Abstract
Introduction:
The present study was conducted to establish the positive predictive value of congenital cardiac malformation diagnoses registered in the Danish National Patient Registry (NPR), thereby exploring whether the NPR can serve as a valid tool for epidemiologic studies of congenital cardiac malformations.
Materials and methods:
The study population comprised every individual born from 2000 to 2008 who was registered in the NPR with a congenital cardiac malformation diagnosis and treated at one of the two national departments of pediatric cardiology. Positive predictive values were established comparing NPR information with the clinical record of each individual.
Results:
A total of 2952 patients with a total of 3536 diagnoses were eligible for validation. Review of their clinical records unveiled no patient without cardiac malformation. In 98% (98%–99%) of the cases, the NPR diagnosis could be found as the discharge diagnosis in the patient’s clinical record, and in 90% (89%–91%) of the cases the NPR diagnosis was considered a true reflection of the patient’s actual malformation.
Conclusions:
Our study verifies that the present study population retrieved from the NPR is a valid tool for epidemiological research within the topic of congenital cardiac malformations, given that the research question is not dependent on a fully established sensitivity of the NPR. Precautions should be made regarding cardiac malformations characterized by low prevalence or poor predictive values, and the reported validity should not be extrapolated beyond the study period.
Keywords: congenital cardiac malformation, registry, validation
Introduction
The etiology of congenital cardiac malformation is heterogeneous and only understood to a limited extent, although both noninherited risk factors and genetic causes have been identified.1–4 Additional knowledge concerning the etiology of different cardiac malformations may be obtained through large population-based epidemiologic studies,5 thereby identifying study populations for follow-up or for case-control studies. Genetic screening studies may also be applied to such populations.
Large datasets of patients with cardiac malformations can be extracted from the Danish National Patient Registry (NPR), which contains data from all hospitalizations in Denmark since 1977.6 Reporting of data to this registry is mandatory for all Danish hospitals and is further encouraged by the government funding system.
Though originally established as an administrative tool, the NPR also serves as a tool for epidemiologic research because registry data provide a substantial number of patients at a low cost and, presumably, with little selection bias.7,8 Evidently, the quality of research based on registry data relies heavily on the validity of the reported diagnoses. Continuous validation of the information in the NPR is therefore of paramount importance.
The completeness and validity of administrative data are good,9–11 whereas the validity of discharge diagnoses, expressed as positive predictive value (PPV), varies depending on the clinical specialty. So far, only one small study has outlined the PPV of selected cardiac malformation diagnoses, reporting excellent validity for common diagnoses but substantial uncertainty regarding less common diagnoses.12
Hence, the aim of the present study was to establish the PPV of cardiac malformation diagnoses registered in the NPR for Danish children born during the period 2000–2008, thereby providing additional knowledge regarding this registry as a tool for epidemiologic studies of congenital cardiac malformations.
Materials and methods
Data sources
The NPR was established in 1977. Since 1994, discharge diagnoses have been recorded according to the 10th revision of the International Classification of Diseases (ICD-10) from the World Health Organization, in which cardiac malformations are categorized into six groups, denoted DQ20–DQ25. A fifth digit specifies the malformation, whereby diagnoses range from DQ20.0–DQ25.9. Data are stored according to a unique personal identification number, which is allocated to every Danish citizen at birth or immigration. With this personal identification number, it is possible to link information from different registries and clinical records (CRs) regarding any particular individual.
The CR of each patient was identified by use of the personal identification number.
The Medical Birth Registry contains information on all births in Denmark since 1973, including gestational age, Apgar score, gender, birth weight, and complications. Reporting is mandatory and performed by midwives subsequent to every delivery.13 This registry was exclusively used to identify patients born prematurely.
The number of live births within the study period was provided by Statistics Denmark.
Study population
The study population comprised every individual born from 2000 to 2008 who was registered in the NPR with a diagnosis of congenital cardiac malformation (DQ20.0–DQ25.9) and evaluated or treated at one of the two national departments of pediatric cardiology. In Denmark, all children with cardiac malformations requiring surgical or medical treatment are referred to one of these national departments at the university hospitals in Copenhagen or Aarhus. Minor defects not requiring treatment are initially referred to the nearest hospital according to admission areas, including the university hospitals. Thus, our strategy resulted in an unbiased population from the university hospitals counting cardiac malformations of all degrees of severity.
Patients registered with patent ductus arteriosus (DQ25.0) were excluded if they were registered as premature in the Medical Birth Registry. In addition, we excluded unspecific malformations (DQ20.9, DQ21.9, DQ22.9, DQ23.9, DQ24.9, and DQ25.9).
The CRs were scrutinized at the two national departments of pediatric cardiology. In Aarhus, there was electronic access to the CR. In Copenhagen, there was electronic access to discharge diagnoses, and when further information was needed, the CR was found in an archive. Three observers scrutinized the CRs according to the same criteria, and cases of doubt were ultimately clarified by the senior pediatric cardiologist (co-author JB).
Definitions and data analysis
The dataset was validated at two levels, measuring the accuracy of the NPR information with the CR as gold standard. These measures were calculated as PPVs, with 95% confidence intervals for every specific diagnosis.
PPV of registration
First, we observed whether the NPR diagnosis was registered as a discharge diagnosis in the patient’s CR. The PPV of registration was calculated as the number of patients with consistency between the NPR and the CR divided by the number of patients registered with the identical diagnosis in the NPR. This figure reflected the likelihood of an NPR diagnosis being registered in the patient’s CR as a discharge diagnosis, irrespective of the diagnosis being correct or not.
PPV of malformation
Second, we evaluated whether the NPR diagnosis reflected the patient’s actual malformation as registered in the CR. We accepted the diagnosis as the patient’s actual malformation if it was persistently recorded at several visits, at surgery or autopsy, or if it was the prevailing view at the end of follow-up (eg, death or emigration). Thus, rather than interpreting the content of the CR, we relied on the conclusions of the investigations in the form of diagnoses. The PPV of malformation was calculated as the number of patients with consistency between the NPR and the patient’s malformation (as described previously) divided by the number of patients registered with the identical diagnosis in the NPR. This figure reflected the likelihood of an NPR diagnosis representing the patient’s actual malformation.
We relied on the normal approximation of the binomial distribution, although some of the less frequent diagnoses did not apply to the numeral criteria for this. Data analysis was performed in Stata 10. Our approach applied accepted guidelines for evaluation of secondary data sources.7
Ethics
The study was approved by the Danish Data Protection Agency (J.no. 2008-41-2288) and the National Board of Health (J.no. 7-505-29-1013).
Results
Study population
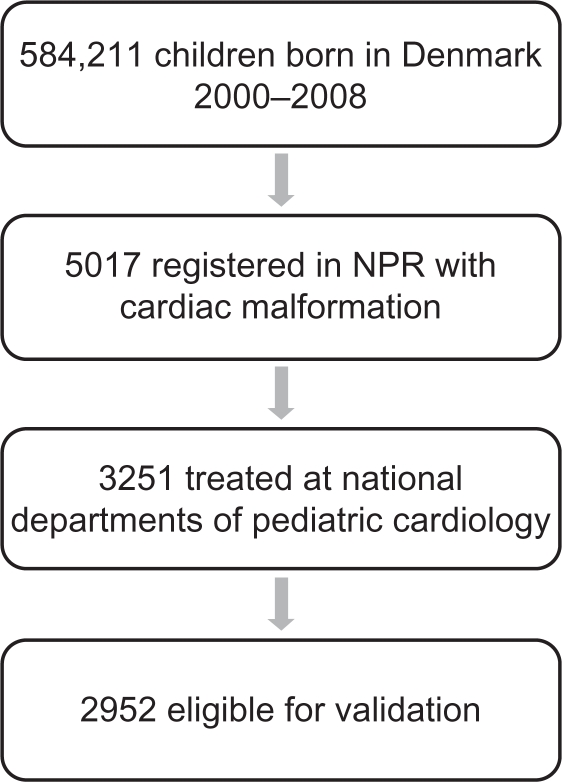
The patient inclusion is summarized in Figure 1. A total of 584,211 children were born in Denmark during 2000–2008. A total of 5017 patients had received a diagnosis of one or more cardiac malformations at the time of data retrieval from the NPR (February 2009). A total of 3251 patients (65%) were evaluated or treated at one of the two national departments of pediatric cardiology in Copenhagen and Aarhus, whereas 1766 (35%) were exclusively diagnosed at the regional hospitals and were therefore excluded from the study. These patients were primarily registered with ventricular septal defects (n = 597), atrial septal defects (n = 459), unspecified malformations (n = 199), and patent ductus arteriosus (n = 190). Altogether, these common malformations comprised 82% of the diagnoses outside Copenhagen and Aarhus; 34 of the patients had died at the time of data retrieval.
Figure 1.
Study population.
Abbreviation: NPR, National Patient Registry.
Of the 3251 patients treated at the national departments of pediatric cardiology, 183 were excluded because of physiologic malformations or unspecific malformations, or both (as described under the study population). Thus, 3068 patients were eligible for validation. Clinical records were unavailable for 116 of the patients. Although not evenly distributed among the diagnostic groups DQ20–DQ25, no single diagnosis contributed considerably to this number, and therefore the missing data were considered negligible. Consequently, our population consisted of 2952 patients. They were registered with a total of 3536 diagnoses within DQ20.0–DQ25.8. Males comprised 50.7%, and females comprised 49.3%. The majority (57.1%) were evaluated in Copenhagen, and the remaining (42.9%) were evaluated in Aarhus. A total of 265 patients had died at the time of data retrieval.
A review of the 2952 clinical records did not unveil any patient without cardiac malformation. Thus, a registration of a cardiac malformation in the NPR was consistent with a cardiac malformation in 100% of the patients.
PPV of registration
The cardiac malformations consisted of 44 specific diagnoses. Overall, PPV of registration was 98% (98%–99%). We observed a similar accuracy between the different groups DQ20–DQ25 ranging from 96% (93%–97%) in DQ20 (congenital malformations of cardiac chambers and connections) to 100% (95%–100%) in DQ24 (other congenital malformations of the heart). The results are listed in Table 1.
Table 1.
Results
| ICD-10 code | N cases |
Positive predictive value of registration |
Positive predictive value of malformation |
||
|---|---|---|---|---|---|
| N | % (95% CI) | N | % (95% CI) | ||
| DQ20.0: Common arterial trunk | 48 | 47 | 98 (89–100) | 27 | 56 (41–71) |
| DQ20.1: Double outlet right ventricle | 90 | 82 | 91 (83–96) | 51 | 57 (46–67) |
| DQ20.2: Double outlet left ventricle | 8 | 6 | 75 (35–97) | 3 | 38 (9–76) |
| DQ20.3: Transposition of great vessels (complete) | 189 | 188 | 99 (97–100) | 171 | 90 (85–94) |
| DQ20.4: Double inlet ventricle | 61 | 57 | 93 (84–98) | 29 | 48 (35–61) |
| DQ20.5: Ventricular inversion | 18 | 17 | 94 (73–100) | 9 | 50 (26–74) |
| DQ20.6: Isomerism of atrial appendages | 10 | 9 | 90 (55–100) | 7 | 70 (35–93) |
| DQ20.8: Other malformations of cardiac chambers and connections | 6 | 5 | 83 (36–100) | 4 | 67 (22–96) |
| DQ20: Congenital malformations of cardiac chambers and connections | 430 | 411 | 96 (93–97) | 301 | 70 (65–74) |
| DQ21.0: Ventricular septal defect | 904 | 899 | 99 (99–100) | 883 | 98 (96–99) |
| DQ21.1: Atrial septal defect | 535 | 528 | 99 (97–99) | 517 | 97 (95–98) |
| DQ21.2: Atrioventricular septal defect | 184 | 183 | 99 (97–100) | 171 | 93 (88–96) |
| DQ21.3: Tetralogy of Fallot | 210 | 209 | 100 (97–100) | 189 | 90 (85–94) |
| DQ21.4: Aortopulmonary septal defect | 8 | 8 | 100 (63–100) | 7 | 88 (47–100) |
| DQ21.8: Other malformations of cardiac septa | 3 | 3 | 100 (29–100) | 1 | 33 (8–91) |
| DQ21: Congenital malformations of cardiac septa | 1844 | 1830 | 99 (99–100) | 1768 | 96 (95–97) |
| DQ22.0: Pulmonary valve atresia | 52 | 52 | 100 (93–100) | 38 | 73 (59–84) |
| DQ22.1: Congenital pulmonary valve stenosis | 178 | 176 | 99 (96–100) | 163 | 92 (86–95) |
| DQ22.2: Congenital pulmonary valve insufficiency | 2 | 2 | 100 (16–100) | 1 | 50 (13–99) |
| DQ22.3: Other congenital malformations of pulmonary valve | 1 | 1 | 100 (3–100) | 1 | 100 (3–100) |
| DQ22.4: Congenital tricuspid stenosis | 18 | 16 | 89 (65–99) | 15 | 83 (59–96) |
| DQ22.5: Ebstein’s anomaly | 14 | 14 | 100 (77–100) | 14 | 100 (77–100) |
| DQ22.6: Hypoplastic right heart syndrome | 22 | 19 | 86 (65–97) | 15 | 68 (45–86) |
| DQ22.8: Other congenital malformations of tricuspid valve | 11 | 8 | 73 (39–94) | 4 | 36 (11–69) |
| DQ22: Congenital malformations of pulmonary and tricuspid valves | 298 | 288 | 97 (94–98) | 251 | 84 (80–88) |
| DQ23.0: Congenital stenosis of aortic valve | 88 | 88 | 100 (96–100) | 85 | 97 (90–99) |
| DQ23.1: Congenital insufficiency of aortic valve | 16 | 16 | 100 (79–100) | 15 | 94 (70–100) |
| DQ23.2: Congenital mitral stenosis | 5 | 5 | 100 (48–100) | 3 | 60 (15–95) |
| DQ23.3: Congenital mitral insufficiency | 21 | 21 | 100 (84–100) | 16 | 76 (53–92) |
| DQ23.4: Hypoplastic left heart syndrome | 98 | 97 | 99 (94–100) | 84 | 86 (77–92) |
| DQ23.8: Other congenital malformations of aortic and mitral valves | 11 | 10 | 91 (59–100) | 9 | 82 (48–98) |
| DQ23: Congenital malformations of aortic and mitral valves | 239 | 237 | 99 (97–100) | 212 | 89 (84–92) |
| DQ24.0: Dextrocardia | 5 | 5 | 100 (48–100) | 4 | 80 (28–99) |
| DQ24.2: Cor triatriatum | 3 | 3 | 100 (29–100) | 3 | 100 (29–100) |
| DQ24.3: Pulmonary infundibular stenosis | 11 | 11 | 100 (72–100) | 10 | 91 (59–100) |
| DQ24.4: Congenital subaortic stenosis | 24 | 24 | 100 (86–100) | 20 | 83 (63–95) |
| DQ24.5: Malformation of coronary vessels | 9 | 9 | 100 (66–100) | 9 | 100 (66–100) |
| DQ24.6: Congenital heart block | 8 | 8 | 100 (63–100) | 8 | 100 (63–100) |
| DQ24.8: Other specified congenital malformations of heart | 7 | 7 | 100 (59–100) | 4 | 57 (18–90) |
| DQ24: Other congenital malformations of heart | 67 | 67 | 100 (95–100) | 58 | 87 (76–94) |
| DQ25.0: Patent ductus arteriosus | 262 | 261 | 100 (98–100) | 252 | 96 (93–98) |
| DQ25.1: Coarctation of aorta | 207 | 207 | 100 (98–100) | 199 | 96 (93–98) |
| DQ25.2: Atresia of aorta | 45 | 43 | 96 (85–99) | 38 | 84 (71–94) |
| DQ25.3: Stenosis of aorta | 17 | 17 | 100 (80–100) | 17 | 100 (80–100) |
| DQ25.4: Other congenital malformations of aorta | 25 | 22 | 88 (69–97) | 17 | 68 (46–85) |
| DQ25.5: Atresia of the pulmonary artery | 32 | 32 | 100 (89–100) | 27 | 84 (67–95) |
| DQ25.6: Stenosis of pulmonary artery | 48 | 48 | 100 (93–100) | 43 | 90 (77–97) |
| DQ25.7: Other congenital malformations of pulmonary artery | 7 | 7 | 100 (59–100) | 6 | 86 (42–100) |
| DQ25.8: Other congenital malformations of great arteries | 15 | 11 | 73 (45–92) | 8 | 53 (27–79) |
| DQ25: Congenital malformations of great arteries | 658 | 648 | 98 (97–99) | 607 | 92 (90–94) |
| DQ20–DQ25 | 3536 | 3481 | 98 (98–99) | 3197 | 90 (89–91) |
Abbreviations: CI, confidence interval; ICD-10, 10th revision of the International Classification of Diseases.
PPV of malformation
Overall, PPV of malformation was 90% (89%–91%). The figures differed significantly according to specific diagnoses. DQ20 (congenital malformations of cardiac chambers and connections) achieved a PPV of 70% (65%–74%), as opposed to DQ21 (congenital malformations of cardiac septa), where the PPV was 96% (95%–97%). The figures from the two hospitals did not differ substantially. The results are listed in Table 1.
Disregarding the least common malformations, the highest PPV was achieved with DQ21.0 ventricular septal defect (98% [96%–99%]), DQ21.1 atrial septal defect (97% [95%–98%]), and DQ23.0 congenital stenosis of the aortic valve (97% [90%–99%]). The lowest PPV was achieved with DQ20.4 double inlet ventricle (48% [35%–61%]), DQ20.0 common arterial trunk (56% [41%–71%]), and DQ20.1 double outlet right ventricle (57% [46%–67%]).
Discussion
This study evaluated registry information in 2952 Danish children with congenital cardiac malformations. Overall, we report PPV of registration 98% (98%–99%) and PPV of malformation 90% (89%–91%) on 44 specific diagnoses. Thus, in 98% of the cases, the NPR diagnosis could be found as a discharge diagnosis in the patient’s clinical record, and in 90% of the cases, the diagnosis was considered a true reflection of the patient’s actual malformation.
The validity of NPR data has been established for many diagnoses with CR as the gold standard. The PPVs vary from 40% in a study of hypertension to 97% in a study comprising patients with Crohn’s disease.14,15 To our knowledge, only one single study has validated registry information of congenital cardiac malformations. Jepsen et al evaluated 418 clinical records of children with 17 different cardiac malformations diagnosed outside the university departments.12 In that study, only 89% (86%–92%) of the children actually carried a cardiac malformation. The PPV of malformations ranged from 0% to 100% and contained many wide confidence intervals due to the small population size.
We report higher PPVs for several reasons. We exclusively evaluated CRs from the national departments of pediatric cardiology, in which cardiac catheterization and cross-sectional conferences clarify cases of doubt. Jepsen et al12 only considered the ICD-10 code of the most severe type of cardiac malformation identified at the patient’s initial hospitalization. Furthermore, nearly one-tenth of the cases in the study by Jepsen et al were evaluated without an echocardiogram. In our study, all of the diagnoses were based on at least one echocardiogram.
However, we did achieve poor PPV for some malformations, reflecting the fact that registration of a discharge diagnosis in the NPR does not necessarily correspond to the prevailing clinical working diagnosis. This aspect is clearly illustrated by the difference between PPV of malformation and registration. For some diagnoses the discrepancy was pronounced. For example, some cases of DQ20.1 (double outlet right ventricle) were confused with tetralogy of Fallot or transposition with ventricular septal defect at first glance, and DQ22.0 pulmonary valve atresia was sometimes confused with pulmonary valve stenosis. In these cases, the first (and wrong) diagnoses reported to the NPR were evidently not corrected when the correct diagnosis was established. Clearly, precautions should be made when using the registry to study specific malformations with poor predictive values.
Limitations and strengths
Our results should be interpreted with the study limitations in mind. First, consistent registration of the same malformation is not necessarily evidence of a correct diagnosis; however, it is a reflection of the diagnosis that the patient is considered to have at a certain time, which is the basic term in clinical practice, as well as in epidemiologic analyses of data from the NPR.11 Second, some diagnoses were indeed very rare, rendering predictive values uncertain. Third, our setup did not allow us to evaluate the completeness (sensitivity) of the NPR, and, consequently, studies requiring a well-established sensitivity cannot be conducted on the present study population. Fourth, the study exclusively included children evaluated or treated at the two national departments of pediatric cardiology where diagnostic precision and expertise are highest. This selection strategy may hamper the external validity of the study. Finally, performing an unblinded review may bias our results. However, in a study by Nielsen et al in which NPR diagnoses were validated by both blinded and unblinded review of CRs, the PPVs were equal (61% [53%–70%] versus 63% [52%–73%]).14
One of the strengths of our study was the large population size, allowing for calculations with high statistical precision. The easy linkage between registries and the CRs allowed us to validate NPR information in 96% of our population. Finally, our study included all congenital cardiac malformations, and PPV calculations were performed on the specific level of 44 diagnoses within the ICD-10 code system.
Perspectives and conclusion
In conclusion, 100% of the patients in our dataset carry a cardiac malformation. The NPR reflects the CR discharge diagnoses in 98% of the cases, and the NPR reflects the patient’s true cardiac malformation in 90% of the cases.
Our study verifies that the present study population retrieved from the NPR is a valid tool for epidemiological research within the topic of congenital cardiac malformations, given that the research question is not dependent on a fully established sensitivity of the NPR. Precautions should be made regarding cardiac malformations characterized by low prevalence or PPVs, and the reported validity should not be extrapolated beyond the study period.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Loffredo CA. Epidemiology of cardiovascular malformations: prevalence and risk factors. Am J Med Genet. 2000;97(4):319–325. doi: 10.1002/1096-8628(200024)97:4<319::aid-ajmg1283>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 2.Jenkins KJ, Correa A, Feinstein JA, et al. Noninherited risk factors and congenital cardiovascular defects: current knowledge: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young: endorsed by the American Academy of Pediatrics. Circulation. 2007;115(23):2995–3014. doi: 10.1161/CIRCULATIONAHA.106.183216. [DOI] [PubMed] [Google Scholar]
- 3.Pierpont ME, Basson CT, Benson DW, Jr, et al. Genetic basis for congenital heart defects: current knowledge: a scientific statement from the American Heart Association Congenital Cardiac Defects Committee, Council on Cardiovascular Disease in the Young: endorsed by the American Academy of Pediatrics. Circulation. 2007;115(23):3015–3038. doi: 10.1161/CIRCULATIONAHA.106.183056. [DOI] [PubMed] [Google Scholar]
- 4.Kornosky JL, Salihu HM. Getting to the heart of the matter: epidemiology of cyanotic heart defects. Pediatr Cardiol. 2008;29(3):484–497. doi: 10.1007/s00246-007-9185-9. [DOI] [PubMed] [Google Scholar]
- 5.Botto LD, Lin AE, Riehle-Colarusso T, Malik S, Correa A. Seeking causes: classifying and evaluating congenital heart defects in etiologic studies. Birth Defects Res A Clin Mol Teratol. 2007;79(10):714–727. doi: 10.1002/bdra.20403. [DOI] [PubMed] [Google Scholar]
- 6.Danish National Patient Registry Homepage. 2010. http://www.sst.dk/Indberetning%20og%20statistik/Landspatientregisteret.aspx. Accessed December 22, 2010.
- 7.Sorensen HT, Sabroe S, Olsen J. A framework for evaluation of secondary data sources for epidemiological research. Int J Epidemiol. 1996;25(2):435–442. doi: 10.1093/ije/25.2.435. [DOI] [PubMed] [Google Scholar]
- 8.Frank L. Epidemiology. When an entire country is a cohort. Science. 2000;287(5462):2398–2399. doi: 10.1126/science.287.5462.2398. [DOI] [PubMed] [Google Scholar]
- 9.Sundhedsstyrelsen (National Board of Health) Evaluation of the Danish National Patient Registry 1990. 1993. Copenhagen.
- 10.Mosbech J, Jorgensen J, Madsen M, Rostgaard K, Thornberg K, Poulsen TD. The national patient registry. Evaluation of data quality. Ugeskr Laeger. 1995;157(26):3741–3745. [PubMed] [Google Scholar]
- 11.Andersen TF, Madsen M, Jorgensen J, Mellemkjoer L, Olsen JH. The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull. 1999;46(3):263–268. [PubMed] [Google Scholar]
- 12.Jepsen B, Jepsen P, Johnsen SP, Espersen GT, Sorensen HT. Validity of diagnoses of cardiac malformations in a Danish population-based hospital-discharge registry. Int J Risk Safe. 2006;18:77–81. [Google Scholar]
- 13.The Medical Birth Registry Homepage. 2010. http://www.sst.dk/Indberetning%20og%20statistik/Sundhedsstyrelsens%20registre/Foedselsregister.aspx. Available December 22, 2010.
- 14.Nielsen HW, Tuchsen F, Jensen MV. Validity of the diagnosis “essential hypertension” in the National Patient Registry. Ugeskr Laeger. 1996;158(2):163–167. [PubMed] [Google Scholar]
- 15.Fonager K, Sorensen HT, Rasmussen SN, Moller-Petersen J, Vyberg M. Assessment of the diagnoses of Crohn’s disease and ulcerative colitis in a Danish hospital information system. Scand J Gastroenterol. 1996;31(2):154–159. doi: 10.3109/00365529609031980. [DOI] [PubMed] [Google Scholar]