Abstract
Background
New patient-centered information technologies are needed to address risks associated with health care transitions for adolescents and young adults with diabetes, including systems that support individual and structural impediments to self- and clinical-care.
Methods
We describe the personally controlled health record (PCHR) system platform and its key structural capabilities and assess its alignment with tenets of the chronic care model (CCM) and the social–behavioral and health care ecologies within which adolescents and young adults with diabetes mature.
Results
Configured as Web-based platforms, PCHRs can support a new class of patient-facing applications that serve as monitoring and support systems for adolescents navigating complex social, developmental, and health care transitions. The approach can enable supportive interventions tailored to individual patient needs to boost adherence, self-management, and monitoring.
Conclusions
The PCHR platform is a paradigm shift for the organization of health information systems and is consistent with the CCM and conceptualizations of patient- and family-centered care for diabetes. Advancing the approach augers well for improvement around health care transitions for youth and also requires that we address (i) structural barriers impacting diabetes care for maturing youth; (ii) challenges around health and technology literacy; (iii) privacy and confidentiality issues, including sharing of health information within family and institutional systems; and (iv) needs for evaluation around uptake, impacts, and outcomes.
Keywords: adherence, consumer informatics, diabetes, health information technology, patient medical record systems, personally controlled health records, self-management, transitions, type 1 diabetes
Introduction
Optimal diabetes management among youth requires regular, comprehensive behavioral monitoring coupled with timely and acceptable clinical and social support. Support is most successful when it involves multiple stakeholders—clinical care team, parents, peers, an engaged patient—all aligned in a developmentally appropriate treatment program.1–3 Key elements of this chronic care model (CCM)4,5 include the timely flow of information to patients and individualized targeting of clinical services. The coherence of this model is threatened as youth move from adolescence to adulthood and undertake social, developmental, and health care transitions. Fractured service and information systems pose problems for maturing youth who are changing social roles, living arrangements, and health care relationships. Risks for nonadherence and clinical and social complications are amplified when youth encounter and “fall through the cracks” of fragmented care environments.6 Onset or intensification of adolescent-patterned risk behaviors and shifting to adult internal medicine settings may reduce self-care and adherence. Risks can be ameliorated through readiness assessment, self-care training, transition planning, screening, and social support interventions.7–11 These strategies are underutilized in pediatric specialty care12 and are under-mined by the geographic mobility of this population.
In this article, we describe a model for using the personally controlled health record (PCHR) to improve patterns of clinical care and self-management of diabetes among adolescents. Our approach is predicated on the assumption that engaging diabetes-affected youth with a personally controlled, nomadic, and longitudinal health record ameliorates care and reduces complications by improving the continuity of health information, coherence of care delivery, timeliness, and accessibility of clinical and social supports. We describe the IndIvoTM PCHR and its configuration as a platformthat supports third-party applications. Applications can be designed that are particularly appropriate for use by adolescents throughout transitions and that are suitable to the rapidly evolving health information system ecosystem.
Personally Controlled Health Record
The PCHRs are a special category of personal health record (PHR),13 a much discussed technology that is the focus of considerable policy and market sector activity intensifying under the Health Information Technology for Economic and Clinical Health (HITECH) Act.14 The PCHR model is for a digital Web-based collection of a patient’s comprehensive medical history: copies of medical records, reports about diagnosed medical conditions, medications, vital signs, immunizations, laboratory results, and personal characteristics. The PCHR design integrates medical and social information across sites of care and over time within a structure that is readily accessible to and controlled by individuals,15 a feature that distinguishes them from PHRs.16 User control is governed by subscription and access control mechanisms and annotation capabilities.17 The emphasis on individual control within the PCHR may help overcome barriers to information flow across institutional borders and foster patient buy-in, engagement, and long-term commitment. Increasing individuals’ abilities to view and share medical histories and clinical decision support messages is assumed to result in better self-care, reductions in treatment and medication errors, and improved health.18–21 The PCHR can support real-time data exchange with clinical and social supports via a patient-controlled sharing feature, enabling shared views and decision making with providers and peers/social supports. Such a feature may be particularly helpful in supporting youth who are making transitions, whose clinical and social supports may be geographically remote. Among early adopters of PCHR systems, high levels of support have been observed for sharing personal health information through a PCHR platform for care improvement or research purposes, including among young adults who are the target group for health care transitions.22,23
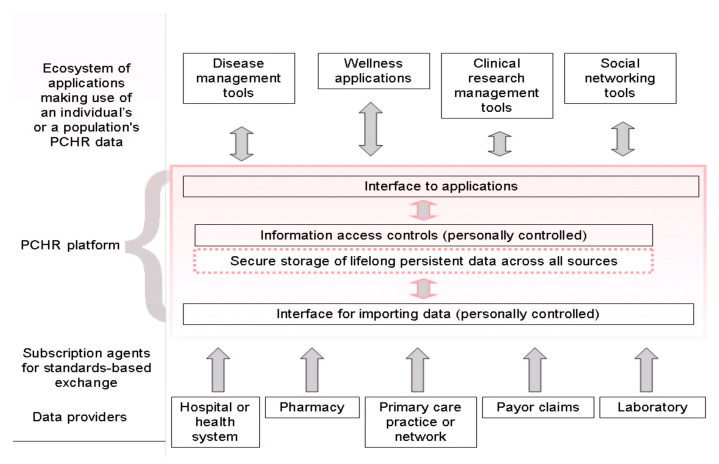
The PCHR development at Children’s Hospital Boston has resulted in the open-source IndIvo PCHR, designed to serve as a lifelong record to promote patient engagement and activation in disease management, communication with clinicians, and shared decision making, factors that may improve transitions, adherence, and health (see Figure 1 ).24 IndIvo leverages the individual’s right to a copy of his or her record, making it possible to generate a persistent longitudinal medical record that would outlast the relationship that each patient has with a particular provider or health care system. Through a series of meetings (www.pchri.org/2006/ and www.pchri.org/2007/), the IndIvo model was diffused. It was adopted by Microsoft, who launched HealthVault containing IndIvo software code; Google, who reimplemented the model as the GoogleHealth Model; and Dossia, a consortium of large employers (including Walmart, AT&T, and Intel), who contracted with Children’s Boston to deploy IndIvo to their employees.
Figure 1.
The INDIVO PCHR platform model that includes interfaces to applications and subscription data sources.
The HITECH Act contains provisions entitling patients to electronic copies of their vital medical records and allowing them to have the records exported from electronic health records to a PCHR of their choice—these provisions will promote substantial data liquidity and enable integration of an individual’s information over time and across sites of care. IndIvo records and toolkits are controlled by patients and families who grant permissions to clinicians, researchers, and institutions.15
In recognition of the rapidly evolving health information ecosystem in which PCHR value is likely to be applications oriented, PCHRs are developed as Web-basedcommunications and service platforms.25 The platform model layers onto the core system third-party applications and tools relevant to cohort and intervention studies, care improvement, and public health efforts. We have likened this model to the success of the iPhone platform, which currently supports over 200,000 applications developed by third parties.26 Configured as such, PCHRs can enable development, by us and others, of supportive interventions tailored to individual patient needs to boost adherence and self-management.
We propose leveraging the PCHR platform approach to foster safer transitions among youth with diabetes by addressing problems related to fragmentation of health information, through
-
•
engaging youth with their health information to foster early and improved self-management and self-care, health literacy, and shared decision making;
-
•
integrating diabetes care medical records with other health and medical records to support comprehensive care, tracking, and attention to adherence, treatment side effects, comorbidities, care processes, and behavioral and lifestyle patterns; and
-
•
supporting applications, communication with social and clinical supports, and connection with research.
The comparison of the traditional health record model and the patient-centered PCHR model is summarized in Table 1 .
Table 1.
Standard and Personally Controlled Health Record Platform Approaches to Health Record
| Domain | Standard health record approach | PCHR platform approach |
|---|---|---|
| “Owner” of record | Provider, organization | Patient |
| Record access | Through authority (provider) | Through patient |
| Data system | Somewhat inflexible | Highly flexible |
| Data model | Vertical by disease, problem | Relational across diseases, problems |
| Record integration | Fragmented across settings | Integrated across settings |
| Institutional relationship | Tethered to a specific care setting, intermediated through provider or care environment | Institutionally tethered through subscription and server storage but may be disintermediated |
| Authentication | Institutional identify | PCHR based |
| Friendly to services, applications | No | Yes, contingent on access, consent, standards |
| Research friendly | Historically not, typically narrow, purpose-driven around care monitoring | Emerging models for engaging cohorts, can support broad investigations |
Affording Opportunities to Monitor Health Risk Behaviors and Psychosocial Problems for Improved Care
Psychosocial stressors and health risk behaviors worsen the potentially adverse effects of poorly managed transitions.27,28 Empowerment of diabetes-affected youth, their families, and the clinicians who care for them to detect and protect against these risks is limited by gaps in behavioral reporting/screening during older adolescence/emergent adulthood, poor communication, and discontinuities in care and insurance.7,29–31 The PCHR survey module can support “real-time” structured and semistructured self-reporting about these factors, with the option to share information with clinical and social supports through the PCHR sharing feature. Collection and storage in PCHRs of data about health risk behaviors and psychosocial status for self-review and sharing with clinical and social supports may ameliorate gaps and improve detection, care, and prevention. The model of long-term multistakeholder monitoring may be especially important given findings that substantial periods of monitoring and “good” glycemic control are necessary to minimize the risks for complications.32 This model has not yet been tested.
Aligning the Personally Controlled Health Record Platform Model with an Evolving Chronic Care Model
The PCHR platform approach is grounded in a conceptualization of the CCM that is centered on effective use of patient-centered health information technology (HIT). Use of a PCHR platform to bridge care environments and support self-care tracking reflects key aspects of the CCM,5,33,34including (a) patient- and family-centered care, (b) improved communication, (c) central access to the patient’s health record, and (d) information support leading to (e) a proactive care team and (f) the development of explicit care plans. This interaction of an activated patient with a proactive, integrated health care team is designed to achieve optimal outcomes.35–37 The CCM has been validated in adult patients with chronic illnesses such as diabetes mellitus, congestive heart failure, depression, asthma, and chronic lung disease.38–40 Our effort focuses on supporting diabetes self-management through effective use of HIT—specifically the PCHR platform—and adoption/application of a systems view of health care services and behavior.41
Health information technology is integral to the CCM. It is estimated that successful implementations of HIT have yielded total cost savings of over $150 billion.42 A review of 109 studies of HIT systems for improving chronic illness care found positive associations between HIT and process measures of care, including guideline adherence, documentation quality, and treatment adherence; a mixed pattern was seen for care outcomes.43 Particularly important to positive outcomes were applications that connected to electronic medical records or provided users with population health reports and feedback. With respect to diabetes, the acceptability to type 1 diabetes mellitus (T1DM)-affected youth of HIT tools for tracking health status and encouraging positive health behavior is suggested by process studies of glucose monitoring, but a mixed pattern for impact on physiological outcomes has been observed. Home-based telehealth interventions show promise in improving adolescent adherence to T1DM treatment when parents are involved.44 Provision of motivational interviewing for glycemic control via telehealth channels is being assessed in trials and shows promise in case reports when peers are involved.45 Feasibility of collecting blood glucose and data on health behaviors for T1DM management using a mobile phone system that supports shared views by patients and supporting physicians has been demonstrated.46 Telehealth communications interventions improved adolescent self-efficacy over a 1-year trial but did not improve glycemic control.47
Benefits of HIT for diabetes appear conditional on the role of social ties and patient engagement with peers to achieve improved disease management. Process measures generally improve with HIT, but physiological outcomes generally have not.48–50 It is unclear whether this is because interventions provide insufficient timeliness, targeting, salience, or personalization—dimensions with potential to improve in the PCHR platform. Evaluation of the effects of engaging youth with their own health information and connecting them to clinically oriented and community-facing support systems represents an important opportunity for advancing outcomes-oriented research.
Discussion
Achieving planned, safe, and appropriate health care transitions for maturing youth with diabetes is a critical issue and, as of yet, an unmet goal.12 Nationally, only 6% of youth with special care needs achieve conditions for transitioning to adult life—health care, work, and independence.51 Half of older youth with special care needs report that they have discussed care transitions with pediatric subspecialists. Of these, less than two-thirds have discussed a transition plan and only two-fifths have discussed adult care.52 This picture applies to the growing number of youth with T1DM and other chronically ill youth.53
One-third (31%) of adolescents with T1DM making health care transitions report 6-month gaps in care between a first adult and last pediatric visit, while 11% are lost to follow-up.30 Adherence to recommended care processes and improved glycemic control can be achieved through intensive clinical management of diabetes,54 including when tailored, targeted care is delivered by a nurse educator or case manager.55–58
Problems related to health care transitions among youth with diabetes persist despite shared concern about transitions among clinicians, patients, and families and despite broad stroke agreement about requirements for effective care transitions: timely and thorough preparation, readiness assessment, care planning, referrals, information transfer, monitoring, and follow-up.1,53,59,60 These service factors and approaches have been integrated effectively with adults61–63 and may be especially important for low-socioeconomic-status youth.64 Bioinformatics tools that engage youth and young adults with their health information and that enable real-time reporting, assess-ment and layering of applications as part of information management may support comprehensive care and motivate engagement. This may be an especially fitting strategy for ameliorating risks related to health care transitions.
Use of the PCHR and associated applications layered onto a PCHR platform comprises a paradigm shift for the organization of health information systems, but one that is consistent with the tenets of the CCM and with conceptualizations of patient- and family-centered care for diabetes-affected youth.2,3,10,65,66 Such an approach, while important, is unlikely to be a panacea. A comprehensive strategy needs to be in place that addresses the following challenges and opportunities:
-
•
The sociology of diabetes care and structural barriers impacting its effective use by adolescents and emergent adults . Many factors are associated with poor health care transitions: cultural and organizational differences between pediatric and adult services that inhibit and delay effective transfer of patients, discontinuities in information systems that impede care coordination and continuity,30,60 poor communications and planning between providers/patients that create missed opportunities to prepare maturing youth and their families for transitions,67 and gaps in insurance coverage.68–71 Systemic improvements may be necessary and “nudged” along72by the PCHR.
-
•
Challenges around health and technology literacy . Greater access to and control by youth of their health records and health information may foster improved activation in health promotion and disease management; however, the demands on youth and their social and clinical supports to better understand health information and make effective use of it may be steep. Planning and resource allocation for technical assistance and support in this area will be especially important to ensure we activate and not abandon patients. While health literacy demands may be high, technology barriers for youth are likely to be low given secular trends in technology adoption.
-
•
Effective management and education around privacy and confidentiality issues . To optimize engagement with these systems, solutions to privacy and confidentiality issues need to be worked out that satisfactorily map conventions for transitioning from parental to patient control of health information.73 Adapting to the PCHR platform rules andconventions for sharing information and controlling health records will require attention, education, and oversight as these systems diffuse. Ultimately, patient control over access and sharing may best suit the complexity of social relationships and family configurations, allowing case-by-case flexibility.
-
•
Maturation and value within the emerging marketplace of applications that dock to a PCHR. Success of the PCHR may be in the platform model that extends the value of the longitudinal record with applications, device connectivity, and services. Traction in these areas will be guaranteed by evidence of effectiveness and alignment with standards of care and maturing toward a rich ecosystem of applications and services that inter-operate with the PCHR. As part of this, tools are needed that offer comprehensive, developmentally appropriate support for youth facing social, development, and health care transitions so they may more effectively manage their disease and avoid problems.41,74
-
•
Evidence of safety and effectiveness . Demonstration evaluation that provides evidence of the broad applicability and benefits of the PCHR approach is needed, including for ameliorating care and reducing problems across the spectrum of at-risk groups, diabetes types, ages, and patient profiles.
Conclusion
Overall, whether HIT-based approaches for diabetes are effective and sustainable and can address behavioral cofactors of self-care, including health risk behaviors, remains underexplored. The HIT-based approaches for disease management and health communications appear generally acceptable to young patients, consistent with societal norms and trends. We hypothesize that the PCHR platform model can bridge stakeholders and information systems to support clinical- and self-care during a vulnerable period when many youth migrate away from the oversight and influence of clinicians and families. Availability of a shared and portable patient-controlled record could unify information shared among clinicians and augment available information by capitalizing on tools for self-reporting and monitoring. This may create crucial opportunities for improved early detection and response to nonadherence, risk behaviors, and/or psychosocial problems from proximal or distal supports.
Engaging adolescents with a PCHR platform may improve self-monitoring and clinical monitoring and management of diabetes in a fashion that is developmentally and technologically relevant. The IndIvo PCHR, a maturing patient-centered open-source information system being refined for this purpose, is poised for evaluation and diffusion. Configured as a platform, IndIvo may support applications that address needs of a high-risk group through an approach that is sociologically and techno-logically appropriate, including to national objectives of strengthening patient-centered health information technologies.14
Abbreviations
- CCR
chronic care model
- HIT
health information technology
- HITECH
Health Information Technology for Economic and Clinical Health
- PCHR
personally controlled health record
- PHR
personal health record
- T1DM
type 1 diabetes mellitus
References:
- 1.Kelly AM, Kratz B, Bielski M, Rinehart PM. Implementing transitions for youth with complex chronic conditions using the medical home model. Pediatrics. 2002;110(6 Pt 2):1322–1327. [PubMed] [Google Scholar]
- 2.Anderson B, Ho J, Brackett J, Finkelstein D, Laffel L. Parental involvement in diabetes management tasks: relationships to blood glucose monitoring adherence and metabolic control in young adolescents with insulin-dependent diabetes mellitus. J Pediatr. 1997;130(2):257–265. doi: 10.1016/s0022-3476(97)70352-4. [DOI] [PubMed] [Google Scholar]
- 3.Wysocki T, Nansel TR, Holmbeck GN, Chen R, Laffel L, Anderson BJ, Weissberg-Benchell J, Steering Committee of the Family Management of Childhood Diabetes Study Collaborative involvement of primary and secondary caregivers: associations with youths’ diabetes outcomes. J Pediatr Psychol. 2009;34(8):869–881. doi: 10.1093/jpepsy/jsn136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the chronic care model in the new millennium. Health Aff (Millwood) 2009;28(1):75–85. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1(1):2–4. [PubMed] [Google Scholar]
- 6.Grant RW, Meigs JB. Overcoming barriers to evidence-based diabetes care. Curr Diabetes Rev. 2006;2(2):261–269. doi: 10.2174/157339906776818604. [DOI] [PubMed] [Google Scholar]
- 7.Cameron FJ, Northam EA, Ambler GR, Daneman D. Routine psychological screening in youth with type 1 diabetes and their parents: a notion whose time has come? Diabetes Care. 2007;30(10):2716–2724. doi: 10.2337/dc07-0603. [DOI] [PubMed] [Google Scholar]
- 8.Northam EA, Todd S, Cameron FJ. Interventions to promote optimal health outcomes in children with type 1 diabetes–are they effective? Diabet Med. 2006;23(2):113–121. doi: 10.1111/j.1464-5491.2005.01678.x. [DOI] [PubMed] [Google Scholar]
- 9.American Academy of Pediatrics Committee on Children with Disabilities and Committee on Adolescence. Transition of care provided for adolescents with special health care needs. Pediatrics. 1996;98(6 Pt 1):1203–1206. [PubMed] [Google Scholar]
- 10.Wysocki T. Behavioral assessment and intervention in pediatric diabetes. Behav Modif. 2006;30(1):72–92. doi: 10.1177/0145445505284275. [DOI] [PubMed] [Google Scholar]
- 11.Martin S, Pawlowski B, Greulich B, Ziegler AG, Mandrup-Poulsen T, Mahon J. Natural course of remission in IDDM during 1st yr after diagnosis. Diabetes Care. 1992;15(1):66–74. doi: 10.2337/diacare.15.1.66. [DOI] [PubMed] [Google Scholar]
- 12.Bates K, Bartoshesky L, Friedland A. As the child with chronic disease grows up: transitioning adolescents with special health care needs to adult-centered health care. Del Med J. 2003;75(6):217–220. [PubMed] [Google Scholar]
- 13.Halamka JD, Mandl KD, Tang PC. Early experiences with personal health records. J Am Med Inform Assoc. 2008;15(1):1–7. doi: 10.1197/jamia.M2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Public Law: Recovery Act Health Information Technology for Economic and Clinical Health. 2009. http://www.hhs.gov/recovery/reports/plans/onc_hit.pdf. Accessed September 24, 2010.
- 15.Mandl KD, Simons WW, Crawford WC, Abbett JM. IndIvo: a personally controlled health record for health information exchange and communication. BMC Med Inform Decis Mak. 2007;7:25. doi: 10.1186/1472-6947-7-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13(2):121–126. doi: 10.1197/jamia.M2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mandl KD, Szolovits P, Kohane IS. Public standards and patients’ control: how to keep electronic medical records accessible but private. BMJ. 2001;322(7281):283–287. doi: 10.1136/bmj.322.7281.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.D’Alessandro DM, Dosa NP. Empowering children and families with information technology. Arch Pediatr Adolesc Med. 2001;155(10):1131–1136. doi: 10.1001/archpedi.155.10.1131. [DOI] [PubMed] [Google Scholar]
- 19.Poon EG, Wald J, Schnipper JL, Grant R, Gandhi TK, Volk LA, Bloom A, Williams DH, Gardner K, Epstein M, Nelson L, Businger A, Li Q, Bates DW, Middleton B. Empowering patients to improve the quality of their care: design and implementation of a shared health maintenance module in a US integrated healthcare delivery network. Stud Health Technol Inform. 2007;129(Pt 2):1002–1006. [PubMed] [Google Scholar]
- 20.Detmer D, Bloomrosen M, Raymond B, Tang P. Integrated personal health records: transformative tools for consumer-centric care. BMC Med Inform Decis Mak. 2008;8:45. doi: 10.1186/1472-6947-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bourgeois FT, Simons WW, Olson K, Brownstein JS, Mandl KD. Evaluation of influenza prevention in the workplace using a personally controlled health record: randomized controlled trial. J Med Internet Res. 2008;10(1):e5. doi: 10.2196/jmir.984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weitzman ER, Kaci L, Mandl KD. Sharing medical data for health research: the early personal health record experience. J Med Internet Res. 2010;12(2):e14. doi: 10.2196/jmir.1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weitzman ER, Kaci L, Mandl KD. Acceptability of a personally controlled health record in a community-based setting: implications for policy and design. J Med Internet Res. 2009;11(2):e14. doi: 10.2196/jmir.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clay D, Farris K, McCarthy AM, Kelly MW, Howarth R. Family perceptions of medication administration at school: errors, risk factors, and consequences. J Sch Nurs. 2008;24(2):95–102. doi: 10.1177/10598405080240020801. [DOI] [PubMed] [Google Scholar]
- 25.Mandl KD, Kohane IS. Tectonic shifts in the health information economy. N Engl J Med. 2008;358(16):1732–1737. doi: 10.1056/NEJMsb0800220. [DOI] [PubMed] [Google Scholar]
- 26.Mandl KD, Kohane IS. No small change for the health information economy. N Engl J Med. 2009;360(13):1278–1281. doi: 10.1056/NEJMp0900411. [DOI] [PubMed] [Google Scholar]
- 27.Bryden KS, Peveler RC, Stein A, Neil A, Mayou RA, Dunger DB. Clinical and psychological course of diabetes from adolescence to young adulthood: a longitudinal cohort study. Diabetes Care. 2001;24(9):1536–1540. doi: 10.2337/diacare.24.9.1536. [DOI] [PubMed] [Google Scholar]
- 28.Bryden KS, Neil A, Mayou RA, Peveler RC, Fairburn CG, Dunger DB. Eating habits, body weight, and insulin misuse. A longitudinal study of teenagers and young adults with type 1 diabetes. Diabetes Care. 1999;22(12):1956–1960. doi: 10.2337/diacare.22.12.1956. [DOI] [PubMed] [Google Scholar]
- 29.Silverstein J, Klingensmith G, Copeland K, Plotnick L, Kaufman F, Laffel L, Deeb L, Grey M, Anderson B, Holzmeister LA, Clark N, American Diabetes Association Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care. 2005;28(1):186–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- 30.Weissberg-Benchell J, Wolpert H, Anderson BJ. Transitioning from pediatric to adult care: a new approach to the post-adolescent young person with type 1 diabetes. Diabetes Care. 2007;30(10):2441–2446. doi: 10.2337/dc07-1249. [DOI] [PubMed] [Google Scholar]
- 31.McGill M. How do we organize smooth, effective transfer from paediatric to adult diabetes care? Horm Res. 2002;57(Suppl 1):66–68. doi: 10.1159/000053316. [DOI] [PubMed] [Google Scholar]
- 32.Writing Team for the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Sustained effect of intensive treatment of type 1 diabetes mellitus on development and progression of diabetic nephropathy: the Epidemiology of Diabetes Interventions and Complications (EDIC) study. JAMA. 2003;290(16):2159–2167. doi: 10.1001/jama.290.16.2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Légaré F, Elwyn G, Fishbein M, Frémont P, Frosch D, Gagnon MP, Kenny DA, Labrecque M, Stacey D, St-Jacques S, van der Weijden T. Translating shared decision-making into health care clinical practices: proof of concepts. Implement Sci. 2008;3:2. doi: 10.1186/1748-5908-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Légaré F, Stacey D, Graham ID, Elwyn G, Pluye P, Gagnon MP, Frosch D, Harrison MB, Kryworuchko J, Pouliot S, Desroches S. Advancing theories, models and measurement for an inter-professional approach to shared decision making in primary care: a study protocol. BMC Health Serv Res. 2008;8:2. doi: 10.1186/1472-6963-8-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.American Academy of Pediatrics Council on Children with Disabilities. Care coordination in the medical home: integrating health and related systems of care for children with special health care needs. Pediatrics. 2005;116(5):1238–1244. doi: 10.1542/peds.2005-2070. [DOI] [PubMed] [Google Scholar]
- 36.Adams K, Greiner AC, Corrigan JM. Committee on the Crossing the Quality Chasm: Next Steps Toward a New Health Care System. 1st annual crossing the quality chasm summit: a focus on communities; Washington DC: Institute of Medicine; 2004. [PubMed] [Google Scholar]
- 37.Healthways. Improving care coordination through physician/disease management collaboration. Ft. Lauderdale: Johns Hopkins University; 2005. [Google Scholar]
- 38.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 39.Adams SG, Smith PK, Allan PF, Anzueto A, Pugh JA, Cornell JE. Systematic review of the chronic care model in chronic obstructive pulmonary disease prevention and management. Arch Intern Med. 2007;167(6):551–561. doi: 10.1001/archinte.167.6.551. [DOI] [PubMed] [Google Scholar]
- 40.Tsai AC, Morton SC, Mangione CM, Keeler EB. A meta-analysis of interventions to improve care for chronic illnesses. Am J Manag Care. 2005;11(8):478–488. [PMC free article] [PubMed] [Google Scholar]
- 41.Glasgow RE, Hiss RG, Anderson RM, Friedman NM, Hayward RA, Marrero DG, Taylor CB, Vinicor F. Report of the health care delivery work group: behavioral research related to the establishment of a chronic disease model for diabetes care. Diabetes Care. 2001;24(1):124–130. doi: 10.2337/diacare.24.1.124. [DOI] [PubMed] [Google Scholar]
- 42.Hillestad R, Bigelow J, Bower A, Girosi F, Meili R, Scoville R, Taylor R. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff (Millwood) 2005;24(5):1103–1117. doi: 10.1377/hlthaff.24.5.1103. [DOI] [PubMed] [Google Scholar]
- 43.Dorr D, Bonner LM, Cohen AN, Shoai RS, Perrin R, Chaney E, Young AS. Informatics systems to promote improved care for chronic illness: a literature review. J Am Med Inform Assoc. 2007;14(2):156–163. doi: 10.1197/jamia.M2255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Adkins JW, Storch EA, Lewin AB, Williams L, Silverstein JH, Malasanos T, Geffken GR. Home-based behavioral health intervention: use of a telehealth model to address poor adherence to type-1 diabetes medical regimens. Telemed J E Health. 2006;12(3):370–372. doi: 10.1089/tmj.2006.12.370. [DOI] [PubMed] [Google Scholar]
- 45.Dale J, Caramlau I, Docherty A, Sturt J, Hearnshaw H. Telecare motivational interviewing for diabetes patient education and support: a randomised controlled trial based in primary care comparing nurse and peer supporter delivery. Trials. 2007;8:18. doi: 10.1186/1745-6215-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Farmer A, Gibson O, Hayton P, Bryden K, Dudley C, Neil A, Tarassenko L. A real-time, mobile phone-based telemedicine system to support young adults with type 1 diabetes. Inform Prim Care. 2005;13(3):171–177. doi: 10.14236/jhi.v13i3.594. [DOI] [PubMed] [Google Scholar]
- 47.Howells L, Wilson AC, Skinner TC, Newton R, Morris AD, Greene SA. A randomized control trial of the effect of negotiated telephone support on glycaemic control in young people with type 1 diabetes. Diabet Med. 2002;19(8):643–648. doi: 10.1046/j.1464-5491.2002.00791.x. [DOI] [PubMed] [Google Scholar]
- 48.McKay HG, King D, Eakin EG, Seeley JR, Glasgow RE. The diabetes network internet-based physical activity intervention: a randomized pilot study. Diabetes Care. 2001;24(8):1328–1334. doi: 10.2337/diacare.24.8.1328. [DOI] [PubMed] [Google Scholar]
- 49.Barrera M Jr, Glasgow RE, McKay HG, Boles SM, Feil EG. Do Internet-based support interventions change perceptions of social support?: An experimental trial of approaches for supporting diabetes self-management. Am J Community Psychol. 2002;30(5):637–654. doi: 10.1023/A:1016369114780. [DOI] [PubMed] [Google Scholar]
- 50.Jennings A, Powell J, Armstrong N, Sturt J, Dale J. A virtual clinic for diabetes self-management: pilot study. J Med Internet Res. 2009;11(1):e10. doi: 10.2196/jmir.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McPherson M, Weissman G, Strickland BB, van Dyck PC, Blumberg SJ, Newacheck PW. Implementing community-based systems of services for children and youths with special health care needs: how well are we doing? Pediatrics. 2004;113(5 Suppl):1538–1544. [PubMed] [Google Scholar]
- 52.Lotstein DS, McPherson M, Strickland B, Newacheck PW. Transition planning for youth with special health care needs: results from the National Survey of Children with Special Health Care Needs. Pediatrics. 2005;115(6):1562–1568. doi: 10.1542/peds.2004-1262. [DOI] [PubMed] [Google Scholar]
- 53.Callahan ST, Winitzer RF, Keenan P. Transition from pediatric to adult-oriented health care: a challenge for patients with chronic disease. Curr Opin Pediatr. 2001;13(4):310–316. doi: 10.1097/00008480-200108000-00004. [DOI] [PubMed] [Google Scholar]
- 54.The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 55.Ahern JA, Ramchandani N, Cooper J, Himmel A, Silver D, Tamborlane WV. Using a primary nurse manager to implement DCCT recommendations in a large pediatric program. Diabetes Educ. 2000;26(6):990–994. doi: 10.1177/014572170002600611. [DOI] [PubMed] [Google Scholar]
- 56.Howe CJ, Jawad AF, Tuttle AK, Moser JT, Preis C, Buzby M, Murphy KM. Education and telephone case management for children with type 1 diabetes: a randomized controlled trial. J Pediatr Nurs. 2005;20(2):83–95. doi: 10.1016/j.pedn.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 57.Babamoto KS, Sey KA, Camilleri AJ, Karlan VJ, Catalasan J, Morisky DE. Improving diabetes care and health measures among Hispanics using community health workers: results from a randomized controlled trial. Health Educ Behav. 2009;36(1):113–126. doi: 10.1177/1090198108325911. [DOI] [PubMed] [Google Scholar]
- 58.Loveman E, Royle P, Waugh N. Specialist nurses in diabetes mellitus. Cochrane Database Syst Rev. 2003;(2):CD003286. doi: 10.1002/14651858.CD003286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.American Academy of Pediatrics; American Academy of Family Physicians; American College of Physicians-American Society of Internal Medicine. A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110(6 Pt 2):1304–1306. [PubMed] [Google Scholar]
- 60.Reiss J, Gibson R. Health care transition: destinations unknown. Pediatrics. 2002;110(6 Pt 2):1307–1314. [PubMed] [Google Scholar]
- 61.Lawrence DB, Allison W, Chen JC, Demand M. Improving medication adherence with a targeted, technology-driven disease management intervention. Dis Manag. 2008;11(3):141–144. doi: 10.1089/dis.2007.0013. [DOI] [PubMed] [Google Scholar]
- 62.Wilhide C, Hayes JR, Farah JR. Impact of behavioral adherence on clinical improvement and functional status in a diabetes disease management program. Dis Manag. 2008;11(3):169–175. doi: 10.1089/dis.2007.0021. [DOI] [PubMed] [Google Scholar]
- 63.Zai AH, Grant RW, Estey G, Lester WT, Andrews CT, Yee R, Mort E, Chueh HC. Lessons from implementing a combined workflow-informatics system for diabetes management. J Am Med Inform Assoc. 2008;15(4):524–533. doi: 10.1197/jamia.M2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Goldman DP, Smith JP. Can patient self-management help explain the SES health gradient? Proc Natl Acad Sci U S A. 2002;99(16):10929–34. doi: 10.1073/pnas.162086599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Anderson BJ, Auslander WF, Jung KC, Miller JP, Santiago JV. Assessing family sharing of diabetes responsibilities. J Pediatr Psychol. 1990;15(4):477–492. doi: 10.1093/jpepsy/15.4.477. [DOI] [PubMed] [Google Scholar]
- 66.Anderson EB. Patient-centeredness: a new approach. Nephrol News Issues. 2002;16(12):80–82. [PubMed] [Google Scholar]
- 67.Mann MY, Lloyd-Puryear MA, Linzer D. Enhancing communication in the 21st century. Pediatrics. 2006;117(5 Pt 2):S315–S319. doi: 10.1542/peds.2005-2633K. [DOI] [PubMed] [Google Scholar]
- 68.Gregg EW, Karter AJ, Gerzoff RB, Safford M, Brown AF, Tseng CW, Waitzfielder B, Herman WH, Mangione CM, Selby JV, Thompson TJ, Dudley RA. Characteristics of insured patients with persistent gaps in diabetes care services: the Translating Research into Action for Diabetes (TRIAD) study. Med Care. 2010;48(1):31–37. doi: 10.1097/MLR.0b013e3181bd4783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lotstein DS, Inkelas M, Hays RD, Halfon N, Brook R. Access to care for youth with special health care needs in the transition to adulthood. J Adolesc Health. 2008;43(1):23–29. doi: 10.1016/j.jadohealth.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 70.Callahan ST. Bridging the gaps in health insurance coverage for young adults. J Adolesc Health. 2007;41(4):321–322. doi: 10.1016/j.jadohealth.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 71.Callahan ST, Cooper WO. Continuity of health insurance coverage among young adults with disabilities. Pediatrics. 2007;119(6):1175–1180. doi: 10.1542/peds.2006-1881. [DOI] [PubMed] [Google Scholar]
- 72.Christensen CM, Grossman JH, Hwang J. The innovator’s prescription: a disruptive solution for health care. New York: McGraw-Hill; 2008. [Google Scholar]
- 73.Bourgeois FC, Taylor PL, Emans SJ, Nigrin DJ, Mandl KD. Whose personal control? Creating private, personally controlled health records for pediatric and adolescent patients. J Am Med Inform Assoc. 2008;15(6):737–743. doi: 10.1197/jamia.M2865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Anderson BJ, Wolpert HA. A developmental perspective on the challenges of diabetes education and care during the young adult period. Patient Educ Couns. 2004;53(3):347–352. doi: 10.1016/j.pec.2003.03.001. [DOI] [PubMed] [Google Scholar]