Abstract
Since the introduction of Picture Archiving and Communications Systems (PACS) into the medical radiology community, the efficiency and workflow of radiology departments adopting this technology has been improved to a degree much greater than initially anticipated. Although technological advances fuel efficiency and improve workflow, medical mistakes become prevalent as a result. This observation underscores the need for active measures by PACS quality assurance personnel to prevent human and machine errors from contributing to the total of avoidable medical errors, particularly in the area of diagnostic imaging.
Key Words: Data mining, databases, PACS, quality assurance
Background
Since the introduction of Picture Archiving and Communications Systems (PACS) into the medical radiology community, the efficiency and workflow of radiology departments adopting this technology has been improved to a degree much greater than initially anticipated. Diagnostic images are easily viewed day in and day out using high-quality LCD monitors; worklist management tools enable radiologists, clinicians, and technologists to select and display exams in the blink of an eye; and in many reading rooms, exams are being interpreted within minutes of image acquisition.
According to the Institute of Medicine, a component of the National Academies of Sciences, as many as 98,000 people die each year in the United States from medical errors,1 e.g., errors occurring from patient identity mix-ups, imaging errors, poor writing on patient orders, etc. This observation underscores the need for active measures by PACS quality assurance (QA) personnel to prevent human and machine errors from contributing to the total of avoidable medical errors, particularly in the area of diagnostic imaging.
The University of Texas M.D. Anderson Cancer Center in Houston, Texas, is using information technology to address identification, correction, and documentation of PACS errors. A multifunctional tool developed by the Department of Imaging Physics, called a PACS change request form (PCRF), enables technologists and radiologists to report any and all errors within diagnostic imaging.2 When PACS first arrived at M.D. Anderson, there was no way of knowing when there was a potential patient misidentification. Other than a radiologist accidentally discovering a patient misidentification error while trying to interpret an exam or a phone call from a technologist, there was no standardized, reliable method for identifying when the occasional machine or human error occurred. Thus, the need to deal with these problems became more pronounced as PACS implementation grew.
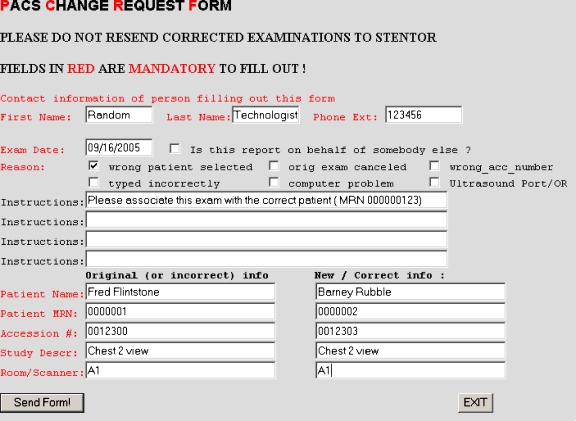
The PCRF is an electronic form that technologists submit to notify the PACS Technical Analyst team of a potential problem with a patient’s examination. This is accomplished through The Division of Diagnostic Imaging intranet home page, where the electronic PCRF can be found. This form allows for the technologists to describe in detail what corrective action is needed. Figure 1 illustrates a properly filled out PCRF form. The PCRF is submitted electronically in nonpublic areas, such as technical corridors, stored in a MySQL®3 database, and distributed among the PACS Technical Analyst team via e-mail in their private offices, and an alphanumeric page. PACS Analysts receive an e-mail with the pertinent data and a beep alert, containing the reference number and type of PCRF, to alert the analysts that a new PCRF is pending. All of the information provided on the form is cross-referenced for patient demographic verification through the Radiology Information System (RIS).
Fig 1.
PCRF as used by the person reporting a problem.
In late 2001/early 2002, we implemented a paper form with the required specifics to resolve incorrect examination and demographic information that included the original exam/patient demographics, i.e., wrong patient information, and also the correct exam/patient demographics. This form provided us with the necessary documentation required to prevent a patient mishap. The paper PCRF was available in all of the imaging departments and was to be faxed in to the PACS Technical Analyst team. Prior to the electronic PCRF, the assumption was made that the patient information provided was accurate. Utilization of the RIS was still an additional verification method; however, if the patient information provided did not appear correct or correlate with the RIS information, the reconciliation process was further delayed by having to contact the technologist to have them reverify and resubmit the information.
By means of some creative programming, the automated PCRF tool was developed utilizing PERL, CGI, UNIX, MySQL®, and mailx, which are available via the Internet. By storing PCRF data in the MySQL® database, information is available for mining with Crystal Reports®4 or other database mining tools to provide supervisors and managers with productivity reports and QA reports.
The PCRF tool can also be reconfigured through manipulation of the program code to accommodate amending of database fields and the addition or removal of any particular field. This can be accomplished in a day’s work without the need to rewrite the entire code for the tool or disrupting the usage of this tool by eliminating the need to take it offline for hours at a time.
Evaluation
Every patient exam carries an associated set of exam and demographic information that is critical at every step of treatment and therefore needs to be available in flawless form. For example, medical record number (MRN) and accession number are a couple of the critical elements that are required in precise form. Studies that require reconciliation as a result of being “broken” or “orphaned” are typically studies that are missing the accession number as an outcome of a system/modality failure, RIS interface down time, or computer errors. Even sophisticated modality worklist management implementation does not preclude the possibility of human error, e.g., picklist problem (i.e., wrong patient, wrong study, and worklist provider outage).5 Thus, a method must be in place to reconcile patient exam data quickly and efficiently. For this to occur, the following elements from Table 1 need to be in place.
Table 1.
Elements required to create a procedure for patient reconciliation
| ▪ A reporting mechanism |
| ▪ Personnel willing to report their own mistakes |
| ▪ Analysts with tools and experience to repair patient exam data |
| ▪ Data mining tools to gather data as feedback for supervisors and technologists |
Reporting Mechanism
To reconcile exams, a reliable and efficient mechanism is required. The PCRF tool provides this mechanism through a multifunctional automated system that enables technologists and radiologists to quickly and efficiently report patient exam errors. By accessing an online form, the end user is able to fill in the required patient information, such as medical record number, patient name, and instructions for what they are requesting.
Personnel Responsibility
Usage of the PCRF tool depends on the integrity of the end user. Without the acknowledgment of the technical staff to an error, the PCRF tool and the mechanisms in place are ineffective.
Experienced Analysts
Experienced analysts serve as the approved personnel to handle the reconciliation of exams that are submitted via the PCRF tool. Analysts at M.D. Anderson are promoted from within the radiological staff and have met the necessary criteria for the job, are registered radiologic technologists, and provide a wide range of modality and protocol experience.
Data Mining
PACS change request form data are stored in a MySQL® database where the information is readily available for mining with database mining tools. Crystal Reports® is our tool of choice for providing supervisors and managers with productivity reports and QA reports. The PCRF data are stored through a variety of categories that pertain to the specific PCRF requests and can even be further analyzed down to event specifics.
Discussion
To implement our patient exam data reconciliation tool, we selected to use a Sparc Ultra 1 running the Solaris 5.8 UNIX operating system. However, any fast PC with the Linux operating system will suffice. All programming and scripting is performed in PERL (practical extraction and report language) and CGI (common gateway interface). PERL code was favored for ease of programming and the benefit of being extensible with a multitude of modules for special purposes such as the CGI module. We use the Apache HTTP Server6 to facilitate a user interface. The Apache HTTP Server is a project of the Apache Software Foundation7 and is commonly used as a reliable HTTP server. We use MySQL® as our database of choice because it is cost-effective (free in most cases) and easy to integrate into an existing UNIX/LINUX environment. The servers and clients used to run this operation are connected to a private subnet that is protected by multiple firewalls and require client log in.
A typical reconciliation effort begins with a technologist recognizing and admitting to a mistake. The technologist or supervisor initiates and completes a reconciliation form, or PCRF, online that includes all of the necessary data to reconcile the exam. A few of the required elements necessary for reconciliation are listed in Table 2.
Table 2.
Elements required to reconcile patient information
| ▪ Patient name |
| ▪ Medical record number |
| ▪ Accession number |
| ▪ Modality and location |
| ▪ Exam/study description |
| ▪ Technologist name and contact number |
Patient Name
For accurate patient identification, the patient name field is designated as a required field that must be accurately filled in. Through the tools programming, the patient name is accurately cross-referenced and identified through the RIS.
Medical Record Number
The medical record number is perhaps the most important factor in patient identification. This field in the PCRF is also required and like the patient name, it is also cross-referenced and accurately identified through the RIS.
Accession Number
Accession numbers are sequentially assigned by the RIS and are associated with each individual patient exam. This is also a required field that is cross-referenced through the RIS for proper exam/patient identification.
Modality and Location
The modality from where the exam and request are originating is important for the exam demographic editing. In the event that an exam is acquired with an incorrect exam description, the PACS analysts must be able to reference the correct modality and exam description from the RIS to edit exams accordingly. The exam location is also equally important in the event of equipment malfunctions. By having the location, we are able to obtain valuable information such as the device IP address in the event that necessary maintenance is required.
Exam/Study Description
The original or incorrect exam/study description is required once again for the purpose of editing the exam. The incorrect description is referenced with the RIS data provided for that patient/exam combination as well as the accession number to ensure that all edits occur accordingly.
Technologist Name and Contact Number
The contact information for the technologist or radiologist originating the request is also an important piece of information. In the event that there are discrepancies within a request, missing information, or instructions that are not clear, it is important to be able to contact the PCRF originator so that all of the correct and appropriate actions are taken on a request.
All of the preceding information is given both for the original flawed exam data as well as the intended and correct version.
The data are stored in a MySQL® database upon receipt. Next, an e-mail to the analysts is generated as well as a beeper alert. In the background, data such as accession number and medical record number are compared with the RIS database to obtain further patient/exam information.
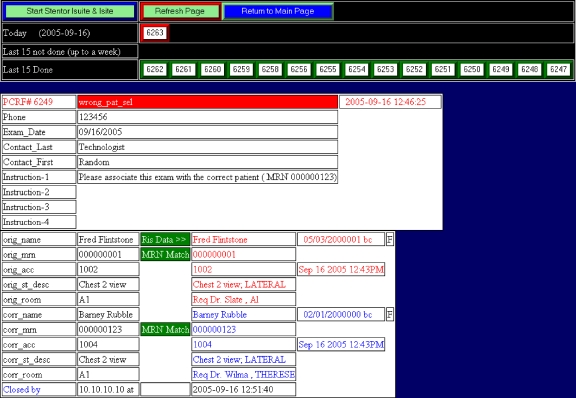
The analyst responding to the alert accesses a Web page from any secure area within the enterprise and upon clicking a button with the particular PCRF number, receives all of the data needed to reconcile the patient exam. Figure 2 illustrates the PCRF request that is seen by the PACS analyst responding to the alert.
Fig 2.
PCRF as seen by the PACS analyst.
Because the PCRF tool is not part of a Vendor PACS nor does it reside in one, porting is unnecessary. The key elements required for reconciliation (MRN, accession number, and patient name) remain constant and do not change from PACS system to PACS system; thus, the tool depends solely on its own Unix/Linux server and the already deployed infrastructure, such as Web-browser-enabled client work stations, of the institution. However, if additional data, such as accession numbers or dictation status, for example, is required from the RIS for cross-referencing the data submitted via the PCRF, then adjustments to the appropriate section of the program that interfaces with the database are required. This can also be accomplished by mining the data from a PACS systems database. The deciding factor as to which method is most efficient lies mainly upon the ease at which of the databases it is easier to interface with.
Conclusion
Using the patient exam data reconciliation tool is a convenient way of automating exam data repair requests. By providing a multifunctional approach through an electronic form, the PCRF tool not only notifies the PACS technical analyst team of a potential problem with a patient’s examination but also allows for the technologists to describe in detail what corrective action is needed. The automated reporting system is more convenient, provides an audit trail, and is available faster than by fax. As an added benefit, the audit trail exists to capture the event and relevant time stamps that provide and enable documentation. Thus, we are able to prove who directed the change, why the change was required, and when it was carried out, and, in doing so, further capitalize upon the tool’s storage and database capabilities. This system places the responsibility for verification of patient demographic and exam information squarely on the shoulders of the technologist performing the exam, and isolates them from being able to correct their errors in anonymity. Radiologists and medical physicists are the secondary method by which errors can be reported should the responsible technologist fail to capture the error. The PACS analysts correct errors only at the direction of the technologists, radiologists, and medical physicists, rather than correcting as they see fit.
Acknowledgments
We would like to thank Charles Willis, PhD, Stephen K. Thompson, MS, and Jeff Shepard, MS, for their invaluable support and contributions toward this project.
References
- 1.Institute of Medicine. Retrieved September 16, 2005 from the World Wide Web at http://www.iom.edu/, 2005
- 2.BNBFORM. All-In-One Form Processing Script. Retrieved June 2003 from the World Wide Web at http://www.bignosebird.com/cgi.shtml
- 3.MySQL. Retrieved July 2004 from the World Wide Web at http://www.MySQL.com
- 4.Crystal Reports® by Business Objects. Retrieved from the World Wide Web at http://www.businessobjects.com/products/reporting/crystalreports/default.asp
- 5.Kuzmak PM, Dayhoff RE. Minimizing digital imaging and communications in medicine (DICOM) modality worklist patient/study selection errors. . J Digit Imaging. June 2001;142(2 Suppl 1):153–157. doi: 10.1007/BF03190323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Apache HTTP Server Project. Retrieved September 2003 from the World Wide Web at http://httpd.apache.org
- 7.The Apache Software Foundation. Retrieved September 2003 from the World Wide Web at http://www.apache.org