Abstract
Recently, the digital imaging and communications in medicine (DICOM) standard introduced rules for the encoding, transmission, and storage of the imaging diagnostic report. This medical document can be stored and communicated with the images in picture archiving and communication system (PACS). It is a structured document that contains text with links to other data such as images, waveforms, and spatial or temporal coordinates. Its structure, along with its wide use of coded information, enables the semantic understanding of the data that is essential for the Electronic Healthcare Record deployment. In this article, we present DICOM Structured Report (SR) and discuss its benefits. We show how SR enables efficient radiology workflow, improves patient care, optimizes reimbursement, and enhances the radiology ergonomic working conditions. As structured input significantly alters the interpretation process, understanding all its benefits is necessary to support the change.
Key Words: Digital Imaging and Communications in Medicine (DICOM), structured report, interpretation, Picture Archiving and Communication System (PACS), Radiology Information System (RIS), Integrating the Healthcare Enterprise (IHE)
Introduction
Prompt access to the patient’s entire relevant clinical information is central to assist in healthcare decisions. Modern electronic health record (EHR) promises to improve patient care by providing timely access to centralized clinical data that constitute the patient medical record. Such data includes patient history, diagnostic reports from different care domains, images, and other clinical data in electronic format. EHR requires defining frameworks for information sharing that offer capabilities for communicating the data. Therefore, most recent efforts have focused on defining unified data models and standards that address data access and security issues.1 However, as EHR provides access to information for a broad number of care providers, defined vocabularies and semantics are needed to ensure a consistent interpretation of that information. Defined vocabularies and semantics also enable the information to be automatically processed and analyzed by computer algorithms to assist in the diagnostic or to extract valuable information that may have a second use such as research or public health surveillance.2
The diagnostic imaging report is an important piece of information in the EHR. Although complete image sets are usually needed by radiologists and some other specialists such as surgeons and orthopedists, the imaging report, along with a very small set of relevant images, is needed by a very broad number of care providers. Therefore, the framework for sharing the report that includes communication capabilities, and common vocabularies and semantics is essential. Traditionally, the imaging report is dictated by a radiologist who is interpreting the images. The report is subsequently transcribed into an electronic document by a typist and verified by the radiologist.3 The generated document is in a prose format. It is shared with the referring physician and other clinicians.
Recently, the Digital imaging and communications in medicine (DICOM) standard introduced the Structured Report (SR) to encode the imaging diagnostic report. It specified rules for its encoding, transmission, and storage. Besides being stored and transferred with the images that were used to generate it, DICOM SR is a structured document that contains text with links to other data such as images, waveforms, and spatial or temporal coordinates. Its structure, along with its wide use of coded information, enables the semantic understanding of the data that is essential for the EHR.4 Using a code to designate the ankle, for example, allows the diagnostic document to travel across local definitions and language barriers. Moreover, SR encoding and structure permit sophisticated queries and data mining operation such as a query for all documents where a malignant mass of a specific dimension is reported. Furthermore, links to other data (e.g., images) provide a way to integrate the image (i.e., the interpretation input) with the interpretation output in the same document.5–7
DICOM SR requires the use of codes, but does not impose constraints on the coded vocabulary. Likewise, it describes possible structures with limited constraints on the relationship between nodes without imposing additional restrictions.3 Many DICOM standard templates have been subsequently defined to constrain the possible structures and to provide some basic codes that can be used to encode specific reports such as breast imaging or vascular ultrasound procedures reports. Codes may be extended to use Radlex, a lexicon for radiology that is being developed by the Radiological Society of North America in collaboration with other professional organizations and standard bodies.
DICOM SR fulfills the imaging document encoding and archiving needs. But DICOM is not used outside the radiology department, primarily because the standard historically addressed mainly the encoding and communication of images, and also because it is based on a binary encoding and imposes rigid encoding and semantic constraints. Consequently, DICOM SR must be encoded and transmitted by using a different standard to travel out of the radiology department. Such standard may consist of Health Level 7 (HL7) when communicating with specialized dedicated healthcare workstation. Or, to broaden its availability, the DICOM report could be rendered on a web-enabled EHR workstation by using a straightforward presentation encoding such as HTML or portable document format (PDF). DICOM SR can be easily transformed into another format by using transform engine software and applying transformation rules.
The biggest challenge that faces the wide adoption of SR is structured input as it affects the radiologist’s interpretation process. Therefore, a recent study8 has focused on using natural language processing to dissect and structure clinical narrative reports. The limitations of this study have been discussed by Langlotz9 and have been presented as inherent shortcomings of narrative reports themselves. It has also been stated that narrative reports do not always address key clinical questions, may contain clinically important errors, are not transmitted in a timely fashion, and may contain ambiguous terms.9 Moreover, if specific organs are not mentioned in the report, then the clinician is unsure whether these organs were examined. Consequently, encoding structured reports is hardly achieved with natural language processing. On the contrary, it is more likely to involve direct structured input by the radiologist, thereby requiring a change in how radiologists record their interpretation. Fortunately, it has been shown in 10 that radiologists and referring physicians prefer structured reports. They also prefer complete reports as opposed to summarized reports that contain essential information.
In this article, we briefly present the structural and coded content of DICOM SR and we focus on its benefits. We believe that these benefits are significant. Understanding their importance helps overcome the possible resistance to change in the interpretation process.
A complete and exhaustive description of DICOM SR can be found in Clunie’s work.7 DICOM SR is a multimedia document that can include references to audio and images. A formal document type definition of the DICOM SR can be found in the work of Noumeir.3 Furthermore, object models are also presented and discussed by Noumeir6 and Clunie.7
SR Content
Similar to a DICOM image, the DICOM report has a header and content. Its header shares the same information with the images header that are interpreted to generate it, such as about the patient and the study information. Therefore, the report usually belongs to the same study as the interpreted images. Additionally, the report header carries specific information about the following:
Status, whether it is verified, or whether it is completed or partial;
Content creation date and time;
Verifying person name and organization;
References to predecessor documents, such as older document versions;
References to identical documents;
References to evidences, such as current images or evidence documents;
References to other pertinent evidences, such as prior images or prior reports.
On the other hand, the report content is hierarchically arranged into a structure. The information at different hierarchy levels lies within information elements that are of different types such as text, numerical values, spatial or temporal coordinates, and references to images or waveforms. The information elements are hierarchically connected to form a tree. The relationship between any two information elements has an explicit type. This type is one of: contains, has properties, inferred from, selected from, has observation context, has acquisition context, and has concept modifier. Images and waveforms are referenced from within the document content. They are not included inside the document but can be managed along with it.
Each information element has a name and a value, as depicted in Figure 1. The name defines what the value represents. For example, the name of a section is its heading. The name of a measurement is what the numerical value represents, for example, a diameter.
Fig 1.
An information element has a name and a value.
To facilitate indexing and searching, the name is always defined by a code, as shown in Figure 2. In fact, the use of defined coded terms—rather than plain text—to describe information values enables precise searches. Codes provide consistency of terminology independently of synonyms and languages. A code is composed of a value and a coding scheme designator. The coding scheme designator ensures that the code value is unique within its scope. A code has also a code meaning whose sole purpose is to describe it in a human readable text.
Fig 2.
The name is defined by a code.
Benefits
DICOM SR has many benefits that will be presented and discussed hereinafter.
Better Communication with the Referring Physician
Referring physicians prefer to read structured report.10 Structured reports can be very concise and complete. They are easier and faster to read, especially when the important elements of the structure are presented in such a way that they are in evidence or highlighted. For instance, the presence of a mass, its dimension, its position, and its characteristics can be automatically displayed or printed in bold for a faster, easier, and more effective communication to the reader about important elements.
More Accurate Coding of Diagnosis, Maximum Reimbursement, and Fewer Rejections
The professional coder needs to know about the findings to accurately determine the most applicable diagnosis codes. With a plain text report, the professional coder reads the report looking for hints in its content to help in choosing the right codes. With a structured content, there is no need to parse the report text. Parsing the structure is straightforward and more accurate as a software algorithm can automatically search for nodes that have “findings” name. Because coding is more accurate, reimbursement is maximized and rejections are minimized. An example of prose report is given in Figure 3. A simplified structure that represents the report text is given in Figure 4. The reader can try parsing the text and the structure searching for findings. This example is adapted from DICOM standard, Breast Imaging Report Templates.
Fig 3.
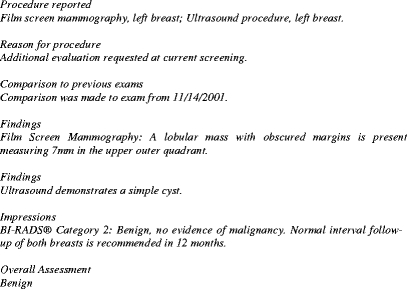
Example of a breast imaging report in prose.
Fig 4.
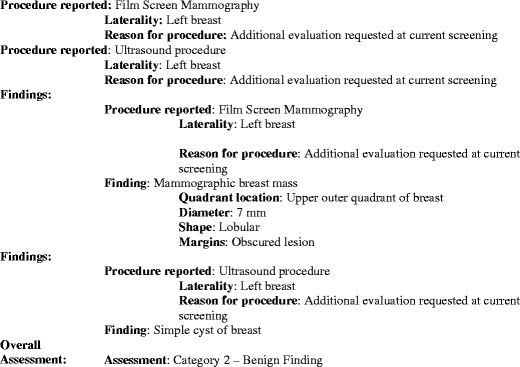
A simple SR structure that encodes the report content of Figure 3. Words in bold represent the content name whereas the content is represented in regular font.
Faster Turnaround
The creation of the radiology report is achieved according to an interpretation process.11 The interpretation process is initiated by the existence of images or other radiology evidences to be interpreted. Typically, the interpretation process is composed of dictation, transcription, and verification steps. The radiology interpretation process is a subprocess of the radiology process, which is a subprocess of an even larger one, the healthcare process. In fact, the radiology process is initiated by a request for a radiology procedure for a specific patient. This is usually part of a radiology order. Hence, the radiology process trigger is a radiology order. The radiology process customer is the recipient of the imaging report. The customer is a healthcare specialist, outside of the radiology department, involved in the patient care. For each requested procedure, there is a radiology process instance that results in an imaging report.
Optimizing the large healthcare process can be achieved by analyzing and optimizing its subprocesses, recursively. Therefore, optimizing the imaging interpretation process contributes to optimizing the radiology process as well as the overall healthcare process.
With a structured input, the interpretation process is faster and results in a faster turnaround that contributes to optimizing the larger processes. In fact, with a structured input, the transcription step can be completely eliminated. Therefore, the radiologist can generate and verify the report in a single step, eliminating all waiting times between steps. In a less optimal situation, where the report cannot be completely generated by the radiologist, as some text needs to be input by a typist, the additional text to input is expected to be small, which in turn reduces the typing time and the error probability, thereby accelerating verification. Moreover, a structured input is expected to be more effective than a speech recognition system, as typographical errors are highly unlikely, resulting in a very effective verification task.
Automatic Coding
As coding can be achieved by parsing the structure, it can be performed automatically. The application can automatically parse the report structure, determine the applicable codes, and present them to the user in the case where many choices are possible and the application cannot decide. Consequently, the overall radiology billing is faster, more effective, and more accurate.
Faster and Less Overtiredness Interpretation
Radiologists usually repeat complete sections by changing few words about the specific findings or do not change anything at all. Some dictation applications provide the user a way to program macros to reduce workload and to save time. In fact, continuously repeating the same sentences induces overtiredness. A structured input application will present the same advantages as a programmed macro or preconfigured templates. They are more effective because they are faster and less tiring for users.
Minimized Typing
When preset structures are used, not only user interaction is minimized but also typing. Thus, typing time is reduced and may be completely eliminated. Moreover, errors are minimized and spelling can be automatically checked by concentrating only on specific sections of text (and leaving out such fields as, e.g., the patient’s name).
Guided Interpretation and for a Complete Examination
The substructure can be constructed on the fly depending on which elements were chosen at the higher level of the report structure. This dynamic structure can be used to guide the interpretation process and prompt the radiologist about the elements to examine, resulting in a complete diagnosis without any missing required examinations. Missing statements in a diagnostic report introduce ambiguities, as the reader cannot determine whether or not the missing element has been examined.
Header Information Consistency
Because the SR shares the same header as the images, the header information is copied from the image by the application that generates the SR. This ensures the correctness and consistency of the patient and study information.
Belongs to the Same Patient Study as the Images
The SR is encoded as a DICOM file. Therefore, it has the same header as the DICOM images that were interpreted to generate it. This practice holds a distinct advantage in that the SR shares the patient name, patient ID, accession number, and other examination IDs with the images. Moreover, it is a separate series within the same study that contains the image series. When the study information is displayed on a picture archiving and communication system (PACS) workstation, the SR will appear as a separate entry along with the images as part of the same study.
Archived, Transferred, and Managed with the Images
The SR can be transferred between various DICOM visualization and archive workstations as the images. Furthermore, it can be stored along with the images. It can be exported on a CD, a DVD, or a long-term archive. It stays with the images within the same study.
No Dictation of Patient’s Name or Accession Number
As the report shares most of its header with the image header, patient name and accession number are copied from the image. Therefore, there is no need to dictate these details (to be typed later), thereby avoiding transcription errors that may result from associating the report with the wrong patient.
References to Images and Presentation States
Images can be referenced inside the document by including their universal unique identifier (UID) in a node. Moreover, semantics associated with the referenced object conveys the purpose of reference. Image frame numbers can also be specified to reference explicit frames within a multiframe image.
Furthermore, a presentation state instance may also be associated with the referenced image to ensure that images are consistently displayed, by providing the geometrical and grayscale contrast transformations to be applied, such as the right orientation, zoom factor, and window settings. For example, the radiologist may point the arrow to a specific feature in an image. This information can be stored in a presentation state. The image, along with its presentation state, may be referenced from within the report content. The rendered report would have the image embedded within its content, and the arrow displayed properly.
References to Regions in an Image
An anatomic or spatial region may be associated with one or more images to denote the epicenter of an anatomic site or lesion or to delineate an open or closed polygon. This is achieved by including information about a region by using basic geometrical shapes, such as a circle or an ellipse, or a set of pixels represented by their spatial coordinates.
Reference to Evidences Used for the Interpretation
The report header includes references to all evidences, such as images, measurements encoded as evidence documents, or presentation states, which are used and interpreted to generate the report content. This gives a persistent link, saved within the report document, between the interpretation result and the information used to generate the interpretation.
References to Prior Images and Reports
Similarly, the report header includes references to prior evidences, such as prior images, prior reports, or prior measurements encoded as evidence documents, which are pertinent and used to generate the report content. This provides another persistent link, within the report document, to all prior evidences that were considered relevant to the current interpretation and result.
References to Previous Versions of the Same Document
In addition to referencing current and prior evidences, the report header includes references to predecessor documents, such as prior or provisional reports, that are deprecated and replaced by the current document. This persistent link allows backtracking to previous versions of the document.
Includes Measurements and Semantics
DICOM SR can include a measurement that consists of a numerical measurement value and a measurement unit. As with other information nodes, a semantic is associated with the measurement to describe it such as a diameter or a length. Furthermore, the measurement can be associated with a specific image by including a relationship, such as inferred from, between the numeric node and the image node.
Coded Semantic
Information lies in the structure nodes. In addition to containing the actual information, each node has a name, described by a code, that defines its meaning. Consequently, a semantic is attached to each element of information. For example, the information element “Diameter: 7 mm” in Figure 4, means that “7 mm” is the measurement of the “diameter,” which is unambiguously specified with a defined code.
Explicit semantic is also associated to the relationship between two nodes, the parent and the child. For example, when a measurement is taken from a specific image, the numeric measurement node can be associated with the image node by mean of an “inferred from” relationship. In this specific example, a measurement bears a persistent relationship to the precise image from which it is estimated.
Automatic Actions
As information is structured and semantic is associated with every node in the structure, it is possible to automatically identify specific types of information, such as identifying the BI-RADS category assessment (see the report example in Figure 4). Moreover, as the vocabulary used to encode the information is constrained by codes, the identified information can be automatically interpreted. As a result, automatic actions can be initiated, such as printing specific lay letters, and ordering or programming specific follow-ups.
Data Mining
Every element of information is described by a code. A code is composed of a code value that can be unambiguously identified and processed by a computer algorithm. This facilitates indexing and enables automatic actions that depend on the report content. Data mining is also enabled by the use of unambiguous codes. Automatic searching for specific diagnosis would be very useful in public surveillance, for instance. The inclusion of the imaging report within the EHR broadens its access. The use of codes makes it useful for secondary uses such as research, statistics, and public surveillance.12
Emphasis on the Content not the Format
DICOM SR does not include any information about how to present, display, or print its content. Presentation of the structured document is left completely to the displaying or printing application. Therefore, the displaying application can apply specific presentation rules to specific type of nodes. For instance, it can display the section header in a specific font (e.g., bold) or in uppercase. It can also underline, for example, the characteristics of a mass. However, this may lead to a lack in the presentation consistency, as the same document can be displayed differently by various applications. Some users can consider this as a limitation. Moreover, typists usually feel insecure when they lose the control of the presentation. They are used to specify the text formatting as they type it. Requiring them to only type the text without any formatting is unusual. Some typists may feel insecure about losing control on the final report layout.
Persistent Printable Format
The lack of presentation consistency of DICOM SR can be worked around with the use of a PDF document that is encapsulated in a DICOM format.13 The report can be made broadly available in a ready-to-display format such as PDF. In fact, the content of a DICOM SR can be easily transformed into a PDF document that can be managed, transferred, and archived with the images after it is encapsulated in a DICOM format. The DICOM file that encapsulates the PDF document shares all DICOM benefits, such as a common framework for persistency management and communication in addition to the wide acceptance of the PDF presentation format. Nevertheless, in order to process the information, PDF is not sufficient and DICOM SR is necessary.
Flexible Formatting of the Radiologist’s Signature
A radiologist may want his or her signature to appear in a specific format such as “Joe Black, MD, Neuroradiologist” (although the radiologist’s signature is not part of the report content). Rendering the radiologist’s signature can be automatically done when drawing up the report content, thus relieving the typist from typing, formatting, or even using a macro to include it every time. In fact, the application managing the report creation has authenticated the user by means of a username and password; therefore, it knows the user’s identity and can automatically include it as the verifying performer. When the report is transformed into a displayable format, the accurate signature can be automatically included.
Stand-Alone Complete Information Object
The imaging report goes through various states before it becomes final. When the report creation is managed by a workflow system, the various statuses are managed by that system. With DICOM SR, these states are saved within the report header, regardless of the information needed by the managing system, resulting in a stand-alone complete information object that is independent of the system that manages or archives it. Moreover, as the status is encoded in the report header, as opposed to the report content, an application can automatically detect such state without any need to parse its content. A preliminary report, for example, can be automatically identified as such by an application.
Fine-Grained Association of Different and Multiple Performers with Various Report Parts
Many persons or computer-aided detection systems may record their input into the report content. Information identifying every performer is encoded with the report. Furthermore, a fine-grained identification of performers can be encoded within the structure. For example, the author of an addendum section can be different from the author of the rest of the report content. The author can be associated with part of the report structure such as a specific section. In Figure 5, the person that recorded the “addendum” section is identified along with the person that verified that same section.
Fig 5.
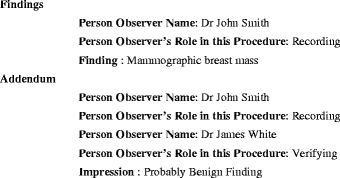
Report structure with different performers associated with different sections.
Recording the performers within the report makes it a consistent and complete piece of information that can be transferred between various systems. As a consequence, the imaging report, an important element of the patient electronic healthcare record, is independent of any proprietary database or system that is used to support its creation. In fact, the various report authors, along with the time and date of their actions, are relevant clinical information included as part of that report content.
Standard Structures or Templates
DICOM has defined various standard structures that are specific to a number of clinical domains. Some of these standard templates define very general structures to encode a complete imaging reports, whereas other define structures to encode evidence document that can be later included as substructures of the final imaging report. The development of such standard structures is continuously evolving. These standard structures include templates for breast imaging, mammography computer-aided detection, chest computer-aided detection, Ob-Gyn ultrasound procedures, catheterization lab, vascular ultrasound procedure, and echocardiography procedure.
Structured and Textual Parts
It is possible to create a DICOM SR with a content that is composed of two major parts: a detailed structure that can be automatically processed by a software application, and a part that can be composed of one or multiple sections of text to be read by a human (Fig. 6). The generation of these two sections can be completely transparent to the user. From the same input information, both parts can be automatically generated.
Fig 6.
Report narrative subtree and a supplementary data subtree.
Automatic Assembly of the Final Report
The final report may be automatically assembled from different inputs. Examples include data from the database (such as the reason for the study), key images with annotations, measurements either calculated by the technologist or by a computer aided detection algorithm. Each part constitutes a subtree of the structure, and an application can construct the final report structure by automatically assembling the subtrees according to preconfigured rules and templates.
Standard Audio Management
DICOM SR has defined a standard way for including audio data within the imaging report. The encoding is very general and can be used to encode any type of waveforms such as audio data or multichannel synchronized electrocardiograms. Waveforms are DICOM objects that can be managed along with images. Consequently, DICOM provides a standard way to archive and transfer audio files along with the images.
Waveforms can be referenced from within a report in the same way an image is referenced. Moreover, temporal coordinates may be used to delineate a temporal region of interest in one or more waveforms. Temporal coordinates can be used with timely related images; they may refer to multiple images and a synchronously acquired waveform to indicate a temporal region on images and waveform.
Integration with Speech Recognition
The creation of a structured report can be integrated with a speech recognition engine or can be implemented with the help of a pointing device to select items from menus and submenus. Speech recognition can be used to input free text information element. Additionally, it can be used to select one option from multiple possible choices.
Relation to other Document Formats
DICOM SR can be very easily transformed into any other document format.3 In fact, as every node of its structure has a precise type, specific transformations can be applied on each node type to generate new encoding of the information contained in that node. Structure transformations are widely used in practice. In fact, the eXtensible Markup Language (XML) is universally used nowadays to encode any type of information as a structured document. An XML document is commonly transformed with widely available transformation engines that represent transformations with Style Sheets. The transformed document can have a different structure such as the HL7 Clinical Document Architecture (CDA). Conversely, it can be encoded without any structure such as a plain text document. DICOM SR may need to be transformed into CDA, HL7 message, plain text, and PDF to make it broadly available as an important element of the patient electronic health record. When transformed, references to images, reports, and other evidence can be preserved. However, rendering applications would not necessary to display them appropriately unless they have some DICOM capabilities, except for PDF files where images can be embedded directly into the document.
Structured Report and Integrating Healthcare Enterprise
SR is essential for many Integrating the Healthcare Enterprise (IHE) integration profiles. IHE is an initiative jointly sponsored by the Radiological Society of North America (RSNA) and the Healthcare Information and Management Systems Society (HIMSS) to stimulate the integration of healthcare information resources. IHE has defined many integration profiles that specify how to implement integration capabilities between different equipment from different vendors (Noumeir, unpublished data).14,15
The Simple Image and Numeric Report Integration Profile (SINR) defines actors for the creation, management, storage, and viewing of DICOM SR in addition to defining transactions to exchange these reports between actors. This IHE profile uses DICOM query/retrieve and store to transfer reports between systems. It also defines two simple templates to encode simple and numerical reports. Furthermore, transforming DICOM SR into an HL7 message is also defined.
The Reporting Workflow (RWF) Profile addresses the need to schedule, distribute, and track the status of the reporting workflow tasks such as interpretation, transcription, and verification. Worklists for each of these tasks are generated and can be queried; workitems can be selected and the resulting status returned from the system performing the work to the system managing the work. The information object that is created and managed while performing the work is a DICOM SR. It is the result of the reporting process.11 The workflow is managed between various systems by using DICOM General Purpose Worklist and General Purpose Performed Procedure Step.
The Evidence Documents Profile defines interoperable ways for observations, measurements, results, and other procedure details recorded in the course of carrying out a procedure step to be output by devices, such as acquisition systems and other workstations. Evidence documents can be stored and managed by archival systems and can be retrieved and presented by display and reporting workstations. This allows measurements or CAD results to be made available as input to the process of generating a diagnostic report or, in some cases, to be included in the diagnostic report. Evidence Documents are encoded as SR. When included in the final report, an Evidence Document is a subtree of the report structure.
The Key Image Note (KIN) Integration Profile specifies transactions that allow a user to mark one or more images in a study as significant by attaching to them a note. The note structure is similar to the SR structure. It includes a title stating the purpose of marking the images and a user comment field. KIN can be automatically included in or attached to the final diagnostic report. In fact, the radiologist can choose a specific title for the note such as “For Report Attachment,” in which case the reporting system can automatically include the images referenced in the KIN as image references in the final SR.
The Access to Radiology Information (ARI) Integration Profile specifies a number of query transactions providing access to radiology information, including images and related reports, in a DICOM format.
The Patient Information Reconciliation (PIR) Integration Profile defines methods to match images, diagnostic reports, and other evidence objects acquired for a misidentified or unidentified patient (e.g., during a trauma case) with the patient’s record. Thus SR header is automatically reconciled with the correct patient and order information, when the patient’s official registration and order information is entered into the Registration and Order Placer Systems.
Conclusion
Despite the numerous advantages of a structured report and the fact that it offers various secondary uses when included in the Electronic Healthcare Record, structured reporting has not yet gained a wide adoption because it induces a major change affecting the way the diagnostic interpretation is recorded. Many individuals or computer algorithms have inputs that contribute to the final report. The radiologist’s findings and impressions constitute a major part of the imaging report content. The imaging report may also contain information entered by other contributors, such as measurements taken by a technologist or a computer algorithm.
To construct a structured content, its various parts need to be structured. The output of a computer algorithm can be expected to be structured. However, structuring the radiologist’s report content is not straightforward. Traditionally, the radiologist’s dictated content is transcribed by a typist, who transforms the audio data into a document. Entering a structure by the typist is not very practical as only a primitive structure, limited to section headings and bodies, is achievable. Therefore, in order for the radiologist’s interpretation to be structurally encoded, the structure needs to be entered, at the interpretation step, by the radiologist. This introduces a major change in the radiologist’s interpretation process.
Although this major change is limiting the wide adoption of structured reports, many radiologists and typist have programmed text editor macros to gain advantage of predefined sections that are repeated. Predefined text is a primitive and limited structured form that may contribute to a rapid turnaround. Complete financial advantages, better service to referring physicians, better patient care, and better radiologist quality of life are only enabled by a structured report.
To implement a structured interpretation, a knowledge base is needed to limit the possible structures that are associated with each imaging procedure. As a consequence, structure encoding can be seen as a guided interpretation process where subsequent possible choices, at a certain moment during the interpretation, depend on the structure encoded so far. Moreover, the final structured report can be composed of two parts, which encode the same information: a part, intended to be read by humans, that can be encoded in a prose style, and a computer readable part that is encoded with an elaborate structure and codes. A visualization application can thus display the writing style text, whereas a computer algorithm can process the structured content. Many DICOM templates allow for such combined encoding. Evidently, the input can be structured and concise, allowing for the automatic construction of the prose and the detailed structure. This knowledge base can also help constrain the result of natural language processing when used to structure narrative reports.
Traditionally, images are managed by PACS and reports are managed by Radiology Information System (RIS). But as the interpretation process involves interacting with images and reports, this raises an integration issue that is discussed and detailed in.11 With structured reporting, particularly when references to images are encoded or measurements are calculated from image features, the integration between the display workstation and the report creation system is even more tied than ever. The user may draw a line on the image and may encode its length as a distance or a diameter, for example. Therefore, a convergence between the visualization workstation and the report creation workstation may result in a single next-generation radiologist workstation that allows the fulfillment of all the radiologist’s tasks.
Nowadays, speech recognition is used to automatically transcribe the report content that is dictated by the radiologist into a document. Speech recognition enables a rapid turnaround and an effective process, as it reduces the transcription time or completely eliminates the transcription step. Even though speech recognition algorithms have been greatly improved in the last decade, errors are still very frequent and correcting them is a tedious and an ineffective task. Structured input offers the same advantages as speech recognition. It eliminates the transcription step, thereby enabling a rapid turnaround and an effective process. Moreover, structured input does not suffer from the problems of speech recognition and offers yet more benefits such as automatic and more accurate diagnosis coding resulting in maximum reimbursement and fewer rejections; it also allows for coded semantics, and less overtiredness interpretation. In fact, using a pointing device to choose one option from multiple possible programmed alternatives is less tiresome than repeatedly reciting the same text. Furthermore, it provides a guided interpretation for a thorough examination.
However, to fully benefit form structured reporting, changes in the interpretation process are required. The radiologist needs to input the structure with a pointing device to select from predefined options instead of dictating, in a prose or coded style, the report content as an audio media. Evidently, voice can be used as a pointing device, in which case the recognition rate would be very high, as the vocabulary would be extremely constrained.
We believe our article will help overcome the challenges required by the structured imaging interpretation. By recognizing all the benefits of a structured report, the end user becomes aware of the great enhancement in patient care and the improvements to the imaging process efficiency and effectiveness that it provides.
Acknowledgment
This work was supported by the Natural Sciences and Engineering Research Council of Canada.
Biography
Rita Noumeir is a professor at the Department of Electrical Engineering of the University of Quebec, École de Technologie Superieure in Montreal. A founding member of the Imaging, Vision, and Artificial Intelligence Laboratory (LIVIA), her main research interest is the Healthcare Information Technology, specifically, Interoperability, Electronic Patient Record, Security, Information Confidentiality, and Image Processing.As a member of both Technical and Planning International IHE Radiology Committees, Dr. Noumeir took part over the last 5 years in developing many Integrating the Healthcare Enterprise (IHE) Integration Profiles in Radiology and in organizing several Integration Demonstrations. She is a cofounder of IHE Canada.Dr. Noumeir contributed to many research and development projects in collaboration with several Canadian and international companies in medical imaging and healthcare information. Currently, she collaborates with the Diagnostic Imaging Team of Canada Health Infoway to define the principles and architecture for sharing imaging information between multiple healthcare institutions. She plays a leading role in the development of this solution that is published as an IHE Integration Profile for which she is the editor.Rita Noumeir holds a Ph.D. and a Masters degree in Biomedical Engineering from École Polytechnique of Montreal specializing in Medical Imaging. She is a professional engineer, and a member of the Ordre des ingénieurs du Québec.
References
- 1.Ratib O, Swiernik M, McCoy JM. From PACS to integrated EMR. Comput Med Imaging Graph. 2003;27(2–3):207–215. doi: 10.1016/S0895-6111(02)00075-7. [DOI] [PubMed] [Google Scholar]
- 2.Pommerening k, Reng M. Secondary use of the electronic health record via pseudonymisation. In: Bos L, Laxminarayan S, Marsh A, editors. Medical Care Compunetics 1. Amsterdam: IOS Press; 2004. pp. 441–446. [Google Scholar]
- 3.Noumeir R: Reporting workflow modeling, progress in biomedical optics and imaging. Medical Imaging 2004-PACS and Imaging Informatics 5(25):8–15, 2004
- 4.Noumeir R. DICOM structured report document type definition. IEEE Trans Inf Technol Biomed. 2003;7(4):318–328. doi: 10.1109/TITB.2003.821334. [DOI] [PubMed] [Google Scholar]
- 5.Clunie DA. DICOM structured reporting: An object model as an implementation boundary. Proc SPIE Int Soc Opt Eng. 2001;4323:207–215. [Google Scholar]
- 6.Noumeir R. Multimedia medical diagnostic document. Proc IEEE Int Conf Multimedia Expo. 2002;2:325–328. [Google Scholar]
- 7.Clunie DA: DICOM Structured Reporting. PixelMed Publishing, 2002
- 8.Hripcsak G, Austin JHM, Philip O, Alderson PO, Friedman C. Use of natural language processing to translate clinical information from a database of 889,921 chest radiographic reports. Radiology. 2002;224:157–163. doi: 10.1148/radiol.2241011118. [DOI] [PubMed] [Google Scholar]
- 9.Langlotz CP. Automatic structuring of radiology reports: Harbinger of a second information revolution in radiology. Radiology. 2002;224:5–7. doi: 10.1148/radiol.2241020415. [DOI] [PubMed] [Google Scholar]
- 10.Naik SS, Hanbidge A, Wilson SR. Radiology reports: Examining radiologist and clinician preferences regarding style and content. AJR. 2001;176:591–598. doi: 10.2214/ajr.176.3.1760591. [DOI] [PubMed] [Google Scholar]
- 11.Noumeir J Biomed Inf. 2;39:103. doi: 10.1016/j.jbi.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Noumeir R, Lemay A, Lina JM: Pseudonymisation of radiology data for research purposes. J Digit Imaging (in press) [DOI] [PMC free article] [PubMed]
- 13.Supplement 104: DICOM Encapsulation of PDF Documents, Digital Imaging and Communications in Medicine (DICOM), March 2005
- 14.IHE Technical Framework, www.ihe.net
- 15.Carr CD, Moore SM. IHE: A model for driving adoption of standards. Comput Med Imaging Graph. 2003;27(2–3):137–146. doi: 10.1016/S0895-6111(02)00087-3. [DOI] [PubMed] [Google Scholar]


