Abstract
A traditional radiological workflow is compared with one based on radiology information system/picture archiving and communication system (RIS/PACS). X-ray workflow process was considered in both radiology departments. First, the study identified the main phases of the research work as follows: Process Analysis, Data Collection and Elaboration, Interpretation. Afterwards, the main steps of the whole image acquisition process were defined, and each step was divided into a number of elementary operations. Then, the time required to complete each of these was measured. Data collected were elaborated and synthesized to obtain time frequency distributions for each step and evaluation of the total time for the whole working flow. Statistical elaboration of the collected data shows that x-ray working time decreases, between 35% and 57%, when RIS/PACS is used. Detailed analysis of the whole working process allows identification of possible critical points to improve the image acquisition process.
Key Words: X-rays, workflow, RIS/PACS
Background
In the past 15 years, there has been a growing number of faster processes to substitute traditional x-ray systems with computer-assisted ones, both for image acquisition and process management. A considerable impact is found both on productivity and management of the workflow process, especially in Diagnostic Imaging departments. A remarkable advantage of radiology information system (RIS) and picture archiving and communication system (PACS), which allow the integration of filmless and paperless operations, is speech recognition integration. As will be discussed below, this feature allows a faster reporting procedure. A difficult point, however, lies in providing a quantitative evaluation of the possible benefit of their use. We define a radiological workflow as the procedure of analyzing individual steps necessary to carry out the whole process in a Radiology department. This workflow has been strongly affected by new technologies such as RIS, PACS, speech recognition, electronic signature, and digital modality (e.g., computed radiography [CR] and direct radiography [DR]); in fact, some steps in the traditional workflow are shortened or even eliminated. For example, it was demonstrated that, after reengineering workflow and integrating information systems, the process was reduced from 59 major steps to only 9 for an inpatient chest radiograph.1,2
In particular, some technologist responsibilities, such as data access, image acquisition, and repeat of lost examinations, are the areas most affected by the transition to filmless imaging in the execution of radiographic examinations.1 Moreover, speech recognition and electronic signature accelerates the process of report production, eliminating interactions between the radiologist and the secretary, before report is finalized.3,4 It was proved that time of report generation (Report Turnaround Time), measured from the end of the examination up to the time when film and report are available for delivery, is largely reduced.3–5 Speech recognition influences time between report dictation and report transcription. In a particular study, the mean turnaround time declined from 87.8 to 32.3 h and the 24-h report availability is 71.1%.4
Another study showed a time saving from 8% to 25% in report turnaround.2 In a study about chest radiographs, it was demonstrated that the median time from transcription to final signature decreased from 10 to 5 days with the introduction of electronic signature.3
Moreover, studies 6,7 were performed on several execution times, such as patient throughput time and technologist examination time. Patient throughput time is the period that the patient spends in the modality room. In a study,6 it was measured as the time a patient entered the chest procedure room subtracted from the time that patient exited the room. In this case, it was deduced that the average number of patients entering and leaving the Radiology Department per hour (patient throughput) increased from 8.2 for screen film (analog) to 9.2 and 10.7 for CR and DR, respectively. The technologist examination time7 was measured as the time from patient arrival in the examination room to the time completed images were ready for radiologist interpretation. It was computed for two types of radiographic exams: chest and orthopedic examinations of the spine in Fort Howard and Philadelphia Veterans Affairs Medical Center with film-based operation and in Baltimore Veterans Affairs Medical Center with filmless operation. The result of this study is that the mean time decreased from 14.0 to 7.4 m for chest, and from 20.8 to 8.8 for spine.7
In this article, we present results on the measured time for the whole radiological process (Process Time). It is defined as the interval running from patient arrival at the Front Office of the Radiology Department (for registration) to report delivery. The times were acquired to compare a traditional radiological workflow with one based on a RIS/PACS system. The analysis is made by comparing management methodologies and computing the average time of each step, after the definition of the main steps for both working flows. The total mean time is then computed.
It is clear that many times can be defined and measured, according to different points of view, such as those of patients or technologists. In our case, the measured time was from standpoint of Radiology Department internal actors: Front Office operators, technologists, radiologists and typists. With this choice, the waiting time of patients before examination was not considered, like all the other dead times within the whole process.
For data acquisition, we measured time by using a stopwatch, similar to what was done in the study carried out at Fort Howard, Philadelphia Veterans Affairs Medical Centers, and Baltimore Veterans Affairs Medical Center.7 This is in contrast to other studies, where time was calculated by using data files of RIS database.3,4
Methods
Details
Data were collected from September 2004 to January 2005 in the Radiology Department of Macerata Hospital, which was equipped with AGFA PACS IMPAX and AGFA RIS Elefante systems, and at Jesi Hospital, where a traditional imaging system is still being followed. The ethics committee of ASUR-Marche Z.T. 9 examined, before commencement of the study, the research proposal and the actual activity plan.
In Jesi Hospital, the working flow is automatic only for booking of examinations and patient registration, whereas the other steps of the process are completely manual and film-based. In Macerata Hospital, the RIS/PACS system has been in place since January 2004, with a complete transition to automatic and paperless operations. In particular, the speech recognition reporting system was implemented in RIS, integrated in a PACS system.
These two structures were selected because of their similarities in terms of yearly number of examinations, and type and number of injuries.
Data were acquired for outpatients whose ailments were not considered urgent, referred to the hospital by “outside” physicians (e.g., family doctor). Moreover, only x-ray examinations without contrast were considered—being the relevant percentage of radiological activity in both hospitals.
The study identified the main phases of the research work: Process Analysis, Data Collection and Elaboration, Interpretation. Next, the main steps of the whole image acquisition process were defined and each step was divided into a number of elementary operations. Thus, the rough data represent times required for each elementary operation.
No selection criteria were used to define the sample for data acquisition. This means that data were collected in days, randomly chosen for both hospitals. The total number of data is about 2,000, distributed between the two radiology departments.
Analysis of the Whole Image Acquisition Procedure: Process Analysis
The radiological workflow starts with examination booking, but our data collection started with patient registration, which marks the time when the patient approaches the Admittance Front Office. The whole process ends when the report is in the hands of the patient.
Workflow phases are identified both in digital and traditional cases, as shown in Figures 1 and 2.
Fig 1.
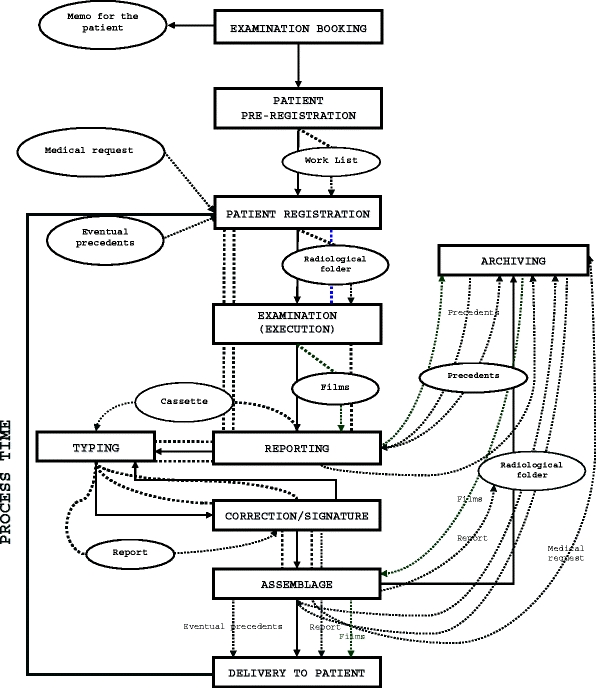
Traditional radiological workflow for an x-ray examination without contrast in the case of a nonurgent outpatient. In particular, rectangles represent the process steps, ovals describe paper documents transiting from a step to another, and dotted lines evidence paper and film movements.
Fig 2.
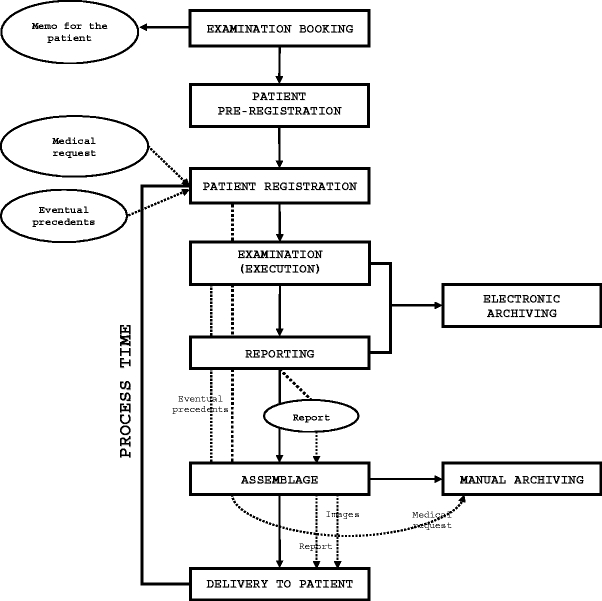
Digital radiological workflow for an x-ray examination without contrast in the case of a nonurgent outpatient. Rectangles, ovals, and dotted lines have the same meaning as in Figure 1. Note that the number of ovals and of dotted lines is greatly lower, because the process is automatic without paper and film movements.
In essence, the difference between the two processes lies in two steps: Report Typing and Signature/Correction, which are only present in the traditional workflow (Figs. 1 and 2). However, another important point is the difference in generation and management of the worklist. In fact, in a traditional system the worklist is manually moved (dotted lines in Fig. 1) from one step to another. In contrast, in a RIS/PACS system the technologists work and the accuracy of the work is improved by DICOM (digital imaging and communication in medicine) modality worklist, this being directly open to operators.
Next, each step was divided into several elementary operations (Table 1).
Table 1.
Elementary operations for each step of a traditional workflow and a digital one
| Traditional workflow steps | Digital workflow steps | |
|---|---|---|
| Registration | Front Office Operations | Front Office Operations |
| Patient Registration | Patient Registration | |
| Back Office Operations | ||
| Radiological folder preparation/eventual retrieval from archives | ||
| Delivery to suitable diagnostic | ||
| Execution | Patient/examination preparation | Patient/examination preparation |
| Performing x-ray examination | Performing x-ray examination | |
| Patient/examination data association | Patient/examination data association | |
| Films development | Image postprocessing | |
| Radiologist consultation | Radiologist consultation | |
| Eventual repetition | Eventual repetition | |
| Radiological folder and films assemblage | ||
| Delivery to radiologist | ||
| Reporting | Reporting | Reporting |
| Data and images analysis | Data and images analysis | |
| Precedents retrieval and analysis | Precedents retrieval and analysis | |
| Eventual consultation | Eventual consultation | |
| Eventual interruption | Eventual interruption | |
| Dictation of the report | Report drawing up | |
| Cassette and papers delivery to typist | Report reading | |
| Typing | Report Correction | |
| Report copying | Report printing | |
| Report printing | Report signature | |
| Report preparation for the signature | ||
| Report delivery to radiologist | ||
| Correction/Signature | ||
| Report reading | ||
| Report Correction | ||
| Report signature | ||
| Radiological folder and report delivery for the assemblage | ||
| Assemblage | Report two copies separation | Images printing |
| Report insertion in the envelope | Envelope preparation | |
| Films retrieval in archives | Images and report insertion in the envelope | |
| Delivery of the exam to Radiology Front Office | Delivery of the exam to Radiology Front Office | |
| Delivery | Delivery to patient | Delivery to patient |
In this table, Typing and Correction/Signature steps of the traditional process were unified under Reporting for a better comparison with the structure of its digital counterpart. In fact, a RIS/PACS system allows the radiologist to manage Reporting as a whole, with Typing and Correction/Signature, too.
This analysis allows the user to define the process total time, which starts from Patient Registration and ends with Report Delivery.
Data Collection and Elaboration
The time data for both departments were measured by using a manual stopwatch (Table 1), in which we directly measured the net time needed to complete each elementary operation. We did not use the process data stored in the RIS database. Examination and comparison of these data (from RIS database vs our data) are discussed below. At least 100 values were collected for each operation. Raw data were examined to remove possible errors due to observer bias (e.g., data transcription, approximation, and calculation) before they were included (Table 2), thereby giving the total time of each step, as the sum of the net time needed to complete each operation. We excluded “dead time” between operations; similarly, the total processing time was computed without considering dead time among different steps.
Table 2.
Scheme according to which raw data were collected
| Patient Progressive Number | |||
| Patient Type | |||
| Study Type | |||
| Patient/Examination Preparation Time | |||
| Performing X-ray Examination Time | |||
| Postprocessing Time | |||
| Patient/Examination data Association and Films Development Time | |||
| Radiologist Consultation Time | |||
| Eventual Repetition Time | |||
| Total Execution Time |
In particular, this example refers to data collected during the execution step of a traditional workflow.
Next, the data were statistically elaborated to obtain the mean, standard deviation and error, and variation coefficient.
Results
Traditional Workflow
Table 3 presents the mean time of each step with its standard error. The total time of the whole process is computed as the sum of mean times of all steps. The error on total time was computed by using the relation for error propagation when quantities are not homogeneous. This time elaboration was performed for three different cases: ST, A, and B (Table 3).
Table 3.
Mean time computed for each step of a traditional workflow with its standard error
| Traditional workflow | |||
|---|---|---|---|
| Case | ST | A | B |
| Incidence | 0.7% | 6.9% | |
| Patient registration time | 1 min 58 s (±6 s) | ||
| Execution time | 9 min 59 s (±27 s) | ||
| Reporting time | 1 min 38 s (±16 s) | ||
| Typing time | 1 min 35 s (±4 s) | 1 min 35 s (±4 s) | |
| Correction/Signature time | 11 min (±1 s) | 11 min (±1 s) | |
| Assemblage time | 1 min 21 s (±4 s) | 4 min 5 s (±42 s) | |
| Delivery time | 1 min 45 s (±18 s) | 1 min 45 s (±18 s) | |
| Operator’s time | 10 min 59 s (±1 min 52 s) | 2 min 55 s (±30 s) | 4 min 12 s (±43 s) |
| Total time | 29 min 26 s (±1 min 58 s) | 29 min 26 s (±1 min 58 s) | 29 min 26 s (±1 min 58 s) |
| Total time | 34 min 7 s (±2 min 2 s) | 39 min 28 s (±2 min 14 s) | |
The computed mean time for cases A and B are also illustrated (see text).
ST = standard case: workflow without mistakes and/or problems; A = case A: report with errors that must be typed again; B = case B: report not available at the delivery to be assembled.
ST means that the whole process run regularly, i.e., without any mistake or need for correction. Case A considers reports containing mistakes identified at the moment of signature, which must be typed a second time and sent again for signature.
Situation B occurs when a report is not available for delivery and searches for other reports and/or films needing to successfully complete the process.
Digital Workflow
The total time of the whole process is computed in the same way as the traditional one—as sum of a simple step and operator mean time. Table 4 shows these mean times and their standard errors. The error on total time is statistically computed as in the traditional workflow. The times of the steps were elaborated only for the standard (ST) case. In fact, it is extremely difficult for situations A and B in the traditional workflow to occur in the digital version, because errors are corrected in real time.
Table 4.
Mean time computed for each step of a digital workflow with its standard error
| Digital Workflow | |
|---|---|
| Case | ST |
| Patient registration time | 2 min 0 s (±7 s) |
| Execution time | 7 min 6 s (±25 s) |
| Reporting time | 3 min 28 s (±20 s) |
| Assemblage time | 2 min 30 s (±15 s) |
| Delivery time | 1 min 42 s (±10 s) |
| Operator time | 2 min 20 s (±14 s) |
| Total time | 19 min 6 s (±40 s) |
Discussion
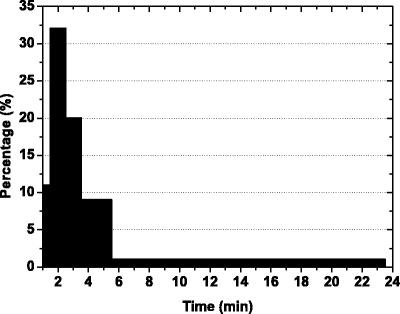
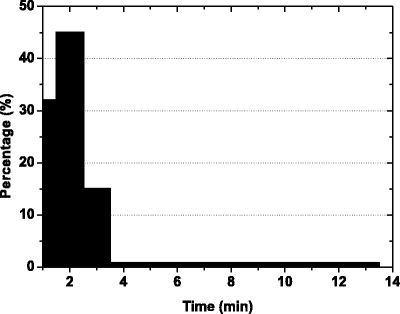
The average values previously presented were computed by using a simple mathematical definition of mean. To take into account the different time distribution of the collected data for each step, we plotted the data as frequency class, by using histograms. This representation allows a comparison of mean values and median that takes into account the weight of each class.
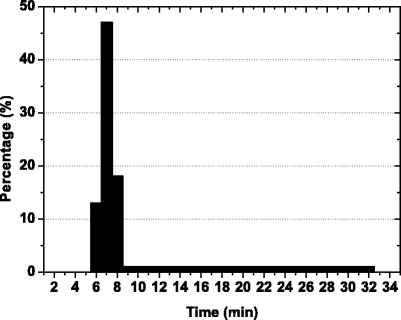
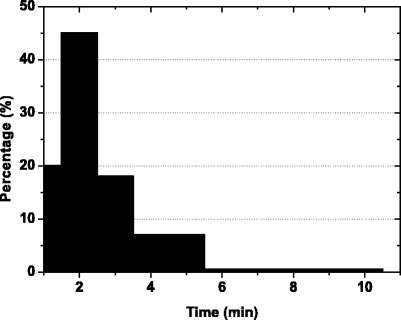
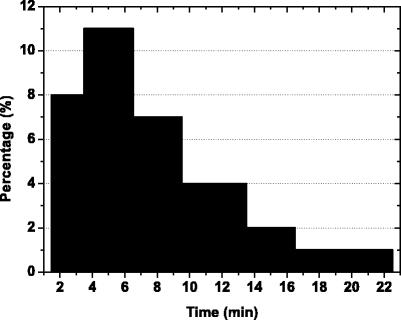
Figures 3, 4, 5, and 6 show the frequency classes vs. time in a traditional process for Patient Registration, Execution, Reporting, and Delivery, respectively. Table 5 resumes the mean time and the median values computed by their simple mathematical definitions or by frequency class distribution.
Fig 3.
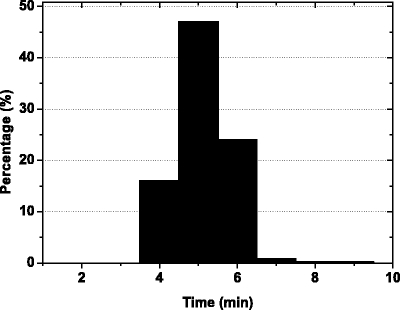
Histogram representing frequency density distribution of patient registration time for a traditional x-ray workflow.
Fig 4.
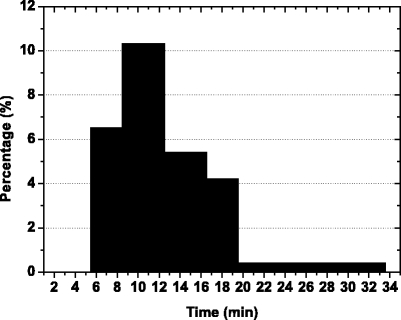
Histogram representing frequency density distribution of execution time for a traditional x-ray workflow.
Fig 5.
Histogram representing frequency density distribution of reporting time for a traditional x-ray workflow.
Fig 6.
Histogram representing frequency density distribution of delivery time for a traditional x-ray workflow.
Table 5.
Mean time and time median value computed for each step of a traditional process by their mathematical definitions or by frequency class distributions
| Traditional process | Arithmetical | Frequency class | ||
|---|---|---|---|---|
| Step | Mean time | Median | Mean time | Median |
| Patient registration | 1 min 58 s | 1 min 45 s | 1 min 55 s | 1 min 44 s |
| Execution | 11 min 49 s | 10 min 31 s | 11 min 55 s | 10 min 57 s |
| Reporting | 7 min 28 s | 6 min 36 s | 9 min 37 s | 6 min 48 s |
| Delivery | 1 min 45 s | 37 s | 1 min 52 s | 49 s |
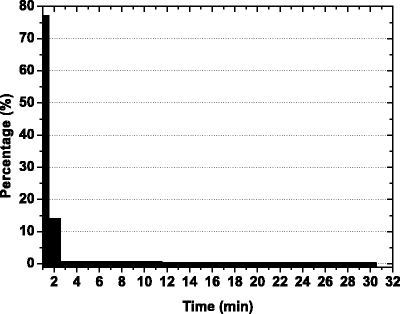
Histograms for the same four steps, but this time for the digital process, are presented in Figures 7, 8, 9 and 10, and the calculated data are shown in Table 6.
Fig 7.
Histogram representing frequency density distribution of patient registration time for a digital x-ray workflow.
Fig 8.
Histogram representing frequency density distribution of execution time for a digital x-ray workflow.
Fig 9.
Histogram representing frequency density distribution of reporting time for a digital x-ray workflow.
Fig 10.
Histogram representing frequency density distribution of delivery time for a digital x-ray workflow.
Table 6.
Mean time and time median value computed for each step of a digital process by their mathematical definitions or by frequency class distributions
| Digital process | Arithmetical | Frequency class | ||
|---|---|---|---|---|
| Step | Mean time | Median | Mean time | Median |
| Patient registration | 2 min 0 s | 1 min 36 s | 1 min 58 s | 1 min 40 s |
| Execution | 7 min 6 s | 6 min 3 s | 7 min 14 s | 6 min 0 s |
| Reporting | 3 min 28 s | 2 min 21 s | 4 min 24 s | 2 min 22 s |
| Delivery | 1 min 42 s | 1 min 14 s | 1 min 52 s | 1 min 24 s |
As shown in Tables 5 and 6, the arithmetical mean and histogram values are generally similar, taking into account the experimental error, as in the Patient Registration step. In contrast, we found relevant differences in Reporting. In our opinion, this difference is attributable to the number of cases, needing more time to be discussed and resolved, and also acquiring possible previous examinations. In fact, the difference between the two mean reporting times is higher in the traditional process than in the digital one, where possibly previous examinations are stored in RIS/PACS system. Our interpretation seems to be supported by the presence of a long tail both for traditional and digital processes (Figs. 5 and 9).
Comparing the total process times (Tables 3 and 4), we can calculate the time percentage reduction of a digital process compared to its traditional counterpart (Table 7).
Table 7.
Time percentage reduction of a digital process compared to a traditional one
| Digital radiology | Traditional radiology | Reduction (%) | |
|---|---|---|---|
| Total time | Case | Total time | |
| 19 min 6 s | ST | 29 min 26 s | 35 |
| A | 34 min 7 s | 44 | |
| B | 39 min 28 s | 52 | |
This result seems very significant and leads to a number of possible interpretations. Obviously, the main point is that the most important time differences are found in Execution and Reporting. As far as Execution is concerned, the complete digital handling of images eliminates the use of film and all operations for film developing. A second advantage is that the bad images no longer require operators to perform the same examinations again, but only postprocessing, perhaps multiple, copies of the acquired image, in order to modify its main parameters. This elaboration is clearly much faster than the traditional one. The digital process also strongly influences the Reporting step as a result of the following factors: a large number of tools to speed up and optimize the analysis of the image, as performed by the radiologist; the use of PC speech recognition; fast access to image database in case of comparison with previous examinations of the same patient; and the printing and signing of the report can be made practically at the same moment, directly from the radiologist. The whole process is filmless and paperless, avoiding also the need for people movements inside department.
Conclusion
Based on the results, the use of a RIS/PACS system in a Radiology Department substantially reduces the time for completion of x-ray examinations, giving a time reduction ranging from 35% to 52%. In principle, this can lead to an increase in the annual number of examinations, and a decrease in general costs. Moreover, the time needed for delivery of results can be reduced. In fact, in Tables 5 and 6 the data on delivery time appears to be essentially the same, but we must consider that this refers to the time when the report is handed to the patient. If we take into account the time it takes to transfer the report from the department to the Front Office, the difference could be 4 days at the least (for the traditional Radiology Department).
Finally, all the time data were acquired by using a manual stopwatch, but we are now doing a comparison of the time data for each step based on data from the RIS/PACS system. A comparison between the two procedures is underway.
Acknowledgments
We (A.T. and C.M.) acknowledge funding from a grant by Provincia di Macerata (Italy). We would like to acknowledge Barbara Maceri and Giacomo Giannini for helpful discussions and support during the work and for the critical reading of the manuscript.
References
- 1.Reneir B, Siegel E, Carrino JA. Workflow optimization: current trends and future directions. J Digit Imaging. 2002;15:141–152. doi: 10.1007/s10278-002-0022-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reiner BI, Siegel EL. The cutting edge: strategies to enhance radiologist workflow in a filmless/paperless imaging department. J Digit Imaging. 2002;15:178–190. doi: 10.1007/s10278-002-0029-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lepanto L. Impact of electronic signature on radiology report turnaround time. J Digit Imaging. 2003;16:306–309. doi: 10.1007/s10278-003-1730-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramaswamy MR, Chaljub G, Esch O, Fanning DD, Sonnenberg E. Continuous speech recognition in MR imaging reporting: advantages, disadvantages, and impact. AJR. 2000;174:617–622. doi: 10.2214/ajr.174.3.1740617. [DOI] [PubMed] [Google Scholar]
- 5.Cavagna E, Berletti R, Schiavon F, Scarsi B, Barbato G. Optimized delivery of radiological reports: applying six sigma methodology to a radiology department. Radiol Med. 2003;105:205–214. [PubMed] [Google Scholar]
- 6.Andriole KP. Productivity and cost assessment of computed radiography, digital radiography, and screen-film for outpatient chest examinations. J Digit Imaging. 2002;15:161–169. doi: 10.1007/s10278-002-0026-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reiner BI, Siegel EL. Technologists’ productivity when using PACS: comparison of film-based versus filmless radiography. AJR. 2002;179:33–37. doi: 10.2214/ajr.179.1.1790033. [DOI] [PubMed] [Google Scholar]
- 8.Palma L, Grisi G, Cuttin R, Rimondini A. Digital vs conventional radiography: cost and revenue analysis. Eur Radiol. 1999;9:1682–1692. doi: 10.1007/s003300050910. [DOI] [PubMed] [Google Scholar]
- 9.Tolkki O, Ahovuo J, Kauppinen T, Fyhr N, Kujala J, Parvinen P: Patient in Process, Benefits of Reduced Throughtput Time-Case HUSpacs. EuroPACS-MIR (2004), Edizioni Università di Trieste, pp 155–158, 2004
- 10.Ralston MD, Coleman RM, Beaulieu DM, Scrutchfield K, Perkins T. Progress toward paperless radiology in the digital environment: planning, implementation, and benefits. J Digit Imaging. 2004;17:134–143. doi: 10.1007/s10278-004-1002-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reiner BI, Siegel EL, Flagle C, Hooper FJ, Cox RE, Scanlon M. Effect of filmless imaging on the utilization of radiologic services. Radiology. 2000;215:163–167. doi: 10.1148/radiology.215.1.r00ap41163. [DOI] [PubMed] [Google Scholar]


