Abstract
OBJECTIVE
To characterize the trends, distribution, potential determinants, and public health implications of meat consumption within the United States.
DESIGN
We examined temporal trends in meat consumption using food availability data from the Food and Agricultural Organization (FAO) and United States Department of Agriculture (USDA); and further evaluated meat intake by type (red, white, processed) in the National Health and Nutrition Examination Surveys (NHANES) linked to the MyPyramid Equivalents Database (MPED).
RESULTS
Overall meat consumption has continued to rise in the U.S., European Union, and developed world. Despite a shift toward higher poultry consumption, red meat still represents the largest proportion of meat consumed in the U.S (58%). Twenty-two percent of the meat consumed in the U.S. is processed. According to NHANES 2003–2004, total meat intake averaged 128 g/day. The type and quantities of meat reported varied by education, race, age, and gender.
CONCLUSIONS
Given the plausible epidemiologic evidence for red and processed meat intake in cancer and chronic disease risk, understanding the trends and determinants of meat consumption in the U.S., where meat is consumed at more than three times the global average, should be particularly pertinent to researchers and other public health professionals aiming to reduce the global burden of chronic disease.
Keywords: red meat, poultry, processed meat, U.S. diet, chronic disease
INTRODUCTION
Meat intake varies widely throughout the world. In the U.S. and other developed countries, meat composes a significant portion of the normal diet, contributing more than 15% to daily energy intake, 40% to daily protein intake, and 20% to daily fat intake(1–3). The demand for meat in developing countries continues to grow as the production and consumption of meat increases with available income(4, 5). A shift toward a dietary pattern characterized by high meat consumption also appears to supplant the consumption of cereals and other foods of plant origin(1, 6, 7).
Early ecologic comparisons provided the first indication that high meat consumption correlated with higher rates of chronic disease(8, 9), including cardiovascular disease (CVD) and cancer, the current leading causes of morbidity and mortality in the U.S. and other westernized countries(10). Health risks associated with meat consumption vary based on the animal the meat is derived from, as well as rearing, processing, and preparation methods. Meat can be further classified as red meat or white meat by the quantity of red versus white muscle fibers, and fresh or processed by preparation methods such as smoking, curing, salting, and/or addition of preservatives. Components of meat linked to chronic disease risk include fat content, particularly saturated fat in red meat, and dietary cholesterol(11, 12). Meat can also be a source of several known mutagens, including N-nitroso compounds (NOCs) in processed meats, and heterocyclic amines (HCAs) and polycyclic aromatic hydrocarbons (PAHs) formed during high-temperature cooking and grilling(13).
Intake of fat and meat, primarily from red meat, has been of public health concern since the late 1950s when the American Heart Association first recommended that dietary cholesterol, saturated fat, and total fat be reduced for the prevention of CVD(12, 14); and to date, numerous epidemiologic studies have investigated meat intake and cancer risk(15–17). According to the World Cancer Research Fund (WCRF)/American Institute for Cancer Research (AICR) report in 2007(18), the evidence linking red and processed meats to colorectal cancer was deemed `convincing'(19); “limited or suggestive” for red meat and cancers of the esophagus, lung, pancreas and endometrium, as well as processed meat and cancers of the esophagus, lung, stomach, and prostate(18). Smoked or grilled (charred) meat was also associated with higher risk of stomach cancer(18). In 2009, a large U.S. prospective cohort study reported an increased risk of death from cancer, CVD, and all causes with high intake of red and processed meat(20).
Based on the evidence to date, current dietary recommendations for the prevention of diet-related chronic diseases(18, 21–23), suggest to limit intake of red and processed meat and to eat mostly foods of plant origin. This report describes the trends, distribution, and potential determinants of meat consumption within the U.S. and other parts of the developed world over the last several decades. Further discussion addresses recent epidemiologic evidence for meat intake and chronic disease risk, and impending public health concerns.
METHODS
We used publicly accessible per capita food availability data provided by the Food and Agricultural Organization (FAO) of the United Nations(24) and the United States Department of Agriculture (USDA)(25) to compare temporal trends in meat consumption in the U.S. and other developed countries (defined by FAO as Japan in Asia, Canada and the U.S. in North America, Australia and New Zealand in Oceania, and all of Europe). FAO and USDA databases provide historical and chronological population-based production and disappearance data (referred to as food availability or consumption). We compared temporal trends in U.S. meat disappearance data to dietary intake data collected at the individual level from the National Health and Nutrition Examination Surveys (NHANES)(26).
FAO
The FAOSTAT(24) is the world's largest online agricultural database (available at http://faostat.fao.org/), and includes data from 190 FAO member countries. This data captures per capita meat consumption based on data submitted by member countries in response to standard questionnaires and supplemented by reviews of national sources and staff estimates or imputations to cover critical gaps(5). The FAO classifies total meat (excluding fish) as the sum of beef, poultry, pork, sheep, goat and other game. Per capita meat consumption (g/capita/day), defined as the total amount of the commodity available for human consumption (that is, after exports, and other waste from farm to household), were available from 1961 through 2005. Data from 1990 were revisited, resulting in changes in the historical data. The methodology for the estimation of food balance sheets were also revised in FAOSTAT, including new aggregation techniques for the conversion of transformed commodities into primary equivalents(27).
USDA
To look at U.S. meat consumption components and trends in more detail, we referenced food availability data (also known as U.S. Food Supply Data or Disappearance Data) from the USDA Economic Research Service (ERS) and accessible at http://www.ers.usda.gov/Data/Foodconsumption(25). The ERS food data system reflects the food availability per capita on an annual basis from 1909 through 2007 at the national level and serves as a popular proxy for actual consumption. This data represents the boneless, trimmed (edible) weight of fresh meat. Loss-adjusted data (removal of non-edible food parts and food lost through spoilage, plate waste, and other losses in the home and marketing system) were only available beginning from 1970. While both adjusted and unadjusted data were examined, only unadjusted values from the more comprehensive time period are presented to better characterize long-term trends. Red meat commodities included beef, veal, pork, lamb, and mutton. Poultry commodities included turkey and chicken. Fish and shellfish included fresh and frozen, canned, and cured products. Figures were calculated on the basis of raw and edible meats, which exclude edible offal, bones, and viscera for red meat and fishery products, but included skin, neck, and giblets for poultry. Consumption of game meats or fishery products and use of chicken for commercially-prepared pet food were also excluded(25). The USDA data provided in pounds/capita/year was converted to grams/capita/day (453.6 g/lb; 365.2 d/yr) for the sake of comparison to other data sources.
NHANES
We examined data from NHANES for 1999–2000 (n=8,074 people), 2001–2002 (n=9,033 people), and 2003–2004 (n=8,273 people). NHANES is a cross-sectional national survey conducted by the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention (CDC). The dietary portion was designed to provide nationally representative estimates of food intake in adults and children (civilian, non-institutionalized population), and to track changes in health and nutritional status over time. A single 24-hour dietary recall from all respondents age 2 and older with reliable dietary data was included and appropriate weighting factors were applied to adjust for differential probabilities of selection and non-response. Additional information on the survey designs, data collection protocols, weighting procedures, and response rates are described elsewhere(26).
To estimate meat intake we merged the NHANES data with the appropriate MyPyramid Equivalents Database (MPED). A new version of the MPED is developed for each NHANES data release; thus, MPED 1.0(28) was applied to survey data prior to 2002 and MPED 2.0(29), the most current version available, to 2003–2004. MPED for USDA Survey Foods translates the amounts of foods eaten in USDA's What We Eat in America (WWEIA) survey, the dietary intake component of NHANES, into the number of equivalents for the 32 MyPyramid major groups and subgroups(29). Meat intake reported in the 24-hour dietary recall is converted to the equivalent number of cup or ounce-equivalents (servings) after disaggregating mixtures and discretionary fats. Allowable fat in the meat group includes that present in lean cuts of meat trimmed of all fat and poultry without skin. Cooked lean meat ounce-equivalents (servings) were defined as no more than 9.28 g fat per 100 g of meat, poultry, or fish; or 3.53 ounces of cooked lean meat per 100 g of product(29). MPED estimates were converted to grams per day (28 g/oz). We used the following food group variables from the database: meat, poultry, fish with high omega-3 fatty acid content, fish with low omega-3 fatty acid content, and processed meat. The poultry group was composed of mainly chicken and turkey. Total fish was the sum of both high and low omega-3 fish and shellfish. To generate a total red meat variable we included red meat (beef, pork, veal, lamb, game) from meat, as well as the appropriate components of processed meat and organ meats, based on the recipe files for each of the food items in these food categories. Similarly, a total white meat variable was generated from poultry and processed or organ components from each of these groups. Total meat was the sum of fresh (not processed) red and white meat, plus cured meat, such as bacon and ham, as well as organ meats and fish. Soy products were excluded. Processed meat, by MPED definition(29), included frankfurters, sausage, and luncheon meats (made from meat or poultry), but did not include cured meats, such as ham or bacon.
We used SUDAAN to generate weighted means and standard errors for each meat item (red meat, poultry, fish, and processed meat; grams per day). We additionally examined meat intake stratified by gender, age (2–11 years, 12–19 years, 20–49 years, 50–69 years, and greater than 70 years), ethnicity (non-Hispanic White, non-Hispanic Black, Mexican-American/Other Hispanic, Other), and education (less than high school, high school, greater than high school). Using Bonferroni correction to adjust for multiple comparisons, a two-sided p<0.0005 was considered statistically significant for any single pair-wise comparison.
RESULTS
Temporal trends in meat consumption in developed countries
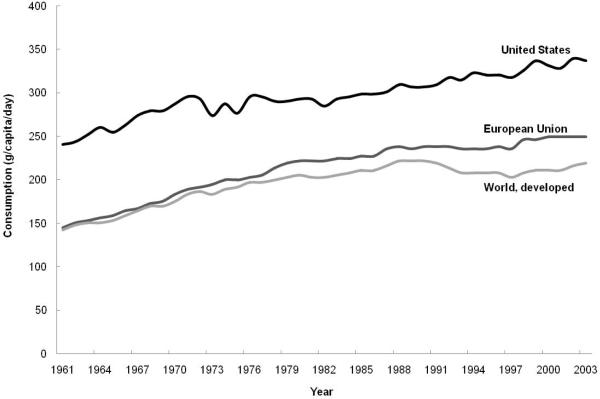
According to international FAO data, total meat consumption (excluding fish) in the U.S., European Union (E.U.), and developed world as a whole has increased relatively steadily over the period from 1961 to 2003 (Figure 1). As early as 1961, total meat consumption in the U.S. was nearly double that of the E.U. and the developed world as a whole. From 1961 to 2003, total meat consumption continued to increase in all regions: nearly doubling in the E.U. and increasing approximately 1.5-fold in the U.S. and developed world, as a whole. There appeared to be a slight decrease and plateau through the 1990s in the developed world, followed by an increase through 2003. Recent U.S. meat consumption appears somewhat unstable, peaking and falling in recent years. Consumption in the E.U. appears to have stabilized from the late 1990s through 2003. Overall, meat consumption appears to be on the rise in the developed world as whole, but remains considerably lower than in the U.S.
Figure 1.
Total meat consumption in the U.S., E.U., and developed world, FAOSTAT, 1961–2003
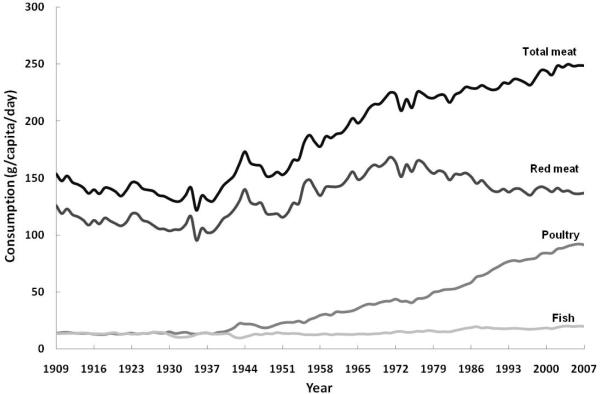
Looking in more detail at U.S. meat consumption, USDA data indicates that total meat consumption has increased notably over the last century, nearly doubling between 1909 and 2007 (Figure 2). The lowest meat consumption occurred in the 1930s and the highest meat consumption was reached during the most recent decade. Further examination attributes much of the increase to a rise in poultry consumption beginning in the 1950s and continuing to escalate through recent decades to make up a high proportion of the total meat consumed in the U.S. Red meat consumption appears to have decreased over the last few decades beginning in the 1980s, but still remains the highest contributor to total meat consumption. In contrast, fish consumption has remained low and stable over the past century.
Figure 2.
Total meat, red meat, poultry, and fish consumption in the U.S., USDA, 1909–2007
The same data adjusted for loss, but only available from 1970, is comparable to the trends shown in Figure 2 with a marked increase in poultry consumption, a slight decrease in red meat consumption, and an overall trend for increasing meat consumption. For the period 1970 to 2007, red meat consumption dropped from 105 to 85 g/cap/d, while poultry consumption more than doubled from 25 to 55 g/cap/d (loss-adjusted data not shown). Total loss-adjusted meat consumption was highest in 2004 at 154 g/cap/d with current estimates remaining close to this value (data not shown).
Components and determinants of meat consumption in the U.S.
NHANES (2003–2004) data from a single 24-hour dietary recall indicates that around 58% of the meat consumed in the U.S. was red meat, 32% poultry, and 10% fish (Figure 3). Processed meat intake constituted 22% of the total meat consumed from either red meat or poultry categories. Women consumed a slightly higher proportion of poultry than men (34% and 30%, respectively), a lower proportion of red meat (55% and 60%, respectively), and nearly equal proportions of processed meat (data not shown).
Figure 3.
Percent intake of different types of meat in U.S. as estimated by a single 24-hour dietary recall, NHANES, 2003–2004
A) Distribution of meat types that contribute to total meat intake. B) Percentage of total meat that is processed.
Table 1 describes U.S. meat intake from NHANES (2003–2004) by gender, age, ethnicity, and education level. In this nationally representative sample, total meat intake averaged 128 g/day (sum of red meat, poultry, and fish). Compared to women, men consumed more of every type of meat per day [all pair-wise comparisons (not shown) statistically significant (p<0.0005)]. With the exception of fish, peak meat consumption occurred in adults aged 20 through 49, particularly for red meat (80.3 g/day), with lower intakes at younger and older ages (p<0.0005 for ages 20–49 compared to 70+ for red meat, poultry, total meat, and processed meat) . Whites, Blacks, and Hispanics all reported similar intakes of red meat. Blacks consumed the highest amount of poultry (54.4 g/day) compared to Whites (p<0.0005) and Hispanics [p<0.001, not statistically significant (NS) for multiple comparisons]. Hispanics reported lower processed meat intake than Whites [p<0.001 (NS)] and Blacks (p<0.0005). Poultry and fish consumption appeared to increase with education level. Results from 1999–2000 and 2001–2002 were not notably different from the 2003–2004 results presented here. Across the 1999–2000, 2001–2002, 2003–2004 surveys, red meat intake appeared to decrease slightly, while poultry intake appeared to increase slightly (data not shown), which is in agreement with the data from the USDA (Figure 2).
Table 1.
Meat intake in the U.S. according to demographic factors, NHANES, 2003–2004
| Meat intake (g/day)◊ | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Red Meat | Poultry | Fish | Total Meat | Processed | |||||||
| Factor | n | mean | SE | mean | SE | mean | SE | mean | SE | mean | SE |
| All | 8,272 | 69.8 | 2.5 | 43.3 | 1.5 | 14.8 | 1.2 | 127.9 | 3.7 | 23.2 | 0.8 |
| Gender | |||||||||||
| Men | 4,036 | 87.6 | 2.8 | 48.8 | 1.7 | 17.4 | 1.6 | 153.8 | 4.1 | 29.0 | 1.0 |
| Women | 4,236 | 52.8 | 2.6 | 38.1 | 1.7 | 12.3 | 1.0 | 103.2 | 3.6 | 17.7 | 0.8 |
| Age (years) | |||||||||||
| 2–11 | 1,663 | 43.5 | 1.9 | 30.6 | 1.6 | 5.9 | 1.0 | 80.1 | 2.3 | 18.8 | 1.0 |
| 12–19 | 2,161 | 68.0 | 3.2 | 46.2 | 2.4 | 7.6 | 1.0 | 121.8 | 3.1 | 25.4 | 1.2 |
| 20–49 | 2,251 | 80.3 | 3.8 | 51.7 | 1.6 | 17.0 | 1.6 | 149.0 | 4.8 | 25.6 | 1.4 |
| 50–69 | 1,229 | 73.0 | 3.5 | 37.2 | 2.8 | 20.8 | 3.1 | 130.9 | 6.4 | 23.2 | 2.0 |
| 70+ | 968 | 53.0 | 2.9 | 29.9 | 1.6 | 13.6 | 1.4 | 96.8 | 3.2 | 15.4 | 1.2 |
| Race | |||||||||||
| White | 3,500 | 69.6 | 3.1 | 41.4 | 2.2 | 13.3 | 1.5 | 124.4 | 4.6 | 24.2 | 1.0 |
| Black | 2,257 | 69.6 | 2.5 | 54.2 | 2.2 | 16.4 | 1.6 | 140.2 | 2.9 | 26.3 | 1.3 |
| Hispanic | 2,280 | 73.1 | 4.5 | 41.3 | 1.9 | 14.2 | 1.4 | 128.6 | 4.3 | 17.6 | 1.2 |
| Other | 235 | 62.3 | 4.7 | 48.8 | 7.0 | 38.2 | 6.1 | 149.4 | 9.8 | 14.5 | 2.2 |
| Education | |||||||||||
| < High School | 4,029 | 65.1 | 2.5 | 39.7 | 1.6 | 11.0 | 1.2 | 115.7 | 3.9 | 21.0 | 0.9 |
| High School | 1,288 | 82.0 | 3.5 | 44.8 | 2.9 | 12.5 | 1.4 | 139.4 | 5.3 | 25.8 | 1.6 |
| > High School | 2,184 | 71.8 | 3.3 | 47.0 | 2.0 | 20.0 | 1.8 | 138.8 | 4.8 | 24.2 | 1.1 |
Cooked lean meat ounce-equivalents (MPED 2.0) converted to grams; weighted means, standard errors (SE)
DISCUSSION
Food availability data indicate that overall meat consumption is on the rise in the developed nations of the world and that the U.S. remains the highest consumer of total meat. Despite a shift toward increased poultry consumption, red meat still represents the largest proportion of meat consumed in the U.S. and nearly a quarter of the meat consumed is processed. Meat selection and consumption behaviors appeared to vary by education, race, age, and gender.
Despite near record-high per capita consumption of total meat in recent years, the proportion of fat, particularly saturated fat, in the U.S. food supply from meat, poultry, and fish has been slowly declining(30). Public health and consumer concerns regarding fat and cholesterol in the late 1980s led to greater demand for lean meat and poultry, increased trimming of visible fat on meat at the retail level, and consumer substitution of poultry for red meat(30, 31). Reports on fat consumption trends in the U.S. have shown a marked reduction in the proportion of fat from foods identified as major sources of saturated fat, including red meat (pork and beef) over the past several decades(32, 33).
Previous reports have shown that consumer's knowledge and awareness of diet and health may affect the proportion of red versus white meat consumed both at home and away from home(34). Chronological USDA data suggest that although poultry consumption has increased, red meat consumption has decreased comparably little, leaving total meat on the rise. Both loss-adjusted USDA data and intake values in NHANES suggest that current total meat intake for adults in the U.S. ranges from 100 to 150 g/day with more than half (50 to 90 g/day) coming from red meat. The affordability of meat in the U.S., combined with rising consumer incomes, may explain this trend. While vertical integration in U.S. poultry production resulted in a large, low-cost supply of poultry, the U.S. remains the world's largest beef producer and exporter, as well as a leading beef importer(30, 35). During the period 1994 to 1996, beef was a close second to yeast bread as the leading source of energy in U.S. adults; and the primary source of both protein and total fat(36). Meat consumption, production, and trade flows are also subject to temporary fluctuations due to food-safety issues. The bovine spongiform encephalopathy (BSE) or “mad cow disease” outbreak identified in the U.K. in the 1980s and later in the U.S. (2003) was a considerable blow to the beef industry and trade(37, 38).
NHANES data suggest that recent patterns of meat intake and overall consumption differ within the U.S. population according to various demographic factors, reflecting perhaps cultural, social, regional, and financial influences on diet. NHANES may provide a different picture of meat intake in U.S. individuals than have large, U.S. prospective cohorts, whose participants are largely Caucasian, age 50 or older, and college-educated. Although on a national-level the demand for meat would be expected to increase with economic growth, individual intake has tended to level off, and may even decline, at the highest levels of socio-economic status (SES)(39). Lower meat intake, particularly red and processed meat, with increasing adult age and education may reflect heightened awareness of health and/or adoption of dietary practices for the prevention or management of chronic disease.
Possible health implications of meat consumption
Meat in the diet provides an important source of protein and micronutrients, such as iron, zinc, and B-vitamins(40). However, energy-dense diets, purported to be high in meat, fats and sugars, and further compounded by sedentary lifestyle, have been implicated in the growing epidemics of obesity and diet-related chronic diseases(18, 41). Evidence suggests vegetarians may be at lower risk for CVD, hypertension, diabetes mellitus, obesity, and cancer(42–45). However, low-fat/high-carbohydrate diets have not been wholly positive or successful in reducing the burden of chronic disease within the general population(46–48); and lean meat and fish continue to be part of recommendations for a balanced, healthy diet (12, 49).
Inflammation and oxidative stress have also been linked to intake of meat and disease risk. Red meat, possibly due to its fat and iron content, may increase inflammation and oxidative stress, but less is known regarding lean and white meats(45, 50). Conversely, intake of fish has been shown to decrease markers of inflammation and oxidative stress(51, 52). Meat cooking (high-temperature, charring) and processing techniques, such as smoking, curing, salting or addition of chemical preservatives lead to the formation of carcinogenic compounds, such as N-nitroso compounds (NOCs), heterocyclic amines (HCAs) and polycyclic aromatic hydrocarbons (PAHs)(53–55). Exposure to NOCs occurs from both endogenous formation, which is directly related to red meat intake(56), as well as exogenous exposure from nitrite-preserved meats(57). While NOCs are also present in non-meat sources, such as vegetables and fruits(58), red meat is a key source of readily available heme iron, which may increase endogenous NOC formation(59). HCAs and PAHs, which are formed during high-temperature cooking of meat(60), dose-dependently generate DNA adducts(61).
The most robust human evidence is for red and processed meat intake and colorectal cancer(18, 19, 62–66). To date, findings for other major cancers such as prostate, breast, lung, kidney, and pancreatic cancer are less consistent and prospective data for rarer cancers are particularly sparse(67–72). However, in a comprehensive investigation from a U.S. prospective study of over 500,000 men and women, a significant increased risk of incident cancers of the colorectum, esophagus, lung, and liver were associated with red meat; and increased risk of colorectal and lung cancer was associated with higher intake of processed meat(53); red and processed meat intake was also associated with all-cause, CVD, and cancer mortality, while higher intake of white meat was associated with lower risk of death(20).
Strengths and Limitations
Results presented herein should be viewed with caution and the limitations of food supply/disappearance and cross-sectional data clearly acknowledged. There are a number of disadvantages of using food availability data, even though it is important for international comparisons as well as for looking at the overall, historic trends. The meat consumption data presented here are primarily based on annual food availability per capita at the national level and serve as popular proxies for actual consumption. The FAO derives their values from data submitted by member countries and are therefore limited by the completeness and accuracy of reporting at the national level.
It is important to recognize that while each data source appears to tell a similar story of U.S. meat consumption trends, USDA food availability and NHANES individual intake data serve different objectives(32). The U.S. food availability and consumption data measure the flow of raw and semi-processed agricultural commodities throughout the U.S. marketing system at an aggregate level(73). For both FAO and USDA food consumption data, human food intake is not directly measured and losses from trimming, cooking, waste, and spoilage are not fully estimable despite use of conversion factors which attempt to adjust for probable losses; this appeared to result in as much as a 100 gram difference between current adjusted and unadjusted USDA values. Individual-level intake data, such as that collected in NHANES from individual sample respondents, measure only edible and reportedly consumed foods from a designated period or point in time. In a large sample, such as NHANES, a single 24-hour dietary recall should provide a valid estimate of total meat intake at a population level and should also be adequate to capture relative consumption of different types of meat(74, 75). The NHANES population itself presents a number of advantages for studying current U.S. meat intake. NHANES sampling aims to capture the diversity, as well as regional variation in the U.S. population. Younger age groups and minority populations sampled in NHANES are often under-represented in most large epidemiologic and U.S. prospective studies. Additionally, most prospective cohorts in the U.S. and Europe began in the mid 1980s to 1990s, serving as the baseline level of intake, which USDA and NHANES data suggest may be considerably lower than current U.S. intake. Thus, comparably modest associations with meat in cohort populations may or may not translate to the broader U.S. population, which national estimates suggest, may be at differential, if not greater, risk in the near future.
Although quantities may not be precise representations of individual consumption, historical data is particularly valuable for understanding changing meat consumption in the U.S. The methodology for measuring food availability has remained relatively consistent over time and comparing USDA and FAO data with dietary assessment data from NHANES is a useful way to corroborate actual meat consumption patterns and trends(33). For the period 2003–2004, we found similar meat intake patterns for the relative proportion of types of meat consumed from both USDA and NHANES data. Unfortunately, the lag in the development and linkage of the MPED, the USDA's food group database, limits our ability to present NHANES meat intake data beyond 2003–2004. NHANES was the only data source in our analysis that shed light on processed meat intake and although it appears to make up a high proportion of the total meat currently consumed, we are unable track long-term changes in its availability and consumption. USDA and FAO tracking methods, by nature, do not allow for historical trend data on meat that has undergone processing, which may be derived from both fresh red meat and poultry. Due to emerging epidemiologic evidence on the risks of various cancers associated with high processed meat intake, recommendations to reduce processed meat are relatively new compared to those for red meat. Additionally, there is no generally agreed upon definition of processed meat, making it difficult to define and target in both public health research and practice.
CONCLUSION
Understanding the trends and determinants of meat consumption in the U.S., where meat is consumed at more than three times the global average(5), should be particularly pertinent to researchers and other public health professionals aiming to reduce the global burden of chronic disease. While saturated fat intake appears to be declining (30–33), other components of red and processed meat continue to pose a health risk particularly when consumed in large quantities(16, 54–57, 59–61). Studying food consumption and selection behaviors sheds light on the barriers we continue to face with the food industry and consumers, as well as international foresight in to future epidemics and their causes. As the main determinant of per capita meat consumption across the world appears to be wealth, examining trends in the U.S. and the rest of the developed world may forecast the global public health and environmental burdens we should expect to face in the highly-populated developing world(4). The growing preference in the U.S. for poultry, but not fish, as a replacement for red meat suggests the need for more epidemiologic investigations of white meat and its relation to long-term health and disease outcomes.
Acknowledgments
The authors' responsibilities were as follows—CRD: concept, analysis, interpretation of results, writing of the manuscript; AJC: interpretation of results, writing of manuscript; CK: analysis, interpretation of results; RS: concept, interpretation of results, writing of manuscript; and all authors: critical review and approval of the final manuscript.
We thank Jill Reedy for her contributions to this manuscript.
This research was supported by the Intramural Research Program of the NIH, National Cancer Institute.
Abbreviations
- (FAO)
Food and Agricultural Organization
- (USDA)
United States Department of Agriculture
- (NHANES)
National Health and Nutrition Examination Surveys
- (CVD)
cardiovascular disease
- (NOC)
N-nitroso compound
- (HCA)
heterocyclic amine
- (PAH)
polycyclic aromatic hydrocarbon
- (WCRF)
World Cancer Research Fund
- (AICR)
American Institute for Cancer Research
- (USDA)
United States Department of Agriculture
- (ERS)
Economic Research Service
- (NCHS)
National Center for Health Statistics
- (CDC)
Centers for Disease Control and Prevention
- (MPED)
MyPyramid Equivalents Database
- (WWEIA)
What We Eat in America
- (E.U.)
European Union
Footnotes
None of the authors had a financial or personal conflict of interest.
References
- 1.Food and Agriculture Organization of the United Nations Statistics Division Food Balance Sheets Millennium Issue 1999–2001 Special Charts (forthcoming publication) http://www.fao.org/statistics/ and http://www.fao.org/es/ess/chartroom/fbs.asp.
- 2.Hiza HAB, Bente L, Fungwe T. Nutrient Content of the U.S. Food Supply, 1909–2005. Home Economics Research Report. 2008;58 [Google Scholar]
- 3.United States Department of Agriculture U.S. Food Supply Database: 1909 to 2005 [Google Scholar]
- 4.Walker P, Rhubart-Berg P, McKenzie S, et al. Public health implications of meat production and consumption. Public Health Nutr. 2005;8:348–356. doi: 10.1079/phn2005727. [DOI] [PubMed] [Google Scholar]
- 5.Speedy AW. Global Production and Consumption of Animal Source Foods. J Nutr. 2003;133:4048S–4053. doi: 10.1093/jn/133.11.4048S. [DOI] [PubMed] [Google Scholar]
- 6.Krebs-Smith SM. Progress in improving diet to reduce cancer risk. Cancer. 1998;83:1425–1432. doi: 10.1002/(sici)1097-0142(19981001)83:7<1425::aid-cncr21>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 7.Terry P, Terry JB, Wolk A. Fruit and vegetable consumption in the prevention of cancer: an update. J Intern Med. 2001;250:280–290. doi: 10.1046/j.1365-2796.2001.00886.x. [DOI] [PubMed] [Google Scholar]
- 8.Dwyer T, Hetzel BS. A comparison of trends of coronary heart disease mortality in Australia, USA and England and Wales with reference to three major risk factors-hypertension, cigarette smoking and diet. Int J Epidemiol. 1980;9:65–71. doi: 10.1093/ije/9.1.65. [DOI] [PubMed] [Google Scholar]
- 9.Armstrong B, Doll R. Environmental factors and cancer incidence and mortality in different countries, with special reference to dietary practices. Int J Cancer. 1975;15:617–631. doi: 10.1002/ijc.2910150411. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization . World Health Statistics 2009. World Health Organization Press; Geneva: [Google Scholar]
- 11.Hu FB, Stampfer MJ, Manson JE, et al. Dietary saturated fats and their food sources in relation to the risk of coronary heart disease in women. Am J Clin Nutr. 1999;70:1001–1008. doi: 10.1093/ajcn/70.6.1001. [DOI] [PubMed] [Google Scholar]
- 12.Lichtenstein AH, Appel LJ, Brands M, et al. Diet and Lifestyle Recommendations Revision 2006: A Scientific Statement From the American Heart Association Nutrition Committee. Circulation. 2006;114:82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]
- 13.Cross AJ, Sinha R. Meat-related mutagens/carcinogens in the etiology of colorectal cancer. Environ Mol Mutagen. 2004;44:44–55. doi: 10.1002/em.20030. [DOI] [PubMed] [Google Scholar]
- 14.AHA American Heart Association Scientific Statements and Practice Guidelines for Researchers and Scientists: Diet/Nutrition. 2008 http://www.americanheart.org.
- 15.Alaejos MS, Gonzalez V, Afonso AM. Exposure to heterocyclic aromatic amines from the consumption of cooked red meat and its effect on human cancer risk: a review. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2008;25:2–24. doi: 10.1080/02652030701474235. [DOI] [PubMed] [Google Scholar]
- 16.Cross AJ, Leitzmann MF, Gail MH, et al. A prospective study of red and processed meat intake in relation to cancer risk. PLoS Med. 2007;4:e325. doi: 10.1371/journal.pmed.0040325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huxley RR, Ansary-Moghaddam A, Clifton P, et al. The impact of dietary and lifestyle risk factors on risk of colorectal cancer: A quantitative overview of the epidemiological evidence. International Journal of Cancer. 2009;125:171–180. doi: 10.1002/ijc.24343. [DOI] [PubMed] [Google Scholar]
- 18.World Cancer Research Fund. American Institute for Cancer Research . Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. AICR; Washington, DC: 2007. [Google Scholar]
- 19.Larsson SC, Wolk A. Meat consumption and risk of colorectal cancer: a meta-analysis of prospective studies. Int J Cancer. 2006;119:2657–2664. doi: 10.1002/ijc.22170. [DOI] [PubMed] [Google Scholar]
- 20.Sinha R, Cross AJ, Graubard BI, et al. Meat intake and mortality: a prospective study of over half a million people. Arch Intern Med. 2009;169:562–571. doi: 10.1001/archinternmed.2009.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krauss RM, Eckel RH, Howard B, et al. Revision 2000: a statement for healthcare professionals from the Nutrition Committee of the American Heart Association. J Nutr. 2001;131:132–146. doi: 10.1093/jn/131.1.132. [DOI] [PubMed] [Google Scholar]
- 22.Kushi LH, Byers T, Doyle C, et al. American Cancer Society Guidelines on Nutrition and Physical Activity for Cancer Prevention: Reducing the Risk of Cancer With Healthy Food Choices and Physical Activity. CA Cancer J Clin. 2006;56:254–281. doi: 10.3322/canjclin.56.5.254. [DOI] [PubMed] [Google Scholar]
- 23.Reedy J, Krebs-Smith SM. A comparison of food-based recommendations and nutrient values of three food guides: USDA's MyPyramid, NHLBI's Dietary Approaches to Stop Hypertension Eating Plan, and Harvard's Healthy Eating Pyramid. J Am Diet Assoc. 2008;108:522–528. doi: 10.1016/j.jada.2007.12.014. [DOI] [PubMed] [Google Scholar]
- 24.Food and Agriculture Organization of the United Nations FAO Statistical Databases (FAOSTAT): Food Consumption Data. 2008 December 16; http://faostat.fao.org/
- 25.United States Department of Agriculture Economic Research Service Food Availability Per Capita Data System. 2009 February 27; http://www.ers.usda.gov/Data/FoodConsumption/
- 26.National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey (NHANES) Data . U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Hyattsville, MD: http://www.cdc.gov/nchs/nhanes.htm. [Google Scholar]
- 27.FAO Statistics Division http://www.fao.org/statistics/ and http://www.fao.org/statistics/pdf/statistics_in_fao.pdf.
- 28.Friday JE, Bowman SA. MyPyramid Equivalents Database for USDA Survey Food Codes, 1994–2002. Version 1.0. USDA, ARS, Community Nutrition Research Group; Beltsville MD: 2006. Online. http://www.ars.usda.gov/ba/bhnrc/fsrg/ [Google Scholar]
- 29.Bowman SA, Friday JE, Mosehfegh A. MyPyramid Equivalents Database, 2.0 for USDA Survey Foods, 2003–2004 [Online] Food Surveys Research Group. Beltsville Human Nutrition Research Center, Agricultural Research Service, U.S. Department of Agriculture; Beltsville, MD: 2008. http://www.ars.usda.gov/ba/fsrg. [Google Scholar]
- 30.United States Department of Agriculture Agriculture Fact Book 2001–2002. Chapter 2: Profiling Food Consumption in America. http://www.usda.gov/factbook/index.html.
- 31.Committee on Technological Options to Improve the Nutritional Attributes of Animal Products . National Research Council. Designing foods: animal product options in the marketplace. National Academy Press; Washington, DC: 1988. [Google Scholar]
- 32.Popkin BM, Siega-Riz AM, Haines PS, et al. Where's the fat? Trends in U.S. diets 1965–1996. Prev Med. 2001;32:245–254. doi: 10.1006/pmed.2000.0807. [DOI] [PubMed] [Google Scholar]
- 33.Chanmugam P, Guthrie JF, Cecilio S, et al. Did fat intake in the United States really decline between 1989–1991 and 1994–1996? J Am Diet Assoc. 2003;103:867–872. doi: 10.1016/s0002-8223(03)00381-x. [DOI] [PubMed] [Google Scholar]
- 34.Lin BH, Yen S, Davis C. Consumer Knowledge and Meat Consumption in the U.S. International Association of Agricultural Economists. Gold Coast; Australia: 2006. [Google Scholar]
- 35.Brester GW, Marsh JM, Plain RL. International red meat trade. Vet Clin North Am Food Anim Pract. 2003;19:493–518. doi: 10.1016/s0749-0720(03)00024-0. [DOI] [PubMed] [Google Scholar]
- 36.Cotton PA, Subar AF, Friday JE, et al. Dietary sources of nutrients among US adults, 1994 to 1996. J Am Diet Assoc. 2004;104:921–930. doi: 10.1016/j.jada.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 37.Nathanson N, Wilesmith J, Griot C. Bovine Spongiform Encephalopathy (BSE): Causes and Consequences of a Common Source Epidemic. Am J Epidemiol. 1997;145:959–969. doi: 10.1093/oxfordjournals.aje.a009064. [DOI] [PubMed] [Google Scholar]
- 38.Harman JL, Silva CJ. Bovine spongiform encephalopathy. Journal of the American Veterinary Medical Association. 2009;234:59–72. doi: 10.2460/javma.234.1.59. [DOI] [PubMed] [Google Scholar]
- 39.Purcell WD, Lusk J. Demand for red meats: principles, research evidence, and issues. Vet Clin North Am Food Anim Pract. 2003;19:463–492. viii. doi: 10.1016/s0749-0720(03)00027-6. [DOI] [PubMed] [Google Scholar]
- 40.Stipanuk M. Biochemical, Physiological & Molecular Aspects of Human Nutrition. 2 ed. Saunders; 1999. [Google Scholar]
- 41.Mente A, de Koning L, Shannon HS, et al. A Systematic Review of the Evidence Supporting a Causal Link Between Dietary Factors and Coronary Heart Disease. Arch Intern Med. 2009;169:659–669. doi: 10.1001/archinternmed.2009.38. [DOI] [PubMed] [Google Scholar]
- 42.Fraser GE. Vegetarian diets: what do we know of their effects on common chronic diseases? Am J Clin Nutr. 2009;89:1607S–1612. doi: 10.3945/ajcn.2009.26736K. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Key TJ, Appleby PN, Spencer EA, et al. Mortality in British vegetarians: results from the European Prospective Investigation into Cancer and Nutrition (EPIC-Oxford) Am J Clin Nutr. 2009;89:1613S–1619. doi: 10.3945/ajcn.2009.26736L. [DOI] [PubMed] [Google Scholar]
- 44.Key TJ, Appleby PN, Spencer EA, et al. Cancer incidence in vegetarians: results from the European Prospective Investigation into Cancer and Nutrition (EPIC-Oxford) Am J Clin Nutr. 2009;89:1620S–1626. doi: 10.3945/ajcn.2009.26736M. [DOI] [PubMed] [Google Scholar]
- 45.Szeto YT, Kwok TC, Benzie IF. Effects of a long-term vegetarian diet on biomarkers of antioxidant status and cardiovascular disease risk. Nutrition. 2004;20:863–866. doi: 10.1016/j.nut.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 46.Hodgson JM, Burke V, Beilin LJ, et al. Partial substitution of carbohydrate intake with protein intake from lean red meat lowers blood pressure in hypertensive persons. Am J Clin Nutr. 2006;83:780–787. doi: 10.1093/ajcn/83.4.780. [DOI] [PubMed] [Google Scholar]
- 47.Appel LJ, Sacks FM, Carey VJ, et al. Effects of Protein, Monounsaturated Fat, and Carbohydrate Intake on Blood Pressure and Serum Lipids: Results of the OmniHeart Randomized Trial. JAMA. 2005;294:2455–2464. doi: 10.1001/jama.294.19.2455. [DOI] [PubMed] [Google Scholar]
- 48.Siri-Tarino PW, Sun Q, Hu FB, et al. Saturated fat, carbohydrate, and cardiovascular disease. Am J Clin Nutr. 91:502–509. doi: 10.3945/ajcn.2008.26285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kant AK, Graubard BI. A comparison of three dietary pattern indexes for predicting biomarkers of diet and disease. J Am Coll Nutr. 2005;24:294–303. doi: 10.1080/07315724.2005.10719477. [DOI] [PubMed] [Google Scholar]
- 50.Hodgson JM, Ward NC, Burke V, et al. Increased Lean Red Meat Intake Does Not Elevate Markers of Oxidative Stress and Inflammation in Humans. J Nutr. 2007;137:363–367. doi: 10.1093/jn/137.2.363. [DOI] [PubMed] [Google Scholar]
- 51.Lopez-Garcia E, Schulze MB, Manson JE, et al. Consumption of (n-3) fatty acids is related to plasma biomarkers of inflammation and endothelial activation in women. J Nutr. 2004;134:1806–1811. doi: 10.1093/jn/134.7.1806. [DOI] [PubMed] [Google Scholar]
- 52.Wijendran V, Hayes KC. Dietary n-6 and n-3 fatty acid balance and cardiovascular health. Annual Review of Nutrition. 2004;24:597–615. doi: 10.1146/annurev.nutr.24.012003.132106. [DOI] [PubMed] [Google Scholar]
- 53.Cross AJ, Leitzmann MF, Gail MH, et al. A Prospective Study of Red and Processed Meat Intake in Relation to Cancer Risk. PLoS Medicine. 2007;4:e325. doi: 10.1371/journal.pmed.0040325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stolzenberg-Solomon RZ, Cross AJ, Silverman DT, et al. Meat and meat-mutagen intake and pancreatic cancer risk in the NIH-AARP cohort. Cancer Epidemiol Biomarkers Prev. 2007;16:2664–2675. doi: 10.1158/1055-9965.EPI-07-0378. [DOI] [PubMed] [Google Scholar]
- 55.Sinha R, Norat T. Meat cooking and cancer risk. IARC Sci Publ. 2002;156:181–186. [PubMed] [Google Scholar]
- 56.Hughes R, Cross AJ, Pollock JR, et al. Dose-dependent effect of dietary meat on endogenous colonic N-nitrosation. Carcinogenesis. 2001;22:199–202. doi: 10.1093/carcin/22.1.199. [DOI] [PubMed] [Google Scholar]
- 57.Mirvish SS, Haorah J, Zhou L, et al. Total N-nitroso compounds and their precursors in hot dogs and in the gastrointestinal tract and feces of rats and mice: possible etiologic agents for colon cancer. J Nutr. 2002;132:3526S–3529S. doi: 10.1093/jn/132.11.3526S. [DOI] [PubMed] [Google Scholar]
- 58.Hord NG, Tang Y, Bryan NS. Food sources of nitrates and nitrites: the physiologic context for potential health benefits. Am J Clin Nutr. 2009;90:1–10. doi: 10.3945/ajcn.2008.27131. [DOI] [PubMed] [Google Scholar]
- 59.Cross AJ, Pollock JR, Bingham SA. Haem, not protein or inorganic iron, is responsible for endogenous intestinal N-nitrosation arising from red meat. Cancer Res. 2003;63:2358–2360. [PubMed] [Google Scholar]
- 60.Sinha R, Rothman N, Salmon CP, et al. Heterocyclic amine content in beef cooked by different methods to varying degrees of doneness and gravy made from meat drippings. Food and Chemical Toxicology. 1998;36:279–287. doi: 10.1016/s0278-6915(97)00162-2. [DOI] [PubMed] [Google Scholar]
- 61.Turteltaub KW, Dingley KH, Curtis KD, et al. Macromolecular adduct formation and metabolism of heterocyclic amines in humans and rodents at low doses. Cancer Letters. 1999;143:149–155. doi: 10.1016/s0304-3835(99)00116-0. [DOI] [PubMed] [Google Scholar]
- 62.Norat T, Bingham S, Ferrari P, et al. Meat, Fish, and Colorectal Cancer Risk: The European Prospective Investigation into Cancer and Nutrition. J Natl Cancer Inst. 2005;97:906–916. doi: 10.1093/jnci/dji164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cross AJ, Ferrucci LM, Risch A, et al. A Large Prospective Study of Meat Consumption and Colorectal Cancer Risk: An Investigation of Potential Mechanisms Underlying this Association. Cancer Res. 2010;70(6):2406–2414. doi: 10.1158/0008-5472.CAN-09-3929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Susanna C, Larsson AW. Meat consumption and risk of colorectal cancer: A meta-analysis of prospective studies. International Journal of Cancer. 2006;119:2657–2664. doi: 10.1002/ijc.22170. [DOI] [PubMed] [Google Scholar]
- 65.Norat T, Lukanova A, Ferrari P, et al. Meat consumption and colorectal cancer risk: Dose-response meta-analysis of epidemiological studies. International Journal of Cancer. 2002;98:241–256. doi: 10.1002/ijc.10126. [DOI] [PubMed] [Google Scholar]
- 66.Chao A, Thun MJ, Connell CJ, et al. Meat consumption and risk of colorectal cancer. JAMA. 2005;293:172–182. doi: 10.1001/jama.293.2.172. [DOI] [PubMed] [Google Scholar]
- 67.Cross AJ, Peters U, Kirsh VA, et al. A prospective study of meat and meat mutagens and prostate cancer risk. Cancer Res. 2005;65:11779–11784. doi: 10.1158/0008-5472.CAN-05-2191. [DOI] [PubMed] [Google Scholar]
- 68.Alexander DD, Cushing CA. Quantitative assessment of red meat or processed meat consumption and kidney cancer. Cancer Detection and Prevention. 2009;32:340–351. doi: 10.1016/j.cdp.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 69.Pala V, Krogh V, Berrino F, et al. Meat, eggs, dairy products, and risk of breast cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Am J Clin Nutr. 2009;90:602–612. doi: 10.3945/ajcn.2008.27173. [DOI] [PubMed] [Google Scholar]
- 70.Lee JE, Spiegelman D, Hunter DJ, et al. Fat, Protein, and Meat Consumption and Renal Cell Cancer Risk: A Pooled Analysis of 13 Prospective Studies. J Natl Cancer Inst. 2008:djn386. doi: 10.1093/jnci/djn386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Larsson SC, Hakanson N, Permert J, et al. Meat, fish, poultry and egg consumption in relation to risk of pancreatic cancer: a prospective study. Int J Cancer. 2006;118:2866–2870. doi: 10.1002/ijc.21732. [DOI] [PubMed] [Google Scholar]
- 72.Missmer SA, Smith-Warner SA, Spiegelman D, et al. Meat and dairy food consumption and breast cancer: a pooled analysis of cohort studies. Int J Epidemiol. 2002;31:78–85. doi: 10.1093/ije/31.1.78. [DOI] [PubMed] [Google Scholar]
- 73.Kantor LS. A comparison of the U.S. food supply with the Food Guide pyramid recommendations. In: Frazao E, editor. American's eating habits: changes and consequences, Information Bull 750. US Department of Agricultureed; Washington, DC: 1999. pp. 71–95. [Google Scholar]
- 74.Sekula W, Nelson M, Figurska K, et al. Comparison between household budget survey and 24-hour recall data in a nationally representative sample of Polish households. Public Health Nutrition. 2005;8:430–439. doi: 10.1079/phn2004695. [DOI] [PubMed] [Google Scholar]
- 75.Basiotis PP, Welsh SO, Cronin FJ, et al. Number of Days of Food Intake Records Required to Estimate Individual and Group Nutrient Intakes with Defined Confidence. J Nutr. 1987;117:1638–1641. doi: 10.1093/jn/117.9.1638. [DOI] [PubMed] [Google Scholar]