Abstract
Vagal maneuvers cause increase in vagal tone, which has been shown to slow many types supraventricular tachycardia, such as atrial fibrillation (AF). However, the conversion of AF to sinus rhythm is usually not associated with vagal manuvers. Thus, AF is classically treated with medication and electrical cardioversion. Here, we present a 29-year-old male with no cardiovascular history and a low atherosclerotic risk profile who developed AF which converted into sinus rhythm immediately after a digital rectal exam. The patient remained asymptomatic after a 3-month follow-up. This implies that the digital rectal exam can be considered as an additional attempt to convert AF to sinus rhythm in AF patients.
Keywords: atrial fibrillation, AF, sinus rhythm, vagal
Introduction
Atrial fibrillation (AF) is commonly associated with congestive heart failure and strokes secondary to atrial thromboemboli.1–3 Lone atrial fibrillation is a subtype that usually occurs in the younger population and represents AF without pre-existing cardiovascular diseases. These patients may have persistent, paroxysmal, or chronic AF. Episodes are often preceded by exercise or emotional stress.1 Hyperthyroidism and pheochromocytoma are other rare causes of AF.1–3 Pathophysiology of AF is not well understood but it is known that ectopic atrial beats stem from areas in the left atrium around the inlet of pulmonary veins.4 An overactive parasympathetic (vagal) nervous system may also cause AF, such as in athletes. People with digestive problems could also develop AF and potentially have weekly episodes which last from a few minutes to several hours. AF in general occurs at night, often ending in the morning following rest, digestive periods (after dinner), and alcohol consumption. Frequent urination (every 20 minutes or so) often occurs during the early phase of an episode and is due to the release of atrial natriuretic peptide from the fibrillating atria. The patients with AF may first be treated with medications to slow the heart rate and to control heart rhythm. Anticoagulants are often given to prevent stroke, depending of the risk of embolic event. In addition, procedures such as synchronized electrical cardioversion may also be used to eliminate AF and return the heart beat to a normal rhythm. Radiofrequency ablation may also be used to prevent recurrence of AF in certain individuals. In this report, we described how a simple digital rectal examination led to the termination of typical AF in a 29-year old male. The case report is valuable for practice in cardiology clinics and emergency medicine for diagnosis and treatment of AF patients.
Case report
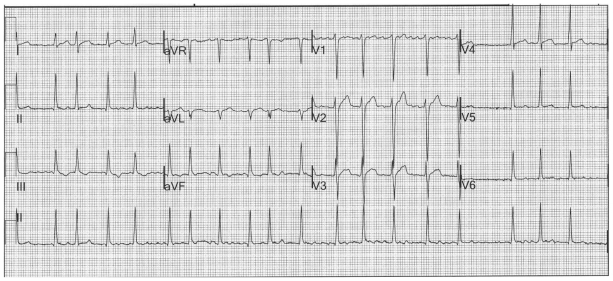
A 29 year-old male with no significant past medical history complained of sudden onset of palpitations while walking home from the store on the night of admission. Palpitations were described as fast-beating heart beats followed by slower heart beats. Onset of palpitations was 3 hours later, just prior to presentation in the Emergency Department. Patient denies shortness of breath, diaphoresis, chest pain, dizziness, loss of consciousness, fever, chills, malaise, recent illnesses, alcohol or recreational drug use. Patient has no other past medical history. He smoked cigarettes (under a pack a day) for 5 years but quit five years ago. Patient’s vitals were as follows, blood pressure: 144/99, Pulse: 113 bpm, Temperature: 97.0 °F, Saturation: 99% on room air. A pertinent physical examination revealed an athletic male with cardiovascular ausculatory findings of an irregularly irregular rhythm with no murmurs or rales. Twelve-lead EKG records showed a typical AF with rapid and irregular rhythm, and coarse fibrillating P waves (Fig. 1).
Figure 1.
The initial 12-Lead EKG of the 29-year-old male before treatment.
Treatment
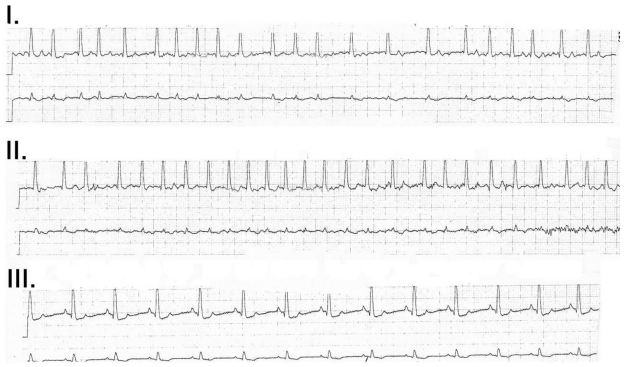
The patient was found to be in rapid atrial fibrillation in the Emergency Department. Predicted onset of atrial fibrillation, based on the patient’s symptoms, is less than 48 hours. He was admitted and monitored by telemetry. Metoprolol 5 mg IV was given for rate control. A heparin drip was planned for the patient in anticipation of his undergoing cardioversion since anticoagulation is necessary prior to cardioversion to prevent development or further development of atrial thrombus and thereby preventing embolic events. However, prior to starting anticoagulation, a digital rectal exam (testing the stool for occult blood) is required to rule out a GI bleed. Before administering the rectal exam, the patient’s heart rate was 140 bpm in rapid atrial fibrillation (Fig. 2, panels I and II). After the digital rectal exam, his rhythm converted to normal sinus and the rate decreased to 80 beats per minute. (Fig. 2, panel III). The patient no longer complained of discomfort and was discharged from the hospital. In addition, the patient remained asymptomatic after a 3-month follow-up.
Figure 2.
The telemetry strip recording of Lead II for the 29-year old male before (panels I and II) and after (panel III) the digital rectal exam.
Discussion
The patient is a typical AF subject as confirmed by the EKG with 140 beats per minute and the loss of the P wave (Fig. 1). After the rectal guiac exam, the second EKG revealed a normal sinus rhythm, which indicated that the exam eliminated the AF. The termination of AF is unlikely a result from medications, because the effect of the medication on the AF occurred immediately during and after the rectal exam. This was very different than the medication-mediated effect which gradually returns the AF to normal within minutes to hours. The mechanism for the effects of the rectal exam on the AF is likely due to the increase in parasympathetic activity through cranial nerve X (Vagus nerve), which also dampens the sympathetic stimulation to the heart. The parasympathetic branch of the Autonomic nervous system has several effects on the heart. First, increased parasympathetic activity slows the rate of impulse formation of the sinus atrial (SA) node. Second, increased parasympathetic activity slows conduction and increases refractory through the atrioventriuclar (AV) node. This prediction is also supported by other studies. For example, in an earlier report, a digital rectal exam stimulated receptors in the rectum causing the increase in parasympathetic activity, after which the procedure was able to eliminate supraventricular tachycardia.5,6
The patient was also told to strain during the rectal guiac exam, causing increased vagal tone through the valsalva maneuver.7 One study compared 27 people with AF against a control group of 27 people with no history of heart disease in their EKG response to valsalva maneuver. They monitored the P-wave dispersion of the two groups and found that the maneuver normalizes the P-wave dispersion and duration. They concluded that decreased sympathetic tone is beneficial in patients with AF.8 Another study measured more EKG parameters in patients with paroxysmal AF in response to the valsalva maneuver.9
Other similar mechanisms of increasing parasympathetic stimuli or decreasing sympathetic stimuli include the carotid massage. This method has been documented to be a diagnostic and therapeutic tool for patients with atrial flutter and atrial fibrillation.10,11
We could not completely exclude the possibility that the conversion to sinus rhythm was occurred by pre-administrated beta-blocker. However, in consideration of the limited half life of the beta-blocker, the possibility by the beta-blocker were less. In general enhanced vagal response may increase AF episodes. But, in this case there was not further AF episode during the three months follow-up. Thus, the reported digital procedure could be an additional (not replaced) method to treat AF patient.
In conclusion, the case report described how a digital rectal exam and/or valsalva maneuver was able to terminate typical AF in a 29-year old male instantly. The rectal exam is a relatively simple procedure that presents little risks for AF patients. Thus, this case report provides an implication to use the rectal exam as an additional therapeutic modality for selective AF patients.
Acknowledgement
The author of this report has checked that he complies with the Principles of Ethical Publishing in the International Journal of Cardiology,12 and would like to thank Mrs. Vanessa Cervantes for the assistance of the manuscript preparation.
Footnotes
Disclosure This manuscript has been read and approved by the author. This paper is unique and is not under consideration by any other publication and has not been published elsewhere. The author and peer reviewers of this paper report no conflicts of interest. The author confirms that they have permission to reproduce any copyrighted material.
References
- 1.American Heart Association, Inc. 2008-12-04. Atrial Fibrillation (for Professionals) Archived from the original on 2009-03-28. http://www.webcitation.org/5fcMx8BUx.
- 2.Benjamin EJ, Wolf PA, D’Agostino RB, et al. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998;98:946–52. doi: 10.1161/01.cir.98.10.946. [DOI] [PubMed] [Google Scholar]
- 3.Wattigney WA, Mensah GA, Croft JB. Increased atrial fibrillation mortality: United States, 1980–1998. Am J Epidemiol. 2002;155:819–26. doi: 10.1093/aje/155.9.819. [DOI] [PubMed] [Google Scholar]
- 4.Haissaguerre M, Jais P, Shah DC, et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998;339:659–66. doi: 10.1056/NEJM199809033391003. [DOI] [PubMed] [Google Scholar]
- 5.Weiss LD. Digital rectal message for PSVT. Ann Emerg Med. 1989;18:330–1. doi: 10.1016/s0196-0644(89)80439-1. [DOI] [PubMed] [Google Scholar]
- 6.Roberge R, Anderson E, MacMath T, et al. Termination of paroxysmal supraventricular tachycardia by digital rectal massage. Ann Emerg Med. 1987;16:1291–3. doi: 10.1016/s0196-0644(87)80243-3. [DOI] [PubMed] [Google Scholar]
- 7.Derbes VJ, Kerr A., Jr Valsalva’s maneuver and Weber’s experiment. N Engl J Med. 1955;253:822. doi: 10.1056/NEJM195511102531907. [DOI] [PubMed] [Google Scholar]
- 8.Tufan Tukek, et al. Effect of Valsalva maneuver on surface electrocardiographic P-wave dispersion in paroxysmal atrial fibrillation. American Journal of Cardiology. 2000;85:896–99. doi: 10.1016/s0002-9149(99)00891-7. [DOI] [PubMed] [Google Scholar]
- 9.Altunkeser, et al. The Effect of Valsalva Maneuver on P Wave in 12-Lead Surface Electrocardiography. Angiology. 2002;53:443–9. doi: 10.1177/000331970205300411. [DOI] [PubMed] [Google Scholar]
- 10.Kirchhof CJ, Gorgels AP, Wellens HJ. Carotid sinus massage as a diagnostic and therapeutic tool for atrial flutter-fibrillation. Pacing Clin Electrophysiol. 1998;21:1319–21. doi: 10.1111/j.1540-8159.1998.tb00196.x. [DOI] [PubMed] [Google Scholar]
- 11.Lown B, Levine SA. The carotid sinus: clinical value of its stimulation. Circulation. 1961;3:271. doi: 10.1161/01.cir.23.5.766. [DOI] [PubMed] [Google Scholar]
- 12.Coats AJ. Ethical authorship and publishing. Int J Cardiol. 2009;131:149–50. doi: 10.1016/j.ijcard.2008.11.048. [DOI] [PubMed] [Google Scholar]