Abstract
Despite advances in medical and surgical techniques, older adults tend to be at high risk for adverse outcomes following burn injury. The purpose of this study was to examine the relative impacts of age and medical comorbidities on outcome following injury in a cohort of older adults. This was a retrospective study of all patients age 55 and over admitted to the University of Washington Burn Center from 1999 to 2003. To examine the effect of baseline medical comorbidities on outcome, a Charlson Comorbidity Index score was calculated for each patient. Multivariate regression analyses were used to examine the impact of age and comorbidities on mortality and other complications. Patient records were also matched with the National Death Index to determine the effects of age and comorbidities on mortality within 1 year following hospital discharge. A total of 325 patients who were of 55 years and older were admitted to the burn center during the 5-year study period. The overall mortality rate was 18.5%. Mortality was independently associated with age, inhalation injury, and burn size. One-year mortality was significantly associated with those older than age 75 and the Charlson score. Longer length of stay was significantly associated with burn size, inhalation injury, and total number of in-hospital complications. This study demonstrates that patient age—independent of baseline medical comorbidities—and TBSA burn are the most significant factors impacting in-hospital mortality risk following burn injury. Higher number of medical comorbidities was associated with increased mortality risk within 1 year following discharge.
In 1902, Weidenfeld described the significant relationship between age and burn-related mortality.1 Despite significant medical advances and improvement in overall mortality rates following injury, the association of increased age and mortality persists.2–5 In fact, the formulae commonly used to estimate survival following burn injury all incorporate age as an important prognostic indicator for survival.6,7 Older adults also tend to be at increased risk for other adverse outcomes including longer lengths of stay and higher hospital costs following burn injury over younger patients with comparable injuries.8
There are several potential reasons for worse outcome in older adults who sustain injury.2,8–12 Preexisting medical problems—including cardiovascular, pulmonary, and renal disease—can complicate fluid resuscitation, a cornerstone of the early postburn management period. Surgical management can also be more complicated in older patients because blood loss, intubation, and anesthesia may be poorly tolerated. However, the relative impact and interaction of age and medical comorbidities on adverse outcome risk remains poorly understood because of the limited scope of previous studies on older adult populations.
Given the increasing number of older adults in the population and their persistent injury risk factors (eg, impaired vision, decreased coordination, medication side effects), there will likely be a greater number of older adults sustaining burn injury. Therefore, there is a clear need to increase our understanding of the patient and injury characteristics and management strategies that impact outcome. The purpose of this study was to examine the relative impact of age and medical comorbidities on a number of outcomes following burn injury in older adults including in-hospital mortality, infectious and noninfectious complications, and 1-year mortality following discharge.
METHODS
Study Overview
This was a retrospective study of all patients who were of 55 years and above admitted to the University of Washington Burn Center from 1999 to 2003. This study was conducted following approval from our Institutional Review Board.
Study Population and Data Sources
Patients age 55 and over were identified from our burn center registry, which provides baseline patient and injury characteristics as well as outcome information on all admitted patients. The selection of 55 as the lower age limit is based on the observation that outcomes following injury begin to significantly change at that age level.13 The medical records of subjects identified by the database query were reviewed to verify injury characteristics, provide detailed information on medical comorbidities, and infectious and noninfectious complications not tracked in our database. Injury characteristics of interest included burn etiology, TBSA burned, presence of inhalation injury, and intubation status on admission to the burn center. Inhalation injury diagnosis was based on history, physical examination, and/or bronchoscopic examination.
To examine the effect of baseline medical comorbidities on outcome, a modified Charlson Comorbidity Index score was calculated for each patient. The standardized Charlson Index has been reported to accurately predict the probability of mortality within 1 year for a number of medical conditions.14,15 The score is the weighted sum of comorbid conditions and age. There are 19 comorbid conditions included in the score and each is assigned a weight from 1 to 6 points. The weighted sum of all comorbid conditions is the patient’s Charlson score.14,15 Typically, each decade above 40 is assigned a sequentially higher comorbidity ranking; however, because all our patients were over 40, age was not included in computation of the overall score. Age was included as an independent covariate in the multivariate analyses.
The outcomes of interest for this study included in-hospital mortality, infectious and noninfectious complications, and hospital length of stay. Noninfectious complications were categorized based on organ system as follows: cardiovascular (myocardial infarction, dysrhythmia requiring pharmacologic treatment, hypertension requiring intravenous medication, or pulmonary embolus), neurologic (cerebrovascular accident, delirium, alcohol withdrawal, peripheral neuropathy, anoxic brain injury, or seizure), pulmonary (Acute Respiratory Distress Syndrome), pulmonary failure requiring intubation, (Chronic Obstructive Pulmonary Disease) exacerbation, or pneumothorax), hematologic (deep venous thrombosis, heparin-induced thrombocytopenia, gastrointestinal bleed, or other bleeding disorder requiring greater than two unit transfusion outside of the operating room) and renal (actue renal failure requiring dialysis). Infectious complications included urinary tract infections, catheter-based infections, bloodstream infections, and pneumonia. Complication occurrence was based on the diagnosis being recorded in the medical record.
Finally, we examined 1-year mortality following hospital discharge using the National Center for Health Statistics’ National Death Index (NDI). Patients in our study were matched with national death certificate data based on full name, date of birth, sex, and state of residence at time of admission. We limited this study to 12 months because of the increased likelihood that other risk factors associated with advanced age may influence mortality more than the burn injury itself after 1 year. The decision to examine mortality 1-year following discharge rather than injury was done to allow us to examine the relative impact of in-hospital events, including length of stay, on mortality risk.
Data Analysis
To more precisely study the effects of age on outcome, patients were stratified into the following age groups: 55 to 64; 65 to 74; and 75 and above. Baseline patient and injury characteristics were compared between each age group using Analysis of Variance for continuous variables and chi-squared for discrete variables. In addition, we compared Charlson score and in-hospital complications across each age group. We employed both univariate and multivariate models in order to determine the relative influence of age and comorbidities when controlling for other factors. We used linear regression to examine hospital length of stay and logistic regression to examine mortality. Several additional models that included interaction terms for age and comorbidities were evaluated in order to better characterize the combined effects of increased age and comorbidity presence on outcome.
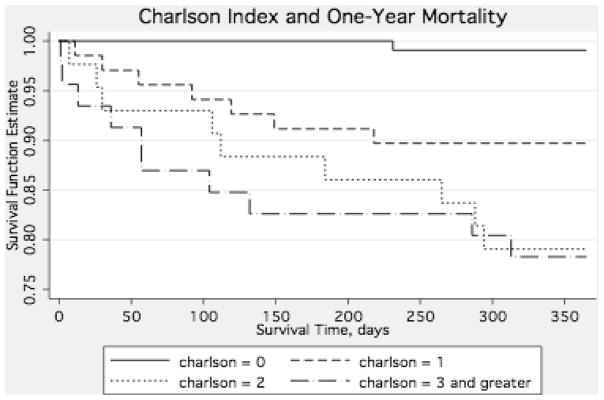
Two survival analyses were performed to examine mortality risk within 1-year of discharge: a Cox Proportional Hazards model that included the covariates of age, sex, burn size, inhalation injury status, Charlson Index score, and hospital length of stay and a Kaplan-Meier curve to demonstrate the relationship between comorbidity score and mortality within 1 year of discharge. Data were analyzed with STATA 9.0 (College Station, TX) and differences were considered significant when P < .05.
RESULTS
Patient and Injury Characteristics
A total of 325 patients 55 years of age and older were admitted to the burn center during the 5-year study period. Patient and injury characteristics are summarized in Table 1. The overall mean patient age was 68 years (SD = 10.2, range 55–93). Average burn size (% TBSA) was 14.9% (SD = 17.2, range 0.5–97.0%). The highest overall mean burn size (18.4% ± 18.5%) was observed in the oldest age (≥75) subgroup (P = .06). Fire and flame burns were the most common burn etiology in all age groups, with flash, scald, contact, and grease burns occurring less often. Inhalation injury was present in 11.3% of patients, with an increasing prevalence in the older age subgroups (P = .06).
Table 1.
Baseline patient and injury characteristics
| All (n = 325) | Age 55–64 (n = 145) | Age 65–74 (n = 85) | Age ≥ 75 (n = 95) | P | |
|---|---|---|---|---|---|
| Age, mean ± SD | 68.1 ± 10.2 | 58.7 ± 2.7 | 69.6 ± 2.6 | 81.3 ± 4.7 | <0.001 |
| Gender, female (%) | 36.3 | 26.2 | 42.4 | 46.3 | 0.003 |
| % TBSA, mean ± SD | 14.9 ± 17.2 | 13.8 ± 16.4 | 12.7 ± 16.5 | 18.4 ± 18.5 | 0.06 |
| TBSA grafted, mean ± SD | 3.1 ± 6.8 | 3.4 ± 7.5 | 1.8 ± 4.4 | 3.8 ± 7.4 | 0.12 |
| Inhalation (%) | 11.3 | 9.1 | 12.2 | 14.0 | 0.50 |
| Etiology (%) | 0.08 | ||||
| Fire/flame | 58.2 | 51.4 | 63.5 | 63.9 | |
| Flash | 15.9 | 21.2 | 10.6 | 12.4 | |
| Scald | 12.5 | 11.6 | 14.1 | 12.4 | |
| Contact | 4.6 | 4.8 | 2.4 | 6.2 | |
| Grease | 3.7 | 3.4 | 5.9 | 2.1 | |
| Other | 3.4 | 3.4 | 3.6 | 3.1 | |
| Electrical | 1.8 | 4.1 | 0 | 0 |
Medical Comorbidities
Charlson Index scores are summarized in Table 2. The majority of patients (51.7%) in the youngest age cohort (55–64) had no preexisting medical comorbidities. A higher percentage of patients in the 65 to 74 (46.5%) and ≥75 (45.8%) age groups had a Charlson score of 2 or higher (46.5% and 45.8%, respectively). The average Charlson Index score increased with increasing age group (1.0 vs 1.4 vs 1.7, P < .001). There was no significant correlation (r = −.01, P = .84) between burn size and Charlson score.
Table 2.
Charlson comorbidity index scores
| Charlson | All | Age 55–64 | Age 65–74 | Age ≥ 75 | P |
|---|---|---|---|---|---|
| 0 | 124 (38.2) | 75 (51.7) | 29 (34.1) | 20 (21.1) | <0.001 |
| 1 | 85 (26.2) | 38 (26.2) | 16 (18.8) | 31 (32.6) | |
| 2 | 55 (16.9) | 16 (11.0) | 22 (25.9) | 17 (17.9) | |
| ≥3 | 61 (18.8) | 16 (11.0) | 18 (21.2) | 27 (28.4) | |
| Total, mean ± SD | 1.3 ± 1.4 | 1.0 ± 1.4 | 1.4 ± 1.3 | 1.7 ± 1.4 | <0.001 |
Length of Stay, Complications, and Disposition Status
Overall length of stay and length of stay per %TBSA was similar across age groups (Table 3). On multivariate regression analysis (Table 4), each percentage point increase in the TBSA was associated with a 0.9-day longer length of stay. Each complication was associated with a 1 week longer hospitalization, when controlling for the other variables. No other factors were significantly associated with length of stay.
Table 3.
Hospital outcomes
| All | Age 55–64 | Age 65–74 | Age ≥ 75 | P | |
|---|---|---|---|---|---|
| Mortality | 18.5% | 9.7% | 16.5% | 32.7% | <0.001 |
| LOS mean ± SD* | 16.4 ± 19.1 | 16.1 ± 18.8 | 15.8 ± 20.4 | 17.7 ± 18.2 | 0.82 |
| LOS/TBSA mean ± SD* | 2.4 ± 4.0 | 2.3 ± 4.2 | 2.4 ± 3.4 | 2.7 ± 4.4 | 0.84 |
| No. of ops mean ± SD* | 1.7 ± 1.3 | 1.9 ± 1.5 | 1.5 ± 1.1 | 1.5 ± 0.8 | 0.46 |
| Disposition (%)* | <0.001 | ||||
| Home | 84.2 | 92.4 | 84.5 | 66.7 | |
| Extended care | 9.4 | 3.1 | 7.0 | 25.4 | |
| Other home | 4.2 | 2.3 | 5.6 | 6.4 | |
| Acute care | 2.3 | 2.3 | 2.8 | 1.6 |
Survivors only.
Table 4.
Factors influencing length of stay
| Patient and Injury Characteristics | Univariate models |
Multivariate model |
||||
|---|---|---|---|---|---|---|
| β-Coefficient | 95% CI | P | β-Coefficient | 95% CI | P | |
| Age | ||||||
| 55–64 (reference) | ||||||
| 65–74 | −0.4 | −5.9–5.2 | 0.98 | 1.4 | −2.2–4.9 | 0.45 |
| 75 and over | 1.6 | −4.2–7.4 | 0.59 | 0.1 | −3.6–3.8 | 0.97 |
| Sex (female) | −1.3 | −6.1–3.6 | 0.61 | −1.6 | −4.8–1.5 | 0.31 |
| % TBSA | 1.3 | 1.1–1.5 | <0.001 | 0.9 | 0.7–1.0 | <0.001 |
| Inhalation injury | 21.5 | 11.5–31.4 | <0.001 | 2.3 | −4.5–9.0 | 0.51 |
| Charlson score | −0.1 | −1.8–1.5 | 0.86 | 0.0 | −1.0–1.0 | 0.99 |
| Number of complications | 10.0 | 8.7–11.3 | <0.001 | 7.4 | 6.1–8.7 | <0.001 |
Infectious complications were overall the most common complication, occurring in 25.9% of all patients, but did not vary significantly by age group. The most common noninfectious complications across all age categories were cardiovascular and pulmonary in nature, both of which were significantly more common in the oldest subgroup (P = .002 and P = .004, respectively). Neurologic, renal, and hematologic complications occurred in 12.7, 8.6, and 9.0%, respectively, of the overall population and each occurred most commonly in the oldest age group. Only cardiovascular complication occurrence was significantly associated with higher Charlson score (P = .02).
In each age group, the majority of the patients were discharged home (Table 3). Patient discharge disposition varied significantly across age categories (P < .001); more patients in the ≥75 years of age subgroup were discharged to an extended care facility and fewer to home.
In-Hospital and 12-Month Mortality
The overall in-hospital mortality rate was 18.5%, (Table 3) with higher rates associated with increasing age. The average burn size of those patients who did not survive was highest in the 55 to 64 age group (42.8%) and was similar in the 65 to 74 age group and ≥75 age group (35.9% and 36.3%, respectively). These differences were not statistically significant. In patients who had inhalation injury, the average burn size of those who did not survive was significantly higher than those without inhalation injury in each age group. On multivariate analysis, higher mortality rate was independently associated with age ≥75 (odds ratio [OR] 4.8, confidence interval [CI] 2.4–9.5); inhalation injury (OR 11.9, CI 5.5–25.4); and %TBSA (OR 1.1, CI 1.1–1.2) (Table 5). Several additional models were constructed that included the interaction terms for age and comorbidity to determine whether the impact of comorbidities on outcome varied by age group; however, we did not find this to be the case.
Table 5.
Factors influencing in-hospital mortality
| Patient and Injury Characteristics | Univariate Models |
Multivariate Model |
||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | P | Odds Ratio | 95% CI | P | |
| Age | ||||||
| 55–64 (reference) | ||||||
| 65–74 | 1.9 | 0.8–4.1 | 0.13 | 4.2 | 1.2–14.9 | 0.03 |
| 75 and over | 4.8 | 2.4–9.5 | <0.001 | 8.4 | 2.8–27.8 | <0.001 |
| Sex (female) | 1.7 | 1.0–3.0 | 0.07 | 1.4 | 0.6–3.3 | 0.46 |
| % TBSA | 1.1 | 1.1–1.2 | <0.001 | 1.1 | 1.1–1.2 | <0.001 |
| Inhalation injury | 11.9 | 5.5–25.4 | <0.001 | 6.0 | 2.0–17.5 | 0.001 |
| Charlson score | 1.2 | 1.0–1.4 | 0.11 | 1.3 | 0.9–1.7 | 0.14 |
CI, confidence interval.
Of those patients discharged from the hospital, 10.2% died within 12 months following discharge with the highest mortality rate in the oldest cohort. Of these mortalities, 30% expired within 30 days of discharge and 70% within 6 months. In a multivariate Cox proportional hazard regression (Table 6), age 75 and over (hazard ratio 3.7, CI 1.6–8.9, P = .007) and Charlson score (hazard ratio 1.6, CI 1.3–1.8, P < .001) were the only two variables significantly associated with 1-year mortality. Survival curves based on Charlson score demonstrate the increased mortality risk with increased comorbidity score within 1 year of discharge (Figure 1).
Table 6.
Mortality within 1 year of discharge
| Independent Variable | Univariate Models |
Multivariate Model |
||||
|---|---|---|---|---|---|---|
| Hazard Ratio | 95% CI | P | Hazard Ratio | 95% CI | P | |
| Age | ||||||
| 55–64 (reference) | ||||||
| 65–74 | 1.4 | 0.5–4.0 | 0.75 | 1.1 | 0.4–3.1 | 0.93 |
| 75 and over | 3.7 | 1.6–8.9 | 0.004 | 3.6 | 1.4–8.8 | 0.006 |
| Sex (female) | 1.0 | 0.4–2.2 | 0.97 | 0.7 | 0.4–1.7 | 0.50 |
| % TBSA | 0.9 | 0.8–1.0 | 0.005 | 0.9 | 0.9–1.1 | 0.32 |
| Inhalation injury | 0.7 | 0.1–0.7 | 0.67 | 2.7 | 0.3–22.3 | 0.36 |
| Charlson score | 1.6 | 1.3–1.9 | <0.001 | 1.5 | 1.3–1.8 | <0.001 |
| Length of stay | 0.9 | 0.9–1.0 | 0.007 | 0.9 | 0.9–1.0 | 0.04 |
CI, confidence interval.
Figure 1.
Mortality following discharge by Charlson Comorbidity Index score.
DISCUSSION
The percentage of elderly people in North America is estimated to reach 20% of the population by 2030 while the risk factors for injury in older adults will likely remain constant.16 Mortality rates in older burn patients have declined over the past several decades in part due to resuscitation, ventilation strategies, nutrition, and early debridement2; yet, trauma and burns continue to be one of the leading causes of mortality in older individuals.2,4,16,17 Improvements in the outcomes of older adults following burn injury require a better understanding of the interaction between baseline patient characteristics, injury characteristics, and hospital course.
Our data show that increasing age was strongly associated with mortality risk both at hospital discharge and within 1 year following discharge—an observation that has been repeatedly demonstrated in studies of burn mortality risk.6,7 There are several potential reasons for the increased mortality seen in the elderly. These include decreased wound healing potential,18–20 decreased physiologic reserve, poor nutritional status,2,19 and medical comorbidities.10,18
We were particularly interested in examining whether age itself or the number of comorbidities accompanying advanced age underlie mortality risk. Previous studies on the impact of comorbidities on mortality following burn injury are conflicting. Lionelli et al and Wibbenmeyer et al2,12 previously reported no correlation between comorbidities and mortality; however, Rao et al and Covington et al11,18 found an association between comorbid conditions and outcome, especially for cardiac and pulmonary diseases. In these studies examining the effect of comorbidities, the comorbidities are usually listed by number without prioritization or gradation of severity. To better account for the likely differential impact of comorbidity type and severity, we used the standardized Charlson Index score for our study.
The Charlson Index has been shown to accurately predict the probability of mortality within 1 year for a number of medical conditions and but has rarely used in trauma and burn research.21–23 Thombs23 used the Charlson Index to examine all adult patients from the ABA National Burn Repository over a 10-year period for the contribution of medical comorbidities to mortality and length of stay. In this study, certain medical conditions were found to be associated with an increased risk of death. However, their study population was younger (age 20–60) than our population and the most strongly associated with mortality were the ones not found in our population such as AIDS and metastatic cancer.
On the basis of our patients’ Charlson Comorbidity scores, we found that age alone, independent of comorbidities, was associated with risk of in-hospital mortality; there was no significant impact of baseline medical comorbidities on mortality. However, when examining mortality within 1 year of discharge, the Charlson Comorbidity Index score was independently associated with mortality risk. The finding of increasing Charlson score correlating with higher 12-month postinjury mortality risk is consistent with other medical disease states where higher score predicts higher mortality risk.14,24,25
The differential impact of comorbidities on mortality may be attributable to any number of factors. First, it is possible that comorbidities were well managed in the hospital and may not have been following discharge. Alternatively, patients may have survived to discharge but did not return to their preinjury health or functional status and that their preexisting medical conditions exerted a strong influence on survival. Finally, it is possible that following discharge patients succumbed to their comorbidities independent of burn injury.
It is likely that all three of these factors underlie the findings of this study. Therefore, an intervention that continues the ongoing multidisciplinary care the burn team provides in the hospital may improve outcomes following discharge. Ideally, this team would include geriatricians, physical therapists, pharmacists, social workers, and dieticians; the team would establish a care plan prior to discharge and monitor patient progress on an interval basis over the subsequent 6 months to 1 year. There have been several studies that have demonstrated a positive effect of interdisciplinary management plans for older adults that are initiated on an inpatient basis and continue following discharge.26,27 Shyu26 developed a program for older adults admitted with hip fracture that included a functional rehabilitation component and a mechanism for ongoing coordinated multidisciplinary care following discharge. Patients managed in this program had improved long-term clinical outcomes including self-care abilities and health-related quality of life. Cohen developed an interdisciplinary care program including geriatricians, dieticians, pharmacists, and physical therapists for older adults that was initiated in the hospital and continued following hospital discharge. Although patients treated in this program did not have improved mortality, other quality of life outcomes were superior to those patients receiving usual care.
In addition to mortality, we examined the inhospital complications and overall hospital length of stay. The most common complications were infectious and cardiovascular (most commonly dysrthymias). The rate of any infection was 26%, but, unlike other studies, we did not find a correlation between mortality and infection.
Overall mean length of hospital stay was 16.3 days or 2.4 days/TBSA among those who survived their injury. This length of stay is higher than the commonly cited goal of 1 day/%TBSA and is twice our overall hospital length of stay for patients of all ages but is similar to other reports of length of stay in older adults.3,11 Total burn size (%TBSA) and number of in-hospital complications were both independently related to overall hospital length of stay. Baseline comorbidities, independent of hospital complications, were not associated with hospital length of stay. Interestingly, the total length of stay did not differ among age groups and did not impact disposition status.
There are several potential limitations to this study. First, this was a retrospective study dependent on chart documentation of medical comorbidities that may have been incomplete at times. As has been shown previously, the extent of chart documentation of comorbidites was less on patients with severe injuries who died shortly following admission.28 In addition, there was little functional and psychological outcome data available for these patients and the importance of quality of life is a critical consideration in evaluating any outcome study. In this study, we did not examine the impact of management decisions such as time to operation, use of skin substitutes, and limb amputation on outcome. These are important issues but were beyond the scope of this study. Finally, we relied on complications as documented in the patient record and we did not have standard diagnostic criteria for each complication ascertained.
In conclusion, this study demonstrates that patient age—independent of baseline medical comorbidities—inhalation injury, and TBSA burn are the most significant factors impacting in-hospital mortality risk following burn injury. Baseline medical comorbidities along with age ≥75 were associated with increased risk of mortality within 1 year following discharge. Clearly, additional work is required in order to better examine the impact of management of older adults with burn injury on outcome and to determine optimal management strategies of these patients in light of age, comorbidities, and potential outcomes. With the increasing number of older adults likely to sustain burn injuries, the need to understand the dynamic and crucial interplay of baseline patient characteristics, injury factors and management practices is clear and present.
Acknowledgments
This study was supported by grant number 5 K12 RR023265-0 from the National Institutes of Health and supported by funds from the National Institute on Disability and Rehabilitation Research in the Office of Special Education and Rehabilitative Services in the U.S. Department of Education.
References
- 1.Anous MM, Heimbach DM. Causes of death and predictors in burned patients more than 60 years of age. J Trauma. 1986;26:135–9. doi: 10.1097/00005373-198602000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Lionelli GT, Pickus EJ, Beckum OK, Decoursey RL, Korentager RA. A three decade analysis of factors affecting burn mortality in the elderly. Burns. 2005;31:958–63. doi: 10.1016/j.burns.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 3.Mann R, Heimbach D. Prognosis and treatment of burns. West J Med. 1996;165:215–20. [PMC free article] [PubMed] [Google Scholar]
- 4.McGill V, Kowal-Vern A, Gamelli RL. Outcome for older burn patients. Arch Surg. 2000;135:320–5. doi: 10.1001/archsurg.135.3.320. [DOI] [PubMed] [Google Scholar]
- 5.Ryan CM, Schoenfeld DA, Thorpe WP, Sheridan RL, Cassem EH, Tompkins RG. Objective estimates of the probability of death from burn injuries. N Engl J Med. 1998;338:362–6. doi: 10.1056/NEJM199802053380604. [DOI] [PubMed] [Google Scholar]
- 6.Baux S. Les sequelles des brulures. Rev Prat. 1980;9:585–8. [PubMed] [Google Scholar]
- 7.Zawacki BE, Azen SP, Imbus SH, Chang YT. Multifactorial probit analysis of mortality in burned patients. Ann Surg. 1979;189:1–5. doi: 10.1097/00000658-197901000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li BG, Hsu WS, Shih TS. Causes of death in aged burn patients: analysis of 36 cases. Burns. 1990;16:207–10. doi: 10.1016/0305-4179(90)90041-t. [DOI] [PubMed] [Google Scholar]
- 9.Hill AJ, Germa F, Boyle JC. Burns in older people—outcomes and risk factors. J Am Geriatr Soc. 2002;50:1912–3. doi: 10.1046/j.1532-5415.2002.50530.x. [DOI] [PubMed] [Google Scholar]
- 10.McGwin G, Jr, Cross JM, Ford JW, Rue LW., III Long-term trends in mortality according to age among adult burn patients. J Burn Care Rehabil. 2003;24:21–5. doi: 10.1097/00004630-200301000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Rao K, Ali SN, Moiemen NS. Aetiology and outcome of burns in the elderly. Burns. 2006;32:802–5. doi: 10.1016/j.burns.2006.03.024. [DOI] [PubMed] [Google Scholar]
- 12.Wibbenmeyer LA, Amelon MJ, Morgan LJ, et al. Predicting survival in an elderly burn patient population. Burns. 2001;27:583–90. doi: 10.1016/s0305-4179(01)00009-2. [DOI] [PubMed] [Google Scholar]
- 13.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–78. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 14.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 15.Needham DM, Scales DC, Laupacis A, Pronovost PJ. A systematic review of the Charlson Comorbidity Index using Canadian administrative databases: a perspective on risk adjustment in critical care research. J Crit Care. 2005;20:12–9. doi: 10.1016/j.jcrc.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 16.Stassen NA, Lukan JK, Mizuguchi NN, Spain DA, Carrillo EH, Polk HC., Jr Thermal injury in the elderly: when is comfort care the right choice? Am Surg. 2001;67:704–8. [PubMed] [Google Scholar]
- 17.Chang EJ, Edelman LS, Morris SE, Saffle JR. Gender influences on burn outcomes in the elderly. Burns. 2005;31:31–5. doi: 10.1016/j.burns.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 18.Covington DS, Wainwright DJ, Parks DH. Prognostic indicators in the elderly patient with burns. J Burn Care Rehabil. 1996;17:222–30. doi: 10.1097/00004630-199605000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Demling RH. The incidence and impact of pre-existing protein energy malnutrition on outcome in the elderly burn patient population. J Burn Care Rehabil. 2005;26:94–100. doi: 10.1097/01.bcr.0000150302.71007.80. [DOI] [PubMed] [Google Scholar]
- 20.Platt AJ, Phipps AR, Judkins K. Is there still a place for comfort care in severe burns. Burns. 1998;24:754–6. doi: 10.1016/s0305-4179(98)00096-5. [DOI] [PubMed] [Google Scholar]
- 21.Gabbe BJ, Magtengaard K, Hannaford AP, Cameron PA. Is the Charlson Comorbidity Index useful for predicting trauma outcomes? Acad Emerg Med. 2005;12:318–21. doi: 10.1197/j.aem.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 22.Taylor MD, Tracy JK, Meyer W, Pasquale M, Napolitano LM. Trauma in the elderly: intensive care unit resource use and outcome. J Trauma. 2002;53:407–14. doi: 10.1097/00005373-200209000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Thombs BD, Singh VA, Halonen J, Diallo A, Milner SM. The effects of preexisting medical comorbidities on mortality and length of hospital stay in acute burn injury: evidence from a national sample of 31,338 adult patients. Ann Surg. 2007;245:629–34. doi: 10.1097/01.sla.0000250422.36168.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jepsen P, Vilstrup H, Andersen PK, Lash TL, Sorensen HT. Comorbidity and survival of Danish cirrhosis patients: A nationwide population-based cohort study. Hepatology. 2008;48:214–20. doi: 10.1002/hep.22341. [DOI] [PubMed] [Google Scholar]
- 25.Tang J, Wan JY, Bailey JE. Performance of comorbidity measures to predict stroke and death in a community-dwelling, hypertensive Medicaid population. Stroke. 2008;39:1938–44. doi: 10.1161/STROKEAHA.107.504688. [DOI] [PubMed] [Google Scholar]
- 26.Shyu YI, Liang J, Wu CC, et al. A pilot investigation of the short-term effects of an interdisciplinary intervention program on elderly patients with hip fracture in Taiwan. J Am Geriatr Soc. 2005;53:811–8. doi: 10.1111/j.1532-5415.2005.53253.x. [DOI] [PubMed] [Google Scholar]
- 27.Cohen HJ, Feussner JR, Weinberger M, et al. A controlled trial of inpatient and outpatient geriatric evaluation and management. N Engl J Med. 2002;346:905–12. doi: 10.1056/NEJMsa010285. [DOI] [PubMed] [Google Scholar]
- 28.Finlayson EV, Birkmeyer JD, Stukel TA, Siewers AE, Lucas FL, Wennberg DE. Adjusting surgical mortality rates for patient comorbidities: more harm than good? Surgery. 2002;132:787–94. doi: 10.1067/msy.2002.126509. [DOI] [PubMed] [Google Scholar]