External approaches to the orbit are well established, including the lateral, medial, and inferior orbitotomy. Orbitozygomatic craniotomy can be used for tumors that extend both intracranially and into the orbit and is used for exposure of the optic nerve and canal.1 Since the 1980s, endoscopic measures have been used to enhance visualization in standard external approaches.2 Endoscopic endonasal orbital and optic nerve decompressions have become accepted treatments for thyroid eye disease and traumatic optic neuropathy that is unresponsive to steroids. A few case reports of endoscopic decompression, biopsy, and resection of tumors that involve the orbit also have been reported.3–5 The expanded endonasal approach (EEA) has been extended to resection of all types of skull base tumors, including posterior, middle, and anterior fossa masses. In this report, we describe the anatomic principles, indications, technical nuances, and limitations of the medial-inferior intraconal EEA to intraorbital tumor surgery, illustrated through a case series of six patients. This approach is ideally suited to benign soft-tissue masses (hemangioma/lymphangioma) in the medial-inferior quadrant of the orbit that do not extend superolaterally. The use of this technique would avoid the technical difficulties in approaching such masses and limit the dissection to the areas bordering the endonasal corridor.
Operative Technique
Approval for this review was obtained from the University of North Carolina Institutional Review Board. The key anatomic difference between intraconal and extraconal orbital tumors is the position relative to the boundaries of the extraocular muscles. For medial/inferior intraconal lesions, the dissection corridor is between the medial and inferior rectus muscles. The extraconal fat is reduced via bipolar cautery, and the rectus muscles are identified. The soft-tissue structures of the orbit are all freely mobile and compressible, thus making entry into the intraconal space difficult.
A technique of rectus muscle retraction was developed whereby the medial and inferior rectus muscles are isolated with vessel loops as they insert on the globe (Fig 1). It allows for traction to be placed on the muscles to make them less compressible and easier to dissect between. Once the intraconal corridor is developed, the tumor is identified and removed with limited bipolar cautery and extensive sharp dissection (Fig 2). It is helpful to have one surgeon retracting the mass inferomedially, while the other surgeon uses a bimanual technique to incise the lateral tumor margin. Because the optic nerve should be superior and lateral to the tumor, once the lateral margin is cleared, the nerve is out of the field of dissection. The remaining soft-tissue tumor attachments are then incised, and the tumor is removed en-bloc. Postoperative magnetic resonance imaging demonstrated complete tumor resection without evidence of residual disease.
Figure 1.
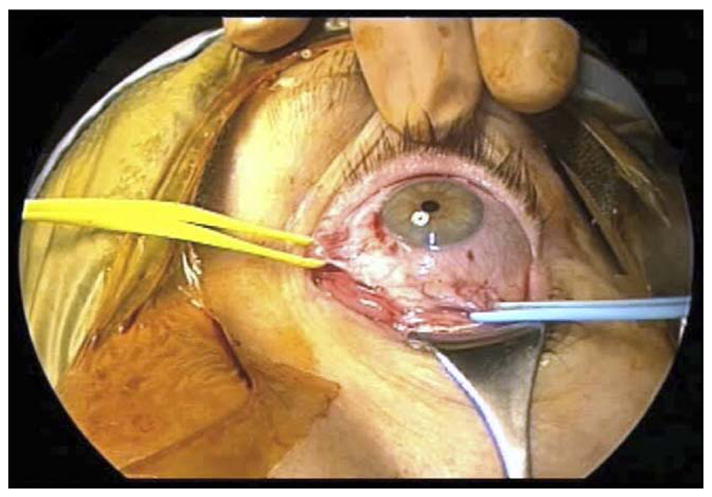
External view of the left extraocular muscles identified and vessel looped for control.
Figure 2.
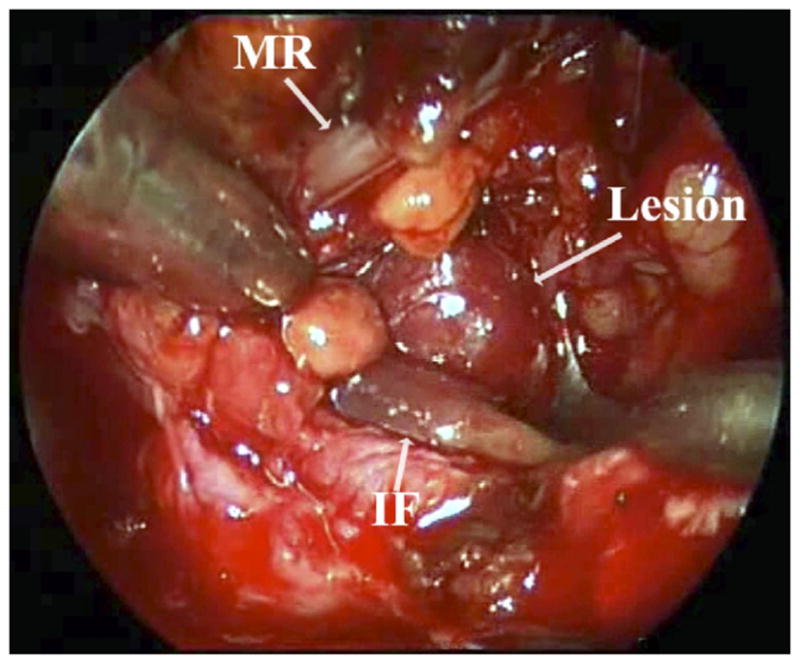
Intraconal identification and dissection of the hemangioma. MR, medial rectus; IF, inferior rectus.
In an alternate technique for controlling the rectus muscles, the medial rectus is detached from the globe and tagged with a long silk suture, which is then passed from the orbit into the nose. This step opens the medial orbit like a book, with the medial rectus pedicled on the annulus of Zinn. A vessel loop is placed endoscopically around the contralateral posterior septum and the posterior medial rectus muscle, which allows for medial retraction of the muscle to open the lateral corridor of the intraconal space.
Once the tumor is removed, meticulous hemostasis is obtained, and the rectus muscle vessel loops are released so that extraocular movements can be assessed. The rectus muscles are placed back into their native positions, and the medial rectus muscle is sutured back onto the globe by an ophthalmologic surgeon. The orbital fat is then pulled over the muscles to prevent scarring. When a septal flap is used, it is placed directly over the defect and bolstered in place with Surgicel (Ethicon, Inc., Somerville, NJ) and fibrin glue. Typically, no packing is used because of the potential for raising the intraocular pressure in the case of a large orbital defect.
Discussion
The medial-intraconal EEA was successfully performed on all six patients in our cohort. Of these, total resection was achieved in four patients (67%) and a subtotal excision in one patient (17%). In the remaining patient, the surgery was performed for diagnostic purposes. In all five of the tumor resections, the patients experienced complete resolution of the presenting symptoms with no evidence of optic nerve injury or worsening of diplopia.
Several key anatomic principles must be followed for safe resection of orbital tumors with an endonasal approach. First, it is critical to avoid crossing the optic nerve. Thus, tumors that are localized to the superior/lateral orbit are contraindicated for an endonasal approach. Second, entry through the lamina papyracea should occur below the level of the ethmoidal foramina to avoid damage to the ethmoid arteries and reduce the risk of retrobulbar hemorrhage and vision loss. Finally, the dissection should occur between muscle groups rather than through individual muscles for preservation of function.
The endonasal corridor has some advantages over external approaches for medial/inferior lesions. The endonasal approach minimizes external scarring and preserves cosmesis. External approaches to lesions of the medial orbital require significant displacement of orbital structures including the globe. Given the deep, cone-shaped surgical window provided by the external approach, it also has the disadvantage of suboptimal visibility relative to the endonasal approach. In addition, external approaches to intraconal lesions may also require deinsertion of extraocular muscles, with subsequent impact on extraocular mobility. The added illumination and magnificence of the endoscope cannot be understated; however, the loss of three-dimensional perception may be disorienting to the surgeon who is unfamiliar with these endoscopic techniques.
Acknowledgments
Sponsorships: Kibwei A. McKinney, National Research Service Award T32 training grant for postdoctoral research in otolaryngology (T32DC005360). This funding source had no direct role in the design and conduct of this study. It provided salary support for Dr. McKinney during the time when this study was conducted.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Author Contributions
Kibwei A. McKinney, data acquisition, interpretation and analysis, and preparation of the manuscript; Carl H. Snyderman, planning of the neurosurgical aspects of the cases, data acquisition and analysis, and preparation of the manuscript; Ricardo L. Carrau, planning of the neurosurgical aspects of the cases, data acquisition and analysis, and preparation of the manuscript; Anand V. Germanwala, planning of the neurosurgical aspects of the cases, data acquisition and analysis, and preparation of the manuscript; Daniel M. Prevedello, planning of the neurosurgical aspects of the cases, data acquisition and analysis, and preparation of the manuscript; Susan T. Stefko, selection of surgical candidates, planning of the ophthalmologic aspects of the cases, data acquisition and analysis, and preparation of the final manuscript; Paul Gardner, surgical planning, data acquisition and analysis, and preparation of the manuscript; Amin B. Kassam, surgical planning, data acquisition and analysis, and preparation of the manuscript; Stephen A. Wheless, data acquisition and analysis, and preparation of the manuscript; Adam M. Zanation, surgical planning, data acquisition and analysis, and preparation of the manuscript.
Disclosures
Competing interests: Ricardo L. Carrau, speakers bureau, payment for travel: Storz Endoscopy.
References
- 1.Mercandetti M. Tumors, Orbital. [Accessed March 1, 2010];eMedicine Chapter. Last Updated February 5, 2010. Available at: http://www.emedicine.com/oph/topic758.htm.
- 2.Norris JL, Cleasby GW. Endoscopic orbital surgery. Am J Ophthalmol. 1981;91:249–52. doi: 10.1016/0002-9394(81)90183-5. [DOI] [PubMed] [Google Scholar]
- 3.Miller NR, Agrawal N, Sciubba JJ, et al. Image-guided transnasal endoscopic resection of an orbital solitary fibrous tumor. Ophthal Plast Reconstr Surg. 2008;24:65–7. doi: 10.1097/IOP.0b013e31815faa9d. [DOI] [PubMed] [Google Scholar]
- 4.Gerencer RZ, Patel U, Hunter C, et al. The role of endoscopic sinus surgery in the diagnosis and treatment of metastatic orbital carcinoid tumors. Ear Nose Throat J. 2007;86:157–61. [PubMed] [Google Scholar]
- 5.Lund VJ, Rose GE. Endoscopic transnasal orbital decompression for visual failure due to sphenoid wing meningioma. Eye. 2006;20:1213–9. doi: 10.1038/sj.eye.6702385. [DOI] [PubMed] [Google Scholar]


