Abstract
Objective
Cannabis is the most widely used illicit drug. Acute cannabis administration increases blood pressure and heart rate and tolerance develops to these effects with heavy use. A valid and reliable withdrawal syndrome occurs in most daily users, but few studies have assessed the cardiovascular effects of withdrawal. The objective of this report is to describe unexpected changes in cardiovascular function during brief periods of supervised cannabis use and abstinence in daily cannabis users.
Methods
A within-subjects ABAC crossover study in which inpatient volunteers smoked cannabis ad-libitum (A), and abstained from cannabis (B/C). Vital signs were obtained three times daily during eleven inpatient days for thirteen daily cannabis users (11 Male, 8 African American).
Results
Blood pressure increased significantly during periods of cannabis abstinence compared with periods of cannabis use. The magnitude of increase was substantial in a subset (N=6) of participants, with mean increases of up to 22.8mmHg systolic and 12.3mmHg diastolic blood pressure observed. Heart rate also increased during abstinence when measures collected during periods of acute intoxication were excluded, but the magnitude of effect was not clinically significant.
Conclusions
Abrupt cessation of heavy cannabis use may cause clinically significant increases in blood pressure in a subset of users. Blood pressure should be monitored among those attempting to reduce or quit frequent cannabis use, particularly those with preexisting hypertension. The time course of this effect is currently unknown and requires further study.
Keywords: Cannabis, Marijuana, Blood Pressure, Hypertension, Withdrawal
Background
Cannabis (marijuana, hashish) is the most widely used illicit drug in the world with an estimated 160 million current users (UNODC, 2007). In the past decade, treatment admissions for cannabis use disorders have increased significantly, and the number of people who meet criteria for dependence on cannabis now exceeds the number who meet dependence criteria for any other illicit drug (UNODC, 2007; AIHW, 2008; EMCDDA, 2008; SAMHSA, 2008). Despite such widespread use and abuse, relatively little is known about the cardiovascular effects and possible associated health risks associated with chronic cannabis use.
Acute cannabis administration has been shown to increase resting heart rate and blood pressure, and induce orthostatic hypotension (Jones, 2002). Increased heart rate following acute cannabis exposure has been shown to be dose-related (Heishman et al., 1989). Peak effects on heart rate appear to occur 10 to 15 minutes after smoking and result in an increase of 20 to 30 beats per minute, but mean increases as high as 43.5 beats per minute have been reported (Chait and Zacny, 1992; Galanter et al., 1972; Heishman et al., 1989; Ilan et al., 2005). There are few studies in which the effects of smoked cannabis administration on blood pressure are reported. Supine blood pressure has been shown to increase following cannabis exposure (Mathew et al., 1993), but blood pressure has also been shown to drop when participants move from a supine to standing position (Renault et al., 1974). Insufficient published data are available to confidently report on the time course or typical magnitude of these effects, and it appears that orthostatic hypotension is reliably observed whereas an increase in supine blood pressure is not. Epidemiological studies and case reports have linked acute cannabis intoxication to myocardial infarction, angina, arrhythmias, transient ischemic attacks, and stroke (Karch, 2006). However, associations between cannabis use and these cardiovascular events are not always consistent, case reports of these types of occurrences are rare, and controlled studies are generally lacking.
Tolerance to the acute cardiovascular effects of cannabis develops rapidly with repeated exposure. In laboratory studies, the acute cardiovascular effects of delta-9-tetrahydrocannabinol (THC; the primary psychoactive component of cannabis) are attenuated with repeated administration, and have even been shown to result in a reduction of heart rate and blood pressure relative to baseline levels (Benowitz and Jones, 1975; Benowitz and Jones, 1981). However, Jones (Jones, 2002) recently pointed out that understanding of the cardiovascular effects of chronic cannabis use is limited by the fact that most human research has been of short duration, used relatively low doses of smoked cannabis or oral THC, and has largely excluded participants who are female, older, or exhibit symptoms of cardiovascular disease.
Because tolerance develops to the acute cardiovascular effects of cannabis with repeated use, it is plausible that a rebound increase in heart rate and blood pressure would be observed following abrupt cessation of heavy use. Recent research has demonstrated that a reliable, valid, and pharmacologically specific withdrawal syndrome occurs in a majority of heavy (daily) cannabis users when they abruptly stop use (Budney et al., 2004; Haney, 2005; Budney and Hughes, 2006), but few published studies of cannabis withdrawal effects have included cardiovascular measures. In a recent outpatient study of cannabis withdrawal, heart rate was higher during abstinence compared with periods of cannabis use (Vandrey et al., 2008). In that study a trend towards increased systolic blood pressure during abstinence was also observed, but was not statistically significant. However, no effect of withdrawal was found on cardiovascular function (HR or BP) in two similar outpatient studies from the same laboratory (Budney et al., 2001; Budney et al., 2003).
This paper describes cardiovascular effects observed during a study of hypnotic medication effects in heavy cannabis users. High blood pressure readings (SBP>160mmHg, DBP >90mmHg) were observed for several study participants during periods of cannabis abstinence, and most of these subjects had no prior evidence of hypertension on study admission or during study periods when cannabis use was allowed. Based on these observations a specific exclusion criterion was adopted prior to study completion to exclude those who exhibited any evidence of hypertension during the study intake process. Here we report on findings from study participants who completed participation prior to the implementation of the hypertension exclusion criterion.
Methods
The study procedures were reviewed and approved by the John Hopkins Medicine Institutional Review Board and conducted in accordance with the ethical standards of the Helsinki Declaration. A within-subject crossover design was used in which participants completed two 5-day inpatient study phases consisting of an initial 2-day period during which participants were allowed to use cannabis ad libitum between 12:00 and 21:00, followed immediately by a 3-day period of forced cannabis abstinence. During one cannabis abstinence period, participants were administered extended-release zolpidem each night at bedtime, and during the other abstinence period placebo was administered. The order in which participants received zolpidem or placebo was counterbalanced across participants. The inpatient study phases were separated by an 8-day outpatient washout period, during which daily cannabis use was reestablished in the participants’ home environment.
Daily cannabis users were recruited to participate in the study via newspaper advertisements. Participants were between 18–55 years of age; used cannabis at least 25 days per month for at least 1 year with no indication that they were seeking treatment for cannabis or using cannabis for medical purposes; had no current Axis I psychiatric disorders other than cannabis or nicotine dependence; were not currently taking psychoactive medication; were not pregnant or breastfeeding; and provided a urine specimen that was positive for THC and negative for other drugs of abuse at study intake. Informed consent was obtained for all participants.
Fourteen participants were enrolled and 13 completed the study (11 male, 2 female). Those who completed the study were mostly African American (N=8), had a mean (SD) age of 31 (9) years, had been using cannabis at least once per week for 16 (9) years, and used cannabis an average of 5 (3) times per day during the 3 months prior to admission in the study. Alcohol and other drug use were infrequent among participants, but all smoked tobacco cigarettes (6 (5) cigarettes/day) daily. One male African American participant (017) was taking lisinopril (20mg/day) and hydrochlorothiazide (12.5mg/day) for hypertension on admission to the study. This medication regimen had been stable for 12 months and was continued uninterrupted during study participation except for one day when lisinopril was increased to 40mg following 2 days of sustained elevated blood pressure during his second cannabis abstinence period. No other study participants reported current or past cardiovascular disease.
Resting heart rate and supine blood pressure were measured at 10:00, 16:00, and 21:30 each day using an automated monitor (Criticare Systems Inc., Waukesha, WI).
A preliminary statistical test was conducted using a one-way analysis of variance (ANOVA) to determine if there was a main effect of drug condition (zolpidem versus placebo) on blood pressure and heart rate during the two cannabis abstinence periods. As expected, zolpidem did not affect daytime cardiovascular function compared with placebo. Because no effect of zolpidem was observed, data collected during the two abstinence periods were collapsed in subsequent analyses.
Blood pressure and heart rate assessments were then analyzed using a repeated measures regression model in which cannabis use condition (ad libitum use versus abstinence) and replication (first study phase versus second study phase) were entered as factors. This model was selected because the unbalanced number of assessments between the cannabis use and abstinence periods precluded use of parametric analyses without either collapsing data into means by cannabis use condition (which would have reduced natural variability) or excluding one day of data during the abstinence condition. The effects of cannabis on blood pressure and heart rate were assessed using Tukey’s post-hoc tests by comparing measures obtained at 10:00 (prior to ad libitum cannabis use) with measures obtained at 16:00 and 21:30 (after initiation of ad libitum cannabis use) on study days in which cannabis smoking was allowed. Data analysis was conducted using SAS statistical software Version 9.1 (Cary, NC).
Results
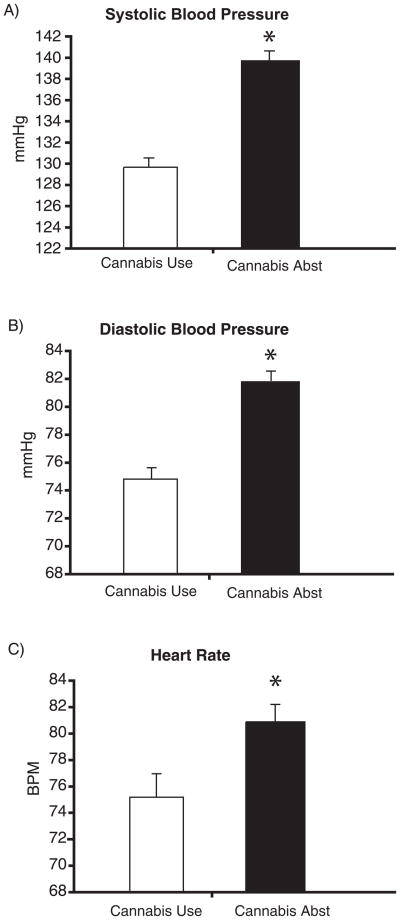
Significant main effects of cannabis use condition were observed for systolic blood pressure (F = 47.05, p < .001) and diastolic blood pressure (F = 23.97, p < .001). Systolic blood pressure increased from a mean (SEM) of 129.6 (0.9) mmHg during cannabis use to a mean of 139.8 (0.8) mmHg during abstinence. Diastolic blood pressure increased from a mean of 74.8 (0.7) mmHg during cannabis use to a mean of 81.8 (0.6) mmHg during abstinence. Mean arterial pressure increased from a mean of 93.0 (0.7) mmHg during cannabis use to a mean of 101.1 (0.6) mmHg during abstinence.
Systolic and diastolic blood pressures measured at the 16:00 and 21:30 time points were lower (p < .01) compared with the 10:00 time point during cannabis use conditions. Post-hoc tests also indicated that blood pressure during the first and second cannabis use periods were not different from each other, but were both lower than during the first abstinence period (p < .01). This suggests that the abstinence-induced increase in blood pressure was reversed with resumed cannabis use.
A main effect of cannabis use condition was not observed for heart rate. Heart rate measured at the 16:00 and 21:30 time points was higher (p < .01) than when measured at the 10:00 time point during cannabis use, suggesting that cannabis induced tachycardia may have washed out an effect of cannabis use condition. The repeated measures regression was repeated using only the 10:00 time points (which eliminated the effects of acute cannabis intoxication) and a main effect of cannabis use condition (F = 5.18, p < .05) was observed. Heart rate assessed at 10:00 increased from a mean of 75 (1.8) bpm during cannabis use to a mean of 81 (1.3) bpm during abstinence. Post-hoc comparisons also indicated that heart rate during the first and second cannabis use periods were not different from each other, but were both lower than during the first abstinence period (p < .01).
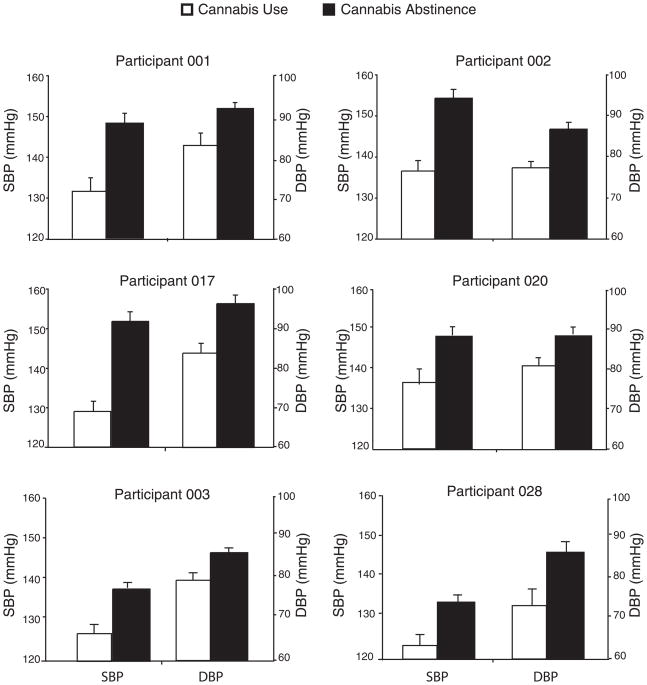
No main effects of replication were observed. Figure 1 shows mean cardiovascular measures collapsed across participants and study phases. Figure 2 shows mean blood pressure measures of 6 participants for which the most pronounced abstinence effects on cardiovascular parameters were observed. These participants, roughly half of the study sample, each showed a mean blood pressure increase that was greater than the mean increase for the entire study sample during abstinence (10mmHg SBP and 7mmHg DBP). In this sub-group of participants, systolic blood pressure increased from a mean (SEM) of 130.9 (2.1) mmHg during cannabis use to a mean of 146.6 (3.1) mmHg during abstinence, and diastolic blood pressure increased from a mean of 78.1 (2.4) mmHg during cannabis use to a mean of 87.0 (2.9) mmHg during abstinence.
Figure 1.
Mean systolic blood pressure (Panel A), diastolic blood pressure (Panel B), and 10:00am heart rate assessments collapsed across participants (N=13). The * indicates a significant difference (p<.05) between mean values obtained during the two ad libitum cannabis use periods and mean values obtained during the two abstinence periods.
Figure 2.
Mean blood pressure by study phase for the 6 participants who demonstrated the greatest abstinence effect. Participant 017 had been diagnosed with hypertension prior to study participation and was taking medication during the study (see Methods for details). Participant 001 is an African American female, participants 003 and 020 are Caucasian males, and the other three are African American males.
Discussion
Cardiovascular disease is the leading cause of death globally (Rosamond et al., 2007; WHO, 2009) and cannabis is the most widely abused illicit drug in the world. The results of this study indicate that abrupt cessation of cannabis use can lead to significant increases in blood pressure and heart rate in a subset of daily cannabis users. These effects were observed reliably across two abstinence periods and were reversed when cannabis use was resumed (i.e., blood pressure and heart rate during the cannabis use period that followed the first abstinence period returned to levels observed during the initial cannabis use period). This suggests a cardiovascular effect pharmacologically specific to cannabis use.
The generally agreed upon classification for hypertension is a sustained systolic blood pressure of >140 mmHg diastolic blood pressure of > 90 mmHg, although lower parameters (≤130/80) are recommended among patients with other cardiovascular risk factors such as diabetes (Chobanian et al., 2003). In the present study, none of the heavy cannabis users had average blood pressure in the hypertensive range during periods of cannabis use, but 4 of 13 (31%) and 2 of 13 (15%) of participants had average blood pressure assessments in the hypertensive range for SBP and DBP respectively during abstinence. Research also indicates that every increase of 20 mmHg systolic and 10 mmHg diastolic blood pressure above 115/75 mmHg results in a doubling of relative risk for cardiovascular disease related mortality (Chobanian et al., 2003). One participant in this study had a mean increase of 22.8 mmHg systolic and 12.3 mmHg diastolic blood pressure, and the half of the study sample showing the greatest effect had mean increases of 15.7 mmHg systolic and 8.9 mmHg diastolic blood pressure. This indicates that the magnitude of the increase in blood pressure observed in this study is clinically meaningful.
There were no clear demographic or cannabis use characteristics that predicted the magnitude of effect observed for individual study participants. While most study participants were male, one of the two female participants was among the subgroup that showed the greatest increase in blood pressure suggesting that this effect is not gender specific. However, with only two female participants we cannot establish whether there are gender differences in the magnitude of cardiovascular response to cannabis cessation. It is also important to note that the participants in this study were older and more likely to be African American compared with prior studies of cannabis withdrawal that included cardiovascular measures. Both age and African American heritage are established risk factors for hypertension (Kaplan, 1994). Also, though the majority of cannabis users are adolescents and young adults, approximately one-third of current users and 23–35% of treatment admissions for cannabis use disorders are age 30 or older (AIHW, 2008; SAMHSA, 2007, 2009). Thus, the current study is representative of a large sub-population of cannabis users, but one that has been generally underrepresented in prior studies.
Due to the short duration of abstinence in this study and the lack of pre-cannabis use cardiovascular measures, it is uncertain whether these effects are a product of cannabis withdrawal (i.e., a time limited increase) or if these effects represent a rebound or offset effect of cannabis-induced decrease in blood pressure and heart rate (i.e., a time unlimited increase). If these cardiovascular changes reflect a withdrawal effect, the cause may be a direct pharmacological withdrawal effect or secondary effects of other symptoms of cannabis withdrawal (e.g. anxiety). On the other hand, a rebound or offset effect would more clearly indicate a direct effect of the endocannabinoid system, and would have significant clinical implications. First, reduction or cessation of frequent cannabis use would be cause for evaluating and likely modifying ongoing treatment for cardiovascular disease among patients. Second, it would suggest the need for careful observation of cardiovascular effects (beneficial or harmful) in the development of medications that modulate the endocannabinoid system.
There are limitations of this study with regard to assessing the risk of an acute cardiovascular event occurring in cannabis users during a quit attempt. First, cardiovascular risk is limited to the duration of the effect, and it is uncertain whether the abstinence-induced effects observed persist for longer than 3 days. Most cannabis withdrawal effects last 1–2 weeks, though sleep-related symptoms have been shown to persist longer (Budney et al., 2003). Greater cardiovascular risk would be expected if the increase in blood pressure resulted from a rebound or drug offset effect, which would persist indefinitely. That said, most participants in this study (69%) did not exhibit cardiovascular effects large enough to meet accepted criteria for a diagnosis of hypertension. Thus, if there is a risk for an acute cardiovascular event as a result of increased blood pressure, it is likely limited to a minority of users, and, even then, may not present a true risk in the absence of other cardiovascular risk factors.
Accounting for all assessment points, there was no effect of cannabis abstinence on heart rate. A statistically significant effect of cannabis abstinence was observed when analysis was limited to assessments conducted in the morning, which eliminated time points that could have been affected by cannabis intoxication during the ad-libitum use periods. However, the increase observed in that analysis (increase of 5 bpm to mean of 81 bpm) does not indicate that this effect is likely to result in clinically relevant cardiovascular risk.
Conclusion
Cannabis withdrawal in this study resulted in a significant increase in blood pressure that was of sufficient clinical magnitude to suggest the need for recognition and further consideration with regards to research eligibility. This effect was reliably observed across 2 different abstinence periods. Mean blood pressure was qualitatively higher for all 13 participants during cannabis abstinence periods compared with ad libitum cannabis use periods, and the increase during abstinence resulted in mean blood pressure in the range of Stage 1 hypertension for 4 participants (31%). These were unexpected findings observed in a research study designed to investigate the effects of cannabis use and abstinence on sleep, and the limitations of the study design preclude understanding the mechanism or duration of this effect. Additional research is required to examine the time course and generality of these results. Studies with larger and more diverse samples (e.g., more females; those with risk factors for cardiovascular disease) may also help clarify whether specific risk factors or genotypes are associated with abstinence-induced hypertension in cannabis users. If additional research confirms these results, independent of the underlying cause and time course of the effect, heavy cannabis users who abruptly abstain should receive cardiovascular monitoring and treatment if indicated by established medical guidelines.
Acknowledgments
This publication was made possible by Grants R21-DA025794 and DA023186 from the National Institute on Drug Abuse (NIDA) and Grant UL1 RR 025005 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. The authors thank the research and medical staff of the Johns Hopkins Behavioral Pharmacology Research Unit and Clinical Research Unit for their valuable contributions to this work. The authors have no conflicts of interest to report in relation to this research. This study is registered at ClinicalTrials.gov (NCT00893269).
Research Support: Grants DA025794 (Vandrey) and DA023186 (Strain) from the National Institute on Drug Abuse (NIDA), and Grant UL1 RR 025005 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research
References
- AIHW. Alcohol and other drug treatment services in Australian Capital Territory 2006–07: findings from the National Minimum Data Set. Australian Institute of Health and Welfare; 2008. [Google Scholar]
- Benowitz N, Jones RT. Cardiovascular and metabolic considerations in prolonged cannabinoid administration in man. J Clin Pharmacol. 1981;21:214S–223S. doi: 10.1002/j.1552-4604.1981.tb02598.x. [DOI] [PubMed] [Google Scholar]
- Benowitz NL, Jones RT. Cardiovascular effects of prolonged delta-9-tetrahydrocannabinol ingestion. Clin Pharmacol Ther. 1975;18:287–297. doi: 10.1002/cpt1975183287. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Hughes JR. The Cannabis Withdrawal Syndrome. Current Opinion in Psychiatry. 2006;19 doi: 10.1097/01.yco.0000218592.00689.e5. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Hughes JR, Moore BA, Novy PL. Marijuana abstinence effects in marijuana smokers maintained in their home environment. Arch Gen Psychiatry. 2001;58:917–924. doi: 10.1001/archpsyc.58.10.917. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Hughes JR, Moore BA, Vandrey RG. A review of the validity and significance of the cannabis withdrawal syndrome. Am J Psychiatry. 2004;161:1967–1977. doi: 10.1176/appi.ajp.161.11.1967. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Moore BA, Vandrey RG, Hughes JR. The time course and significance of cannabis withdrawal. J Abnorm Psychol. 2003;112:393–402. doi: 10.1037/0021-843x.112.3.393. [DOI] [PubMed] [Google Scholar]
- Chait LD, Zacny JP. Reinforcing and subjective effects of oral delta-9-THC and smoked marijuana in humans. Psychopharmacology. 1992;107:255–262. doi: 10.1007/BF02245145. [DOI] [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- EMCDDA. Annual report on the state of the drugs problem. European Monitoring Centre for Drugs and Drug Addiction; Lisbon: 2008. [Google Scholar]
- Galanter M, Wyatt RJ, Lemberger L, Weingartner H, Vaughan TB, Roth WT. Effects on humans of 9 -tetrahydrocannabinol administered by smoking. Science. 1972;176:934–936. doi: 10.1126/science.176.4037.934. [DOI] [PubMed] [Google Scholar]
- Haney M. The marijuana withdrawal syndrome: Diagnosis and treatment. Current Psychiatry Reports. 2005;7:360–366. doi: 10.1007/s11920-005-0036-1. [DOI] [PubMed] [Google Scholar]
- Heishman SJ, Stitzer ML, Yingling JE. Effects of tetrahydrocannabinol content on marijuana smoking behavior subjective reports and performance. Pharmacol Biochem Behav. 1989;34:173–179. doi: 10.1016/0091-3057(89)90369-9. [DOI] [PubMed] [Google Scholar]
- Ilan AB, Gevins A, Coleman M, ElSohly MA, de Wit H. Neurophysiological and subjective profile of marijuana with varying concentrations of cannabinoids. Behav Pharmacol. 2005;16:487–496. doi: 10.1097/00008877-200509000-00023. [DOI] [PubMed] [Google Scholar]
- Jones RT. Cardiovascular System Effects of Marijuana. J Clin Pharmacol. 2002;42:58S–63S. doi: 10.1002/j.1552-4604.2002.tb06004.x. [DOI] [PubMed] [Google Scholar]
- Kaplan NM. Ethnic aspects of hypertension. Lancet. 1994;344:450–452. doi: 10.1016/s0140-6736(94)91774-4. [DOI] [PubMed] [Google Scholar]
- Karch SB. Cannabis and Cardiotoxicity. Forensic Science, Medicine, and Pathology. 2006;2:13–18. doi: 10.1385/FSMP:2:1:13. [DOI] [PubMed] [Google Scholar]
- Mathew RJ, Wilson WH, Humphreys D, Lowe JV, Weithe KE. Depersonalization after marijuana smoking. Biol Psychiatry. 1993;33:431–441. doi: 10.1016/0006-3223(93)90171-9. [DOI] [PubMed] [Google Scholar]
- Renault PF, Schuster CR, Freedman DX, Sikic B, de Mello DN. Repeat administration of marihuana smoke to humans. Arch Gen Psychiatry. 1974;31:95–102. doi: 10.1001/archpsyc.1974.01760130071012. [DOI] [PubMed] [Google Scholar]
- Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics--2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69–171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- SAMHSA. National Household Survey on Drug Use and Health, data from 2006 survey. Substance Abuce and Mental Health Data Archive; Ann Arbor, MI: 2007. [Google Scholar]
- SAMHSA. Treatment episode data set (TEDS) 1995 -2007: National admissions to substance abuse treatment services. US Department of Health and Human Services; Rockville, MD: 2008. [Google Scholar]
- SAMHSA. Treatment Episode Data Set (TEDS) Highlights - - 2007 National Admissions to Substance Abuse Treatment Services. Substance Abuse and Mental Health Services Administration, Office of Applied Studies; Rockville, MD: 2009. [Google Scholar]
- UNODC. World Drug Report - 2007. United Nations Office on Drugs and Crime; New York, NY: 2007. [Google Scholar]
- Vandrey RG, Budney AJ, Hughes JR, Liguori A. A within-subjects comparison of withdrawal symptoms during abstinence from cannabis, tobacco, and both substances. Drug Alcohol Depend. 2008;92:48–54. doi: 10.1016/j.drugalcdep.2007.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Cardiovascular Diseases (CVDs) Fact Sheet. World Health Organization; Geneva: 2009. [Google Scholar]