injury
The aorta was cannulated and the hearts perfused in a Langendorff apparatus as described previously with minor modifications 10,16. Isolated hearts were perfused at a constant pressure of 80 mmHg with modified Krebs-Henseleit buffer containing 118 mM NaCl, 24 mM NaHCO3, 10 mM glucose, 4.7 mM KCl, 1.2 mM KH2PO4, 1.2 mM MgSO4, 2.5 mM CaCl2, and 2 mM pyruvate, pH 7.4, at 37 °C. The perfusate was saturated with continuous gas flow consisting of 95% O2 and 5% CO2. A balloon was made with wrapped saran film connected to a PE-50 polyethylene tube. The neck to tip distance of the balloon was about 6–7 mm. The balloon was inserted into the LV chamber through the mitral valve with an incision in the left atrium, and was connected to a pressure transducer (APT300, Harvard Apparatus, Holliston, MA) for continuous measurement of LV pressure. The balloon was inflated with deionized water (15 – 20 μl) to adjust LV end-diastolic pressure (LVEDP) to 6–10 mmHg. The perfused hearts were then immersed in the perfusate maintained at 37 ± 0.5 °C and paced at 420 beats/min with pacing electrodes placed on the right atrium. After a 30 min of constant pressure perfusion, the hearts were subjected to 30 min of zero-flow ischemia followed by reperfusion for 60 min. Pacing was interrupted during ischemia and resumed 3 min after the start of reperfusion. LV Function data were recorded continuously on a data acquisition system (PowerLab, AD Instruments, Colorado Springs, CO). LV developed pressure (LVDP) was calculated as the difference between peak-systolic pressure and LVEDP. dP/dt max was calculated as the maximum rate of increase of LVDP. The recovery of the LV function during the reperfusion was expressed as the percentage of the baseline LVDP and dP/dt max, which were recorded prior to the ischemic phase.
Determination of MI sizes
Infarct sizes were determined by triphenyltetrazolium chloride (TTC, Sigma) staining as described previously 16,17. The hearts were removed from Langendorff device at the end of reperfusion. Each heart was sliced into four sections. The myocardial sections were incubated in 1% TTC in phosphate buffered saline for 15 min at 37 °C. The infarct area (white) and noninfarct area (red) from each section were measured using an image analysis program. Ratios of infarct area/left ventricle were calculated and expressed as the percentage of LV (MI/LV × 100%).
Measurement of plasma nitrate/nitrite
The plasma nitrate/nitrite was measured according to the manusfacturer’s instructions of the NOx fluorometric assay kit (Cayman Chemical Company, Ann Arbor, MI). Briefly, the plasma was filtered through 30 kDa molecular weight cut-off Amicon ultra centrifugal filters (Millipore, Billerica, MA). Ten μl of appropriately diluted samples were incubated with nitrate reductase and cofactor at room temperature for 2 h to convert nitrate to nitrite. The assay mixture was then incubated with 10 μl of DAN reagent in the dark for 10 min. The reaction was stopped by adding 20 μl of NaOH solution into the mixture. The fluorescence was measured in a SpectraMax M5 (Molecular Devices, Sunnyvale, CA) with an excitation of 360 nm and an emission of 430 nm. Nitrite concentrations in the plasma samples were calculated from a standard curve.
Statistical Analysis
Statistical analysis was performed using Graphpad Prism 5 software (GraphPad, La Jolla, CA). The distributions of the continuous variables were expressed as mean ± SE. For LVDP and dP/dtmax data analysis, statistical significance of the difference between two groups (e.g., normal saline vs. lipopolysaccharide or WT vs. Knockout) at the different time points was measured by two-way ANOVA with Bonferroni post hoc tests and repeated measurements. Of note, these specific comparisons were made based on a priori hypotheses rather than pure statistical considerations. Paired Students’ t-test was used for echocardiographic data analysis, MI size, and nitrate/nitrite measurements. The null hypothesis was rejected for P < 0.05.
RESULTS
Low dose (0.1 mg/kg) of lipopolysaccharide pretreatment improves LV function and reduces MI sizes following I/R injury through a TLR4-dependent mechanism
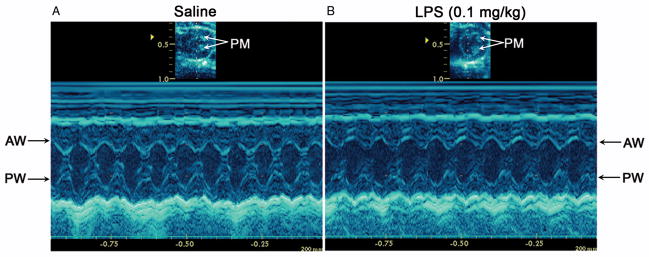
Lipopolysaccharide is known for inducing cardiac dysfunction during endotoxemia. In mice, at the doses of 5 mg/kg and 25 mg/kg, lipopolysaccharide induces significant LV contractile dysfunction through a TLR4-dependent mechanism 7. To test if at a low dose (0.1 mg/kg), lipopolysaccharide induces any LV dysfunction, mice were treated with either normal saline or lipopolysaccharide by intraperitoneal injection. Cardiac function was assessed before and 24 h after the injection by echocardiography (fig. 1 and table 1) and by LV pressure measurement (table 2). As indicated in figure 1 and table 1, 0.1 mg/kg of lipopolysaccharide did not impact the LV function, nor did it change the LV chamber sizes. The saline- and lipopolysaccharide-treated mice had similar EF, FS, and LVID before and 24 h after the treatment. We also calculated the EF with the end diastolic/systolic volumes as measured by area-length method in a 2-D long-axis view and confirmed that there was no difference between the saline and LPS groups (data not shown).
Fig. 1. Representative M-mode echocardiograms of WT mice 24 h after normal saline or lipopolysaccharide injection.
Echocardiography was performed 24 h after normal saline (A) or 0.1 mg/kg of lipopolysaccharide (LPS) (B) was administered to wild-type C57BL/6J mice by intraperitoneal injection. M-mode echocardiographic measurements confirmed normal left ventricular (LV) contractile function and normal LV sizes in both saline- and lipopolysaccharide-treated mice. PM = papillary muscle; AW = anterior wall; PW = posterior wall.
Table 1.
Serial Echocardiographic Measurements before and 24 Hours after Normal Saline or Lipopolysaccharide Administration
| Saline |
LPS (0.1 mg/kg) |
|||
|---|---|---|---|---|
| Baseline | 24 h | Baseline | 24 h | |
| HR, beats/m | 686 ± 12 | 698 ± 16 | 670 ± 20 | 675 ± 16 |
| FS, % | 49.8 ± 1.4 | 52.8 ± 1.9 | 51.7 ± 1.1 | 52.1 ± 1.2 |
| LVEF, % | 82.4 ± 1.3 | 85.1 ± 1.7 | 84.0 ± 1.0 | 84.5 ± 0.9 |
| LVIDED, mm | 3.1 ± 0.1 | 3.0 ± 0.1 | 3.2 ± 0.1 | 3.0 ± 0.0 |
| LVIDES, mm | 1.6 ± 0.1 | 1.4 ± 0.1 | 1.5 ± 0.1 | 1.5 ± 0.0 |
Values are mean ± SE, n = 5/group. FS = fractional shortening; HR = heart rate; LPS = lipopolysaccharide; LVEF = left ventricular ejection fraction; LVIDED = left ventricular end-diastolic internal diameter; LVIDES = left ventricular end-systolic internal diameter.
Table 2.
Baseline LVDP and dP/dtmax before Ischemia-Reperfusion in Isolated Hearts.
| LVDP (mmHg) |
dP/dtmax (mmHg/sec) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Saline | LPS | Saline | LPS | |||||
| Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | |
| WTBL/6 | 86.7 ± 2.2 | 10 | 90.0 ± 2.2 | 11 | 3652.7 ± 131.1 | 10 | 3583.4 ± 143.4 | 11 |
| WTBL/10 | 85.3 ± 2.2 | 9 | 88.2 ± 1.0 | 8 | 3672.9 ± 150.0 | 9 | 3467.6 ± 57.9 | 8 |
| TLR2−/− | 84.5 ± 2.4 | 8 | 90.1 ± 1.4 | 8 | 3438.1 ± 225.5 | 8 | 3520.2 ± 200.7 | 8 |
| TLR4-def | 85.9 ± 3.3 | 6 | 85.2 ± 1.3 | 6 | 3368.9 ± 207.9 | 6 | 3299.4 ± 172.9 | 6 |
| Trif−/− | 74.7 ± 4.6 | 5 | 77.0 ± 4.4 | 6 | 2963.7 ± 239.4 | 5 | 3033.0 ± 157.9 | 6 |
| MyD88−/− | 88.6 ± 4.3 | 7 | 94.8 ± 1.9 | 6 | 3376.7 ± 131.9 | 7 | 3732.8 ± 83.7 | 6 |
| iNOS−/− | 84.8 ± 3.2 | 6 | 83.3 ± 2.4 | 6 | 3058.2 ± 120.8 | 6 | 2969.5 ± 40.9 | 6 |
| sGC−/− | 90.2 ± 1.9 | 10 | 91.8 ± 2.1 | 11 | 3564.2 ± 117.5 | 10 | 3723.7 ± 114.1* | 11 |
P < 0.05 versus the Saline control.
iNOS = inducible nitric-oxide synthase; LPS = lipopolysaccharide; LVDP = left ventricular developed pressure; MyD88 = myeloid differentiation factor 88; sGC = soluble guanylate cyclase; WTBL/6 = wild-type C57BL/6J; WTBL/10 = wild-type C57BL/10ScSn; TLR = toll-like receptor; Trif = TIR-domain-containing adaptor protein inducing interferon-β mediated transcription-factor.
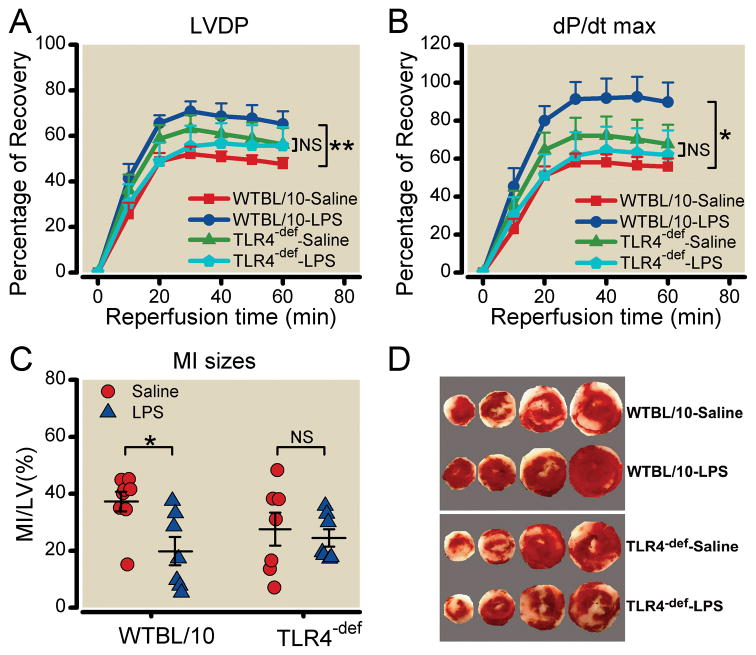
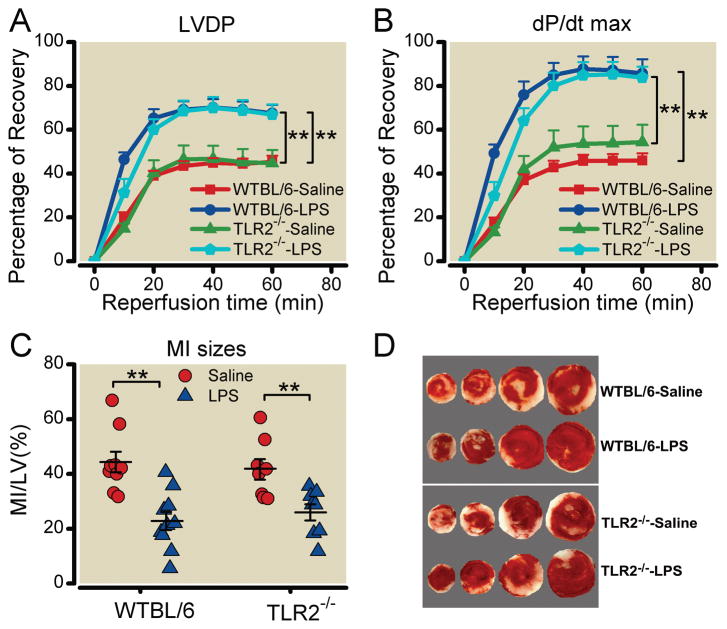
Pretreatment with the low dose of lipopolysaccharide, however, conferred a marked cardiac protection against I/R injury. As indicated in figure 2 A–B, after 30 min of ischemia and 60 min of reperfusion, LV function, as measured by LVDP and dP/dtmax, recovered to 47.6 ± 2.8% and 55.8 ± 4.4% of the baseline, respectively, in WT mice treated with saline (WTBL/10-Saline) (n = 9/group). In comparison, the hearts isolated from the lipopolysaccharide-treated mice (WTBL/10-lipopolysaccharide) exhibited significantly better LVDP (65.2 ± 5.6% at 60 min, P < 0.01) and dP/dtmax (89.8 ± 10.2% at 60 min, n = 8, P < 0.05) compared to the WTBL/10-saline group. The significant difference between WTBL/10-Saline and WTBL/10-LPS displayed as early as 10 min after reperfusion based on Bonferroni post hoc test. In addition, 30 min of ischemia and 60 min of reperfusion resulted in significant myocardial infarction in WT mice (MI/LV: 37.2 ± 3.4%, n = 8). lipopolysaccharide pretreatment led to a marked reduction in MI sizes (19.8 ± 4.9%, n = 7 P < 0.05,) (fig. 2 C–D). To determine whether TLR4 mediates the lipopolysaccharide-elicited cardiac protection, we tested the lipopolysaccharide preconditioning in the TLR4-deficient mice (TLR4-def). As indicated in figure 2, LVDP, dP/dtmax, and MI sizes after 30 min of ischemia and 60 min of reperfusion were similar in saline and lipopolysaccharide-treated TLR4-def mice, suggesting the inability of lipopolysaccharide to induce cardiac protection in the TLR4-def mice. In contrast, similar to their WT controls (C57BL/6J), TLR2−/− mice treated with lipopolysaccharide had improved LV function and reduced MI sizes (fig. 3). It is noteworthy that the two strains of WT mice, TLR4-def and TLR2−/− mice all had the same baseline LV function prior to I/R as demonstrated by LVDP and dP/dtmax in the Langendorff system (table 2). Taken together, these data demonstrate that TLR4, not TLR2, specifically mediates the lipopolysaccharide-induced cardiac protection against I/R injury.
Fig. 2. Lipopolysaccharide-elicited preconditioning against I/R injury is present in WT, but not in TLR4-def mice.
Wild-type C57BL/10ScSn strain (WTBL/10) and Toll-like receptor 4-deficient (TLR4-def ) mice were treated with normal saline or 0.1 mg/kg of lipopolysaccharide (LPS) intraperitoneally. Twenty-four hours later, mouse hearts were isolated and perfused in a Langendorff apparatus. After 30 min of perfusion, the hearts were subjected to 30 min of no-flow global ischemia followed by 60 min of reperfusion as described in the Methods. Left ventricular developed pressure (LVDP) and dP/dtmax were continuously measured and recorded. A. LVDP and B. dP/dtmax , expressed as percentage of the baseline. Each data point and error bar in A–B represents the mean ± SE. The number of mice in each group is as follows: WTBL/10-Saline: 9, WTBL/10-LPS: 8, TLR4-def-Saline: 6, TLR4-def-LPS: 6. *P < 0.05, **P < 0.01. NS, not significant. C. Myocardial infarction (MI) sizes expressed as the percentage of LV area. The horizontal lines represent the mean ± SE. *P < 0.05. D. Representative heart slices after triphenyltetrazolium chloride staining from WT and TLR4-def mice. Viable myocardium was stained red and infarcted myocardium white.
Fig. 3. TLR2 deficiency has no impact on lipopolysaccharide-elicited preconditioning against I/R injury.
Wild-type C57BL/6J (WTBL/6) and Toll-like receptor 2 knockout (TLR2−/−) mice were treated with normal saline or 0.1 mg/kg of lipopolysaccharide (LPS) intraperitoneally. Twenty-four hours later, mouse hearts were isolated and perfused in a Langendorff system. After 30 min of perfusion, the hearts were subjected to 30 min of no-flow global ischemia followed by 60 min of reperfusion. A. Left ventricular developed pressure (LVDP); B. dP/dtmax, expressed as percentage of the baseline. Each data point and error bar in A–B represents the mean ± SE. The number of mice in each group is as follows: WTBL/6-Saline: 10, WTBL/6-LPS: 11, TLR2−/−-Saline: 8, TLR2−/−-LPS: 8. **P < 0.01. C. Myocardial infarction (MI) size as expressed as the percentage of left ventricle area (LV). The horizontal lines represent the mean ± SE. **P < 0.01. D. Representative heart slices after triphenyltetrazolium chloride staining from WT and TLR2−/− mice. Viable myocardium was stained red and infarcted myocardium appeared white.
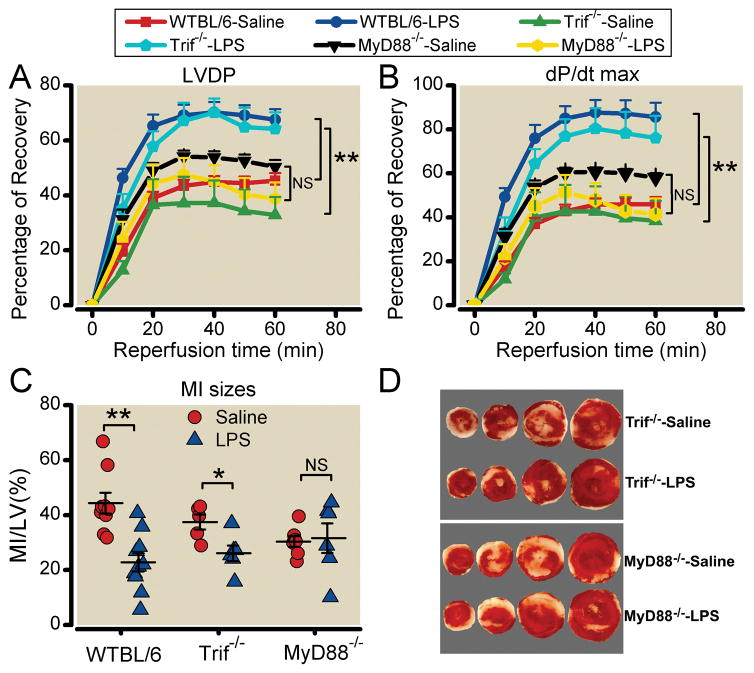
MyD88, not Trif, is essential for the TLR4-mediated cardioprotection against I/R injury
MyD88 and Trif are two adaptors that are critical for TLR4 signaling and mediate activation of NF-κB and interferon regulatory factor 3 (IRF3), respectively. To determine whether the two signaling pathways control the TLR4-induced cardioprotection, we tested the lipopolysaccharide preconditioning effect in MyD88−/− and Trif−/− mice. Both MyD88−/− and Trif−/− mice had the same baseline LV function compared to WT mice prior to I/R (table 2). LV function was similarly impaired in the saline-treated MyD88−/− and Trif−/− mice (fig. 4). Compared to the saline-treated Trif−/− animals, lipopolysaccharide-treated Trif−/− mice had a significant improvement in LVDP and dP/dtmax, and reduced MI sizes following I/R, a protective effect similar to that seen in the WT controls (WTBL6-LPS) (fig. 4). In contrast, lipopolysaccharide pretreatment failed to improve the LV function or reduce MI size in MyD88−/− mice (fig. 4). These data suggest that MyD88, but not Trif, signaling mediates the lipopolysaccharide-induced cardioprotection against I/R injury.
Fig. 4. Lipopolysaccharide-elicited preconditioning against I/R injury is MyD88-dependent, but Trif-independent.
Wild-type C57BL/6J (WTBL/6), Myeloid differentiation factor 88 knockout (MyD88−/−), and TIR-domain-containing adaptor protein inducing interferon-β–mediated transcription-factor knockout (Trif−/−) mice were treated with normal saline or 0.1 mg/kg of lipopolysaccharide (LPS) intraperitoneally. Twenty-four hours later, mouse hearts were isolated and perfused in a Langendorff system. After 30 min of perfusion, the hearts were subjected to 30 min of no-flow global ischemia followed by 60 min of reperfusion. A. Left ventricular developed pressure (LVDP); B. dP/dtmax, expressed as percentage of the baseline. Each data point and error bar in A–B represents the mean ± SE. The number of mice in each group is as follows: WTBL/6-Saline: 10, WTBL/6-LPS: 11, Trif−/−-Saline: 6, Trif−/−-LPS: 6, MyD88−/−-Saline: 7, MyD88−/−-LPS: 7. **P < 0.01. NS, not significant. C. Myocardial infarction (MI) size as expressed as the percentage of left ventricle area (LV). The long and short horizontal lines represent the mean ± SE. *P < 0.05, **P < 0.01, NS, not-significant. D. Representative heart slices after triphenyltetrazolium chloride staining from Trif−/− and MyD88−/− mice. Viable myocardium was stained red and infarcted myocardium appeared white.
TLR4 activation induces nitric oxide production in a MyD88-dependent manner
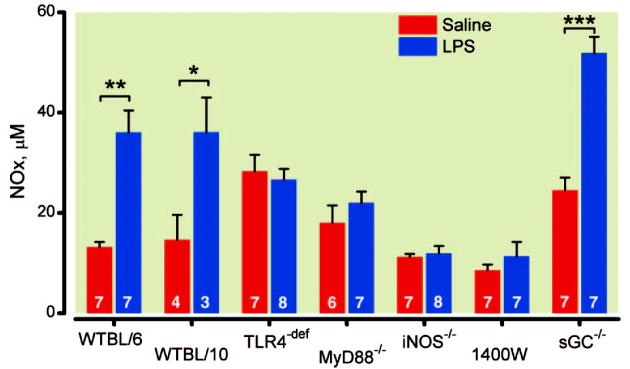
TLR4 stimulation induces iNOS induction 7,21 and activates the nitric oxide-sGC signaling pathway. To determine if iNOS-NO-sGC signaling mediates the TLR4-induced cardioprotection, we tested whether lipopolysaccharide, at the dose of 0.1 mg/kg, induced nitric oxide production. Nitric oxide has an extremely short life of a few ms in vivo, making direct measurement of nitric oxide particularly challenging. Plasma nitrate and nitrite levels, as a measure of N nitric oxide production, were measured at 24 h after saline or lipopolysaccharide injection. As indicated in figure 5, lipopolysaccharide induced a 2.7-fold increase in the plasma level of NOx of WTBL/6 mice (13.2 ± 1.0 vs. 36 ± 4.4 μM, P < 0.01) and a 2.5-fold increase in WTBL/10 mice (14.6 ± 5.0 vs. 36.1 ± 6.9 μM, P < 0.05). TLR4 or MyD88 deficiency resulted in an inability of lipopolysaccharide to increase the plasma levels of NOx although the TLR4-def mice had a higher level of baseline NOx than that of WT (C57BL/10) (P < 0.05). Moreover, iNOS−/− mice did not respond to lipopolysaccharide with the plasma NOx at the baseline level of the saline group (fig. 5). Importantly, 1400W, a highly selective and potent iNOS inhibitor 30, blocked NO induction in the lipopolysaccharide-treat WT mice. These data suggest that a low dose of lipopolysaccharide induces nitric oxide production in a TLR4- and MyD88-dependent manner and that either iNOS genetic deletion or inhibition blocks nitric oxide production in response to lipopolysaccharide in vivo.
Fig. 5. Effect of low dose lipopolysaccharide on the plasma concentrations of nitrite/nitrate in different mouse strains.
Mice were treated with normal saline or 0.1 mg/kg of lipopolysaccharide (LPS) intraperitoneally. 1400W (20 mg/kg) was given to wild-type C57BL/6J (WTBL/6) mice 2 hours before saline or LPS administration. Twenty-four hours later, blood was collected and plasma prepared. Nitrite and nitrate were measured using a fluorometric assay. Each error bar represents the mean ± SE. The number shown in each bar represents the sample size in the group. *P < 0.05, **P < 0.01, ***P < 0.001. iNOS−/− = inducible nitric-oxide synthase knockout; 1400W = N-(3-(Aminomethyl)benzyl)acetamidine; MyD88−/− = myeloid differentiation factor 88 knockout; sGC−/− = soluble guanylate cyclase knockout; TLR4-def = toll-like receptor 4-deficient; WTBL/6 = wild-type C57BL/6J; WTBL/10 = wild-type C57BL/10ScSn.
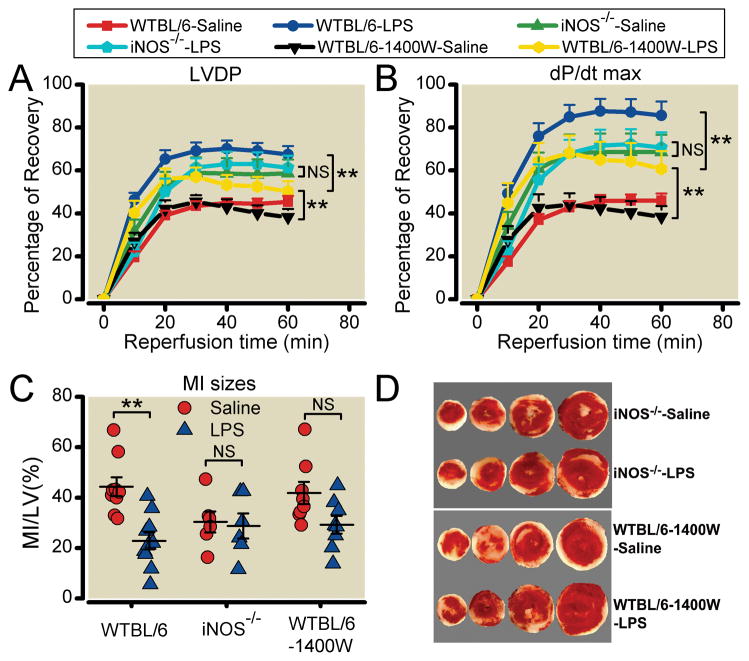
iNOS is critical for the TLR4-mediated cardioprotection
We next tested the impact of iNOS genetic deletion or pharmacological inhibition on the TLR4-mediated cardioprotection. As indicated in figure 6, iNOS genetic deletion (iNOS−/−) abolished the lipopolysaccharide-induced cardiac preconditioning. LV function and MI size were similar between the saline- and lipopolysaccharide-treated iNOS−/− mice (LVDP: 58.7 ± 6.4% vs. 61.3 ± 5.6%; dP/dtmax: 68.6 ± 8.1% vs. 70.7±7.0%; MI sizes: 30.4 ± 4.1% vs. 28.8 ± 5.1%, n = 6) (fig. 6). On the other hand, iNOS inhibition by 1400W significantly attenuated the ability of lipopolysaccharide to protect against I/R-induced LV dysfunction. While lipopolysaccharide treatment still resulted in a partial improvement in LV function in 1400W-pretreated mice (WTBL/6-1400W-LPS) compared to the saline control (WTB/6-1400W-Saline), the LV function recovery was significantly lower than that of the lipopolysaccharide-treated mice without 1400W pretreatment (WTBL/6-LPS) (P < 0.01) (fig. 6 A–B). 1400W pretreatment also blocked the lipopolysaccharide-induced MI reduction (fig. 6 C–D). Taken together, this series of studies demonstrate that iNOS genetic deletion or pharmacological inhibition blocks or inhibits the lipopolysaccharide-induced preconditioning, suggesting that iNOS and nitric oxide contribute to the lipopolysaccharide-induced and TLR4-mediated cardioprotection against I/R injury.
Fig. 6. Effect of iNOS deletion or inhibition on the lipopolysaccharide-elicited preconditioning against I/R injury.
Wild-type C57BL/6J (WTBL/6), WTBL/6 pre-treated with 1400W, and inducible nitric-oxide synthase knockout (iNOS−/−) mice were treated with normal saline or 0.1 mg/kg of lipopolysaccharide (LPS) intraperitoneally. 1400W was given at the dose of 20 mg/kg to WTBL/6 mice 2 hours before saline or LPS administration. Twenty-four hours later, mouse hearts were isolated and perfused in a Langendorff system and subjected to the I/R protocol. A. Left ventricular developed pressure (LVDP); B. dP/dtmax. expressed as percentage of the baseline. Each data point and error bar in A–B represents the mean ± SE. The number of mice in each group is as follows: iNOS−/−-Saline: 7, iNOS−/−-LPS: 8, WTBL/6-1400W-Saline: 7, WTBL/6-1400W-LPS: 7. **P < 0.01. NS, not-significant. C. Myocardial infarction (MI) size as expressed as the percentage of left ventricle area (LV). The long and short horizontal lines represent the mean ± SE. **P < 0.01. D. Representative heart slices after triphenyltetrazolium chloride staining from iNOS−/− and WT mice pretreated with 1400W. Viable myocardium was stained red and infarcted myocardium appeared white.
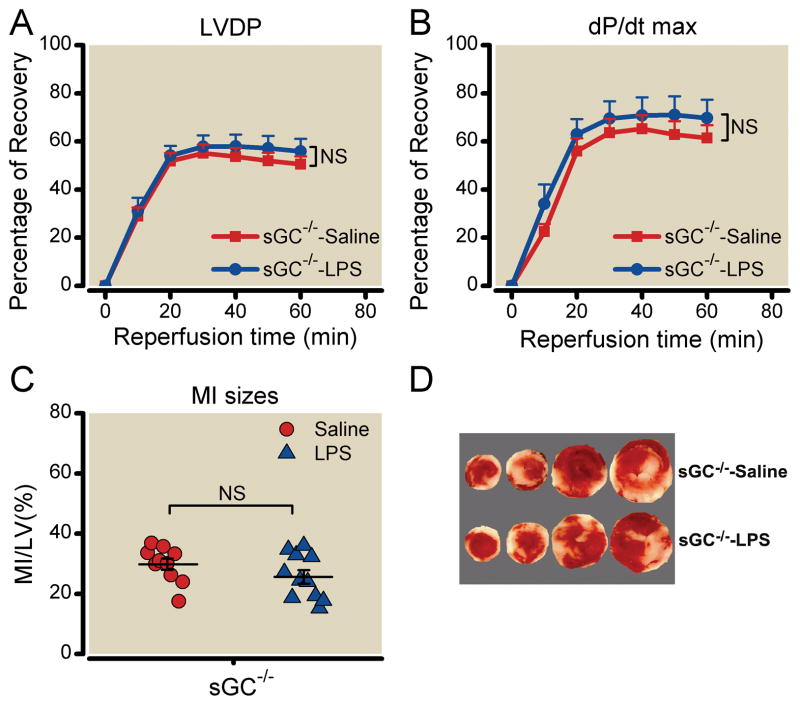
TLR4-mediated cardioprotection is sGC-dependent
Nitric oxide elicits its biological activity via either cGMP-dependent or cGMP-independent mechanisms. Soluble guanylate cyclase (sGC) is the primary target of nitric oxide and a heme-containing heterodimeric enzyme that is responsible for cGMP generation. The sGCα β heterodimer is considered to be the principal cardiovascular isoform. To determine if TLR4-induced cardioprotection is sGC-dependent, we employed mice deficient in the sGCα1 subunit 28. These mice have severely impaired sGC enzymatic activity that is not activated by NO or synthetic sGC activator 28. As expected, as a downstream target of nitric oxide, sGCα1 deficiency had no apparent effect on the ability of lipopolysaccharide to enhance nitric oxide production. sGCα1−/− mice had a marked increase in NOx production in response to lipopolysaccharide (P < 0.001) although these mice also had higher level in their baseline NOx compared to the WT control mice (24.5 ± 2.5 μM vs.13.2 ±1.0 μM, P < 0.01) (fig. 5). Importantly, despite the robust nitric oxide production following the lipopolysaccharide treatment, these sGCα1−/− mice were not protected by the lipopolysaccharide-elicited preconditioning. As indicated in figure 7, sGCα1−/− treated with lipopolysaccharide had the same level of LVDP and dP/dtmax, and same MI size as the saline-treated sGCα1−/− controls. It is noteworthy that similar to other genetically modified mice, sGCα1−/− mice had the same baseline LV function prior to ischemia as demonstrated by LVDP and dP/dtmax (table 2).
Fig. 7. Effect of sGC-deficiency on the lipopolysaccharide-elicited preconditioning against I/R injury.
Soluble guanylate cyclase knockout (sGCα1−/−) female mice were treated with normal saline or 0.1 mg/kg of lipopolysaccharide (LPS) intraperitoneally. Twenty-four hours later, mouse hearts were isolated and perfused in a Langendorff system. After 30 min of perfusion, the hearts were subjected to 30 min of no-flow global ischemia followed by 60 min of reperfusion. A. Left ventricular developed pressure (LVDP); B. dP/dtmax, expressed as percentage of the baseline. Each data point and error bar in A–B represents the mean ± SE. The number of mice in each group is as follows: WTBL/6-Saline: 10, WTBL/6-LPS: 11, sGCα1−/−-Saline: 10, sGCα1−/−-LPS: 11. *P < 0.05, **P < 0.01, NS, not-significant. C. Myocardial infarction (MI) size as expressed as the percentage of left ventricle area (LV). The long and short horizontal lines represent the mean ± SE. *P < 0.05, **P < 0.01. D. Representative heart slices after triphenyltetrazolium chloride staining from sGCα1−/− mice. Viable myocardium was stained red and infarcted myocardium white.
DISCUSSION
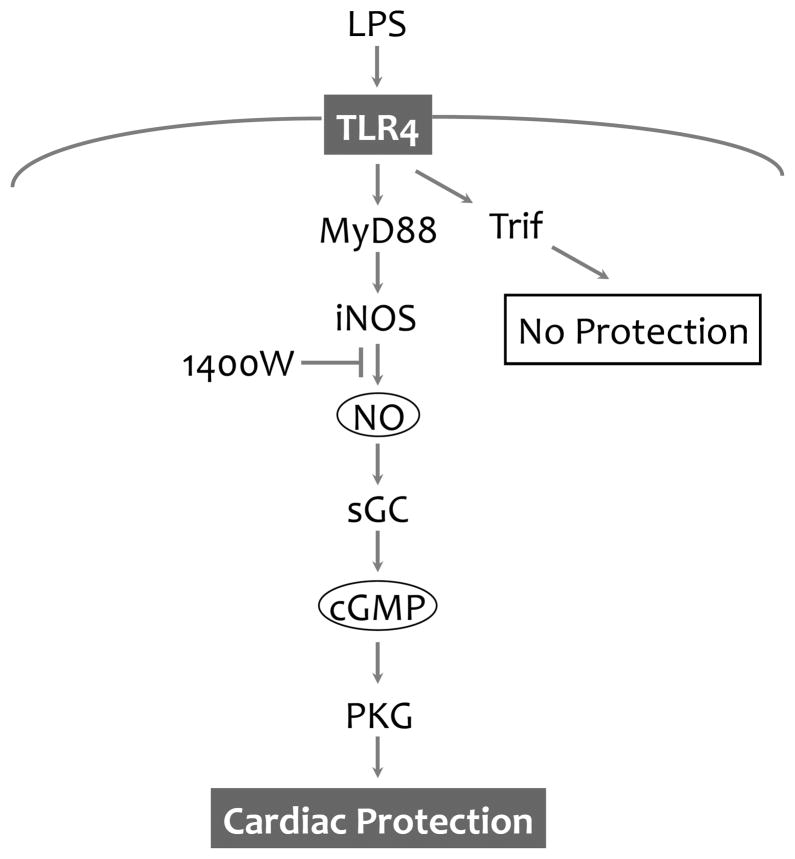
The current study was designed to delineate the intracellular signaling pathway that leads to the lipopolysaccharide-induced cardiac preconditioning against I/R injury. A small dose of lipopolysaccharide (0.1 mg/kg) did not effect the baseline LV function as assessed by serial echocardiography and LV pressure measurements, but it elicited a marked cardiac protective effect against I/R. Using genetically modified mouse strains and an ex-vivo model of cardiac I/R injury, we demonstrated that TLR4 mediated the lipopolysaccharide-elicited cardiac protection and MyD88, but not Trif, was essential for the TLR4-induced protection. The small dose of lipopolysaccharide also resulted in a significant increase in the plasma level of nitrate/nitrite. The lipopolysaccharide-induced NOx production and cardiac protection were abolished or significantly attenuated in iNOS−/− mice or in WT pretreated with an iNOS inhibitor. While sGCα1−/− mice responded to lipopolysaccharide with a robust nitric oxide production, they were not protected from I/R injury. Taken together, these data suggest that TLR4 activation confers a potent cardiac protection against I/R injury via a MyD88-dependent, but Trif-independent mechanism. Moreover, iNOS and sGCα1 are proven to be essential for the TLR4-induced cardiac protection (fig. 8).
Fig. 8. Proposed signaling pathway for the TLR4-mediated cardiac protection against I/R.
TLR4 activation by its ligand such as LPS leads to iNOS induction and increased NO production through a MyD88-dependent mechanism. NO protects myocardium via sGC- and cGMP/PKG-dependent mechanisms. 1400W, a potent iNOS inhibitor, blocks LPS/TLR4-induced NO production and inhibits its cardiac protection. In contrast, Trif is not required for the TLR4-mediated cardiac protection. LPS = lipopolysaccharide; iNOS = inducible nitric-oxide synthase; MyD88 = myeloid differentiation factor 88; sGC = soluble guanylate cyclase; PKG = protein kinase G; TLR = toll-like receptor; Trif = TIR-domain-containing adaptor protein inducing interferon-β–mediated transcription factor.
Cardiac preconditioning is a well-documented phenomenon where a brief treatment triggers endogenous survival mechanisms that protect the heart against I/R injury. Classic ischemic preconditioning, e.g., a brief period (e.g., 5 min) of repeated coronary artery occlusion, protects the myocardium against subsequent lethal I/R injury 18. Inhaled anesthetics also triggers cardiac preconditioning that improves cardiac function and reduced infarction sizes 19. Similarly, a few TLR ligands including lipopolysaccharide, monophosphoryl Lipid A (MLA), and lipoteichoic acid (a TLR2 ligand) can trigger cardiac protection that mimics the ischemic or anesthetic cardiac preconditioning 31–35. While lipopolysaccharide-induced cardiac protection has been well documented 5,20,23,31,36–39, the exact mechanisms that lead to the protection have not been fully understood. Administration of lipopolysaccharide leads to a robust systemic production of various cytokines and chemokines, such as TNFα, IL-1, and IL-6, and hemodynamic disturbance, which can impact on cardiac function. Given the systemic responses following in vivo lipopolysaccharide administration, it is unclear whether the observed cardiac benefits in lipopolysaccharide-treated animals are the direct results of TLR4 signaling or due to other events secondary to systemic TLR4 activation. The current study has clearly established that TLR4 signaling mediates the lipopolysaccharide-induced cardioprotective effect.
We also demonstrate that the TLR4-mediated preconditioning is MyD88-dependent but Trif-independent. These finding appear consistent with our previous in vitro finding that in isolated cardiomyocytes, direct activation of TLR4 by lipopolysaccharide confers a marked survival benefit in cardiomyocytes against apoptotic cell death during hypoxia and serum deprivation. The TLR4-induced cell survival pathway is mediated via MyD88 21. MyD88 is a key adaptor protein that is critical for transducing signals from all TLR family members 2,40–42, except TLR3, and interleukin-1 receptor family members. MyD88 signals via IRAK-1 and other downstream kinases including IKKβ and IκB, eventually leading to the activation of NF-κB and inflammatory cytokine production 3. On the other hand, Trif is a key adaptor protein responsible for TLR3 and TLR4 signaling pathways that respond to viral and bacterial stimulation and result in the production of type I interferons including IFNα, IFNβ, and other IFNs 4. Stimulation of type I interferon pathways leads to induction of a specific set of genes including chemokines (e.g., CXCL10) 43 and anti-microbial/antiviral response genes 44. The detailed mechanisms by which each of the signaling component lead to the cardioprotection seen in lipopolysaccharide-treated animals need to be further investigated. Nevertheless, the present finding strongly suggests that TLR4-MyD88 signaling, upon activated, triggers a potent survival mechanism that protects the heart against I/R injury (fig. 8).
NOS and nitric oxide have been implicated as a key intracellular mediator responsible for both ischemic preconditioning and anesthetic preconditioning 45,46. iNOS, the inducible form of NOS, is considered essential for the late phase of ischemic preconditioning in an in vivo model of I/R injury 45. Moreover, over-expression of iNOS is found sufficient to protect myocardium from I/R injury 47. Interestingly, NOS1 or endothelial NOS, but not iNOS, has been proposed as the trigger for the isoflurane-induced preconditioning in a rabbit model of I/R injury 46. Our finding that TLR4-MyD88 signaling is required for nitrate/nitrite production in response to a preconditioning dose of lipopolysaccharide and that iNOS genetic deletion as well as pharmacological inhibition attenuate the TLR4-mediated cardiac preconditioning strongly suggest that iNOS- nitric oxide is the downstream effector of TLR4 signaling leading to the lipopolysaccharide-elicited preconditioning benefit against I/R. This is consistent with a previous study by Xi and colleagues who reported that monophosphoryl lipid A-induced preconditioning was abolished in iNOS−/− mice 32. The notion that cardiac TLR4 is directly activated by lipopolysaccharide and subsequently leads to an iNOS-dependent cardiac protection against I/R injury is supported by our previous finding that TLR4 activation in isolated cardiomyocytes leads to a direct anti-apoptotic survival pathway that is dependent on endogenous iNOS 21,22. It is noteworthy that while the selective iNOS inhibitor 1400W completely inhibited the increase in the nitrate/nitrite production in the lipopolysaccharide-treated mice, it only partially blocked the lipopolysaccharide-elicited LV functional improvement. These may suggest that in addition to nitric oxide, other factor(s) may also contribute to the TLR4-induced and iNOS-dependent cardiac protection.
Nitric oxide may confer myocardial protection by cGMP-dependent as well as cGMP-independent mechanisms. For example, nitric oxide inhibits caspase-3 activity via S-nitrosylation and thus may promote cell survival in a sGC/cGMP-independent manner 48. On the other hand, nitric oxide can bind to the heme moiety of sGC and activate the enzyme to generate cGMP. sGC is a main downstream effector of nitric oxide and responsible for many nitric oxide-elicited biological effects. Here we demonstrate that the TLR4-mediated cardioprotection against I/R injury is indeed dependent on sGCα1. Mice deficient in sGCα1 completely lost the protection conferred by lipopolysaccharide despite sGCα1−/− mice responded normally to lipopolysaccharide with a robust nitric oxide production.
Another endogenous survival pathway, namely phosphatidylinositol-3 kinase (PI3 kinase)/Akt, has been proposed for the lipopolysaccharide-induced cardiac protective effect. We have previously demonstrated that PI-3 kinase/Akt, extracellular signal-regulated kinase 1/2 (ERK1/2), and IκB kinase β (IKKβ) pathways all contribute to the lipopolysaccharide-induced anti-apoptotic survival effect in cardiomyocytes 22. Moreover, in vivo, the cardiac benefit of lipopolysaccharide against I/R injury is abolished by a PI-3 kinase inhibitor or in transgenic mice expressing inactive Akt mutant 39.
Some limitations of the present study should be acknowledged. First, using the in vivo model, we were not able to determine whether the cardiac ischemic protection in the lipopolysaccharide-treated mice is result of direct myocardial TLR4 activation. While our previous in vitro data suggest a direct survival benefit of TLR4-MyD88 signaling in cardiomyocytes 22, other approaches will be needed, such as cardiac specific TLR4 knock-out or chimera model 17, to define the specific role of cardiac TLR4 in myocardial protection against I/R injury. Second, lipopolysaccharide is a potent pyrogenic agent and thus clearly not a good candidate to test its therapeutic value in attenuating I/R injury. Nonpyrogenic TLR4 agonists will be needed to further test the efficacy of TLR4 signaling to protect against I/R injury. Finally, I/R injury model in this study was developed in isolated hearts perfused in a Langendorff apparatus. While the ex-vivo system offers certain advantages, such as relative ease to perform, the ability to control left ventricular pre- and after-load, and the ability to continuously measure cardiac contractile function throughout I/R period, the heart is perfused with cell- and serum-free buffer and thus certain neuro-hormonal factors in response to I/R could have been omitted. In this regard, in vivo I/R injury model involving coronary artery occlusion offers clear advantage 49–51. Both experimental models have been widely used by numerous laboratories including ours10,16,17.
Nevertheless, the present study establishes that TLR4 activation confers a potent cardiac protection against I/R injury via a MyD88-dependent, but Trif-independent mechanism. Moreover, iNOS and sGC 1 are proven to be essential for the TLR4-induced cardiac protection (fig. 8). Our study suggests that selective targeting TLR4-MyD88 signaling may represent a novel therapeutic strategy for cardioprotection against ischemic myocardial injury.
Acknowledgments
This work was supported by the National Institutes of Health grant GM-080906 (Bethesda, Maryland) and American Heart Association grant 0755890T (Dallas, Texas).
The authors would like to thank Dr. Fumito Ichinose of Massachusetts General Hospital for the critical discussions on the project and Dr. Hui Zheng of Massachusetts General Hospital Biostatistics Center for his advice on statistical analysis.
References
- 1.Akira S, Takeda K, Kaisho T. Toll-like receptors: Critical proteins linking innate and acquired immunity. Nat Immunol. 2001;2:675–80. doi: 10.1038/90609. [DOI] [PubMed] [Google Scholar]
- 2.Kawai T, Akira S. TLR signaling. Cell Death Differ. 2006;13:816–25. doi: 10.1038/sj.cdd.4401850. [DOI] [PubMed] [Google Scholar]
- 3.O'Neill LA, Bowie AG. The family of five: TIR-domain-containing adaptors in Toll-like receptor signalling. Nat Rev Immunol. 2007;7:353–64. doi: 10.1038/nri2079. [DOI] [PubMed] [Google Scholar]
- 4.Uematsu S, Akira S. Toll-like receptors and Type I interferons. J Biol Chem. 2007;282:15319–23. doi: 10.1074/jbc.R700009200. [DOI] [PubMed] [Google Scholar]
- 5.Chao W. Toll-like receptor signaling: A critical modulator of cell survival and ischemic injury in the heart. Am J Physiol Heart Circ Physiol. 2009;296:H1–H12. doi: 10.1152/ajpheart.00995.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Knuefermann P, Nemoto S, Baumgarten G, Misra A, Sivasubramanian N, Carabello BA, Vallejo JG. Cardiac inflammation and innate immunity in septic shock: Is there a role for toll-like receptors? Chest. 2002;121:1329–36. doi: 10.1378/chest.121.4.1329. [DOI] [PubMed] [Google Scholar]
- 7.Nemoto S, Vallejo JG, Knuefermann P, Misra A, Defreitas G, Carabello BA, Mann DL. Escherichia coli LPS-induced LV dysfunction: Role of toll-like receptor-4 in the adult heart. Am J Physiol Heart Circ Physiol. 2002;282:H2316–23. doi: 10.1152/ajpheart.00763.2001. [DOI] [PubMed] [Google Scholar]
- 8.Zhu X, Bagchi A, Zhao H, Kirschning CJ, Hajjar RJ, Chao W, Hellman J, Schmidt U. Toll-like receptor 2 activation by bacterial peptidoglycan-associated lipoprotein activates cardiomyocyte inflammation and contractile dysfunction. Crit Care Med. 2007;35:886–92. doi: 10.1097/01.CCM.0000256723.37586.A2. [DOI] [PubMed] [Google Scholar]
- 9.Knuefermann P, Sakata Y, Baker JS, Huang CH, Sekiguchi K, Hardarson HS, Takeuchi O, Akira S, Vallejo JG. Toll-like receptor 2 mediates Staphylococcus aureus-induced myocardial dysfunction and cytokine production in the heart. Circulation. 2004;110:3693–8. doi: 10.1161/01.CIR.0000143081.13042.04. [DOI] [PubMed] [Google Scholar]
- 10.Zou L, Feng Y, Chen YJ, Si R, Shen S, Zhou Q, Ichinose F, Scherrer-Crosbie M, Chao W. Toll-like receptor 2 plays a critical role in cardiac dysfunction during polymicrobial sepsis. Crit Care Med. 2010;38:1335–42. doi: 10.1097/CCM.0b013e3181d99e67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaczorowski DJ, Mollen KP, Edmonds R, Billiar TR. Early events in the recognition of danger signals after tissue injury. J Leukoc Biol. 2008;83:546–52. doi: 10.1189/jlb.0607374. [DOI] [PubMed] [Google Scholar]
- 12.Arslan F, Smeets MB, O'Neill LA, Keogh B, McGuirk P, Timmers L, Tersteeg C, Hoefer IE, Doevendans PA, Pasterkamp G, de Kleijn DP. Myocardial ischemia/reperfusion injury is mediated by leukocytic toll-like receptor-2 and reduced by systemic administration of a novel anti-toll-like receptor-2 antibody. Circulation. 2010;121:80–90. doi: 10.1161/CIRCULATIONAHA.109.880187. [DOI] [PubMed] [Google Scholar]
- 13.Oyama J, Blais C, Jr, Liu X, Pu M, Kobzik L, Kelly RA, Bourcier T. Reduced myocardial ischemia-reperfusion injury in toll-like receptor 4-deficient mice. Circulation. 2004;109:784–9. doi: 10.1161/01.CIR.0000112575.66565.84. [DOI] [PubMed] [Google Scholar]
- 14.Chong AJ, Shimamoto A, Hampton CR, Takayama H, Spring DJ, Rothnie CL, Yada M, Pohlman TH, Verrier ED. Toll-like receptor 4 mediates ischemia/reperfusion injury of the heart. J Thorac Cardiovasc Surg. 2004;128:170–9. doi: 10.1016/j.jtcvs.2003.11.036. [DOI] [PubMed] [Google Scholar]
- 15.Kim SC, Ghanem A, Stapel H, Tiemann K, Knuefermann P, Hoeft A, Meyer R, Grohe C, Knowlton AA, Baumgarten G. Toll-like receptor 4 deficiency: Smaller infarcts, but no gain in function. BMC Physiol. 2007;7:5. doi: 10.1186/1472-6793-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feng Y, Zhao H, Xu X, Buys ES, Raher MJ, Bopassa JC, Thibault H, Scherrer-Crosbie M, Schmidt U, Chao W. Innate immune adaptor MyD88 mediates neutrophil recruitment and myocardial injury after ischemia-reperfusion in mice. Am J Physiol Heart Circ Physiol. 2008;295:H1311–8. doi: 10.1152/ajpheart.00119.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Feng Y, Zou L, Si R, Nagasaka Y, Chao W. Bone marrow MyD88 signaling modulates neutrophil function and ischemic myocardial injury. Am J Physiol Cell Physiol. 2010;299:C760–9. doi: 10.1152/ajpcell.00155.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bolli R. Preconditioning: A paradigm shift in the biology of myocardial ischemia. Am J Physiol Heart Circ Physiol. 2007;292:H19–27. doi: 10.1152/ajpheart.00712.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bienengraeber MW, Weihrauch D, Kersten JR, Pagel PS, Warltier DC. Cardioprotection by volatile anesthetics. Vascul Pharmacol. 2005;42:243–52. doi: 10.1016/j.vph.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 20.Meng X, Ao L, Brown JM, Meldrum DR, Sheridan BC, Cain BS, Banerjee A, Harken AH. LPS induces late cardiac functional protection against ischemia independent of cardiac and circulating TNF-alpha. Am J Physiol. 1997;273:H1894–902. doi: 10.1152/ajpheart.1997.273.4.H1894. [DOI] [PubMed] [Google Scholar]
- 21.Zhu X, Zhao H, Graveline AR, Buys ES, Schmidt U, Bloch KD, Rosenzweig A, Chao W. MyD88 and NOS2 are essential for toll-like receptor 4-mediated survival effect in cardiomyocytes. Am J Physiol Heart Circ Physiol. 2006;291:H1900–9. doi: 10.1152/ajpheart.00112.2006. [DOI] [PubMed] [Google Scholar]
- 22.Chao W, Shen Y, Zhu X, Zhao H, Novikov M, Schmidt U, Rosenzweig A. Lipopolysaccharide improves cardiomyocyte survival and function after serum deprivation. J Biol Chem. 2005;280:21997–2005. doi: 10.1074/jbc.M413676200. [DOI] [PubMed] [Google Scholar]
- 23.Wang YP, Sato C, Mizoguchi K, Yamashita Y, Oe M, Maeta H. Lipopolysaccharide triggers late preconditioning against myocardial infarction via inducible nitric oxide synthase. Cardiovasc Res. 2002;56:33–42. doi: 10.1016/s0008-6363(02)00506-0. [DOI] [PubMed] [Google Scholar]
- 24.Poltorak A, He X, Smirnova I, Liu MY, Van Huffel C, Du X, Birdwell D, Alejos E, Silva M, Galanos C, Freudenberg M, Ricciardi-Castagnoli P, Layton B, Beutler B. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: Mutations in Tlr4 gene. Science. 1998;282:2085–8. doi: 10.1126/science.282.5396.2085. [DOI] [PubMed] [Google Scholar]
- 25.Takeuchi O, Hoshino K, Kawai T, Sanjo H, Takada H, Ogawa T, Takeda K, Akira S. Differential roles of TLR2 and TLR4 in recognition of gram-negative and gram-positive bacterial cell wall components. Immunity. 1999;11:443–51. doi: 10.1016/s1074-7613(00)80119-3. [DOI] [PubMed] [Google Scholar]
- 26.Kawai T, Adachi O, Ogawa T, Takeda K, Akira S. Unresponsiveness of MyD88-deficient mice to endotoxin. Immunity. 1999;11:115–22. doi: 10.1016/s1074-7613(00)80086-2. [DOI] [PubMed] [Google Scholar]
- 27.Yamamoto M, Sato S, Hemmi H, Hoshino K, Kaisho T, Sanjo H, Takeuchi O, Sugiyama M, Okabe M, Takeda K, Akira S. Role of adaptor TRIF in the MyD88-independent toll-like receptor signaling pathway. Science. 2003;301:640–3. doi: 10.1126/science.1087262. [DOI] [PubMed] [Google Scholar]
- 28.Buys ES, Sips P, Vermeersch P, Raher MJ, Rogge E, Ichinose F, Dewerchin M, Bloch KD, Janssens S, Brouckaert P. Gender-specific hypertension and responsiveness to nitric oxide in sGCalpha1 knockout mice. Cardiovasc Res. 2008;79:179–86. doi: 10.1093/cvr/cvn068. [DOI] [PubMed] [Google Scholar]
- 29.Garvey EP, Oplinger JA, Tanoury GJ, Sherman PA, Fowler M, Marshall S, Harmon MF, Paith JE, Furfine ES. Potent and selective inhibition of human nitric oxide synthases. Inhibition by non-amino acid isothioureas. J Biol Chem. 1994;269:26669–76. [PubMed] [Google Scholar]
- 30.Garvey EP, Oplinger JA, Furfine ES, Kiff RJ, Laszlo F, Whittle BJ, Knowles RG. 1400W is a slow, tight binding, and highly selective inhibitor of inducible nitric-oxide synthase in vitro and in vivo. J Biol Chem. 1997;272:4959–63. doi: 10.1074/jbc.272.8.4959. [DOI] [PubMed] [Google Scholar]
- 31.Zacharowski K, Frank S, Otto M, Chatterjee PK, Cuzzocrea S, Hafner G, Pfeilschifter J, Thiemermann C. Lipoteichoic acid induces delayed protection in the rat heart: A comparison with endotoxin. Arterioscler Thromb Vasc Biol. 2000;20:1521–8. doi: 10.1161/01.atv.20.6.1521. [DOI] [PubMed] [Google Scholar]
- 32.Xi L, Jarrett NC, Hess ML, Kukreja RC. Essential role of inducible nitric oxide synthase in monophosphoryl lipid A-induced late cardioprotection: Evidence from pharmacological inhibition and gene knockout mice. Circulation. 1999;99:2157–63. doi: 10.1161/01.cir.99.16.2157. [DOI] [PubMed] [Google Scholar]
- 33.Mersmann J, Berkels R, Zacharowski P, Tran N, Koch A, Iekushi K, Dimmeler S, Granja TF, Boehm O, Claycomb WC, Zacharowski K. Preconditioning by toll-like receptor 2 agonist Pam3CSK4 reduces CXCL1-dependent leukocyte recruitment in murine myocardial ischemia/reperfusion injury. Crit Care Med. 2010;38:903–9. doi: 10.1097/CCM.0b013e3181ce50e6. [DOI] [PubMed] [Google Scholar]
- 34.Dong JW, Vallejo JG, Tzeng HP, Thomas JA, Mann DL. Innate immunity mediates myocardial preconditioning through Toll-like receptor 2 and TIRAP-dependent signaling pathways. Am J Physiol Heart Circ Physiol. 298:H1079–87. doi: 10.1152/ajpheart.00306.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chatterjee PK. Cardiac preconditioning by specific ligands of Toll-like receptors: Is it wither or whither? Crit Care Med. 38:1003–4. doi: 10.1097/CCM.0b013e3181cd10e5. [DOI] [PubMed] [Google Scholar]
- 36.Brown JM, Grosso MA, Terada LS, Whitman GJ, Banerjee A, White CW, Harken AH, Repine JE. Endotoxin pretreatment increases endogenous myocardial catalase activity and decreases ischemia-reperfusion injury of isolated rat hearts. Proc Natl Acad Sci U S A. 1989;86:2516–20. doi: 10.1073/pnas.86.7.2516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Song W, Furman BL, Parratt JR. Delayed protection against ischaemia-induced ventricular arrhythmias and infarct size limitation by the prior administration of Escherichia coli endotoxin. Br J Pharmacol. 1996;118:2157–63. doi: 10.1111/j.1476-5381.1996.tb15657.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Belosjorow S, Schulz R, Dorge H, Schade FU, Heusch G. Endotoxin and ischemic preconditioning: TNF-alpha concentration and myocardial infarct development in rabbits. Am J Physiol. 1999;277:H2470–5. doi: 10.1152/ajpheart.1999.277.6.H2470. [DOI] [PubMed] [Google Scholar]
- 39.Ha T, Hua F, Liu X, Ma J, McMullen JR, Shioi T, Izumo S, Kelley J, Gao X, Browder W, Williams DL, Kao RL, Li C. Lipopolysaccharide-induced myocardial protection against ischaemia/reperfusion injury is mediated through a PI3K/Akt-dependent mechanism. Cardiovasc Res. 2008;78:546–53. doi: 10.1093/cvr/cvn037. [DOI] [PubMed] [Google Scholar]
- 40.Medzhitov R, Preston-Hurlburt P, Kopp E, Stadlen A, Chen C, Ghosh S, Janeway CA., Jr MyD88 is an adaptor protein in the hToll/IL-1 receptor family signaling pathways. Mol Cell. 1998;2:253–8. doi: 10.1016/s1097-2765(00)80136-7. [DOI] [PubMed] [Google Scholar]
- 41.Muzio M, Ni J, Feng P, Dixit VM. IRAK (Pelle) family member IRAK-2 and MyD88 as proximal mediators of IL-1 signaling. Science. 1997;278:1612–5. doi: 10.1126/science.278.5343.1612. [DOI] [PubMed] [Google Scholar]
- 42.Janssens S, Beyaert R. A universal role for MyD88 in TLR/IL-1R-mediated signaling. Trends Biochem Sci. 2002;27:474–82. doi: 10.1016/s0968-0004(02)02145-x. [DOI] [PubMed] [Google Scholar]
- 43.Toshchakov V, Jones BW, Perera PY, Thomas K, Cody MJ, Zhang S, Williams BR, Major J, Hamilton TA, Fenton MJ, Vogel SN. TLR4, but not TLR2, mediates IFN-beta-induced STAT1alpha/beta-dependent gene expression in macrophages. Nat Immunol. 2002;3:392–8. doi: 10.1038/ni774. [DOI] [PubMed] [Google Scholar]
- 44.Sadler AJ, Williams BR. Interferon-inducible antiviral effectors. Nat Rev Immunol. 2008;8:559–68. doi: 10.1038/nri2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Guo Y, Jones WK, Xuan YT, Tang XL, Bao W, Wu WJ, Han H, Laubach VE, Ping P, Yang Z, Qiu Y, Bolli R. The late phase of ischemic preconditioning is abrogated by targeted disruption of the inducible NO synthase gene. Proc Natl Acad Sci U S A. 1999;96:11507–12. doi: 10.1073/pnas.96.20.11507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chiari PC, Bienengraeber MW, Weihrauch D, Krolikowski JG, Kersten JR, Warltier DC, Pagel PS. Role of endothelial nitric oxide synthase as a trigger and mediator of isoflurane-induced delayed preconditioning in rabbit myocardium. Anesthesiology. 2005;103:74–83. doi: 10.1097/00000542-200507000-00014. [DOI] [PubMed] [Google Scholar]
- 47.Li Q, Guo Y, Xuan YT, Lowenstein CJ, Stevenson SC, Prabhu SD, Wu WJ, Zhu Y, Bolli R. Gene therapy with inducible nitric oxide synthase protects against myocardial infarction via a cyclooxygenase-2-dependent mechanism. Circ Res. 2003;92:741–8. doi: 10.1161/01.RES.0000065441.72685.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rossig L, Fichtlscherer B, Breitschopf K, Haendeler J, Zeiher AM, Mulsch A, Dimmeler S. Nitric oxide inhibits caspase-3 by S-nitrosation in vivo. J Biol Chem. 1999;274:6823–6. doi: 10.1074/jbc.274.11.6823. [DOI] [PubMed] [Google Scholar]
- 49.Michael LH, Entman ML, Hartley CJ, Youker KA, Zhu J, Hall SR, Hawkins HK, Berens K, Ballantyne CM. Myocardial ischemia and reperfusion: A murine model. Am J Physiol. 1995;269:H2147–54. doi: 10.1152/ajpheart.1995.269.6.H2147. [DOI] [PubMed] [Google Scholar]
- 50.Tarnavski O, McMullen JR, Schinke M, Nie Q, Kong S, Izumo S. Mouse cardiac surgery: Comprehensive techniques for the generation of mouse models of human diseases and their application for genomic studies. Physiol Genomics. 2004;16:349–60. doi: 10.1152/physiolgenomics.00041.2003. [DOI] [PubMed] [Google Scholar]
- 51.Eckle T, Grenz A, Kohler D, Redel A, Falk M, Rolauffs B, Osswald H, Kehl F, Eltzschig HK. Systematic evaluation of a novel model for cardiac ischemic preconditioning in mice. Am J Physiol Heart Circ Physiol. 2006;291:H2533–40. doi: 10.1152/ajpheart.00472.2006. [DOI] [PubMed] [Google Scholar]