Abstract
Background
Circadian Locomotor Output Cycles Kaput (CLOCK), an essential element of the positive regulatory arm in the human biological clock, is involved in metabolic regulation. The aim was to investigate the behavioral (sleep duration, eating patterns and chronobiological characteristics) and hormonal (plasma ghrelin and leptin concentrations) factors which could explain the previously reported association between the CLOCK 3111T/C SNP and weight loss.
Methodology/Principal Findings
We recruited 1495 overweight/obese subjects (BMI: 25–40 kg/m2) of 20–65 y. who attended outpatient obesity clinics in Murcia, in southeastern Spain. We detected an association between the CLOCK 3111T/C SNP and weight loss, which was particularly evident after 12–14 weeks of treatment (P = 0.038). Specifically, carriers of the minor C allele were more resistant to weight loss than TT individuals (Mean±SEM) (8.71±0.59 kg vs 10.4±0.57 kg) C and TT respectively. In addition, our data show that minor C allele carriers had: 1. shorter sleep duration Mean ± SEM (7.0±0.05 vs 7.3±0.05) C and TT respectively (P = 0.039), 2. higher plasma ghrelin concentrations Mean ± SEM (pg/ml) (1108±49 vs 976±47)(P = 0.034); 3. delayed breakfast time; 4. evening preference and 5. less compliance with a Mediterranean Diet pattern, as compared with TT homozygotes.
Conclusions/Significance
Sleep reduction, changes in ghrelin values, alterations of eating behaviors and evening preference that characterized CLOCK 3111C carriers could be affecting weight loss. Our results support the hypothesis that the influence of the CLOCK gene may extend to a broad range of variables linked with human behaviors.
Introduction
The current prevalence of obesity has been attributed to changes in our diet and physical activity; however, recent research has raised interest in the possibility that changes in our daily behavioral patterns may be a significant contributing factor [1]. Thus, in industrial countries, the amount of daily sleep has declined by 1.5 h over the past century, concurrent with a significant increase in obesity [2]. Although these observed correlations do not support a causal relationship, additional evidence based on data from night-shift workers and sleep-restricted subjects supports the notion that [3] a sleep disruption and therefore, modification of the circadian rhythm, may play a significant role in the etiology of obesity.
Circadian Locomotor Output Cycles Kaput (CLOCK), an essential element of the positive regulatory arm in the human biological clock, is involved in metabolic regulation [4]–[7]. Therefore, CLOCK disruptions may affect the homeostasis of different metabolic pathways. Along these lines, we previously demonstrated associations between the CLOCK 3111T/C (rs1801260) single nucleotide polymorphism (SNP), baseline body weight and weight reduction in obese patients participating in a Mediterranean diet based weight reduction program [8]. Allele specific behavioral habits in sleep and food intake may be responsible for these effects. Indeed, previous studies have shown that this particular SNP may be associated with sleep disorders in subjects affected by major depressive and bipolar disorders [9].
The specific mechanisms driving these effects are unknown; however, these could be mediated through ghrelin and leptin; both follow circadian rhythmicity and are implicated in food intake. Ghrelin stimulates appetite and recent evidence suggests that ghrelin affects sleep [10], [11]. This is consistent with the notion that the neurophysiologic and metabolic mechanisms responsible for the control of food-seeking and sleep behaviors, are coordinated, thus pairing hunger and vigilance during the daylight and satiety and sleep during darkness [12].
The aims of the present study were to evaluate behavioral and chronobiological aspects of resistance to weight loss associated with the CLOCK 3111T/C SNP in an obese, mostly sedentary population. Specifically, we investigated sleep duration, eating behaviour and circadian characteristics as well as ghrelin and leptin plasma values as possible markers of sleep and intake-related processes.
Materials and Methods
Subjects and methods
We recruited overweight or obese subjects (BMI>25 kg/m2 and <40 kg/m2) within the age range of 20–65 years, (n = 1495). Most of the population studied were females (82.5%). Patients attended five outpatient obesity clinics from 2009–2010 in the city of Murcia, located in southeastern Spain. Patients receiving thermogenic or lipogenic drugs, or those diagnosed with diabetes mellitus, chronic renal failure, hepatic diseases or cancer were excluded from the study. 1290 individuals were genotyped for the CLOCK 3111T/C SNP. All procedures were in accordance with good clinical practice. Written consent was obtained from each patient before participation and the study protocol was approved by the Research Ethics Committee of the Virgen de la Arrixaca Hospital. Patient data were codified to guarantee anonymity.
Characteristics of the treatment
The characteristics of the weight reduction program (Garaulet method©) have been described elsewhere [13], [14]. Briefly, during the initial months, subjects attended a weekly 60-min therapy session in support groups (n = 10), followed by a 5-month maintenance period. Sessions were conducted by a nutritionist. Treatment was based on the following: Dietary treatment. Dietary individual energy requirements were assessed by calculating [1] resting energy expenditure (REE) according to the Harris-Benedict formula and [2] total energy expenditure (TEE) according to the type and duration of physical activity estimated by the International Physical Activity Questionnaire (IPAQ). Next, about 600 kcal per day were subtracted from the TEE. The final dietary energy content ranged from 1200–1800 kcal per day for women and 1500–2000 kcal per day for men to induce an approximate loss of 0.5–1 kg per week. The recommendations were consistent with the Mediterranean type of diet [13], [14] and the macronutrient distribution followed the recommendations of the Spanish Society of Community Nutrition [15]. Nutritional education was given during group therapy sessions to help subjects plan their own menus and to educate subjects to adopt appropriate lifetime eating habits. Physical activity emphasized individual goals of 15–30 min or more of moderate intensity physical activity, at least 2 or 3 times a week. Patients were encouraged to use a pedometer to reach at least 10 000 steps per day. Behavioral techniques included stimulus control, self-monitoring, positive reinforcement and cognitive behavioral therapy.
Anthropometric and biochemical measurements
Subjects were weighed barefoot wearing light clothes, with a digital scale to the nearest 0.1 kg, at the same time each day weekly to assess weight loss during treatment. Height was measured using a Harpenden digital stadiometer (rank 0.7–2.05). The subject was positioned upright, relaxed and with the head in the Frankfurt plane. BMI was calculated according to these measurements as weight (kg)/(height(m))2. Total body fat was measured by bioelectrical impedance using TANITA TBF-300 (TANITA Corporation of America, Arlington Heights, IL, USA) equipment. Body fat distribution was assessed by the measurement of different circumferences: waist circumference, at the level of the umbilicus, and hip circumference, as the widest circumference over the greater trochanters [16]. All measurements were made with a flexible and inextensible tape measure.
Ghrelin and leptin
Fasting blood samples, collected at 08:00AM were centrifuged at 4°C, and the plasma was stored at −70°C for subsequent analysis. Plasma leptin and ghrelin samples were measured by radioimmunoassay (Linco Research, St. Charles, MO). All samples for leptin and ghrelin were run in duplicate.
Sleep Hours
Habitual sleep time was estimated by a questionnaire. ‘During week days: How many hours (and minutes) do you usually sleep? and; ‘During weekend days: How many hours (and minutes) do you usually sleep? A total weekly sleep score was calculated as: ((min Weekdays x 5) + (min Weekend days x 2))/7.
Morning-evening Questionnaire
Subjects completed the Morningness/eveningness (M/E) questionnaire (MEQ) 19 item scale of Horne and Ostberg, 1976 [17]. M/E typology is a way to characterize subjects depending on individual differences of wake/sleep patterns and the time of day people feel or perform best. Some people are night “owls” and like to stay up late at night and sleep late in the morning (Evening type), while others are early birds and prefer to go to bed at an early hour and arise with the break of dawn (Morning types). The majority of people are in between and categorized as “Neutral types” [18]. Evening types were considered as scoring under 53 and morning types above 64. All subjects within the range of 53 to 64 were classified as neutral type [18].
Habitual dietary intake
To evaluate food habits, initial nutrient intake was determined by a 24-h dietary recall. Interviews were conducted from Monday to Friday, including 24-h recalls of food intake from weekend and weekdays. Total energy intake and macronutrient composition from the initial 24-h recalls were analyzed with the nutritional evaluation software program Grunumur [19], [20] on the basis of Spanish food composition tables [20]. The intakes of fatty acids were calculated from Spanish food-composition tables [21]. Over the course of one week, patients recorded the time of day that each meal (eg, breakfast, lunch, dinner) was eaten.
Physical activity (PA) questionnaire
To assess PA within the last 7 days, the International Physical Activity Questionnaire (IPAQ), was administered with the help of a nutritionist. It was developed for adults between 18–65 years, assessing the different domains of PA (work, transport, house and garden and leisure time) and the volume of activity was computed by weighting each type of activity by its energy requirements defined in metabolic equivalents METs [22]. It is known to be a valid and reliable instrument to measure PA at the population level [23].
DNA isolation and clock genotyping
DNA was isolated from blood samples using routine DNA isolation sets (Qiagen). We performed genotyping of CLOCK gene polymorphisms using a TaqMan assay with allele specific probes on the ABI Prism 7900HT Sequence Detection System (Applied Biosystems, Foster City, CA, USA) according to the standardized laboratory protocols [24].
Statistical analyses
We used Pearson's chi-square (χ2) test and the Fisher test as statistical procedures to evaluate differences in frequencies. We applied ANOVA and the Student t-test to compare crude means across genotype groups. We tested different genetic inheritance models and a dominant model was applied in the final analyses. We performed multivariate adjustments of the associations by analysis of covariance and estimated adjusted means. We adjusted analyses for potential confounders including sex, age, and study site. We also tested the statistical homogeneity of the effects by sex in the corresponding regression model with interaction terms. Statistical analyses were performed using SPSS 15.0 software (SPSS). A two-tailed P-value of <0.05 was considered statistically significant.
Results
General characteristics
General characteristics of the population studied are shown in Table 1 . By study design, subjects were overweight or obese and they had low levels of physical activity. On average they slept 7 hours/day with a predominance of morning type individuals. The dietary habits were consistent with lower carbohydrate and higher protein and fat intakes than those recommended in Spanish guidelines [25]. However, the type of dietary fat was consistent with the Mediterranean diet pattern (>50% of total fat quantity in grams as monounsaturated fat). The distribution of the 3111T/C genotypes did not differ significantly from that expected according to Hardy Weinberg equilibrium (X2 = 1.167; P = 0.279). During the treatment period which included dietary advice, 81% of the population fulfilled the Mediterranean Diet recommendations.
Table 1. General characteristics of the population studied.
| Mean | SD | |
| Age (yrs) | 39.37 | 12.29 |
| Anthropometric | ||
| BMI (kg/m2) | 31.12 | 5.38 |
| Weight (kg) | 84.10 | 17.34 |
| Height (m) | 1.64 | 0.08 |
| Body fat (%) | 37.34 | 6.63 |
| Waist (cm) | 102 | 15 |
| Hip (cm) | 114 | 10 |
| Weight loss | ||
| Weight loss (Kg) | 9.01 | 5.61 |
| Percentage of weight loss (%) | 11.1 | 6.16 |
| Treatment Weeks (n) | 21 | 17 |
| Rate of weight loss (g/week) | 500 | 450 |
| Activity (n = 1204) | ||
| Exercise (METs) | 4474 | 7544 |
| Dietary intake | ||
| Total Energy (kcal/day) | 2066.7 | 715.4 |
| Proteins (%) | 17.0 | 4.6 |
| Carbohydrates (%) | 41.8 | 10.6 |
| Fats (%) | 42.2 | 9.6 |
| MUFA% (Total fat) | 55.5 | 8.1 |
| Food-Intake Hormones | ||
| Ghrelin (pg/ml) | 1057.81 | 995.3 |
| Leptin (ng/ml) | 19.60 | 14.11 |
| Chronobiological Characteristics | ||
| Sleep (hours per day) | 7.23 | 1.25 |
| Morning-evening-score | 51.70 | 10.10 |
| Morning evening classification | n | (%) |
| Neutral type | 359 | 24 |
| Morning type | 628 | 42 |
| Evening type | 508 | 34 |
| CLOCK Polymorphism. (n = 1290) | n | (%) |
| TT | 684 | 53.0 |
| TC | 500 | 38.8 |
| CC | 106 | 8.2 |
Abbreviations used: BMI; Body mass index, METs; Metabolic equivalents, MUFA; Monounsaturated Fatty Acids.
CLOCK 3111T/C SNP and weight loss
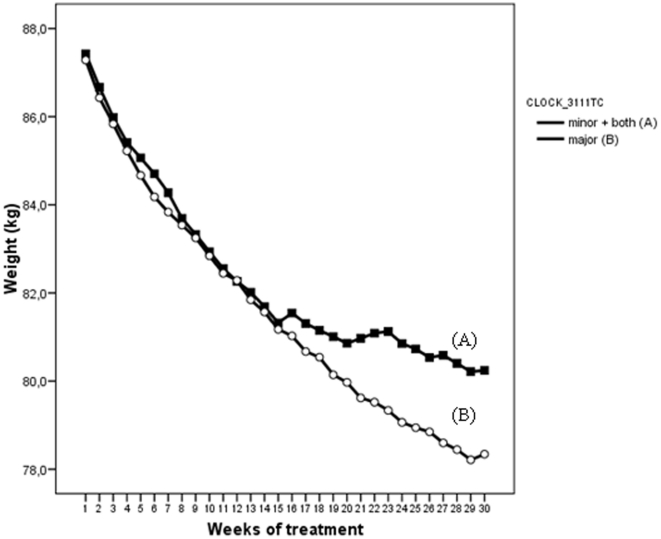
We found an association between the CLOCK 3111T/C SNP and weight loss. Subjects carrying the minor C allele lost significantly less weight (Mean±SEM) (8.71±0.59 kg) compared to TT subjects (10.4±0.57 kg). This effect was particularly evident after 16 weeks of treatment (P = 0.038) ( Figure 1 ). When patients were divided into low and high groups according to median age, differences in weight loss among C and TT carriers were only significant in the older group (≥38 y.) (P = 0.035) while differences were not significant in the younger group (P = 0.297).
Figure 1. CLOCK 3111T/C genotype and weight loss progression during 28 weeks of treatment.
CLOCK 3111T/C, ghrelin, leptin, and eating behaviors
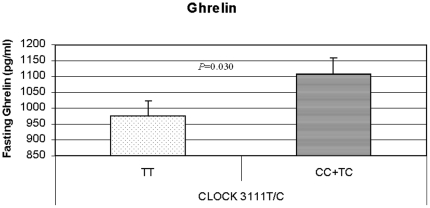
We obtained significant associations between the CLOCK 3111T/C and plasma ghrelin levels that were higher in carriers of the minor allele (C) than in non-carriers (TT) ( Figure 2 ) (P = 0.034). The statistical association was stronger among the older patients (aged ≥38 y; P = 0.022). Moreover, among C carriers we also observed a negative and significant correlation between ghrelin and weight loss (r = −1.37; P = 0.009). However, we did not find a significant association between leptin and the CLOCK 3111T/C SNP.
Figure 2. Significant associations between CLOCK 3111T/C and fasting ghrelin.
Analysis of eating behaviors revealed a trend towards overeating at certain times of the day (P = 0.06) in minor allele (C) carriers, and these subjects also started to eat later in the morning than non-carriers, particularly during week-ends (P = 0.044) (10.00AM vs. 9:43AM, respectively).
CLOCK 3111TC SNP and Mediterranean dietary habits
Minor C allele carriers showed a lower adherence to a Mediterranean Diet pattern than non-carriers ( Table 2 ). Specifically they consumed a higher percent of their daily energy intake as protein (P = 0.032) and higher amount of trans fatty acids (P = 0.039). Conversely, they reported a significantly lower intake of monounsaturated fatty acids (MUFA) (P = 0.045). Moreover, they had a tendency to consume a higher percent as fat (P = 0.072) and a lower percent as carbohydrate (P = 0.065).
Table 2. Associations of CLOCK 3111TC SNP with dietary intake.
| TT | CC+TC | ||||
| Mean | SEM | Mean | SEM | P | |
| Total Energy (kcal/day) | 2069.96 | 34.78 | 2086.91 | 37.63 | 0.741 |
| Proteins (%) | 16.58 | 0.23 | 17.29 | 0.24 | 0.032 |
| g/day | 84.59 | 1.59 | 87.26 | 1.72 | 0.257 |
| Carbohydrates (%) | 37.87 | 0.47 | 36.76 | 0.44 | 0.065 |
| g/day | 151.66 | 2.80 | 146.02 | 3.00 | 0.149 |
| Fiber (g/day) | 19.25 | 0.54 | 18.15 | 0.58 | 0.163 |
| Fats (%) | 45.20 | 0.38 | 46.18 | 0.41 | 0.072 |
| g/day | 86.75 | 1.85 | 96.41. | 1.73 | 0.894 |
| MUFA% (total fat) | 56.02 | 0.39 | 54.92 | 0.42 | 0.045 |
| PUFA% (total fat) | 13.65 | 0.19 | 13.75 | 0.20 | 0.711 |
| SFA% (total fat) | 29.58 | 0.41 | 30.42 | 0.44 | 0.162 |
| Trans FA (g) | 0.58 | 0.06 | 0.76 | 0.06 | 0.039 |
Abbreviations used: MUFA; Monounsaturated fatty acids, PUFA; Polyunsaturated fatty acids, SFA; Saturated fatty acids.
Adjusted for sex, age and study site.
CLOCK 3111T/C, Sleep duration, Morningness/eveningness questionnaire and physical activity
Carriers of the minor C allele reported shorter daily sleep duration (h) Mean ± SEM (7.0±0.051) than TT homozygotes (7.3±0.058) (P = 0.039). With respect to the Morningness/eveningness questionnaire, in response to the question “At what time of the day do you think that you reach your “feeling best” peak?” C carriers were more represented in the “feeling best in the evening” category than TT subjects who comprised a larger proportion of the ‘feeling best in the morning’ subjects (P = 0.007; Table 3). Specifically, 57% of the subjects feeling best in the morning were TT subjects while 43% were C carriers whereas 53% of subjects feeling best in the evening were C carriers and 47% were TT carriers. Similar findings were obtained for other morningness/eveningness related questions which supports the classification of C carriers as evening persons ( Table 3 ). This evening preference could contribute to lower physical activity and resistance to weight loss among C carriers. Indeed, among the minor allele C carriers an inverse and significant correlation was found between evening preference (as assessed by the morning-evening-score) and physical activity (r = −0.186, P = 0.007).
Table 3. Genotype distribution of CLOCK 3111T/C according to Morningness/Eveningness characteristics.
| Time of the day feeling best | Time of the day with high mental performance | |||||||||||||
| Morning | Evening | Feeling best in the morning | Morning | Evening | Morning mental performance | |||||||||
| CLOCK 3111T/C | n | % | n | % | P value | OR (95% CI) | P value | n | % | n | % | P value | OR (95% CI) | P value |
| CC+TC | 225 | 43 | 109 | 53 | 0.007 | 0.684(0.491–0.953) | 0.024 | 276 | 44 | 58 | 54 | 0.028 | 0.664(0.440–1.00) | 0.049 |
| TT | 301 | 57 | 96 | 47 | 351 | 56 | 49 | 45 | ||||||
ORs were calculated for combined groups of minor allele carriers (CC+TC) compared with TT subjects. Adjusted for sex, age and study site.
Discussion
We initially detected a relationship between the CLOCK 3111T/C SNP and weight loss in a subset (n = 500) of the current population in which carriers of the minor allele (C) were less successful losing weight in response to a Mediterranean diet than their TT counterparts [8]. In the current study, we investigated factors underlying this association and demonstrated that these effects may be driven by behavioral factors and changes in ghrelin levels. Our results support the notion that the CLOCK locus influences behaviors related to weight loss, such as sleep reduction and evening preference, as well as appetite regulators such as plasma ghrelin levels.
Successful treatment of obesity represents a major health care challenge. Behavioral therapy has been proposed as part of weight loss programs. Its purpose is to facilitate the identification of triggers of inappropriate behavior conducive to weight gain, including excessive caloric intake and reduced physical activity [26]. Behavioral therapy is also used to develop appropriate responses based on the individual triggers [27]. Identification of loci involved in behavior may help to achieve more effective and individually tailored therapeutic strategies [28]–[30]. Our previous and current results show that the CLOCK 3111T/C SNP may contribute to this goal. Specifically, carriers of the minor allele C had more difficulty losing weight in the long term than TT carriers (3 kg difference).
It has been previously reported the CLOCK 3111T/C SNP may be functional through modification of mRNA stability and half life, thus influencing CLOCK translation and protein levels and affecting circadian rhythms and sleep duration [31]. Genotype-based differences in activity and sleep patterns have been shown in the context of bipolar disorders. Affected subjects and carriers of the minor C allele demonstrate a reduction in sleep duration which may affect the psychological and behavioral aspects of this mental illness [32], [33]. Likewise in our obese population, CLOCK 3111C carriers reported shorter sleep duration than TT carriers, and reduced sleep has reported to be obesogenic [34].
A number of mechanisms have been proposed to explain the association between reduced sleep and obesity [35]. One of them involves increased appetite resulting from alterations in leptin and/or ghrelin levels [36]. Alternatively short sleep duration could lead to weight gain by increasing the time available to eat [35]. Finally, it has been hypothesized that weight gain may be related to decreased energy expenditure resulting from increased fatigue and altered thermoregulation [35], [37].
With respect to the CLOCK 3111T/C variant, C carriers displayed significantly higher ghrelin plasma values than non-carriers, and this situation was particularly evident in the older group (≥38 ys). Moreover among C carriers, ghrelin was significantly and inversely correlated with weight loss. Epidemiological studies have shown a strong association between short sleep duration and higher ghrelin values. This mechanism activates neuropeptide Y (NPY)/agouti-related protein (AgRP) and inhibits proopiomelanocortin (POMC)/cocaine- and amphetamine-regulated transcript (CART) neurons, resulting in a net positive feeding signal [38]. Further support for the regulation of ghrelin by circadian clocks derived from mice models showed that in the absence of circadian clocks, ghrelin is no longer rhythmically expressed [39]. It remains to be determined how gastric clock genes regulate ghrelin synthesis and secretion; moreover, ghrelin plays a role in the anticipation of eating, including timing of meals, further affecting long-term regulation of body weight [40].
We did not find any relationship between leptin plasma values and the CLOCK SNP suggesting that this specific variant did not exert a significant effect on leptin regulation or, alternatively, that the specific characteristics of this population, all subjects in the overweight/obese range, prevented us from detecting associations that might be present in the general population.
Dietary habits could also be an underlying factor in the particular resistance of minor C allele carriers to losing weight. Evidence suggests that the Mediterranean Diet contributes to maintaining a healthy body weight [41]–[43]. In our study, C carriers of the CLOCK3111 T/C SNP showed a lower adherence to the Mediterranean Diet than TT subjects, and favored the consumption of protein, from animal sources and processed food, as suggested by the higher intake of trans fatty acids. This dietary pattern may be driving the less successful outcome of the weight loss program observed among the C allele carriers. In fact, olive oil consumed in the context of an energy balanced diet may facilitate weight control. Our group has shown that consumption of oleic acid is associated with lower adipocyte numbers in adipose tissue, suggesting that oleic acid intake may limit hyperplasia in obese subjects [44].
The other side of the energy balance is expenditure [35]. It has been reported that chronic sleep deprivation leads to morning tiredness and daylong feelings of fatigue that leads to reduced physical activity [45]. In the present study, the presence of the minor C allele was associated with reduced sleep and, consequently, with increased reporting of morning fatigue, lower mental performance in the morning and a preference for the evening hours. Moreover, among C allele carriers the evening preference was inversely correlated to physical activity in the current study, which was consistent with a previous report using objective measures of activity levels based on actigraphic devices [33], reinforcing our findings for the role of the CLOCK locus in sleep and behavioral preferences.
In conclusion, sleep reduction with changes in ghrelin values, alterations of eating behaviors and evening preference could be affecting weight and weight loss among CLOCK 3111C carriers. Our results support the hypothesis that the influence of the CLOCK gene may extend to a broad range of variables linked with human behaviors. Identifying CLOCK genotypes in patients may assist therapists in identifying the roots of the weight problem at the individual level and contribute to a more personalized and successful treatment.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work was supported by the Government of Education, Science and Research of Murcia (Project BIO/FFA 07/01-0004) and by The Spanish Government of Science and Innovation (projects AGL2008-01655/ALI) National Heart, Lung, and Blood Institute grants HL-54776, National Institute of Diabetes and Digestive and Kidney Diseases, Grant Number DK075030 and by contracts 53-K06-5-10 and 58-1950-9-001 from the US Department of Agriculture Research. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Garaulet M, Madrid JA. Chronobiological aspects of nutrition, metabolic syndrome and obesity. Adv Drug Deliv Rev May 22. 2010;22 doi: 10.1016/j.addr.2010.05.005. Available: http://www.ncbi.nlm.nih.gov/pubmed/20580916. Accesed 2010 Jul. [DOI] [PubMed] [Google Scholar]
- 2.Garaulet M, Gómez-Abellán P, Madrid JA. Chronobiology and obesity: the orchestra out of tune. Clin Lipidol. 2010;5:181–188. [Google Scholar]
- 3.Karlsson B, Knutsson A, Lindahl B. Is there an association between shift work and having a metabolic syndrome? Results from a population based study of 27,485 people. Occup Environ Med. 2001;58:747–752. doi: 10.1136/oem.58.11.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.von Schantz M. Phenotypic effects of genetic variability in human clock genes on circadian and sleep parameters. J Genet. 2008;87:513–519. doi: 10.1007/s12041-008-0074-7. [DOI] [PubMed] [Google Scholar]
- 5.Garaulet M, Lee YC, Shen J, Parnell LD, Arnett DK, et al. CLOCK genetic variation and metabolic syndrome risk: modulation by monounsaturated fatty acids. Am J Clin Nutr. 2009;90:1466–1475. doi: 10.3945/ajcn.2009.27536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scott EM, Carter AM, Grant PJ. Association between polymorphisms in the Clock gene, obesity and the metabolic syndrome in man. Int J Obes (Lond) 2008;32:658–662. doi: 10.1038/sj.ijo.0803778. [DOI] [PubMed] [Google Scholar]
- 7.Sookoian S, Gemma C, Gianotti TF, Burgueño A, Castaño G, et al. Genetic variants of Clock transcription factor are associated with individual susceptibility to obesity. Am J Clin Nutr. 2008;87:1606–1615. doi: 10.1093/ajcn/87.6.1606. [DOI] [PubMed] [Google Scholar]
- 8.Garaulet M, Corbalán MD, Madrid JA, Morales E, Baraza JC, et al. CLOCK gene is implicated in weight reduction in obese patients participating in a dietary programme based on the Mediterranean diet. Int J Obes (Lond) 2010;34:516–523. doi: 10.1038/ijo.2009.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lamont EW, Legault-Coutu D, Cermakian N, Boivin DB. The role of circadian clock genes in mental disorders. Dialogues Clin Neurosci. 2009;9(3):333–42. doi: 10.31887/DCNS.2007.9.3/elamont. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kotronoulas G, Stamatakis A, Stylianopoulou F. Hormones, hormonal agents, and neuropeptides involved in the neuroendocrine regulation of sleep in humans. Hormones (Athens) 2009;8:232–48. doi: 10.14310/horm.2002.1239. Review. [DOI] [PubMed] [Google Scholar]
- 11.Gangwisch JE. Epidemiological evidence for the links between sleep, circadian rhythms and metabolism. Obes Rev. 2009;10:37–45. doi: 10.1111/j.1467-789X.2009.00663.x. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vanitallie TB. Sleep and energy balance, Interactive homeostatic systems. Metabolism. 2006;55:S30–35. doi: 10.1016/j.metabol.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 13.Garaulet M, Pérez-Llamas F, Zamora S, Tébar FJ. Weight loss and Possible Reasons for Dropping out of a Dietary/Behavioural Programme in the Treatment of Overweight Patients. J Hum Nutr Diet. 1999;219-227 [Google Scholar]
- 14.Corbalán MD, Morales EM, Canteras M, Espallardo A, Hernández T, et al. Effectiveness of cognitive-behavioral-therapy based on the Mediterranean diet for the treatment of obesity. Nutrition. 2009;25:861–869. doi: 10.1016/j.nut.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 15.Serra-Majem L, Aranceta J. SENC Working Group on Nutritional Objectives for the Spanish Population. Spanish Society of Community Nutrition. Nutritional objectives for the Spanish population. Consensus from the Spanish Society of Community Nutrition. Public Health Nutr. 2001;4:1409–1413. doi: 10.1079/phn2001229. [DOI] [PubMed] [Google Scholar]
- 16.Ferrario VF, Sforza C, Schmitz JH, Miani A, Taroni G. Fourier analysis of human soft tissue facial shape: Sex differences in normal adults. J Anat. 1995;187:593–602. [PMC free article] [PubMed] [Google Scholar]
- 17.Horne JA, Östberg O. A self-assessment questionnaire to determine morningness–eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110. [PubMed] [Google Scholar]
- 18.Taillard J, Philip P, Chastang JF, Bioulac B. Validation of Horne and Ostberg morningness-eveningness questionnaire in a middle-aged population of French workers. J Biol Rhythms. 2004;19:76–86. doi: 10.1177/0748730403259849. [DOI] [PubMed] [Google Scholar]
- 19.Perez-Llamas F, Garaulet M, Herrero F, Palma JT, Pérez de Heredia F, et al. Multivalent informatics application for studies of the nutritional status of the population. Assessment of food intake. Nutr hosp. 2004;19:160–166. [PubMed] [Google Scholar]
- 20.Mataix J, Mañas M, Llopis J, Martínez E. Granada, Spain: Instituto de Nutrición y Tecnología, Universidad de Granada; 1995. Tabla de composición de alimentos españoles (in Spanish). (Table of composition of Spanish foods.) [Google Scholar]
- 21.Moreiras O, Carvajal A, Cabrera L. Pirámide, SA, ed. Madrid; 1995. Tablas de composición de alimentos (in Spanish). (Tables of composition of foods.) [Google Scholar]
- 22. IPAQ (International Physical Activity Questionnaire) website. Available: http://www.ipaq.ki.se/ipaq.htm. Accessed 2010.
- 23.Craig C, Marshall AL, Sjöström M, Bauman AE, Booth ML, et al. International Physical Activity Questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 24. HelixTree Manual, Version 5.3.0. (2010) Available: http://goldenhelix.com/HelixTreeManual/compositehaplotypemethodchm.html#x133-75400023.7. Accessed 2010 July 13. [Google Scholar]
- 25.Departamento de Nutrición y Bromatología I. Tablas recomendadas de energía y nutrientes para la población española (in Spanish). 1994. (Recommended Tables for energy and nutrients for Spanish population). Universidad Complutense de Madrid. Madrid.
- 26.Garaulet M, Pérez de Heredia F. Behavioural therapy in the treatment of obesity (II): role of the Mediterranean diet. Nutr Hosp. 2010;25:9–17. Review. [PubMed] [Google Scholar]
- 27.Garaulet M, Pérez de Heredia F. Behavioural therapy in the treatment of obesity (I): new directions for clinical practice. Nutr Hosp. 2009;24:629–39. Review. [PubMed] [Google Scholar]
- 28.Haupt A, Thamer C, Machann J, Kirchhoff K, Stefan N, et al. Impact of Variation in the FTO Gene on Whole Body Fat Distribution, Ectopic fat and Weight Loss. Obesity. 2008;16:1969–1972. doi: 10.1038/oby.2008.283. [DOI] [PubMed] [Google Scholar]
- 29.Aberle J, Flitsch J, Beck NA, Mann O, Busch P, et al. Genetic variation may influence obesity only under conditions of diet: Analysis of three candidate genes. Mol Genet Metab. 2008;95:188–191. doi: 10.1016/j.ymgme.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 30.Sørensen TI, Boutin P, Taylor MA, Larsen LH, Verdich C, et al. NUGENOB Consortium. Genetic polymorphisms and weight loss in obesity: a randomised trial of hypo-energetic high- versus low-fat diets. PLoS Clin Trials. 2006;1:e12. doi: 10.1371/journal.pctr.0010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Monteleone P, Tortorella A, Docimo L, Maldonato MN, Canestrelli B, et al. Investigation of 3111T/C polymorphism of the CLOCK gene in obese individuals with or without binge eating disorder: Association with higher body mass index. Neurosci Lett. 2008;435:30–33. doi: 10.1016/j.neulet.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 32.Benedetti F, Radaelli D, Bernasconi A, Dallaspezia S, Falini A, et al. Clock genes beyond the clock: CLOCK genotype biases neural correlates of moral valence decision in depressed patients. Genes Brain Behav. 2008;7:20–25. doi: 10.1111/j.1601-183X.2007.00312.x. [DOI] [PubMed] [Google Scholar]
- 33.Benedetti F, Dallaspezia S, Fulgosi MC, Lorenzi C, Serretti A, et al. Actimetric evidence that CLOCK 3111 T/C SNP influences sleep and activity patterns in patients affected by bipolar depression. Am J Med Genet B Neuropsychiatr Genet. 2007;144B:631–635. doi: 10.1002/ajmg.b.30475. [DOI] [PubMed] [Google Scholar]
- 34.Hamet P, Tremblay J. Genetics of the sleep-wake cycle and its disorders. Metabolism. 2006;55:S7–S12. doi: 10.1016/j.metabol.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 35.Van Cauter E, Knutson KL. Sleep and the epidemic of obesity in children and adults. Eur J Endocrinol. 2008;159:S59–66. doi: 10.1530/EJE-08-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLOS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shaw PJ. Thermoregulatory changes. In: Kushida CA, editor. Sleep Deprivation: Basic Science, Physiology, and Behavior. New York: Marcel Dekker; 2005. pp. 319–338. [Google Scholar]
- 38.Adamantidis A, de Lecea L. Sleep and metabolism: shared circuits, new connections. Trends Endocrinol Metab. 2008;19:362–70. doi: 10.1016/j.tem.2008.08.007. Review. [DOI] [PubMed] [Google Scholar]
- 39.LeSauter J, Hoque N, Weintraub M, Pfaff DW, Silver R. Stomach ghrelin-secreting cells as food-entrainable circadian clocks. Proc Natl Acad Sci U S A 106: 13582-13587. Erratum in: Proc Natl Acad Sci U S A (2009) 2009;106:17241–17242. doi: 10.1073/pnas.0906426106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cummings DE, Purnell JQ, Frayo RS, Schmidova K, Wisse BE, et al. A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes. 2001;50:1714–1719. doi: 10.2337/diabetes.50.8.1714. [DOI] [PubMed] [Google Scholar]
- 41.Buckland G, Bach A, Serra-Majem L. Obesity and the Mediterranean diet: A systematic review of observational and intervention studies. Obes Rev. 2008;9:582–593. doi: 10.1111/j.1467-789X.2008.00503.x. [DOI] [PubMed] [Google Scholar]
- 42.Giugliano D, Esposito K. Mediterranean diet and metabolic diseases. Curr Opin Lipidol. 2008;19:63–68. doi: 10.1097/MOL.0b013e3282f2fa4d. [DOI] [PubMed] [Google Scholar]
- 43.Méndez MA, Popkin BM, Jakszyn P, Berenguer A, Tormo MJ, et al. Adherence to a Mediterranean diet is associated with reduced 3-year incidence of obesity. J Nutr. 2006;136:2934–2938. doi: 10.1093/jn/136.11.2934. [DOI] [PubMed] [Google Scholar]
- 44.Garaulet M, Hernandez-Morante JJ, Lujan J, Tebar FJ, Zamora S. Relationship between fat cell size and number and fatty acid composition in adipose tissue from different fat depots in overweight/obese humans. Int J Obes (Lond) 2006;30:899–905. doi: 10.1038/sj.ijo.0803219. [DOI] [PubMed] [Google Scholar]
- 45.Knutson KL. The association between pubertal status and sleep duration and quality among a nationally representative sample of U. S. adolescents. Am J Hum Biol. 2005;17:418–424. doi: 10.1002/ajhb.20405. doi: 10.1002/ajhb.20405. [DOI] [PubMed] [Google Scholar]