Abstract
Background
As America’s baby boom generation reaches retirement, the number of elders, and, in turn, the number of lay individuals who support them, will continue to increase. With the important services caregivers provide, it is critical that we recognize and provide assistance to the informal caregivers who play this important role in our society. The network of support provisioned by relatives, partners, friends, and neighbors suggests that the dyadic, unidirectional caregiver–care recipient relationship assumed by caregiver research so far and by resources deployed to assist caregivers may be insufficient to ascertain and meet the needs of the care community.
Methods
In this article, we describe the extension of a Web-based personal health record system, iHealthSpace, for explicitly and openly incorporating caregivers into the care community.
Results
Using this portal, a set of business rules was implemented to support the creation of custodial accounts. These business rules will be used to create modules that support diabetes care in an adult population.
Conclusions
We successfully extended an existing patient portal to accommodate the creation of custodial accounts. We will use this portal to assess the impact of custodial access in the care of older patients with diabetes.
Keywords: caregivers, patient portal, personal health records
Background
“Health care” is often defined as services provided by medical professionals in hospitals, doctors’ offices, and nursing homes. However, for most individuals with chronic illness or disability, the foundation of health care is often delivered at home, everyday, and is provided informally by family members, friends, and neighbors. This care ranges from providing help with taking medications, scheduling appointments for medical visits, and understanding medical advice to more basic assistance with eating, bathing, housework, grocery shopping, and meal preparation.1
More than 65 million people, 29% of the U.S. population, provide this care for a chronically ill, disabled, or aged family member or friend during any given year.2 Already, physicians, nurses, and other care providers depend heavily on family members. In a 2008 report, the Institute of Medicine (IOM) called for a new perspective on family caregivers: “The definition of the health care workforce must be expanded to include everyone involved in a patient’s care: health care professionals, direct-care workers, informal caregivers (usually family and friends), and patients themselves. All of these individuals must have the essential data, knowledge, and tools to provide high-quality care.” 3
As the IOM committee also noted, “Exactly when and how providers need to incorporate the family into the health care process is not yet well understood, but such incorporation is relevant across the full spectrum of institutional, ambulatory, and residential patient-care settings.”4 Complicating these recommendations, however, are anecdotal perceptions that families can be “troublesome, interfering with proper care, fighting among themselves, challenging physicians’ or nurses’ authority and generally behaving badly.”5 Further, while studies suggest that caregiver support may be more significant among specific cultures,6,7 cognitively impaired,7 and specific disease domains,8,9 these studies are small and generally divided on caregiver efficacy in effecting outcomes.
A Framework for Caregiving
Most studies of family caregiving define care recipients as those who require assistance with care and, in turn, label the relative who accompanies or cares for them as the caregiver. The discourse on family caregiving generally treats care receiving and caregiving discretely, suggesting that informal care and support flow in a unidirectional manner from healthy caregiver to chronically ill or disabled care recipient.10
Sociologically informed exploration reveals that “informal care dynamics,” particularly in the social context of a family, are more aptly relational11 and reciprocal.12 Lingler and colleagues13 illustrated three main ways in which care patterns may depart from traditional notions of dyadic unidirectional family caregiving: (a) couples who are aging and chronically ill may compensate for one another’s deficits in reciprocal relationships and serve as mutual caregivers and care recipients; (b) patients may be cared for by multiple family members and other informal caregivers who share in the caregiving duties; and (c) “family care chains,” where a given individual functions as caregiver to one relative and care recipient to another.
Although these dynamics are common in care situations, designs in most research on caregiving and current systems to assist caregivers do not accommodate them, calling into question the implications of study findings for practice.13 Studies may overestimate the impact of the caregiving burden by limiting their subject pools to traditionally defined primary caregivers. Alternatively, researchers can underestimate the aggregate burden of caregiving by failing to capture shared-care dynamics. The characteristics of the full range of care that is provided may not be evaluated accurately, and the interpretation of the effects of interventions may have limited applicability when one of these other caregiving models, in fact, applies.13
An Opportunity for Personal Health Record Systems
Personal health care record systems that offer patients access to their health records, connect patients with their care providers, and help patients find peer support are emerging to become part of the larger strategy to engage patients in effective self-management and potentially contribute to improved outcomes. Providing a place for caregivers in such systems presents an untapped opportunity to improve transparency and further reduce fragmentation of care. This effect may be particularly potent among elderly patients with chronic illness for whom caregivers are often the only people who have experienced the entire course of their family member’s illness.
The nearly 66 million caregivers are a critical extension of our formal health care system—they already are turning to health care providers, the Internet, and other caregivers for information and support. Almost half of them report using technology, such as electronic organizers or calendars, emergency response systems, electronic systems that send information to a doctor or care manager, and electronic sensors to detect safety problems.14 Among the strategies advocated to support caregivers so that they can continue in their roles is to identify and promote the use of technologies that can facilitate caregiving.
In this article, we describe the extension of a Web-based personal health record system, iHealthSpace, to formally incorporate caregivers, and its potential application in diabetes care.
iHealthSpace Overview
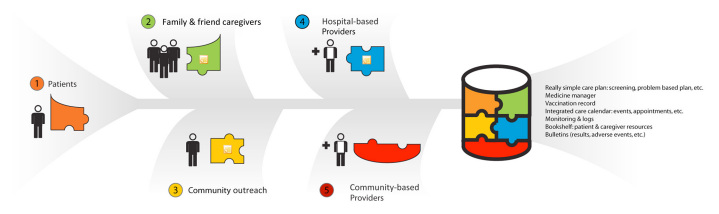
iHealthSpace (Figure 1 ) is a Web site where patients and their providers can communicate plans and share information, but it also makes this trusted network available to the patient’s broader community of caregivers and other providers (Figure 2 ). The site is designed to allow anyone with Internet access to register and join. In addition, an organization, record system, or individual practice may seek partnership with iHealthSpace so that attendant patients can take advantage of greater connectivity—either through messaging their care team and/or access to clinical data. One of the legacy electronic health record systems in place at the institution, Oncall, was used as an exemplar partnership to demonstrate how iHealthSpace may balance the requirements of local systems and the practices in which those systems are in place with those of patients and their caregivers who wish to collaborate and share resources.
Figure 1.
iHealthSpace main page.
Figure 2.
Individual care comprises communication and coordination among multiple entities, including their doctors, visiting home nurses, nutritionists, physical therapists, psychotherapists, emergency personnel, alternative medicine providers, and family/friend caregivers.
iHealthSpace beta was released February 2010 to patients belonging to a subset of primary care providers in the largest ambulatory clinic at a large tertiary care academic medical center. Minimal features were released initially in order to drive development according to patient and provider mandate. In fact, iHealthSpace was released only with the ability for patients to view their medications lists, order prescriptions, modify and reconcile their medication lists, view appointments, and read patient literature authored or vetted by the Primary Care Operations Improvement Group at the Massachusetts General Hospital.
Twelve providers and 500 patients were enrolled over the subsequent 55-month period. The “Copilot” program was deferred from this beta release. However, early feedback from staff and patients identified that family and friend caregivers, unclearly appointed, were creating accounts on the patient’s behalf with relative frequency.
In response to the number of reports coming “from the file” of couples attempting to use their shared emails and the adult children and relatives already creating iHealthSpace accounts on behalf of parents or other family members, the design and implementation of the initial version iHealthSpace “Copilot” program was expedited.
The iHealthSpace Copilot Program
The iHealthSpace Copilot program is designed to allow patients to grant caregivers access to their health record and to the services offered through iHealthSpace on their behalf. The program, in particular, allows certain caregivers either as “copilot” or activated health care proxies to explicitly create accounts on offline patient’s behalf. Given the complexity and attendant issues related to the care of children, scenarios involving minor patients are planned for a subsequent version of the Copilot Program.
Establishing a Caregiver: Scenarios
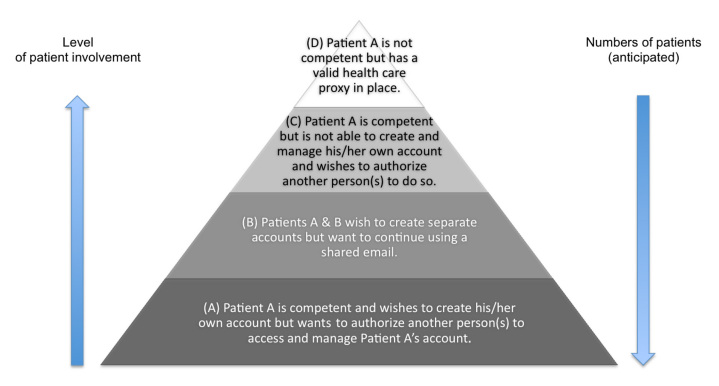
In the establishment of a caregiver relationship where both parties are adults, four scenarios were identified (see Figure 3 ). In the most common case, a patient is competent and wishes to create his/her own account, but wants to authorize another person(s) to access and manage the account. Second, two patients (typically a couple) wish to create separate accounts but want to continue using a shared email address. Third, the patient is competent but does not feel comfortable creating and managing his own account and wants to authorize another individual(s) to create, access, and manage the account on his/her behalf. Lastly, a patient is not competent but has a valid and clinically determined activated health care proxy who wants to create an account on the patient’s behalf.
Figure 3.
Caregiver scenarios.
Establishing a Caregiver: Due Process
In scenarios A and B, because the patient is actively involved and has an online presence that he or she controls, the establishment of caregiver relationships is also completely under the patient’s control. While the recommended practice is to keep separate email accounts, as some limited private information may pass through to the email, ultimately the decision of to whom and how many will reside with the patient. Scenario D, in contrast, enforces that only the legal and activated health care proxy, already assisting in medical decision-making, may have access to the patient’s records and, by extension, create an account on the patient’s behalf.
Scenario C depicts the key challenge in the Copilot program. In this scenario, the patient is competent, but is uncomfortable with using computers or the Internet on their own or may have other language, basic literacy, or numeracy barriers and wants someone else to create and manage an account. Behind the scenes, more likely, it is a family member who is comfortable with the Internet and may be providing a range of informal caregiving services, who wishes to create this account on the patient’s behalf. Practically, since the patient is not establishing an online presence of their own with which to directly control access to their health records, the only party remaining to steward the establishment of caregiver access is the practice. Information about the Copilot program is made available to all patients on customized visit intake forms. All patients have the opportunity to review a short set of frequently asked questions about the program and, if interested, to review and name a specific caregiver in a written agreement made with the practice. The patient may also request to review and sign the agreement verbally with a staff member. This agreement is retained by the practice in the patient’s records, and a scanned copy is saved in iHealthSpace on the patient’s behalf. Office staff are trained in the constituent elements of the program and are available to address attendant questions At this point, the Copilot program allows only patients who wish to share complete transparency with their caregiver to participate in the program; the ability to offer more limited access and identifying the component pieces of this access will be the basis of future work.
Tying In with the Caregiver Framework
The caregiver models just described suggest that caregiver relationships can be simple and unidirectional, reciprocal between two people (as in couples), shared among a group of family members and friends, and “chained” where a care recipient (e.g., a grandmother, may also function as a caregiver (e.g., for her grandchild). While the Copilot program can account for these models technically, there is a balance to be struck between the reality of patient life and the demands of provider care. From the provider standpoint, assigning a single person to act as caregiver is critical to ensuring a common portal of communication. Legally, particularly in scenario C, where the practice acts as steward, the organization’s interest is in limiting liability resulting from unexpected disclosure of private health information, the risks of which are assumed to increase with the number of people given primary access. Reconciling these differences remains a challenge.
Adapting these real-life scenarios led to the development of the following specific policies:
-
•
An iHealthSpace user may serve as Copilot for any number of patients.
-
•
Two or more iHealthSpace users may share an email address.
-
•
A pair of patients may elect each other to serve as copilot, as long as both are registered users, even if they share the same email address.
-
•
An iHealthSpace patient with his or her own account may invite any number of users to have copilot privileges. Patients are encouraged to limit this permission to those who are most closely involved in their care. All copilots will have read access, the ability to communicate with other caregivers, and the ability to send limited types of messages to the practice. At this juncture, copilots will have access to all parts of the patient’s iHealthSpace until a framework for more tightly refined access controls are established. For offline patients who wish to make a more limited set of services available to caregivers, further work will involve identifying this feature set.
-
•
A patient without his/her own online presence may designate only one person to have copilot privileges. The system will allow for more copilots as this becomes necessary in the future and once more limited types of-copilot relationship can be established. At that time, one primary copilot will be designated by the patient and will serve as the patient’s primary online caregiver.
-
•
Copilot status may be revoked or changed by the patient at any time, by verbal or written request to the practice. Online patients will be able to remove and update privileges through their iHealthSpace account.
-
•
Online patients will be able to audit caregiver activity from their iHealthSpace account. Offline patients may at any time request this information from the practice on paper and may be provided with this information automatically at the time of their visits.
Applications in Diabetes Care
Diabetes provides an ideal target domain to study the caregiver role. National surveillance has demonstrated improvements in overall glycemic control among Americans,15 but diabetes prevalence has continued to rise since the 1990s, and now affects approximately 7.8% (>23 million) of the U.S. population.14,16Another 57 million people have prediabetes—blood glucose levels that are higher than normal, but not yet high enough to be diagnosed as diabetes. Prediabetes, diabetes, and diabetes-related health complications,14,17,18 such as high blood pressure, heart disease, hyperlipidemia, and obesity, are all subject to prevention and improvement with lifestyle modifications, such as healthy eating, weight loss, tobacco cessation, and staying active. Patients diagnosed with diabetes are additionally burdened with many day-to-day responsibilities such as taking multiple medications and monitoring blood glucose—all tasks in which the assistance of family and other caregivers can be critical. In particular, diabetes imposes a substantial burden on elderly individuals and their families, both through increased rates of disability and the significant time that informal caregivers must spend helping address the associated functional limitations.
Example 1: ACCORD: Shared Care Plans
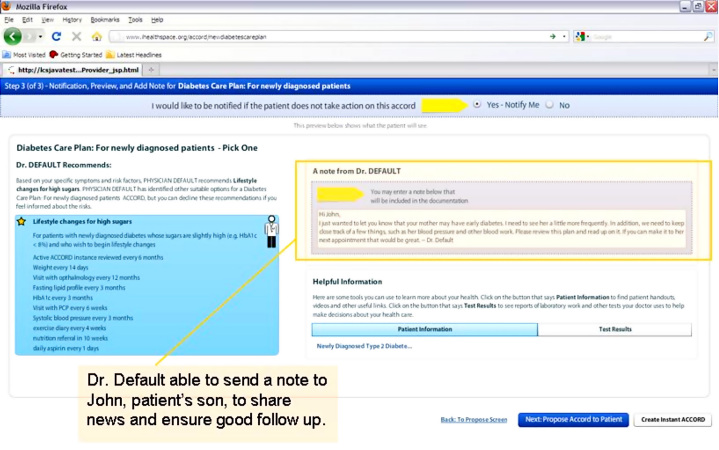
ACCORD (Ambulatory Care Compact to Organize Risk and Decision-making) is a Web application funded by the Agency of Healthcare Research and Quality that enables patients and primary care providers to review and explicitly share care plans that incorporate patient and provider preferences. Offered through iHealthSpace, ACCORD allows patients and their caregivers to view options for preventive health care as well as for chronic disease management, like diabetes. Figure 4 shows a screenshot from the ACCORD application with a message from the provider to the patient’s son (designated through iHealthSpace).
Figure 4.
A screenshot from the ACCORD application.
Example 2: Shared Visit Agenda
The shared visit agenda in iHealthSpace allows patients, caregivers, and clinical staff to coauthor a list of items that they wish to introduce during any upcoming visit. Available to providers through their visit notes and through their schedule, it allows caregivers the opportunity to make sure that certain issues rise to the provider’s attention at the right time even when they are not present at the actual visit. Items such as a “Mom’s blood sugar has been out of control since her last visit with you, usually 20–250 in the morning” allows the caregivers to share important updates with the care team that might otherwise be left on a message pad, buried in an email, or not communicated at all. Conversely, the shared visit agenda allows the provider to enlist the support of caregivers if needed, e.g. “Follow up on cholesterol: Please have Mom arrive for her visit after a 7–8 h fast so we can check her cholesterol levels,” or “Follow up on blood glucose: Bring in her blood sugar logs for the last month.”
ACCORD and the shared visit agenda are examples of next generation applications that explicitly engage patients in the care process. These and other community applications to be offered through iHealthSpace present the opportunity to access and support patients who would otherwise not be online, to augment interventions directed towards online patients with the support of their caregivers, and to direct resources and training to caregivers themselves. We anticipate that the explicit participation of caregivers has the potential to improve qualitative outcomes (patient, caregiver, and provider satisfaction) and quantitative outcomes at the patient level (e.g., improved control of hemoglobin A1c, blood pressure, or weight, and reduce emergency room visits or hospitalizations for complications of diabetes), as well as at the caregiver level (e.g., improvement in depression scales). We expect that the benefits accrued to patients who would not otherwise be online will be clear but are particularly interested in learning what, if any, additive benefit there will be for those who are already online.
Discussion
We anticipate that systems that are informed by a broader understanding of the reality of caregiving will offer greater opportunities for appropriate intervention than has been possible previously.13 However, as it has become clear, the nature of caregiving is variegated. Providing caregivers access to personal, private health information and the power to communicate with the practice on patient’s behalf, while natural in many circumstances, may be very problematic in others. These risks are less worrisome, though not trivial, in cases where the online patient (or activated health care proxy) is alerted in real time to changes in their online milieu. The risks become greater when the patient is the offline partner in a copilot relationship. The patient may not fully comprehend that all his health information may be made available to the caregiver for a variety of reasons and may inappropriately assign copilot privileges where much less is actually required: because of inattention or simple misunderstanding of a competent patient, because the patient may have limited literacy and be afraid to ask appropriate questions about the process, or because of staff misjudgment of the patient’s capacity to make such decisions in the first place. In all cases, the inability to directly “police” their space only reinforces their incomplete or hazy understanding of the process. We anticipate that offering differing levels of copilot support will ameliorate some of the risk, but ultimately, the appropriate assignation of a copilot will require continued education of patients and staff and ongoing needs assessment of this population.
We believe the iHealthSpace Copilot program represents a first step toward including a more broadly based and comprehensive definition of family caregiver. Expansion of the Copilot program to titrate the level of sharing and include multiple caregivers would allow us to reach out to a more diverse population of caregivers and “formalize” their important role in health care. This would permit the study of research questions that help us to at least enumerate and understand multiple caregivers, shifting and shared caregiving roles, and care recipients as caregivers and their differential impact on both caregiver and care recipient outcomes. Ultimately, this would enable the development and study of interventions that acknowledge and are responsive to the real experiences of family caregiving.
Abbreviations
- ACCORD
Ambulatory Care Compact to Organize Risk and Decisionmaking
- IOM
Institute of Medicine
References:
- 1.AARP Public Policy Institute. Chronic care: a call to action for health reform. Washington DC: AARP; 2009. p. 5. [Google Scholar]
- 2.National Alliance for Caregiving in collaboration with AARP. Caregiving in the United States. November 2009.
- 3.Institute of Medicine, Board on Health Care Services. Retooling for an aging America: building the health care workforce [report brief] Washington (DC): National Academies Press; 2008. [PubMed] [Google Scholar]
- 4.Institute of Medicine, Board on Health Care Services. Retooling for an aging America: building the health care workforce [report] Washington (DC): National Academies Press; 2008. [PubMed] [Google Scholar]
- 5.Levine C, Halper D, Peist A, Gould DA. Bridging troubled waters: family caregivers, transitions, and long-term care. Health Aff (Millwood) 2010;29(1):116–124. doi: 10.1377/hlthaff.2009.0520. [DOI] [PubMed] [Google Scholar]
- 6.Weiler DM, Crist JD. Diabetes self-management in a Latino social environment. Diabetes Educ. 2009;35(2):285–292. doi: 10.1177/0145721708329545. [DOI] [PubMed] [Google Scholar]
- 7.Finucane ML, McMullen CK. Making diabetes self-management education culturally relevant for Filipino Americans in Hawaii. Diabetes Educ. 2008;34(5):841–853. doi: 10.1177/0145721708323098. [DOI] [PubMed] [Google Scholar]
- 8.Okura T, Heisler M, Langa KM. Association between cognitive function and social support with glycemic control in adults with diabetes mellitus. J Am Geriatr Soc. 2009;57(10):1816–1824. doi: 10.1111/j.1532-5415.2009.02431.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dunbar SB, Clark PC, Deaton C, Smith AL, De AK, O’Brien MC. Family education and support interventions in heart failure: a pilot study. Nurs Res. 2005;54(3):158–166. doi: 10.1097/00006199-200505000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Lyons KS, Zarit SH, Sayer AG, Whitlatch CJ. Caregiving as a dyadic process: perspectives from caregiver and receiver. J Gerontol B Psychol Sci Soc Sci. 2002;57(3):P195–P204. doi: 10.1093/geronb/57.3.p195. [DOI] [PubMed] [Google Scholar]
- 11.Keith C. Family caregiving systems: models, resources, and values. J Marriage Family. 1995;57:179–189. [Google Scholar]
- 12.Feld S, Dunkle RE, Schroepfer T, Shen HW. Expansion of elderly couples’ IADL caregiver networks beyond the marital dyad. Int J Aging Hum Dev. 2006;63(2):95–113. doi: 10.2190/CW8G-PB6B-NCGH-HT1M. [DOI] [PubMed] [Google Scholar]
- 13.Lingler JH, Sherwood PR, Crighton MH, Song M, Happ MB. Conceptual challenges in the study of caregiver-care recipient relationships. Nurs Res. 2008;57(5):367–372. doi: 10.1097/01.NNR.0000313499.99851.0c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. 2007 national diabetes fact sheet. http://www.cdc.gov/diabetes/pubs/estimates07.htm#1.
- 15.Hoerger TJ, Segel JE, Gregg EW, Saaddine JB. Is glycemic control improving in U.S. adults? Diabetes Care. 2008;31(1):81–86. doi: 10.2337/dc07-1572. [DOI] [PubMed] [Google Scholar]
- 16.Cowie CC, Rust KF, Byrd-Holt DD, Eberhardt MS, Flegal KM, Engelgau MM, Saydah SH, Williams DE, Geiss LS, Gregg EW. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health and Nutrition Examination Survey 1999-2002. Diabetes Care. 2006;29(6):1263–1268. doi: 10.2337/dc06-0062. [DOI] [PubMed] [Google Scholar]
- 17.Wexler DJ, Grant RW, Wittenberg E, Bosch JL, Cagliero E, Delahanty L, Blais MA, Meigs JB. Correlates of health-related quality of life in type 2 diabetes. Diabetalogia. 2006;49(7):1489–1497. doi: 10.1007/s00125-006-0249-9. [DOI] [PubMed] [Google Scholar]
- 18.Grant RW, Cagliero E, Murphy-Sheehy P, Singer DE, Nathan DM, Meigs JB. Comparison of hyperglycemia, hypertension, and hyper-cholesterolemia management in patients with type 2 diabetes. Am J Med. 2002;112(8):603–609. doi: 10.1016/s0002-9343(02)01103-8. [DOI] [PubMed] [Google Scholar]