Abstract
Background
Social networks may protect depressed elders against suicidal behavior. However, conflict in important relationships may undermine one’s sense of social support, potentially negating the protective effects. Thus, we investigated the role of chronic interpersonal difficulties and perceived social support in depressed elders with and without suicidal thoughts and attempts.
Methods
106 individuals aged 60 and older participated in this cross-sectional, case-control study: suicidal depressed, non-suicidal depressed and non-depressed elders. Following a detailed clinical characterization, we assessed perceived social support (Interpersonal Support Evaluation List), and chronic interpersonal difficulties (Inventory of Interpersonal Problems). Using general linear models, we explored the relationship between suicidal thoughts/attempts, social support, and chronic interpersonal difficulties. We also examined whether lower perceived social support explained the relationship between chronic interpersonal difficulties and suicidal thoughts/attempts.
Results
Suicidal depressed elders reported the lowest levels of perceived social support (belonging, tangible support, and self-esteem) and higher levels of chronic interpersonal difficulties (struggle against others and interpersonal hostility), compared to both non-suicidal depressed and non-depressed elders. The relationship between chronic interpersonal difficulties and suicidal behavior was partially explained by low perceived social support.
Conclusions
The experience of strong affects, interpersonal struggle, and hostility in relationships may undermine the sense of social support in depressed elders, possibly leading them to contemplate or attempt suicide. Depressed elders with a history of interpersonal difficulties need to be carefully monitored for suicidal behavior.
Keywords: aged; aged, 80 and over; suicide; suicide, attempted; social isolation; social support; interpersonal relations; personality; stress, psychological
INTRODUCTION
Elderly people have the highest suicide rates in almost every country, including the US. While depression, physical illness, and loss are known to precipitate suicidal behavior in the elderly (Conwell et al., 2002; Duberstein et al., 1998; Heikkinen and Lonnqvist, 1995; Luoma and Pearson, 2002), only a minority of older people with these risk factors attempt or complete suicide. Thus, clinicians need a better understanding of what makes elderly vulnerable to suicidal behavior in order to predict and prevent it.
Among other factors, social support networks have been suggested to have a buffering effect, protecting people from the impact of stressors (Krause and Jay, 1991; Sheldon Cohen, 1983). Elderly who have limited social support appear to be at higher risk for suicidal ideation (Raue et al., 2007; Rowe et al., 2006) and death by suicide (Duberstein et al., 2004b; Turvey et al., 2002). Social networks are protective, but perhaps not for everyone. According to Joiner’s interpersonal-psychological theory of suicide (Joiner, 2005), lack of belonging, resulting from unpleasant, unstable, and distant relationships, is a key contributor to suicide. We have also observed that elders who attempt suicide perceive social problems as threatening (Gibbs et al., 2009). In our clinic, we have observed that many depressed older people who attempt or seriously contemplate suicide experience discord in their relationships, perceiving them as sources of stress rather than support. Earlier psychological autopsy studies have also found that discord in relationships affected many elderly suicide victims (Beautrais, 2002; Duberstein et al., 2004a; Harwood et al., 2006). To the extent that it is possible to generalize results obtained from those who died by suicide to suicide attempters, they lend further weight to the idea that it is important to understand what factors affect the sense of social support in vulnerable depressed elders, potentially contributing to suicidal ideation and behavior.
To answer this question, we assessed perceived social support and chronic interpersonal difficulties in three groups: depressed elderly with and without suicide attempts or serious suicidal ideation and non-depressed elderly. We conceptualize chronic interpersonal difficulties as a marker of personality factors, which are likely to impact important relationships. Our focus on a very high-risk group of depressed elderly is consistent with the notion that these patients are most likely to possess vulnerabilities associated with suicide. In-person assessments allowed us to gather information on perceived social support and chronic interpersonal difficulties firsthand, eliminating the use of secondhand data inherent in psychological autopsy studies. We hypothesized that suicidal thoughts or attempts would be associated with lower perceived social support and higher levels of interpersonal discord, above and beyond the effects of depression. Finally, as elders with chronic interpersonal difficulties may strain their protective social networks, we hypothesized that low perceived social support would partly explain the relationship between interpersonal discord and suicide attempts or ideation.
METHODS
All participants and their significant others provided written informed consent as required by the University of Pittsburgh Institutional Review Board. A total of 106 elderly aged 60 and older with a score of 18 or greater on the Mini-Mental State Exam (MMSE) participated. Depressed patients were required to meet criteria for major depression, adjustment disorder with depressed mood, depression secondary to medical condition, or depressive disorder NOS using the Structured Clinical Interview of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition Axis I Disorders (SCID/DSM-IV). We screened 290 patients for eligibility in the suicidal depressed or non-suicidal depressed groups; of those 161 were ineligible, 42 refused to participate, and 87 gave consent and contributed to this analysis.
Suicidal Depressed Elderly
We recruited 29 suicidal participants from an inpatient psychogeriatric unit and a late-life depression clinic. Of these participants, 19 had attempted suicide, defined here as a self-injurious act with the intent to die (O’Carroll, 1996); 11/19 attempted suicide within a month of assessments, and 14/19, within a year; 11/19 had their first suicide attempt after age 60; 9/19 had repeat attempts. Suicide attempt history was verified by a psychiatrist, using the interview, medical records, information from the treatment team, and information from family or friends. We excluded participants with significant discrepancies between these sources, for example, patients whose self-injurious act may have been the result of an accidental drug overdose were excluded. An additional 10 participants had experienced suicidal ideation with a specific plan to take their life, as recorded in items 4 and 12 of the Beck Suicidal Ideation Scale, and this ideation was severe enough to trigger an inpatient admission or increased level of care. Twenty-five suicidal participants were inpatients and 4 were outpatients.
Non-Suicidal Depressed Elderly
In a similar fashion, we recruited 58 age-, gender-, and education-equated depressed, non-suicidal participants. Non-suicidal depressed participants had never experienced suicidal ideation or made an attempt during any lifetime episodes of depression, as reflected in their worst lifetime and current scores on the Beck Scale of Suicidal Ideation.
Non-Depressed Elderly
We recruited 19 age-, gender-, and education-equated non-depressed comparison participants from university and community primary care practices. These participants had no lifetime history of any DSM-IV Axis I disorder, suicidal ideation or suicide attempt.
Exclusion Criteria
We excluded elderly with bipolar disorder, schizophrenia, schizoaffective disorder, and with sensory disorders that precluded cognitive testing. —Although patients with dysthymia were included, no patients in the current sample had dysthymia without a current major depression diagnosis at the time of baseline assessments. Patients who received electroconvulsive therapy in the previous 6 months and those with neurological disorders, such as stroke, epilepsy, known neurodegenerative disorders, and brain tumors, were also excluded, as these conditions interfered with cognitive testing results. Lifetime and current substance abuse or dependence were not grounds for exclusion.
Assessments
We assessed participants’ perceived levels of social support using the Interpersonal Support Evaluation List (ISEL), which includes four sub-scales (appraisal, belonging, self-esteem, and tangible support) and also provides an overall measure of support (Cohen et al., 1985). The appraisal subscale of the ISEL is intended to measure the perceived availability of someone to talk to about one’s problems; the belonging subscale, the perceived availability of people one can engage in social activities with; the self-esteem subscale, the positive comparison when measuring one’s self against others; and the tangible subscale, perceived availability of material aid, such as having someone to drive you to a doctor’s appointment.
We used a shortened version of the Inventory of Interpersonal Problems (IIP), the IIP-15, to assess chronic interpersonal difficulties. The original scale was developed to identify chronic difficulties in interpersonal relationships and has been shortened for use as a screening measure for personality disorders (Morse, 2007). These interpersonal difficulties represent one of the best markers of personality disorders, which play a role in maintaining or exacerbating affective symptoms and may be an important focus of clinical attention in elderly with depression and suicidal behavior. Sub-scales on the IIP-15 include measures of interpersonal sensitivity, interpersonal ambivalence, and aggression. Interpersonal sensitivity items reflect strong affectivity and reactivity in interpersonal settings. Interpersonal ambivalence items suggest a struggle against others and an inability to join collaboratively with others. Aggression items capture active hostile interpersonal content (Horowitz et al., 1988).
Psychiatric diagnosis was made by trained study clinicians using the Structured Clinical Interview for DSM-IV Axis I Disorders – Patient Edition (SCID) (First M, 1995). SCID diagnoses were reviewed and verified with a minimum of two geriatric psychiatrists at consensus conferences. Depression severity was measured using the 16-item version of the 17-item Hamilton Rating Scale for Depression (HRSD) (Hamilton, 1960) (we excluded the suicide item, which is collinear with group status). Burden of physical illness was assessed with the Cumulative Illness Rating Scale adapted for Geriatrics (Miller et al., 1992). Hopelessness was measured by the Beck Hopelessness Scale (Beck et al., 1975b), and current suicidal ideation, by the Beck Scale of Suicidal Ideation (Beck et al., 1979). Medical lethality of attempt was measured using Beck’s Lethality Scale (LS) (Beck et al., 1975a), completed by an interviewer based on clinical examination, medical records, and information from the treatment team. This scale measures the medical lethality of a suicide attempt for one of the eight possible methods (sedative drugs, non-sedative drugs and other substances, shooting, immolation, drowning, cutting, jumping, hanging) on a scale from 0 (no or minimal damage) to 8 (death). All depressed participants were asked to nominate a significant other. These significant others were then approached for informed consent. Interviews with significant others focused on details of suicidal behavior and psychiatric history.
Procedures
Study participants were assessed within two weeks of inpatient admission or at the beginning of treatment as outpatients at the clinic. Participants continued to receive psychotropic medications as clinically indicated. The study assessments, including SCID interviews, were administered by trained study clinicians, all of whom were required to complete regular inter-rater reliability testing. In cases of in-patient admission, extensive reviews were conducted of patients’ clinical charts to determine past history and severity of suicide attempts. Any discrepancies between medical records and patient-reported histories were clarified with significant others. Intra-class correlation coefficients measuring interrater reliability among our assessors were: 0.92 for HRSD, 0.94 for CIRS-G, and 0.96 for MMSE. SCID diagnoses were discussed at consensus case conferences which included at least two board-certified psychiatrists. In our “best estimate” process we used comprehensive data from all available sources (patient interviews, records, and collateral history from significant others).
Statistical Analysis
We used SAS software version 9 (SAS Institute Inc., Cary, NC) for all analyses. Demographic and clinical measures were compared across the 3 groups using chi-square tests for categorical measures and analysis of variance (ANOVA) for continuous measures. Measures of perceived social support (ISEL) and chronic interpersonal difficulties (IIP) were analyzed across the three groups using ANOVA, co-varying for education. In the intervening variable analysis (Freedman and Schatzkin, 1992) of the role of social support in the relationship between chronic interpersonal difficulties and suicidality, we performed ANOVA with IIP score as the dependent variable and ISEL score as an independent variable, in addition to group. A diminished and non-significant effect size for the relationship between IIP score and group after the addition of the ISEL score to the model would signify that social support is a critical intervening variable.
RESULTS
Group characteristics
The three groups were similar in demographic characteristics and MMSE scores, although the burden of physical illness differed across groups, as non-depressed elders had lower levels of physical illness (omnibus ANOVA: p=0.039; all post-hoc comparisons: NS). Comorbid anxiety disorders and substance abuse/dependence were similarly prevalent in the two depressed groups. Suicidal depressed and non-suicidal depressed participants had similar levels of current depression severity, but suicidal elderly reported onset of depression at an earlier age (Table 1). Suicidal depressed elderly reported high levels of current suicidal ideation on the Beck Suicidal Ideation Scale (mean 17.8, SD= 7.1). For the 19 participants who had made a suicide attempt, mean medical lethality of the most recent attempt on the Beck Medical Lethality Scale was 4.2 (SD = 2) and respective mean suicide intent on the Beck Intent Scale was 17.3 (SD=5), indicative of medically serious and determined suicide attempts.
Table 1.
Demographic and Clinical Characteristics by Group
| Suicidal depressed (S) n=29 | Non-suicidal Depressed (D) n=58 | Non- depressed (C) n=19 | p | Post-hoc | |
|---|---|---|---|---|---|
| Age | 69.8 (7.8) | 72.1 (8.4) | 69.2 (8.6) | .28 | |
| %Men | 55 | 47 | 68 | .24 | |
| %White | 79 | 83 | 89 | .66 | |
| %Married %Widowed %Sep/Divorced |
52 34 7 |
48 26 20 |
63 21 11 |
.63 | |
| Education in years | 13.3 (3.4) | 14.3 (2.9) | 15.7 (3.0) | .083 | Non-significant (NS) |
| CIRS total | 8.4 (3.6) | 9.8 (3.7) | 7.5 (3.0) | .039 | NS |
| CIRS count | 5.1 (1.8) | 6.0 (2.0) | 4.8 (1.8) | .032 | NS |
| HRSD-Q3 | 20.5 (5.3) | 18.8 (3.9) | 2.8 (2.0) | .0001 | S,D>C |
| MMSE | 27.3 (2.1) | 27.3 (2.9) | 27.4 (1.7) | .99 | |
| Hopelessness | 8.7 (5.9) | 5.8 (5.5) | 1.8 (1.7) | .0001 | S>D>C |
| Age of depression onset | 47.9 (22.8) | 60.9 (16.7) | - | .004 | |
| %Recurrent | 48% | 49% | - | .93 | |
| Median duration of current episode in weeks | 55 | 72 | .52 | ||
| %Lifetime substance use disorder | 28% | 17% | - | .26 | |
| %Lifetime anxiety disorder | 55% | 67% | - | .27 | |
| Current Scale for suicidal ideation score | 17.8 (7.1) | - | - | ||
| Current Intent | 17.3 (5.0) | - | - |
Perceived social support
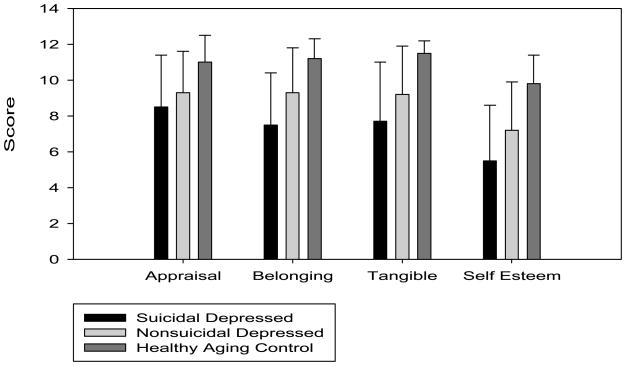
Suicidal depressed elderly reported the lowest levels of perceived overall social support as measured by the total ISEL score, followed by non-suicidal depressed elderly and non-depressed elderly (F[2, 99]=15.93, p=0.0001; post-hoc: suicidal depressed (S) < non-suicidal depressed (D) < non-depressed (C)) (Figure 1). Suicidal depressed elderly also reported the lowest levels of belonging (F[2, 99]=9.94, p=0.0001; post-hoc: S<D<C), tangible support (F[2, 99]=9.28, p=0.0002; post-hoc: S<D<C), and self-esteem (F[2, 99]=12.96, p=0.0001; post-hoc: S<D<C), as measured by the respective subscales of the ISEL. On the appraisal subscale, suicidal and non-suicidal depressed elderly had lower scores than non-depressed elderly (F[2, 99]=6.66, p=0.002; post-hoc: S,D<C), but the difference between the suicidal and non-suicidal depressed groups was not statistically significant.
Figure 1. Perceived Social Support, Depression, and Suicidal Behavior: Interpersonal Support Evaluation List subscores.
Figure illustrates self-reported levels of perceived social support by group, as measured by Interpersonal Support Evaluation List subscores. Lower scores indicate lower levels of perceived social support. Tukey post-hoc comparisons were used. Total ISEL score: F(2, 99)=15.93, p=0.0001. Appraisal: F(2, 99)=6.66, p=0.002. Belonging: F(2, 99)=9.94, p=0.0001. Tangible: F(2, 99)=9.28, p=0.0002. Self-esteem: F(2, 99)=12.96, p=0.0001.
Chronic interpersonal difficulties
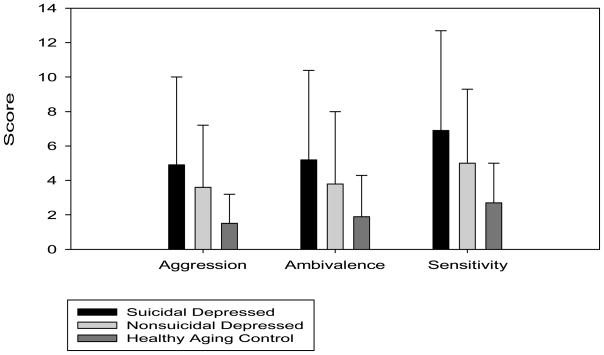
Suicidal depressed elderly reported significantly higher levels of chronic interpersonal difficulties as measured by the total IIP score when compared with non-depressed elderly (F[2, 93]=4.26, p=0.017; post-hoc: S>C) (Figure 2). This was also true for the aggression (F[2, 93]=3.4, p=0.038; post-hoc: S>C) and ambivalence (F[2, 93]=3.59, p=0.032; post-hoc: S>C) subscales of the IIP. The only subscale which did not show significant differences between the suicidal and non-depressed elderly groups was the sensitivity subscale (F[2, 93]=2.76, p=0.068). The level of chronic interpersonal difficulties in non-suicidal depressed participants was intermediate between the two other groups and did not significantly differ from them.
Figure 2. Chronic Interpersonal Difficulties, Depression, and Suicidal Behavior: Inventory of Interpersonal Problems scores and subscores.
Figure illustrates self-reported levels of chronic interpersonal difficulties by group, as measured by Inventory of Interpersonal Problems subscores. Lower scores indicate lower levels of chronic interpersonal difficulties. Tukey post-hoc comparisons were used. For IIP total score: F(2, 93)=4.26, p=0.017; Aggression: F(2, 93)=3.4, p=0.038; Ambivalence: F(2, 93)=3.59, p=0.032; Sensitivity: F(2, 93)=2.76, p=0.068.
Role of social support in the relationship between chronic interpersonal difficulties and suicide attempts/ideation
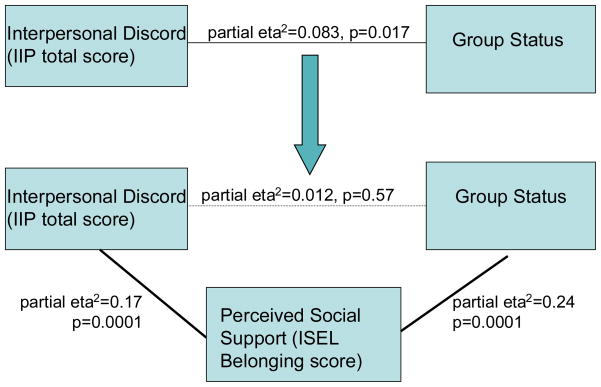
Lack of perceived social support was a significant intervening variable in the relationship between chronic interpersonal difficulties and suicidal behavior. When the ISEL total score (representing perceived social support) was entered into our general linear model, the relationship between IIP scores (representing chronic interpersonal difficulties) and group (suicidal, non-suicidal depressed, non-depressed) became weaker (partial η2 decreased from 0.10 to 0.008 and was no longer statistically significant (p=0.68); Fig. 3).
Figure 3. Lack of Social Support Explains the Effect of Interpersonal Discord on Suicidal Behavior.
Figure illustrates how a lack of social support explains the effect of interpersonal discord on group status. Groups include suicidal depressed elderly, non-suicidal depressed elderly, or non-depressed elderly. IIP: Inventory of Interpersonal Problems; ISEL: Interpersonal Support Evaluation List.
DISCUSSION
In our study, elderly with suicide attempts and severe suicidal ideation reported low perceived social support, as manifested in the lack of a sense of belonging, tangible support, and self-esteem. They also reported more chronic interpersonal difficulties, particularly expressed in interpersonal aggression and ambivalence. The relationship between chronic interpersonal difficulties and suicidal behavior was partly explained by low perceived social support. These findings are consistent with the idea that depressed elderly who have difficulty dealing with rejection or criticism, struggle against others and experience hostility in their relationships tend to feel a lack of social support, rendering them more likely to consider or attempt suicide.
Low perceived social support in late-life suicide
Old age is characterized by interpersonal losses and shrinking social networks, and psychological research suggests that successfully aging people rely on self-regulation strategies and smaller, closely knit social networks to deal with the sense that their life is limited (Lang and Carstensen, 2002). Conversely, psychological autopsy studies implicate lacking social supports and relationship problems in late-life suicide (Beautrais, 2002; Duberstein et al., 2004a; Duberstein et al., 2004b; Harwood et al., 2006). The perceived level of social support – the sense that one’s needs are met and that one is needed – may be more important for psychological well-being than the objective availability of people in the social network (Sheldon Cohen, 1983). Ideally, support is given unconditionally and no account is kept, however in real life the quality of support is affected by the degree of dependency and interdependency between parties. This may be particularly true for frail elderly who become increasingly dependent on family and friends. For example, physical illness may suddenly increase demands for practical and emotional support, and chronic illness may exhaust support and put a constant strain on relationships. Another factor explaining low levels of perceived social support could be that long-standing depression erodes relationships, with guilt and worthlessness further distorting the perception of available support. Our finding of earlier depression onset in suicidal elderly, both in previous research (Szanto et al., 2007) and in this sample, are consistent with this notion.
Interpersonal difficulties and suggestions for further research in late-life suicide
Our findings suggest that a persistent pattern of poor interpersonal relationships, interpersonal sensitivity, struggle against others and hostility in relationships may be a key factor undermining perceived social support in elderly at risk for suicide. Our research complements the findings of earlier psychological autopsy studies highlighting the contribution of conflict in important relationships to late-life suicidal behavior. In their psychological autopsy study of 100 suicides aged 60 and older, Harwood and colleagues found interpersonal problems – conflict being the most common – to be one of the three most frequent life problems associated with suicide, present in 55% of the cases and contributing to suicide in 31% (Harwood et al., 2006). Interestingly, however, interpersonal problems were no less frequent in matched controls, and no between-group differences were found. On the other hand, Duberstein and colleagues found that family discord was more common in 86 suicides aged 50 years and older than in matched controls – a difference that was no longer significant after accounting for current mental disorders (Duberstein et al., 2004a). Thus, one may conclude from these studies that while older people who die by suicide often experience conflict in their relationships, the mere presence of conflict does not specifically predict suicide. In this context, our findings of increased chronic interpersonal difficulties in suicidal elderly suggest that an enduring sense of interpersonal ambivalence and vulnerability may not only precipitate conflict but also increase its emotional impact on vulnerable individuals.
The suggestion that a persistent pattern of poor interpersonal relationships may be a key factor undermining perceived social support in elderly at risk for suicide raises the question of what contributes to this persistent pattern in the first place. Difficulties in interpersonal relationships can reflect personality factors, although our findings do not directly link personality disorders to attempted or contemplated suicide. The literature is also not clear as to what particular personality profiles predispose elderly to suicidal behavior. Some studies link late-life suicide to emotional restriction and rigidity: low openness to experience has been found to be more common in elderly who die by suicide than in mid-life suicide completers (Duberstein et al., 1994), and anxious and obsessional (anankastic) personality accentuation(Harwood et al., 2001) has been associated with death by suicide in late life. On the other hand, lack of openness to experience was not related to attempted suicide in depressed older adults (Duberstein et al., 2000) and was even found to be inversely associated with reported suicidal ideation (Heisel et al., 2006), indicating that risk factors for suicidal ideation, attempt, and death by suicide may differ. The presence of a personality disorder has been associated with suicide attempts and death by suicide among older adults (Harwood et al., 2001), although the prevalence of personality disorders among elders who attempt or die by suicide is lower than the figures reported for younger age groups (Appleby, 1999; Harwood et al., 2001; Marttunen, 1995). A recent study of older adults with major depressive disorder found that dependent personality disorder in men and antisocial personality disorder in women increased the odds of suicide attempt, although borderline and narcissistic personality disorders were not assessed (Bolton et al., 2008). In summary, while personality factors appear to play a role in late-life suicide, no firm conclusions can yet be drawn about traits or specific disorders that confer risk. This lack of agreement may indicate heterogeneity: it is possible that both emotionally restricted and emotionally unstable elderly are at risk. In this context, our data suggest that a dimensional assessment of personality and a focus on interpersonal function may help elucidate the pathways leading to late-life suicide.
Strengths and limitations
Our analyses benefited from a well-characterized clinical sample, which included elders with serious suicidal ideation and behavior. The inclusion of two control groups allowed us to account for the effects of depression. Our results were limited, however, by the relatively modest sample size and a cross-sectional, case-control design. Our cross-sectional design prevents us from drawing definitive conclusions about the relationship among chronic interpersonal difficulties, social support and suicidal behavior. In addition, it is possible, that a fourth, in this study unmeasured variable may account for interpersonal conflict, low social support, and suicidality. For example, impulsivity and emotion regulation difficulties (Wilson, 2007; Wilson et al., 2006) have been associated with suicide in young adults and in mid-life, which may also undermine interpersonal relationships and limit social support. In addition, while we recruited every in- and out-patient who met criteria for our study and agreed to participate, suicide attempters were over-represented on the in-patient unit, and so are in our sample, as well. Since our observations are naturalistic, we cannot conclude that low perceived social support and chronic interpersonal difficulties play a causal role in the emergence of suicidal ideation and behavior. It is possible that both are related to a third causal factor, such as emotional dysregulation, or poor problem-solving. Further, this design did not allow us to examine whether low social support mediated the effects of chronic interpersonal difficulties on suicidal behavior. However, since such a relationship is psychologically plausible, we felt that the intervening variable analysis performed here was an important initial step in identifying such a relationship, to be further tested in longitudinal studies. The lack of a categorical assessment of DSM-IV or ICD-10 personality disorders did not allow us to further examine the correlates of chronic interpersonal difficulties. Next, although the severity of current depression was not different between the two depressed groups, longitudinal follow-up data are necessary to rule out a higher cumulative burden of depression in suicidal elderly. Further, despite similar prevalence of substance use disorders in our depressed groups, we cannot rule out the possible effects comorbid substance use disorders on the relationships of suicidal participants based on this relatively modest sample. We should also note that while our suicidal participants were predominantly inpatients, the non-suicidal depressed participants were mostly oupatients. We feel that such a difference is mostly due to current admission criteria established by US third-party payers: suicidal ideation or attempt warrant admission, while serious depression by itself does not. Finally, it is unclear to what extent our findings generalize to older suicide victims.
Acknowledgments
K. Szanto’s NIMH career development award (MH070471) was the principal source of support for this work. Additional support was provided by P30 MH71944 (PI: C.F. Reynolds), the John A. Hartford Foundation and an NIMH career development award (MH086022; A.Y. Dombrovski), the American Foundation for Suicide Prevention (K. Szanto and A.Y. Dombrovski), and the UPMC Endowment in Geriatric Psychiatry (C.F. Reynolds).
Footnotes
CONFLICT OF INTEREST
None.
DESCRIPTION OF AUTHORS’ ROLES
Katalin Szanto designed the study. Katalin Szanto and Alexandre Dombrovski collected the data. Alexandre Dombrovski, Katalin Szanto, Jennifer Morse, and Patricia Houck planned the analyses, and Patricia R. Houck performed them. Katrin Harrison and Alexandre Dombrovski drafted the manuscript. Katalin Szanto, Jennifer Morse, Maryann Schlernitzauer, and Charles F. Reynolds, 3rd edited the manuscript.
References
- Appleby L, Cooper J, Amos T, Faragher B. Psychological autopsy study of suicides by people aged under 35. British Journal of Psychiatry. 1999;175:168–174. doi: 10.1192/bjp.175.2.168. [DOI] [PubMed] [Google Scholar]
- Beautrais AL. A case control study of suicide and attempted suicide in older adults. Suicide Life Threat Behav. 2002;32:1–9. doi: 10.1521/suli.32.1.1.22184. [DOI] [PubMed] [Google Scholar]
- Beck AT, Beck R, Kovacs M. Classification of suicidal behaviors: I. Quantifying intent and medical lethality. Am J Psychiatry. 1975a;132:285–287. doi: 10.1176/ajp.132.3.285. [DOI] [PubMed] [Google Scholar]
- Beck AT, Kovacs M, Weissman A. Hopelessness and suicidal behavior. An overview. Jama. 1975b;234:1146–1149. [PubMed] [Google Scholar]
- Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47:343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- Bolton JM, Belik SL, Enns MW, Cox BJ, Sareen J. Exploring the correlates of suicide attempts among individuals with major depressive disorder: findings from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2008;69:1139–1149. doi: 10.4088/jcp.v69n0714. [DOI] [PubMed] [Google Scholar]
- Cohen S, Mermelstein R, Kamarck T, Hoberman H. Measuring the functional components of social support. In: Sarason IG, Sarason B, editors. Social support: Theory, research and applications. The Hague: Martinus Nijhoff; 1985. pp. 73–94. [Google Scholar]
- Conwell Y, Duberstein PR, Caine ED. Risk factors for suicide in later life. Biological Psychiatry. 2002;52:193–204. doi: 10.1016/s0006-3223(02)01347-1. [DOI] [PubMed] [Google Scholar]
- De Leo D, Dello Buono M, Dwyer J. Suicide among the elderly: the long-term impact of a telephone support and assessment intervention in northern Italy. Br J Psychiatry. 2002;181:226–229. doi: 10.1192/bjp.181.3.226. [DOI] [PubMed] [Google Scholar]
- Duberstein PR, Conwell Y, Caine ED. Age differences in the personality characteristics of suicide completers: preliminary findings from a psychological autopsy study. Psychiatry. 1994;57:213–224. [PubMed] [Google Scholar]
- Duberstein PR, Conwell Y, Conner KR, Eberly S, Caine ED. Suicide at 50 years of age and older: perceived physical illness, family discord and financial strain. Psychol Med. 2004a;34:137–146. doi: 10.1017/s0033291703008584. [DOI] [PubMed] [Google Scholar]
- Duberstein PR, Conwell Y, Conner KR, Eberly S, Evinger JS, Caine ED. Poor social integration and suicide: fact or artifact? A case-control study. Psychol Med. 2004b;34:1331–1337. doi: 10.1017/s0033291704002600. [DOI] [PubMed] [Google Scholar]
- Duberstein PR, Conwell Y, Cox C. Suicide in widowed persons. A psychological autopsy comparison of recently and remotely bereaved older subjects. American Journal of Geriatric Psychiatry. 1998;6:328–334. [PubMed] [Google Scholar]
- Duberstein PR, Conwell Y, Seidlitz L, Denning DG, Cox C, Caine ED. Personality traits and suicidal behavior and ideation in depressed inpatients 50 years of age and older. Journals of Gerontology Series B-Psychological Sciences & Social Sciences. 2000;55:P18–26. doi: 10.1093/geronb/55.1.p18. [DOI] [PubMed] [Google Scholar]
- First MSR, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I Disorders. 1995. Patient Edition (SCID-I/P). Version 2.0 ed. [Google Scholar]
- Freedman LS, Schatzkin A. Sample size for studying intermediate endpoints within intervention trials or observational studies. Am J Epidemiol. 1992;136:1148–1159. doi: 10.1093/oxfordjournals.aje.a116581. [DOI] [PubMed] [Google Scholar]
- Gibbs LM, Dombrovski AY, Morse J, Siegle GJ, Houck PR, Szanto K. When the solution is part of the problem: problem solving in elderly suicide attempters. Int J Geriatr Psychiatry. 2009 doi: 10.1002/gps.2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harwood D, Hawton K, Hope T, Jacoby R. Psychiatric disorder and personality factors associated with suicide in older people: a descriptive and case-control study. Int J Geriatr Psychiatry. 2001;16:155–165. doi: 10.1002/1099-1166(200102)16:2<155::aid-gps289>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Harwood DM, Hawton K, Hope T, Harriss L, Jacoby R. Life problems and physical illness as risk factors for suicide in older people: a descriptive and case-control study. Psychol Med. 2006;36:1265–1274. doi: 10.1017/S0033291706007872. [DOI] [PubMed] [Google Scholar]
- Heikkinen ME, Lonnqvist JK. Recent life events in elderly suicide: a nationwide study in Finland. Int Psychogeriatr. 1995;7:287–300. doi: 10.1017/s1041610295002043. [DOI] [PubMed] [Google Scholar]
- Heisel MJ, Duberstein PR, Conner KR, Franus N, Beckman A, Conwell Y. Personality and reports of suicide ideation among depressed adults 50 years of age or older. J Affect Disord. 2006;90:175–180. doi: 10.1016/j.jad.2005.11.005. [DOI] [PubMed] [Google Scholar]
- Horowitz LM, Rosenberg SE, Baer BA, Ureno G, Villasenor VS. Inventory of interpersonal problems: psychometric properties and clinical applications. J Consult Clin Psychol. 1988;56:885–892. doi: 10.1037//0022-006x.56.6.885. [DOI] [PubMed] [Google Scholar]
- Joiner T. Why People Die by Suicide. Cambridge: Harvard University Press; 2005. What Roles Do Genetics, Neurobiology, and Mental Disorders Play in Suicide Behavior? pp. 172–202. [Google Scholar]
- Krause N, Jay G. Stress, social support, and negative interaction in later life. Research on Aging. 1991;13:333–363. [Google Scholar]
- Lang FR, Carstensen LL. Time counts: future time perspective, goals, and social relationships. Psychol Aging. 2002;17:125–139. doi: 10.1037/0882-7974.17.1.125. [DOI] [PubMed] [Google Scholar]
- Luoma JB, Pearson JL. Suicide and marital status in the United States, 1991–1996: is widowhood a risk factor? American Journal of Public Health. 2002;92:1518–1522. doi: 10.2105/ajph.92.9.1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marttunen M, Henriksson MM, Aro HM, Heikkinen ME, Isometsä ET, Lönnqvist JK. Suicide among female adolescents: characteristics and comparison with males in the age group 13 to 22 years. Journal of the American Academy of Child and Adoloscent Psychiatry. 1995;34:1297–1307. doi: 10.1097/00004583-199510000-00015. [DOI] [PubMed] [Google Scholar]
- Miller MD, Frank E, Cornes C, Houck PR, Reynolds CF., 3rd The value of maintenance interpersonal psychotherapy (IPT) in older adults with different IPT foci. Am J Geriatr Psychiatry. 2003;11:97–102. [PubMed] [Google Scholar]
- Miller MD, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry Res. 1992;41:237–248. doi: 10.1016/0165-1781(92)90005-n. [DOI] [PubMed] [Google Scholar]
- Morse JP, PA Screening for personality disorders. Journal of Personality Disorders. 2007;21:179–198. doi: 10.1521/pedi.2007.21.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatr Serv. 2001;52:828–833. doi: 10.1176/appi.ps.52.6.828. [DOI] [PubMed] [Google Scholar]
- O’Carroll P, Berman AL, Maris RW, Mosciki EK, Tanney BL, Silverman MM. Beyond the Tower of Babel: A nomenclature for suicidology. Suicide Life Threat Behav. 1996;26:237–252. [PubMed] [Google Scholar]
- Raue PJ, Meyers BS, Rowe JL, Heo M, Bruce ML. Suicidal ideation among elderly homecare patients. Int J Geriatr Psychiatry. 2007;22:32–37. doi: 10.1002/gps.1649. [DOI] [PubMed] [Google Scholar]
- Rowe JL, Conwell Y, Schulberg HC, Bruce ML. Social support and suicidal ideation in older adults using home healthcare services. Am J Geriatr Psychiatry. 2006;14:758–766. doi: 10.1097/01.JGP.0000218324.78202.25. [DOI] [PubMed] [Google Scholar]
- Sheldon Cohen HMH. Positive Events and Social Supports as Buffers of Life Change Stress<sup>1</sup>. Journal of Applied Social Psychology. 1983;13:99–125. [Google Scholar]
- Szanto K, et al. Emergence, persistence, and resolution of suicidal ideation during treatment of depression in old age. J Affect Disord. 2007;98:153–161. doi: 10.1016/j.jad.2006.07.015. [DOI] [PubMed] [Google Scholar]
- Turvey CL, et al. Risk factors for late-life suicide: a prospective, community-based study. American Journal of Geriatric Psychiatry. 2002;10:398–406. [PubMed] [Google Scholar]
- Wilson S, Stanley B, Oquendo MA, Goldberg P, Zalsman G, Mann JJ. Comparing impulsiveness, hostility, and depression in borderline personality disorder and bipolar II disorder. Journal of Clinical Psychiatry. 2007;68:1533–1539. doi: 10.4088/jcp.v68n1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson ST, Fertuck EA, Kwitel A, Stanley MC, Stanley B. Impulsivity, suicidality and alcohol use disorders in adolescents and young adults with borderline personality disorder. Int J Adolesc Med Health. 2006;18:189–196. doi: 10.1515/ijamh.2006.18.1.189. [DOI] [PubMed] [Google Scholar]