Abstract
American Indian (AI) adolescents experience higher rates of suicide and psychological distress than the overall U.S. adolescent population, and research suggests that these disparities are related to higher rates of violence and trauma exposure. Despite elevated risk, there is limited empirical information to guide culturally appropriate treatment of trauma and related symptoms. We report a pilot study of an adaptation to the Cognitive Behavioral Intervention for Trauma in Schools in a sample of 24 AI adolescents. Participants experienced significant decreases in anxiety and PTSD symptoms, and avoidant coping strategies, as well as a marginally significant decrease in depression symptoms. Improvements in anxiety and depression were maintained 6 months post-intervention; improvements in PTSD and avoidant coping strategies were not. Feasibility, appropriateness, and acceptability of CBITS are discussed in the context of efforts to develop culturally sensitive interventions for AI youth.
Keywords: Adolescent, American Indian, CBT, Evidence-Based Intervention, Mental Health, Trauma
Introduction
American Indians (AI) and Alaska Natives (AN) experience higher rates of psychological symptoms than the overall population of the United States, including the highest rate of suicide among 15 to 24 year-olds (Health United States, 2004). A growing body of evidence suggests that many health disparities experienced by AI/AN youth are related to disparities in violence and trauma exposure. AI/ANs witness more than twice as many traumatic events as non-Hispanic white populations (U.S. Department of Health and Human Services, Office of the Surgeon General, & SAMHSA, n.d.). Among AI/AN children, the victimization rate is double that of non-Hispanic white children (U.S. Department of Justice Bureau of Justice Statistics, 2004), and they are at 2.5 times the risk for experiencing trauma (National Center for Children in Poverty, 2007). Tribally-based studies support these findings (Jones, Daughinais, Sack, & Somervell, 1997; Manson, et al., 1996).
Such high rates of traumatic experiences may render AI/ANs especially susceptible to post-traumatic stress disorder (PTSD), and indeed it has been found that lifetime rates of PTSD are 2–3 times that of the general population (Beals, et al., 2005). In several studies, these high rates of traumatic loss and trauma exposure have been linked to PTSD (Deters, Novins, Fickenscher, & Beals, 2006; Jones, et al., 1997) and substance abuse (Boyd-Ball, Manson, Noonan, & Beals, 2006; Kilpatrick, et al., 2000) among AI/AN youth. The link between trauma exposure and depression and anxiety in a diversity of adolescent populations has been established (Martinez & Richters, 1993; M. Singer, Anglin, Song, & Lunghofer, 1995; Zinzow, et al., 2009). In addition, post-traumatic stress has been found to mediate the relationship between trauma and depression/anxiety symptoms among diverse youth in juvenile detention (Kerig, Ward, Vanderzee, & Moeddel, 2009).These empirical links are less well-established for AI/AN adolescents, which may be in part due to the limited research in this area.
Empirical evidence suggests that active and support-seeking coping strategies may be related to decreased depression and anxiety symptoms among adolescents in the U.S. (Wright, Banerjee, Hoek, Rieffe, & Novin). There is also some evidence of this relationship among AI youth (Rieckmann, 2001). Conversely, avoidant coping has been linked to increased PTSD and anxiety symptoms among adolescents who have experienced trauma (Pina, et al., 2008).
Very little empirical data exists for mental health interventions developed specifically with and/or for AI/AN youth. They are nearly excluded from the youth treatment outcome literature. In part, this is because studies documenting the effectiveness of mental health treatments have been done almost entirely on White populations. Miranda and colleagues were unable to find any studies evaluating outcomes of mental health care for American Indians (Miranda, et al., 2005). There is a small, but growing evidence-base for prevention work with AI/AN youth (Hawkins, Cummins, & Marlatt, 2004), but limited evidence-based treatments (EBTs) for AI/AN youth with symptoms of trauma or PTSD have been developed (Huey & Polo, 2008). Morsette and colleagues (2009), however, have published preliminary support, based on case studies of four AI youth, for an adaptation of Cognitive Behavioral Intervention for Trauma in Schools (CBITS). Their data suggested that CBITS had promise in reducing PTSD and depression symptoms among three of the four treatment completers. AI/AN community members and the literature on AI/AN mental health have identified a need for the development of culturally-based mental health interventions that build upon traditional healing practices already successful within communities, and which include a recognition of the impacts of past and current oppressive policies and intergenerational trauma (Brave Heart, 2003; Gone & Alcantara, 2007). Taken together, these limitations and critiques suggest that we cannot take for granted the appropriateness of EBTs for these populations, and furthermore that efforts to adapt, implement and evaluate EBTs be undertaken in close collaboration with AI/AN communities.
Accessibility to services is another barrier for rural AI/AN communities in need of mental health care. Mental health services in many areas are very limited, and it has been shown that upwards of 75% of rural youth do not get the mental health treatment they need (Ringel & Sturm, 2001). Addressing violence in childhood and adolescence may be a powerful tertiary prevention strategy, especially considering the link between exposure to violence in childhood and the experience of future violence, PTSD, and other mental health disturbances (Duncan, Saunders, Kilpatrick, Hanson, & Resnick, 1996). However, this can work only if interventions are delivered to rural areas where they are needed the most. Providing services within school-based health centers can be an effective and de-stigmatizing way to direct services to youth who would otherwise not be able to access much needed care (Miranda, et al., 2005).
In sum, violence exposure and trauma are negatively impacting the mental health and well-being of AI/AN adolescents. However, limited research exists on effective trauma-focused interventions for these populations. Given the high rates of exposure to traumatic stress among AI/AN youth, it is essential to implement culturally appropriate, accessible interventions and to begin to establish an evidence base for them. There are several options for these efforts: to attempt to empirically validate existing traditional healing practices; to co-develop and test interventions that bring together strengths from traditional healing practices and evidence-based interventions; or to rigorously test feasibility, acceptability, and effectiveness of adaptations to existing evidence-based interventions (see Gone, 2009, for some discussion of merits and limitations of these approaches for AI populations). This study exemplifies the latter approach by adapting, implementing, and evaluating an evidence-based, trauma-focused intervention (CBITS) in three American Indian communities in the Southwestern United States. Our literature review highlights that AI youth experience higher rates of PTSD, depression, and anxiety symptoms due to their elevated trauma exposure; CBITS has been shown to be effective in reducing depression and PTSD symptoms as well as other elements of youths’ psychosocial functioning. We therefore hypothesized that the adapted CBITS intervention would decrease participants’ symptoms of PTSD, depression, and anxiety over time. We also explored the impact of CBITS on coping strategies, as well as characteristics of participants that might result in variability in the effects of the intervention.
Method
Setting
The study was implemented in 2005 in three American Indian communities served by the University of New Mexico Prevention Research Center (UNM PRC) school-based health centers (SBHCs). Through a partnership established with the communities in 1983, the SBHCs address student and family health issues through primary prevention and clinical services.
Intervention
Data provided by the Indian Health Service (IHS) facilities of the three communities in which this study occurred indicated that there is a need for improvement in access, coordination, and follow-up services in the behavioral health care system designed for AI youth. In order to address the mental health needs of AI youth in a culturally appropriate manner, the purpose of THRIVE (Teen Health Resiliency Intervention for Violence Exposure) was to adapt, pilot, and evaluate an evidence-based school intervention to address trauma resulting from violence exposure in these AI communities. In response to needs implied by the IHS data, and expressed by youth, parents, teachers, and service providers in the three American Indian communities, we searched for effective school-based interventions for youth exposed to violence. At the time, we identified only one evidence-based intervention: Cognitive Behavioral Intervention for Trauma in Schools (CBITS). In a randomized-controlled trial, a diverse sample of urban adolescents who participated in CBITS experienced significant reductions in PTSD and depression symptoms (Stein, et al., 2003). However, it was developed for urban youth in Los Angeles and therefore needed to be adapted for use with rural AI youth.
As members of the National Child Traumatic Stress Network (NCTSN), we selected a cognitive-behavioral approach to addressing trauma among AI youth in consultation with two other AI-focused NCTSN sites (Montana Center for Investigation and Treatment of Childhood Trauma and Indian Country Child Trauma Center in Oklahoma). Although evidence related to the use of cognitive-behavioral treatment interventions with AI youth was limited, we found that suicide and substance abuse prevention interventions with AI youth had employed cognitive behavioral approaches that focused on improving coping and problem solving (LaFromboise & Bigfoot, 1988; Schinke, 1985). CBITS was specifically designed to treat children from ethnically diverse populations; one of our primary goals was to determine feasibility and appropriateness of this evidence-based intervention for AI youth. Both our New Mexico site and the Montana site selected CBITS for simultaneous adaptation and implementation (see Morsette et al., 2009, for Montana’s results and Ngo et al., (2008), for a brief discussion of some of the adaptations made). CBITS is intended for use with groups of adolescents ages 11–15 who are experiencing symptoms of PTSD as a result of exposure to a significant trauma. CBITS also targets depressive and general anxiety symptoms that are often experienced with PTSD symptoms. CBITS involves six techniques geared toward making maladaptive thoughts and behaviors more functional: education, relaxation training, cognitive therapy, real life exposure, stress or trauma exposure, and social problem-solving (see Table 1 for descriptions of each session). The intervention consisted of 10 weekly meetings in groups of 5–10 students from the same school and was led by a member of the Teen Center clinical staff and a co-facilitator. The intervention also included one or two individual meetings between each youth and one of the clinicians, two parent meetings, and one teacher session. All youth meetings (group and individual) occurred during school hours. In order to minimize academic disruption, group sessions were rotated among the class periods. See Jaycox (2004) for a complete description of the CBITS intervention.
Table 1.
Description of the Manualized CBITS Curriculum and Adaptations
| CBITS Manualized Treatment | Adaptations Made | |
|---|---|---|
| Group Session 1 |
|
|
| Group Session 2 |
|
|
| Individual Sessions |
|
|
| Group Session 3 |
|
|
| Group Session 4 |
|
|
| Group Session 5 |
|
|
| Group Session 6 |
|
|
| Group Session 7 |
|
|
| Group Session 8 |
|
|
| Group Session 9 |
|
|
| Group Session 10 |
|
|
| Parent Education Session 1 |
|
|
| Parent Education Session 2 |
|
|
Implementation
We sought and obtained approval from the Tribal or Chapter Councils and the School Boards in the three communities, school administrators and teachers at each of the schools, our university institutional review board and one tribal institutional review board. This involved numerous community presentations and written documents from which we received support and feedback from tribal leaders, school board members, service providers, and community members that addressing trauma and violence exposure were priorities. One of the stipulations we agreed to was that we would maintain confidentiality at the community level in all presentations, reports, or publications. We also shared the revised curriculum and results of the study with tribal officials, school personnel, and other community members.
At each school, there was a team of two facilitators who worked together to implement the intervention. Because part of our goal was to make the intervention sustainable within the schools, each team consisted of a clinician from our SBHCs and a school or tribal employee who received facilitator training from our clinicians. Two of the SBHCs clinicians were masters-level licensed clinical social workers (LISWs) and one was a PhD licensed clinical psychologist. Their co-facilitators were a PsyD licensed clinical psychologist (paired with one of the LISW), a masters-level clinical psychologist (paired with the other LISW), and a Licensed Alcohol and Drug Abuse Counselor (paired with the PhD licensed clinical psychologist). One of the SBHC facilitators participated in formal CBITS training, and she then trained the other facilitators.
All facilitators received the CBITS manual, as well as an addendum that included written adaptations (supplements/changes) for each session. Fidelity to the adapted intervention was assessed by Facilitator Implementation Forms (FIF), completed after each session (because we had made adaptations to the intervention, we wanted to obtain additional data on feasibility of maintaining fidelity of the model). These forms documented whether all components and objectives of each session were covered, any omissions or changes, participants’ reactions to the session, and other facilitator reflections. Although fidelity ratings were not calculated, analyses of the FIF indicated that all session objectives and activities were completed. Sometimes objectives or activities required more time than specified, which resulted in completing certain activities in a subsequent session. FIF also documented additional material included in sessions.
Adaptations and special considerations
Resnicow and colleagues (Resnicow, Baranowski, Ahluwalia, & Braithwaite, 1999; Resnicow, Soler, Braithwaite, Ahluwalia, & Butler, 2000) have described the process of designing, tailoring or adapting interventions to be culturally sensitive as occurring at either surface structure or deep structure levels, where surface structure considerations are those which affect the ‘fit’ of the intervention to the context. For example, a change of materials, channels of delivery, or settings constitute surface structure changes, which would result in a culturally targeted intervention. Deep structure changes, however, are those that attend to cultural, social, psychological, environmental, and historical factors which may be unique to a particular racial or ethnic group. For instance, deep structure changes could include incorporating cultural beliefs about the way in which trauma affects health, the causes of trauma-related illnesses, and effective cultural practices for treating these problems. These types of changes would result in a culturally tailored intervention. While our adaptation process included some deep structure changes, our primary emphasis was on surface structure changes in order to determine whether an existing intervention designed specifically for youth of diverse backgrounds was feasible, acceptable, appropriate, and effective for AI youth.
We engaged in an adaptation process that involved two formal meetings attended by our SBHC prevention and clinical staff (three AI and two non-AI), two research team members (one AI and one non-AI), and two community members from each of the three AI communities (including at least one person from each community who was knowledgeable in traditional cultural practices and teachings). During these meetings, we discussed and made adaptations to each of the ten group sessions, the individual sessions, and parent sessions of the curriculum. A “practice” implementation of the curriculum was also conducted at one of the three schools in order to further explore the need for other adaptations.
Table 1 outlines the adaptations made prior to implementing CBITS in this sample. These included surface structure changes such as removing inadvertently offensive, Eurocentric examples of cognitive restructuring, as well as deep structure changes such as utilizing stories and examples based upon participants’ cultural teachings and addressing differing cultural beliefs about how long it is acceptable to talk about someone after they have died. For example, if a student’s trauma related to a death, it was important to explore how to address this in a culturally appropriate manner in the group. This exploration involved talking with the student and his or her parents, as well as including certain culturally specific questions in our initial screening to provide clinicians with knowledge about participants’ cultural and spiritual beliefs because we recognized the heterogeneity within each AI community around ethnic identity, religious/spiritual beliefs, and adherence to traditional practices.
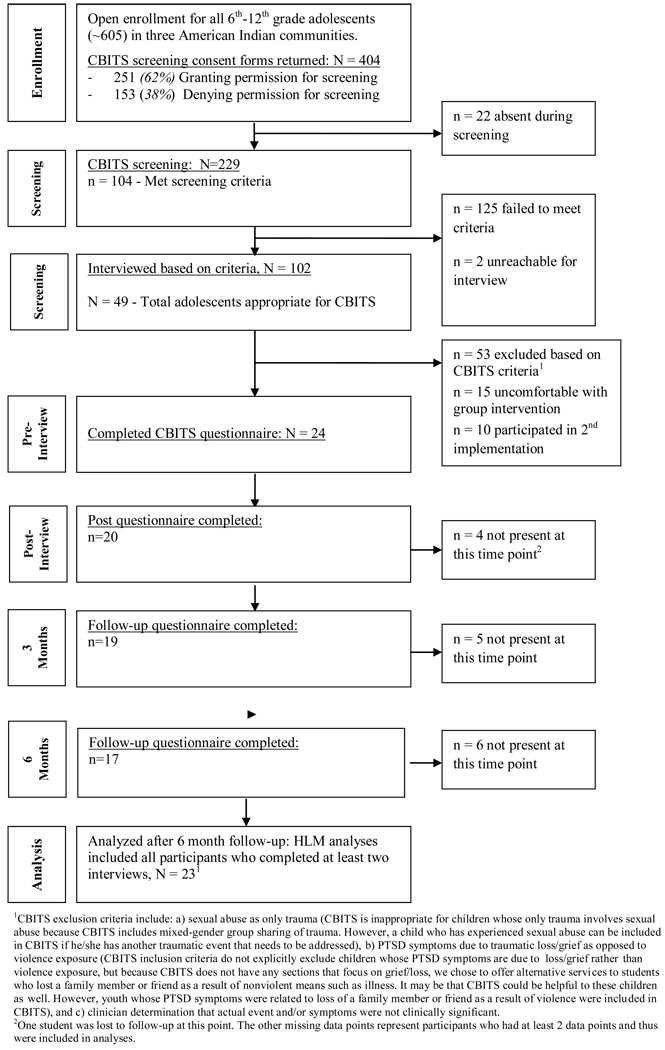
Participants
Figure 1 provides a detailed break-down of the flow of the study. Of approximately 650 adolescents in 6th–12th grade in our three communities, 229 were screened. With parental consent and youth assent, groups of about 25 students filled out a questionnaire at school which asked about seeing or experiencing violent events and any distress that they felt because of those events. Our goal was to recruit all students in the three communities for screening. Toward this end, an AI member of our research team visited each English class at all three schools (English is a required subject) to explain the study. Each student was given a recruitment flyer and a consent/assent form for screening. We provided $10 incentives to students who returned completed consent/assent forms, regardless of whether they and their parent/guardian signed yes or no, if 90% of their English class returned the forms.
Figure 1.
THRIVE intervention flowchart.
Of the 229 students we screened, 104 (45%) had experienced clinically significant levels of both violence exposure and PTSD symptoms. The SBHC clinicians individually interviewed 102 of the 104 students. They determined that 49 students were appropriate for CBITS; the other 53 students were excluded based upon CBITS criteria (see Figure 1). At the end of the individual clinical interviews, the SBHC clinicians discussed the intervention with the 49 students for whom CBITS was appropriate. Fifteen of the 49 eligible students stated that they did not want to participate in a group intervention. If students indicated they were interested in participating, the clinician gave them a consent/assent form for the intervention to share with their parents, and asked students for their parents’ contact information. Most students returned the consent/assent forms on their own; SBHC clinicians called and/or visited a few parents to obtain consent. The percentage of youth who screened into the intervention but did provide parental consent and/or assent (31%) is somewhat higher than Stein et al.’s (2003) rate of 21%.
Overall, 24 students from the three communities were enrolled in the first implementation of the CBITS program in spring 2005. Of the 24 intervention participants, 23 were included in analyses. The other participant completed the intervention but did not participate in quantitative assessment after the pre-intervention time point. All 23 participants were AI (participants could check multiple boxes for racial/ethnic identification. In addition to AI, two students checked Hispanic and one student checked White). Participants also provided their tribal affiliations. Three Southwestern AI tribes were represented in our sample. Youth had a mean age of 13.39 (range 12–15). Seven participants were male and 16 were female.
Measures
We utilized the screening and outcome measures recommended by Stein and colleagues (2003) for use with CBITS implementation and evaluation. In addition, based on the focus in CBITS on problem-solving and coping, as well as community advisory input regarding the overemphasis of negative mental health within AI communities and the importance of including positive, strengths-based competencies, we added a measure of children’s coping strategies. Although not all measures had been validated with AI children, they were selected by Stein and colleagues specifically for use with racially, culturally, and linguistically diverse populations. We held two formal meetings to review the measures for their appropriateness, including a review of all individual items. The meetings included three AI and 3 non-AI research team members, and at least two community members from each of the communities. We removed one item from the MASC and we made minor wording changes to two items. Next, we piloted the measures with ten AI youth. Based on our pilot-testing and consultation with Stein, we decided to use short versions of several of the scales because participants were fatigued with the large number of items and were therefore not providing accurate responses. The written screening and assessment instrument included the following measures:
Recent Exposure to Violence Scale is a measure of adolescents’ exposure to violence in the past year that has high reliability (M. Singer, et al., 1995). The short 9-item form includes questions about witnessing violence, experiencing violence, and being threatened. It was adapted from the full scale by Stein and colleagues (2003), who called the adapted version the Life Events Scale (range 0 – 27). This measure was used by Stein et al. (2003) and in our study for intervention screening only. Reliability (Cronbach’s alpha) for this scale in our sample ranged (across the four time points) from .67 to .86.
Childhood PTSD Symptom Scale (CPSS) is a 17-item child self-report measure, which showed good psychometric characteristics, including test-retest reliability, internal consistency, and discriminant validity in its validation study (Foa, Treadwell, Johnson, & Feeny, 2001). The short 7-item version of this measure was adapted and validated by Stein and colleagues (2003) and has a range of 0 – 21. The CPSS was used for screening and as an outcome measure. Reliability for this scale in our sample ranged from .72 to .91.
Children’s Depression Inventory (CDI) is a widely used measure of depression in children that assesses cognitive, behavioral, and affective symptoms. It has good test-retest reliability and validity (Kovacs, 1992). The short form has 10 items (range 0 – 30). Reliability for this scale in our sample ranged from .84 to .92.
Multidimensional Anxiety Scale for Children (MASC) assesses cognitive, physical, emotional, and behavioral aspects of anxiety. It has good internal reliability, test-retest reliability, convergent and divergent validity, and discriminant validity (March & Parker, 1999). The short form has 10 items (range 0 – 30). Cronbach’s alphas in our sample ranged from .77 to .90.
Children’s Coping Strategies Checklist is a self-report measure of children’s coping efforts across four dimensions: active coping, distraction, avoidance, and support seeking strategies. It has high internal consistency (Ayers, Sandler, West, & Roosa, 1996). In our sample, reliabilities for the four shortened subscales were good (range of .72 to .88).
Design and Analysis
In order to determine the feasibility, acceptability, and appropriateness of the intervention, we tracked eligibility and recruitment of participants and conducted separate focus groups with youth participants, facilitators, and community members. We employed a within-group longitudinal design with four time points; participants were assessed on outcome measures prior to beginning the intervention, at the end of the 10-week intervention, and at two follow-up time points 3 and 6 months post-treatment. A longitudinal design allows for an in-depth understanding of the processes at work and can explore mediating effects and potential moderators, such as individual characteristics of participants. When examining the impact of an intervention, it is important to understand individuals’ growth trajectories, which are obscured in group-comparison designs (Nugent, 1996). We worked to strengthen our quasi-experimental design by collecting data at four time points which produces observable patterns of change, and allows for exploration of whether effects persist over time. We tested three statistical hypotheses:
Hypothesis 1: Participants would show significant decrease in PTSD symptoms from pre-treatment through the final follow up time point.
Hypothesis 2: Participants would show significant decrease in anxiety symptoms from pre-treatment through the final follow up time point.
Hypothesis 3: Participants would show significant decrease in depression symptoms from pre-treatment through the final follow up time point.
Additionally, we explored the effects of the intervention on participants’ coping strategies. Finally, variability in initial status and growth trajectories was examined across participants and over time for all outcome variables. This variability reflects that participants may not have similar symptom levels prior to the intervention, and that they may not demonstrate similar patterns of change over time. In those cases where this was true, we attempted to find individual-level variables that accounted for this variability.
In order to test these hypotheses, growth curve modeling was implemented using hierarchical linear modeling or HLM (Raudenbush & Byrk, 2002). This technique is feasible with a minimum of 20 individuals (Kreft & De Leeuw, 1998) and has been successfully conducted with small samples in a variety of fields. HLM is more flexible in handling missing data than traditional parametric approaches, as it can estimate trajectories for participants missing data at a particular time point.
Conceptually, growth curve modeling was done for two reasons: first, to find the best fitting ‘average change’ function, which is indicated by the significance of the fixed effects. A significant linear fixed effect, for example, indexes average change of a linear form across all participants. A significant quadratic fixed effect describes average change of a quadratic form, which can mean that the observed linear change is speeding up or slowing down, or can indicate a reversal of the linear change altogether. This pattern may be expected in studies with extended follow-up, as symptom levels may decline from baseline during and/or immediately post-treatment, but may rise again as time from treatment increases. Secondly, HLM analyses enabled us to detect individual differences in change. The significance of the random effects indexes significant variability across participants in the observed fixed effects, indicating that participants are different in their initial status, linear growth rates, or quadratic growth rates.
Data were screened for relevant assumptions, and found acceptable. The process of modeling proceeded in an iterative fashion: the best fitting level 1 model was arrived at by first fitting a baseline model and establishing its fit to the data. Then a fully parameterized model, including linear and quadratic fixed and random effects, was fit and its fit was compared to the baseline model. The process involved fitting decreasingly complex models to the data until the model which best fit the observed data was found. Deviance statistics were used to determine the combination of fixed and random effects that best fit the data.
Second, level 2 predictors were added to explain significant variability in the random effects at level 1, if present. Because there were no specific hypotheses regarding level 2 predictors, we chose the possible explanatory variables of sex, age, and school affiliation, which were tested for significance one at a time. We included school affiliation because each school was in a different tribal community and had different intervention facilitators, which therefore could constitute important explanatory variability. All modeling used full maximum likelihood estimation, and models were centered at baseline.
The effect of primary interest in this study is the effect of the intervention over time. For this reason, as an effect size measure, we report the percent of variance explained (PVE) or pseudo-R2 (J. D. Singer & Willett, 2003) by the best fit level 1 model relative to a level 1 intercept-only model. This can be conceptualized as an R2 measure, which represents the percent of variance explained by the addition of time to the model.
Results
Feasibility, Acceptability, and Appropriateness
In order to assess the feasibility, acceptability, and appropriateness of the intervention, we examined our recruitment efforts in terms of willingness to complete screening (parental consent and child assent), appropriateness of the intervention for adolescent needs (clinical interviews), and adolescent interest in participating in the intervention if the screening criteria were met (refusal rate). We also examined intervention attendance and completion, and participant, parent, and facilitator feedback. Our findings (see Figure 1) indicate concerns with the acceptability of the screening to adolescents and their parents, appropriateness of the intervention given the need to exclude so many youth, acceptability of the group intervention for adolescents, and overall feasibility of recruitment. However, for those who did participate, intervention session attendance and completion was good; all 24 participants completed the intervention and 71% of participants attended 8 or more of the 10 sessions. Furthermore, of the 96 potential assessments (24 participants at four time points), 81 (84%) were completed. Separate focus groups with participants and facilitators suggested that adolescents enjoyed the intervention, felt they benefited, and would participate in a similar group in the future, although clinicians found recruitment efforts and assessment procedures somewhat burdensome.
Outcomes
Descriptive statistics for all outcome variables are shown in Table 2. Means and standard deviations reported are for all of the participants present at each time point for each measure.
Table 2.
Means (Standard Deviations) for All Outcome Measures at Each Time Point
| Scale | Pre | Post | 3-month | 6-month |
|---|---|---|---|---|
| PTSD Symptoms | 9.33 (3.59) | 7.40 (3.47) | 7.95 (6.05) | 10.65 (7.34) |
| Anxiety Symptoms | 13.29 (6.50) | 9.64 (5.07) | 10.41 (7.12) | 10.34 (7.42) |
| Depression Symptoms | 16.06 (3.97) | 14.64 (4.52) | 15.08 (5.21) | 15.44 (8.34) |
| Active Coping | 1.63 (.70) | 1.34 (.62) | 1.38 (.68) | 1.47 (.86) |
| Support Seeking Coping | 1.31 (.88) | 1.20 (.59) | 1.32 (1.02) | 1.32 (1.06) |
| Avoidant Coping | 1.83 (.80) | 1.50 (.73) | 1.47 (.92) | 1.65 (.86) |
| Distraction Coping | 1.83 (.83) | 1.65 (.83) | 1.76 (.73) | 1.65 (.86) |
Hypotheses 1–3
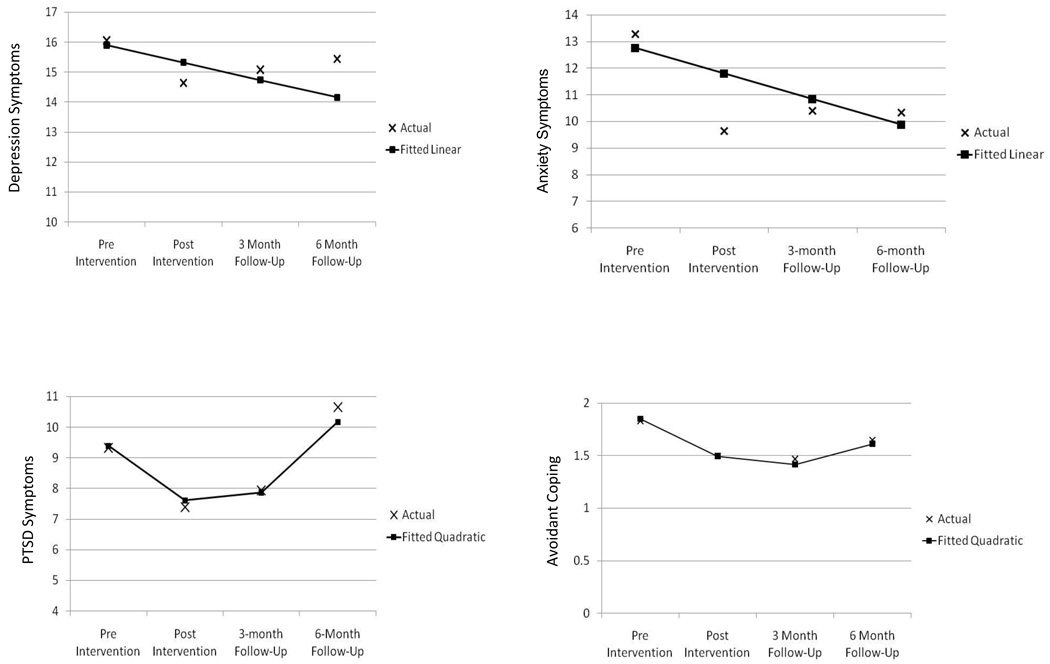
Our hypotheses predicted improvement in PTSD, anxiety, and depression symptoms. Hypothesis 1 was partially supported. For post-traumatic stress disorder symptoms (total CPSS scores) there was both a significant linear (t (76) = 2.10, p < .05) and a significant quadratic fixed effect (t(76) = 2.30, p < .05), indicating symptom decreases at a rate of 2.80 points per 3-month interval, but also that the decrease attenuated significantly after the intervention ended (e.g., the change demonstrated began to slow down or reverse direction at follow-up). The proportionate variance explained (PVE) moving from an intercept only model to the model of both average linear and average quadratic growth was .10.
Hypothesis 2 was supported. For anxiety symptoms (total MASC scores), there was a significant linear fixed effect (t(75) = 2.15, p < .05) indicating a significant linear decrease in anxiety symptoms of approximately 1 point per 3-month interval. See Table 3 for all model coefficients. The PVE for this linear effect over an intercept-only model was .08.
Table 3.
Parameters of Growth Curve Models for all Outcome Variables (N = 23 individuals, 92 observations across 4 time points)
| Parameter | PTSD Symptoms | Anxiety Symptoms |
Depression Symptoms |
Avoidant Coping |
|---|---|---|---|---|
| Average (fixed) effects | ||||
| Intercept – initial level (β00) | 9.39 *** | 12.76 *** | 15.90 *** | 1.85 *** |
| Linear change (β10) | −2.80 * | −.96 * | −.58 ~ | −.164 * |
| Quadratic change (β20) | 1.02 * | NE | NE | .0153 ~ |
| Random effects (variance estimates) | ||||
| Intercept variance (τ00) | 7.99 *** | 22.50 *** | 14.89 *** | .2677 *** |
| Linear change variance (τ10) | NE | NE | 3.22 *** | NE |
| Quadratic change variance (τ20) | NE | NE | NE | NE |
Note.
p < .001,
p < .01,
p < .05,
p < .06
NE = not estimated in ‘best fit’ model
Hypothesis 3 was marginally supported. For depression symptoms (total CDI score), the best fitting model had a fixed effect for linear change that was marginally significant and negative (t(22) = 1.98, p = .06), indicating a reduction in CDI scores across participants of approximately one-half point per 3 months. The PRV for the linear fixed effect was .078.
Analyses of coping strategies
We examined the fixed effects for change over time for the four coping variables. We found a significant decrease in avoidant coping of .16 points per 3-month interval (t(22) = 2.28, p < .05), with a marginally significant quadratic fixed effect, t(76) = 1.95, p = .055. The PVE for this model relative to a intercept only model was .13. There was no significant change over time in active, support seeking or distraction coping strategies.
Analyses of intercept and trajectory variability
These analyses tested for significance in the variance components of the HLM models. As described in the methods section, for each model, we examined variability for all fixed effects, and when it was found to be significant it was modeled as a function of the background variables of sex, age, and school. For depression symptoms, both random effects were significant (intercept and linear trajectory variance), although none of the possible explanatory background variables were significant predictors of this variability. For all other variables, significant variance was found in the intercept terms (baseline scores) only, indicating, for instance, that participants had significantly different levels of symptoms at baseline, but that they followed a similar pattern of change in symptoms over time. For the anxiety variable, the significant variance in the intercept term (χ2 (20) = 40.84, p <.001) was successfully accounted for by participants’ sex (t(20) = 3.10, p < .01). Specifically, girls’ initial anxiety score was almost six points higher than boys. The significant intercept variances for the PTSD variable (p < .01) and for avoidant coping strategies (p < .001) could not be successfully accounted for by the possible explanatory variables.
Discussion
This is one of only a very small number of studies to test a school-based mental health intervention for AI youth who have experienced trauma, and to attempt to target and tailor an evidence-based mental health curriculum to be culturally sensitive for this population. Our results suggest that the adapted CBITS intervention has positive effects on AI youth in 6th – 8th grades. Youth in this study showed significant decreases in PTSD symptoms, anxiety symptoms, and avoidant coping strategies at 3 month follow-up. We also identified a marginally significant decrease in participants’ depression symptoms.
For PTSD symptoms and avoidant coping strategies, the positive effects observed in the quantitative data as linear change over time began to reverse direction after the 3-month follow-up time period. Our results are consistent with Stein and colleagues’ (2003) findings that participants’ decreases in PTSD and depression symptoms were maintained three months after the end of the intervention. However, in addition to a 3-month follow-up, we added a 6-month follow-up time point at which reductions in PTSD symptoms and avoidant coping strategies evidenced by participants through the 3-month follow-up time period had returned to baseline or near baseline levels (see Figure 2). Given the high rates of violence exposure among AI youth, it is reasonable to suggest these elevated PTSD symptoms are a response to additional violence exposure. Further, reductions in avoidant coping were not sustained which may suggest that the return of PTSD symptoms could be related to a return to avoidant coping strategies that might immediately follow new violence exposure. It is also important to consider that the attenuation of positive effects might suggest that the CBITS intervention, which focuses on acute events of trauma, might not fully address the complex, chronic traumas that most AI youth in our study were experiencing. This suggests that maximizing the length of time that participants are followed is important, particularly for adolescents who may be at risk for continuing trauma exposure. Future research should investigate whether depression and anxiety symptom reductions remain stable beyond six months post-intervention, as it is possible that the effects of trauma exposure on depression and anxiety are delayed. It might be that more intense or longer intervention is required to permanently impact these symptoms and behaviors. A “booster” intervention might be a way to increase and/or sustain positive effects of the intervention.
Figure 2.
Graphs for outcomes showing significant or trend change over time.
Although it was encouraging to observe reductions in avoidant coping, no changes in active, support-seeking, or distraction coping were found. It may be that the effects of the intervention were not related to participants’ use of coping strategies. Alternatively, these findings may be related to our use of an abbreviated version of the Coping Strategies Checklist. The original scale has 58 items, while we selected only 12 items (including only two items each for the distraction and support-seeking subscales), which could have reduced our power to detect changes in these constructs.
Implementing CBITS in American Indian Reservation Communities
Although our findings are promising, we have some concerns about the acceptability, feasibility, and appropriateness of CBITS for American Indian communities. In terms of acceptability, although past research suggests that AI/AN youth will participate in school-based group prevention interventions (Miranda, et al., 2005), the large number of parents who declined to give consent for their children to be screened and the 30% of youth who screened in but did not want to participate in a group intervention for trauma raises questions about the potentially stigmatizing nature of the screening and intervention processes. It might be that an individual trauma-focused intervention or community-based inclusive intervention that incorporates prevention and treatment would be more palatable to many AI youth.
On the other hand, youth who did elect to participate in the intervention seemed to find it acceptable, as indicated by our 100% retention rate and the high attendance rate at treatment sessions (71%). This high rate of attendance is likely due in part to the CBITS sessions being held during school hours and in partnership with our school-based health centers. CBITS was intentionally designed to be delivered in school as a way to make trauma treatment more accessible to youth. The high attendance rates we observed lend support to the growing literature on the importance of school-based health centers and other school-based interventions in making mental health services available to youth who need them (Brindis, et al., 2003; Kaplan, Calonge, Guernsey, & Hanrahan, 1998). One of the original objectives of CBITS was to develop an intervention that was feasible for school systems to administer and sustain.
Given CBITS’ explicit focus on feasibility within ethnically diverse school settings with limited resources, we found that implementing CBITS in AI communities was time and labor intensive. Acquiring tribal approvals was an important but lengthy process. The recruitment process, including obtaining parent consent and youth assent for both the screening and intervention involved significant time and resulted in treating only 24 of the 104 youth who met initial intervention screening criteria related to violence exposure and PTSD symptoms.
In this study, issues of appropriateness were the most complex. In the literature on cultural adaptations to evidence-based interventions, there is recognition that cultural additions may constitute active ingredients of treatment above and beyond the core components of an existing treatment. Resnicow and colleagues (2000) suggest that deep-structure cultural adaptations to an intervention (those that take into account cultural beliefs and practices, as well as other contextual factors that impact health behavior) are necessary to maximize cultural sensitivity and increase the likelihood of effectiveness. However, Rousseau and Kirmayer (2009) argue that any cultural adaptations raise questions of internal validity, as treatment effects could be attributed to the original core components of an intervention or to the addition of cultural practices. In this study, we intentionally focused primarily, but not solely, on what Rescinow and colleagues (2000) might call surface-level adaptations in order to test the cultural appropriateness and relevance of CBITS. However, the attenuation of our positive findings, as well as concerns with feasibility and acceptability, suggest that more deep structure adaptations to CBITS may be warranted for AI youth in rural reservation communities.
For instance, as was discussed previously, there were high rates of trauma and PTSD symptoms in the sample. When examining high rates of violence exposure, mental health challenges, and health disparities faced by AI/AN youth, it is important to understand the context from which these disparities emerged. Adolescents who live in such environments may be at constant risk for the triggering of PTSD symptoms. Also, it has been suggested that trauma might be transmitted across generations, either psychologically through processes of transposition and identification with ancestors’ past suffering, behaviorally through parenting practices (Brave Heart, 1998), and/or biologically (van der Kolk, 1994). This concept has been referred to as historical trauma (Brave Heart, 1998; Duran, Duran, & Brave Heart, 1998). It is clear that suffering results from political, economic, and institutional forces – in the case of American Indians and Alaska Natives some of these forces began with first European contact and continue with political, legal, financial, and social inequities today. Recent efforts by researchers and clinicians have been directed at demonstrating links between these past events and current suffering through explication of the concept of historical trauma (e.g., (Brave Heart, 2003; Evans-Campbell, 2008; Whitbeck, Adams, Hoyt, & Chen, 2004). They emphasize that when examining the high rates of violence exposure, mental health challenges, and health disparities faced by AI/AN youth, these contextual issues are important to consider.
Further, CBITS does not include a component to address unresolved grief as a result of losses experienced in the child’s lifetime. Children in this study had high rates of losses of loved ones and were experiencing a great deal of grief. Childhood traumatic grief is a related but distinct concept from PTSD, which has recently been successfully integrated with PTSD treatment in children (Cohen, Mannarino, & Knudsen, 2004; Cohen, Mannarino, & Staron, 2006)
Limitations
Although our findings are promising, there are several methodological limitations that should be noted. First, our small sample size of 24 youth is a limitation in terms of power and generalizability. Given that caveat, our ability to detect significant changes in outcome measures over time with this small sample is encouraging. A second important concern is the lack of a control group in our study design. A true experimental design is the ideal method to test intervention effectiveness, and we recommend that for future study. In this setting, however, where resources were limited and random assignment was not feasible (in terms of preventing contamination across groups within a single school), we strove to strengthen our quasi-experimental design by collecting data at multiple time points and using an analytic strategy that allowed for thorough examination and elimination of some potential threats to validity.
Implications for Research, Policy, and Practice
The results of this study suggest that an adapted version of the CBITS intervention has potential for reducing PTSD, anxiety, and depression symptoms among AI youth, and may also result in decreased use of less effective coping strategies. However, given the limitations already described, concerns remain about the feasibility, acceptability, and appropriateness of the screening process and intervention for AI youth. Thus, additional resources may be necessary to more adequately evaluate the utility of CBITS for AI youth, including additional testing to determine how to increase its acceptability and long-term effectiveness.
Possible adaptations could include creating an individual format of the intervention, developing combined prevention/treatment approaches that do not involve screening, integrating a traditional healing component into the intervention, and/or addressing chronic and historical trauma more explicitly. In addition, findings from the screening component of our study highlight the importance of research and interventions that address traumatic grief/loss.
We believe that it is also essential to develop non-stigmatizing interventions in collaboration with AI communities that address the complex realities of youths’ lives, including the legacies of past oppression and current inequities, that include parents and other family members in change efforts, and that build on cultural traditions, strengths, and the effective healing practices that already exist. In response to these lessons learned, we developed a second component of THRIVE, which involved a community-based participatory research partnership with one of the AI communities to develop, implement, and evaluate a community-based mental health intervention for AI youth and their families that emphasized traditional cultural teachings, parenting and social-skill building, healing historical trauma, and equine activities.
In addition to this type of community-based universal intervention, it is also important to develop methods of recruitment and screening that are more consistent with rural AI cultures in order to provide targeted intervention for youth who have experienced trauma and who need services. The impact of improved interventions will not be fully realized if we do not reach youth who most need them. In our study, we were able to screen 38% of youth in the schools. More culturally framed recruitment and screening processes that are more relationship-based and build upon connectedness within small communities may be more successful.
Finally, the resources required to implement the intervention raise questions about potential sustainability. Fortunately, current efforts by the National Native Children’s Trauma Center in Montana may soon provide data on real-world sustainability of CBITS in AI communities. In our implementation, even though CBITS was specifically designed to be sustainable within school systems, our facilitators found it to be prohibitively resource and time intensive. This was in part because implementation initially involved numerous resource considerations related to the research component of the study (as opposed to exclusive focus on service delivery), but also reflects the time burdens currently faced by school providers. This in turn points to overarching issues of limited funding for mental health treatment and prevention, and current systemic funding inequities. Thus, this suggests the need to consider whether and how CBITS could be sustainable within AI communities, as well as the overall importance of creating more equitable and culturally competent systems of care.
Acknowledgments
This research was supported by grants from the SAMHSA National Childhood Traumatic Stress Network through the New Mexico Alliance for Children with Traumatic Stress and as part of the Core Research Project for the UNM Prevention Research Center through a grant from the Centers for Disease Control & Prevention (Cooperative Agreement #1-U48-DP-0000061). Grateful acknowledgement to Steve Adelsheim, Richard Hough, and Martin Kileen who conceptualized the project; Peou Lakhana, Lynn Abeita, Gloria Blea Johnson, Charlene Poola, Eugene Tsinajinnie, Lance Freeland, Christopher Lee, and Willa Ortega who were instrumental in adapting the intervention and implementing the research; all of the students, families, facilitators, tribal leaders, school personnel, and community members who participated in or supported the study; Deborah Bybee for statistical consultation, and Douglas Novins for his helpful feedback on the manuscript.
Contributor Information
Jessica R. Goodkind, University of New Mexico School of Medicine, Department of Pediatrics, Division of Prevention and Population Sciences, MSC11 6145, Albuquerque, NM 87131, phone: (505) 272-4462, fax: (505) 272-4857.
Marianna D. LaNoue, University of New Mexico School of Medicine, Department of Family and Community Medicine.
Jaime Milford, James A. Haley VA Medical Center, Tampa, Florida.
References
- Ayers TS, Sandler IN, West SG, Roosa MW. A dispositional and situational assessment of children's coping: Testing alternative models of coping. Journal of Personality. 1996;64:923–958. doi: 10.1111/j.1467-6494.1996.tb00949.x. [DOI] [PubMed] [Google Scholar]
- Beals J, Manson SM, Whitesell NR, Spicer P, Novins DK, Mitchell CM, et al. Prevalence of DSM-IV Disorders and Attendant Help-Seeking in 2 American Indian Reservation Populations. Arch Gen Psychiatry. 2005;62:99–108. doi: 10.1001/archpsyc.62.1.99. [DOI] [PubMed] [Google Scholar]
- Boyd-Ball AJ, Manson SM, Noonan C, Beals J. Traumatic events and alcohol use disorders among American Indian adolescents and young adults. Journal of Traumatic Stress. 2006;19:937–947. doi: 10.1002/jts.20176. [DOI] [PubMed] [Google Scholar]
- Brave Heart MYH. The return to the sacred path: Healing the historical trauma and historical unresolved grief response among the Lakota through a psychoeducatioal group intervention. 1998 Unpublished manuscript. [Google Scholar]
- Brave Heart MYH. The historical trauma response among natives and its relationship with substance abuse: A Lakota illustration. Journal of Psychoactive Drugs. 2003;35:7–13. doi: 10.1080/02791072.2003.10399988. [DOI] [PubMed] [Google Scholar]
- Brindis CD, Klein J, Schlitt J, Santelli J, Juszczak L, Nystrom RJ. School-based health centers: Accessibility and accountability. Journal of Adolescent Health. 2003;32:98–107. doi: 10.1016/s1054-139x(03)00069-7. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Knudsen K. Treating Childhood Traumatic Grief: A Pilot Study. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43:1225–1233. doi: 10.1097/01.chi.0000135620.15522.38. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Staron VR. A Pilot Study of Modified Cognitive-Behavioral Therapy for Childhood Traumatic Grief (CBT-CTG) Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45:1465–1473. doi: 10.1097/01.chi.0000237705.43260.2c. [DOI] [PubMed] [Google Scholar]
- Deters PB, Novins DK, Fickenscher A, Beals J. Trauma and Posttraumatic Stress Disorder Symptomatology: Patterns Among American Indian Adolescents in Substance Abuse Treatment. American Journal of Orthopsychiatry. 2006;76:335–345. doi: 10.1037/0002-9432.76.3.335. [DOI] [PubMed] [Google Scholar]
- Duncan RD, Saunders BE, Kilpatrick DG, Hanson RF, Resnick HS. Childhood physical assault as a risk factor for PTSD, depression, and substance abuse: Findings from a national survey. American Journal of Orthopsychiatry. 1996;66:437–448. doi: 10.1037/h0080194. [DOI] [PubMed] [Google Scholar]
- Duran B, Duran E, Brave Heart MYH. Native Americans and the Trauma of History. In: Thornton R, editor. Studying Native America: Problems and Prospects in Native American Studies. Madison: University of Wisconsin Press; 1998. [Google Scholar]
- Evans-Campbell T. Historical trauma in American Indian/Native Alaska communities: A multilevel framework for exploring impacts on individuals, families, and communities. Journal of Interpersonal Violence. 2008;23:316–338. doi: 10.1177/0886260507312290. [DOI] [PubMed] [Google Scholar]
- Foa EB, Treadwell K, Johnson K, Feeny NC. The Child PTSD Symptom Scale: A Preliminary examination of its psychometric properties. Journal of Clinical Child Psychology. 2001;30:376–384. doi: 10.1207/S15374424JCCP3003_9. [DOI] [PubMed] [Google Scholar]
- Gone JP. A community-based treatment for Native American historical trauma: Prospects for evidence-based practice. Journal of Consulting and Clinical Psychology. 2009;77:751–762. doi: 10.1037/a0015390. [DOI] [PubMed] [Google Scholar]
- Gone JP, Alcantara C. Identifying effective mental health interventions for American Indians and Alaska Natives: A review of the literature. Cultural Diversity and Ethnic Minority Psychology. 2007;13:356–363. doi: 10.1037/1099-9809.13.4.356. [DOI] [PubMed] [Google Scholar]
- Hawkins EH, Cummins LH, Marlatt GA. Preventing Substance Abuse in American Indian and Alaska Native Youth: Promising Strategies for Healthier Communities. Psychological Bulletin. 2004;130:304–323. doi: 10.1037/0033-2909.130.2.304. [DOI] [PubMed] [Google Scholar]
- Health United States. Health, United States, 2004. Hyattsville, Maryland: National Center for Health Statistics; 2004. [PubMed] [Google Scholar]
- Huey SJ, Jr, Polo AJ. Evidence-based psychosocial treatments for ethnic minority youth. Journal of Clinical Child and Adolescent Psychology. 2008;37:262–301. doi: 10.1080/15374410701820174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaycox L. CBITS: Cognitive behavioral intervention for trauma in schools. Longmont, CO: Sopris West Educational Services; 2004. [Google Scholar]
- Jones MC, Daughinais P, Sack WH, Somervell PD. Trauma-related symptomatology among American Indian adolescents. Journal of Traumatic Stress. 1997;10:163–173. doi: 10.1023/a:1024852810736. [DOI] [PubMed] [Google Scholar]
- Kaplan DW, Calonge BN, Guernsey BP, Hanrahan MB. Managed care and school-based health centers. Use of health services. Archives of Pediatric Adolescent Medicine. 1998;152:25–33. doi: 10.1001/archpedi.152.1.25. [DOI] [PubMed] [Google Scholar]
- Kerig PK, Ward RM, Vanderzee KL, Moeddel MA. Posttraumatic stress as a mediator of the relationship between trauma and mental health problems among juvenile delinquents. Journal of Youth and Adolescence. 2009;38:1214–1225. doi: 10.1007/s10964-008-9332-5. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Saunders B, Resnick HS, Best CL, Schnurr PP. Risk factors for adolescent substance abuse and dependence: Data from a national sample. Journal of Consulting and Clinical Psychology. 2000;68:19–30. doi: 10.1037//0022-006x.68.1.19. [DOI] [PubMed] [Google Scholar]
- Kovacs M. The Children's Depression Inventory Manual. North Tonawanda, NY: Multi-Health Systems, Inc; 1992. [Google Scholar]
- Kreft I, De Leeuw J. Introducing multilevel modeling. London: Sage Publications; 1998. [Google Scholar]
- LaFromboise TD, Bigfoot DS. Cultural and cognitive considerations in the prevention of American Indian adolescent suicide. Journal of Adolescence. 1988;11:139–153. doi: 10.1016/s0140-1971(88)80049-6. [DOI] [PubMed] [Google Scholar]
- Manson SM, Beals J, O'Nell T, Piasecki J, Bechtold D, Keane E, et al. Wounded spirits, ailing hearts: PTSD and related disorders among American Indians. In: Marsella MJFAJ, Gerrity ET, Scurfield RM, editors. Ethnocultural Aspects of Post-Traumatic Stress Disorder. Washington, D.C.: American Psychological Association; 1996. pp. 255–283. [Google Scholar]
- March JS, Parker JD. The Multidimensional Anxiety Scale for Children (MASC) Mahwah, NJ: Lawrence Erlbaum Associates; 1999. [Google Scholar]
- Martinez P, Richters JE. The NIMH Community Violence Project: II. Children's distress symptoms associated with violence exposure. Psychiatry: Interpersonal and Biological Processes. 1993;56:22–35. doi: 10.1080/00332747.1993.11024618. [DOI] [PubMed] [Google Scholar]
- Miranda J, Bernal G, Lau A, Kohn L, Hwang W, LaFromboise T. State of the science on psychosocial interventions for ethnic minorities. Annual Review of Clinical Psychology. 2005;1:113–142. doi: 10.1146/annurev.clinpsy.1.102803.143822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morsette A, Swaney G, Stolle D, Schuldberg D, van den Pol R, Young M. Cognitive behavioral intervention for trauma in schools (CBITS): School-based treatment on a rural American Indian reservation. Journal of Behavior Therapy and Experimental Psychiatry. 2009;40:169–178. doi: 10.1016/j.jbtep.2008.07.006. [DOI] [PubMed] [Google Scholar]
- National Center for Children in Poverty. Facts about trauma for policymakers. 2007 Retrieved November 23, 2009, from http://www.nccp.org/publications/pub_746.html.
- Ngo V, Langley A, Kataoka SH, Nadeeem E, Escudero P, Stein BD. Providing evidence-based practice to ethnically diverse youths: Examples from the Cognitive Behavioral Intervention for Trauma in Schools (CBITS) program. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:858–862. doi: 10.1097/CHI.0b013e3181799f19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nugent WR. Integrating single-case and group-comparison designs for evaluation research. Journal of Applied Behavioral Science. 1996;32:209–226. [Google Scholar]
- Pina AA, Villalta IK, Ortiz CD, Gottschall AC, Costa NM, Weems CF. Social support, discrimination, and coping as predictors of posttraumatic stress reactions in youth survivors of Hurricane Katrina. Journal of Clinical Child and Adolescent Psychology. 2008;37:564–574. doi: 10.1080/15374410802148228. [DOI] [PubMed] [Google Scholar]
- Raudenbush S, Byrk A. Hierarchical Linear Models. Newbury Park, CA: Sage Publications; 2002. [Google Scholar]
- Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethnicity and Disease. 1999;9:10–21. [PubMed] [Google Scholar]
- Resnicow K, Soler R, Braithwaite RL, Ahluwalia JS, Butler J. Cultural sensitivity in substance use prevention. Journal of Community Psychology. 2000;28:271–290. [Google Scholar]
- Rieckmann TR. Explanatory style, coping, and depression in Navajo adolescents. ProQuest Information & Learning, US; 2001. [DOI] [PubMed] [Google Scholar]
- Ringel JS, Sturm R. National estimates of mental health utilization and expenditures for children in 1998. Journal of Behavioral Health Services & Research. 2001;28:319–333. doi: 10.1007/BF02287247. [DOI] [PubMed] [Google Scholar]
- Rousseau Cc, Kirmayer L. Cultural adaptation of psychological trauma treatment for children. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48:954–955. doi: 10.1097/CHI.0b013e3181b21669. [DOI] [PubMed] [Google Scholar]
- Schinke SP. Preventing substance abuse with American Indian youth. Social Casework. 1985;66:213–217. [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY US: Oxford University Press; 2003. [Google Scholar]
- Singer M, Anglin TM, Song Ly, Lunghofer L. Adolescents' exposure to violence and associated symptoms of psychological trauma. JAMA: Journal of the American Medical Association. 1995;273:477–482. [PubMed] [Google Scholar]
- Stein BD, Jaycox LH, Kataoka SH, Wong M, Tu W, Elliott MN, et al. A mental health intervention for schoolchildren exposed to violence: A randomized control trial. JAMA: Journal of the American Medical Association. 2003;290:603–611. doi: 10.1001/jama.290.5.603. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Office of the Surgeon General, & SAMHSA (n.d.) Native American Indians Fact Sheet. Retrieved December 3, 2009, from http://mentalhealth.samhsa.gov/cre/fact4.asp.
- U.S. Department of Justice Bureau of Justice Statistics. A BJS statistical profile, 1992–2002: AI/ANs and crime. 2004 Retrieved November 23, 2009, from http://www.ojp.usdoj.gov/bjs/pub/pdf/aic07.pdf.
- van der Kolk B. The body keeps the score: Memory and the evolving psychobiology of posttraumatic stress. Boston, Massachusetts: Harvard Medical School; 1994. [DOI] [PubMed] [Google Scholar]
- Whitbeck LB, Adams GW, Hoyt DR, Chen X. Conceptualizing and measuring historical trauma among American Indian people. American Journal of Community Psychology. 2004;33:119–130. doi: 10.1023/b:ajcp.0000027000.77357.31. [DOI] [PubMed] [Google Scholar]
- Wright M, Banerjee R, Hoek W, Rieffe C, Novin S. Depression and social anxiety in children: Differential links with coping strategies. Journal of Abnormal Child Psychology: An official publication of the International Society for Research in Child and Adolescent Psychopathology. 38:405–419. doi: 10.1007/s10802-009-9375-4. [DOI] [PubMed] [Google Scholar]
- Zinzow HM, Ruggiero KJ, Resnick H, Smith D, Saunders B, Kilpatrick D. Prevalence and mental health correlates of witnessed parental and community violence in a national sample of adolescents. Journal of Child Psychology and Psychiatry. 2009;50:441–450. doi: 10.1111/j.1469-7610.2008.02004.x. [DOI] [PMC free article] [PubMed] [Google Scholar]