Abstract
Background
Point mutations of the BCR-ABL tyrosine kinase domain are considered the predominant cause of imatinib resistance in chronic myeloid leukemia. The expansion of mutant BCR-ABL-positive clones under selective pressure of tyrosine kinase inhibition is referred to as clonal selection; there are few data on the reversibility of this phenomenon.
Design and Methods
The changes of expression of mutant BCR-ABL-positive alleles after cessation of tyrosine kinase inhibitor treatment were examined in 19 patients with chronic myeloid leukemia harboring different mutations in a longitudinal follow-up. The proportion of mutant alleles was quantified by amplification of rearranged ABL sequences followed by mutation-specific restriction digestion, electrophoresis and densitometry. The size of mutant clones was established as a measure of the absolute amount of mutant cells considering the proportion of mutant BCR-ABL transcripts and the total level of BCR-ABL obtained by quantitative reverse transcriptase polymerase chain reaction.
Results
The median proportion of mutant transcripts was 97% before and 8% after cessation of tyrosine kinase inhibitor treatment indicating a relative decline of 88% within a median of 6 months. The relative decrease in the size of the mutant clones was 86%. Repeated selection and deselection of the mutant clone after resumption and second cessation of tyrosine kinase inhibitor treatment was observed in individual patients.
Conclusions
Deselection of mutant BCR-ABL-positive clones after cessation of tyrosine kinase inhibitor treatment might be a common, rapid and reproducible phenomenon, although some patients harboring the T315I mutation showed no deselection. Cessation of tyrosine kinase inhibitor treatment may lead to the regression of T315I mutant clones to a level under the limit of detection, offering the therapeutic option of resumed tyrosine kinase inhibitor treatment under close surveillance of the mutation status.
Keywords: chronic myeloid leukemia, imatinib resistance, drug resistance, BCR-ABL mutation
Introduction
Point mutations of the BCR-ABL tyrosine kinase domain are the major cause of imatinib resistance in chronic myeloid leukemia (CML).1–3 Up to now more than 100 mutations have been described affecting more than 70 amino acids causing resistance by heterogeneous molecular mechanisms.4–6 Highly sensitive methods for the detection of mutations in the case of suboptimal response have been introduced in the management of CML.1,7,8 Mutant BCR-ABL-positive clones have been shown to pre-exist treatment in imatinib-naïve patients and to outgrow the unmutated clone under the selective pressure of tyrosine kinase inhibition in a process known as clonal selection.9–12 Anecdotal cases of reversibility of clonal selection after cessation of treatment with a tyrosine kinase inhibitor (TKI) have been reported.13–15
In theory, the proliferative advantage of a resistant clone in the presence of a TKI does not imply a proliferative disadvantage in the absence of the TKI, indicating that the general assumption of clonal deselection after TKI discontinuation remains controversial. Besides, inhibition of drug affinity mutations may also contribute to alterations in the activity and substrate specificity of the BCR-ABL tyrosine kinase suggesting a possible gain or loss of function.2,16–19 Furthermore, clinical studies have revealed mixed dynamics in the outgrowth of mutant clones in the presence of imatinib supporting the notion that the model of clonal selection alone does not fully reflect the in vivo situation.10,20,21 Recently, it has been reported that imatinib-resistant mutant clones can disappear in patients receiving treatment with second-generation TKI.22,23
In this study we sought to investigate the dynamics of mutant BCR-ABL alleles in 19 CML patients resistant to imatinib and exposed to alternative non-TKI treatment modalities.
Design and Methods
Patients
Between 2001 and 2007, 75 CML patients who had hematologic resistance to TKI therapy due to a BCR-ABL kinase domain mutation detected by direct sequencing were identified (44 males, 31 females; median age 62 years, range 30–80). The disease phase at the start of TKI treatment was chronic phase (n=35), accelerated phase (n=25), and blast crisis (n=15). All patients were initially treated with imatinib; one patient was switched to nilotinib and one to dasatinib after failure of imatinib therapy.
A subgroup of 19 patients (11 males, 8 females; median age 63 years, range 31–73) received subsequent alternative treatment consisting of non-specific chemotherapy (17 after imatinib, one after imatinib/nilotinib, one after imatinib and subsequently after dasatinib, patient n. 8, Table 1), and had a follow up of at least 4 months after the change of treatment regimen (median 13 months, range 4–33). The disease phase at the onset of TKI treatment was chronic phase in 11 patients, accelerated phase in five patients and blast crisis in four (patient n. 8 started imatinib treatment in chronic phase and dasatinib treatment in accelerated phase). This subgroup expressed five different mutations, for which a semiquantitative detection assay had been established: Y253F, n=1; Y253H, n=4; E255K, n=5; T315I, n=8; M351T, n=2 (Table 1). Patient n. 8 was examined for two different mutations at two time-points: the first mutation (E255K) emerged under imatinib treatment and disappeared after its cessation, the second (T315I) occurred under dasatinib treatment. Patient n. 16 showed the D276G mutation under imatinib; this mutation was lost after switching to nilotinib therapy. Subsequently, the T315I mutation emerged which was retrospectively found to have been present in a small clone during the prior imatinib therapy. All patients were included in studies approved by the Heidelberg University Institutional Review Board and gave informed consent to participation in this study according to the Declaration of Helsinki.
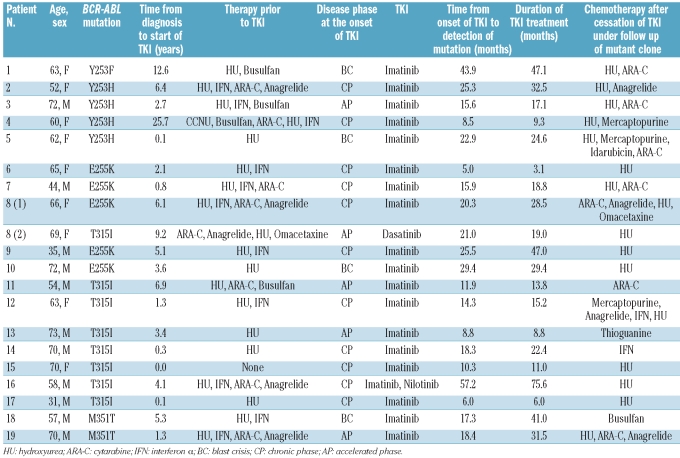
Table 1.
Patient and treatment characteristics.
Real-time quantitative polymerase chain reaction, direct sequencing
RNA was extracted from total peripheral blood leukocytes and reverse transcribed according to standard methods.24 Real-time quantitative polymerase chain reaction (PCR) was performed to determine the numbers of transcripts of BCR-ABL and the control genes ABL and β-glucuronidase (GUS).25,26 A 675 bp product encoding ABL amino acids 207 to 414 was generated using a heminested PCR to allow specific amplification of the translocated ABL alleles.3 Products were directly sequenced in both directions and compared with the wild-type ABL sequence (GenBank accession # U07563).
Quantification of the proportion of mutant BCR-ABL alleles
A mutation-specific nested PCR generated transcripts flanking the different mutation sites. The first step used the primers B2B (BCR exon 13) ACAGCATTCCGCTGACCATCAATAAG and A7- (ABL exon 7) AGACGTCGGACTTGATGGAGAACT spanning the BCR-ABL junction site, thus ensuring that the normal unrearranged ABL allele was not amplified and subjected to analysis. The second step comprised mutation-specific primers yielding products of different lengths. Mutation-specific restriction digestion was performed to quantify the proportion of mutant alleles. Mutations led to loss of RsaI (codon 253), MnlI (codon 255), DdeI (codon 315), and NcoI (codon 351) restriction sites. Gel electrophoresis on 1.8% ethidium bromide-stained agarose gels showed the proportion of mutant alleles by differential band intensity of the digested and the undigested transcripts. A correction factor was used to compensate for differences of band intensity due to different transcript lengths (Table 2, Figure 1). The linearity of the assay was demonstrated using dilutions of pCR®2.1-TOPO® plasmids (Invitrogen, Carlsbad, CA, USA) harboring mutations in unmutated pCR®2.1-TOPO® plasmids.3
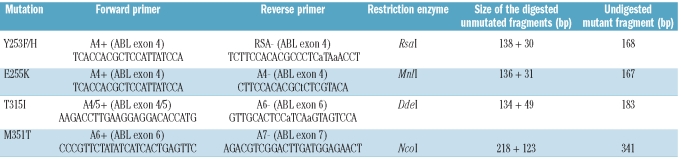
Table 2.
PCR primers and digestion products. Lower case letters indicate mismatches introduced to avoid further restriction sites.
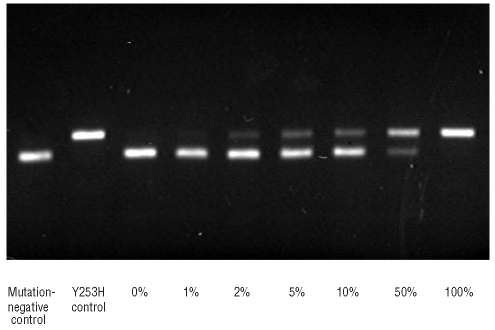
Figure 1.
Restriction digest assay for a dilution of Y253H mutant BCR-ABL in mutation-negative BCR-ABL (tracks 3–9). The lower band represents the long fragment after digestion of mutation-negative transcripts, the upper band the undigested, i.e. the mutant transcripts. Mutation-negative and mutant controls (tracks 1 and 2).
Results
Proportion of mutant BCR-ABL transcripts
The proportion of mutant BCR-ABL transcripts is given by the ratio of mutant BCR-ABL transcripts to total BCR-ABL transcripts (BCR-ABLmut/BCR-ABLtotal). Assuming a homogeneous transcriptional activity of mutated and unmutated BCR-ABL-positive cells, the proportion of mutant BCR-ABL transcripts reflects the proportion of mutant BCR-ABL-positive alleles and cells in total BCR-ABL-positive alleles and cells.
Overall, the median proportion of mutant transcripts was 97% (range, 38–100%) before cessation of TKI treatment and 8% after cessation of TKI treatment (range, 0–100%; P<0.0001) indicating a relative decline of 88% (range, 13–100%; Table 3). The median time to the nadir (lowest proportion) of mutant alleles after cessation of TKI treatment was 6 months (range, 1–26 months; Table 3).
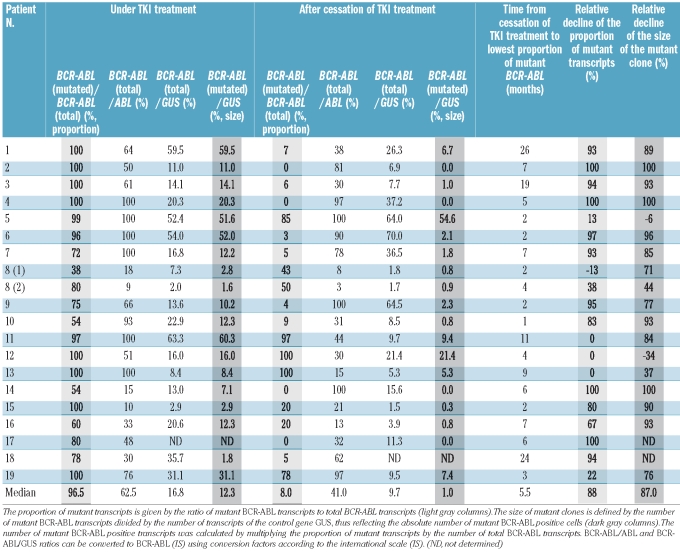
Table 3.
Proportion (light gray columns) and size (dark gray columns) of mutant clone before and after cessation of TKI treatment, time to lowest proportion for single patients.
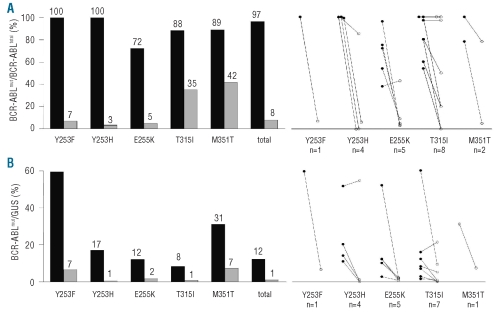
Mutations showed different patterns of deselection (Figure 2A). The P-loop mutations examined (Y253F/H and E255K) showed an almost complete regression of mutant transcripts under non-specific chemotherapy. In contrast, the median expression of mutant transcripts remained at higher levels for the T315I and M351T mutations. The patterns for T315I were heterogeneous: mutant transcripts declined under the level of threshold in two patients (patients # 14 and 17), whereas three other patients expressed 100% mutant BCR-ABL until the end of follow-up (patients n. 11–13). The median relative decline of the proportion of mutant BCR-ABL transcripts ranged from 52% to 97% for the different subgroups of mutations (Table 4).
Figure 2.
(A) Median proportion of mutant transcripts before (black columns) and after (gray columns) cessation of TKI treatment for different mutations (left). Proportions of mutant transcripts for single patients before (left dots) and after (right dots) cessation of TKI treatment (right). (B) Median size of mutant clones before (black columns) and after (gray columns) cessation of TKI treatment for different mutations (left). Sizes of mutant clones for single patients before (left dots) and after (right dots) cessation of TKI treatment (right).
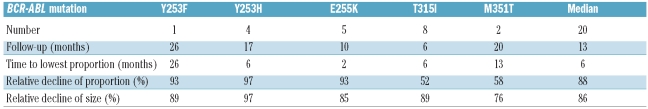
Table 4.
Median follow-up, time to lowest proportion of mutant transcripts, relative decline of the proportion of mutant transcripts, and relative decline of the size of mutant clones for the different subgroups of mutations. The relative decline of the proportion of mutant transcripts reflects the relative decline of the proportion of mutant BCR-ABL-positive cells in total BCR-ABL-positive cells. The relative decline of the size of mutant clones reflects the relative decline of the absolute number of mutant BCR-ABL-positive cells.
Size of mutant clones
While the proportion of mutant BCR-ABL-positive transcripts reflects the proportion of mutant BCR-ABL-positive cells in total BCR-ABL-positive cells, a measure of the absolute number of mutant BCR-ABL-positive cells is needed. To obtain an estimate of the absolute number of mutant BCR-ABL-positive cells, we introduced the size of a mutant clone as BCR-ABLmut/GUS=(BCR-ABLtotal/GUS)* proportion of mutant transcripts. Assuming a similar transcriptional activity of mutant and unmutated clones the size of a mutant clone gives an absolute quantification of the number of mutant BCR-ABL-positive cells.
The median size of mutant clones was 12% (range, 2–60%) before and 1.8% (range, 0–55%; P=0.0003) after cessation of TKI treatment, corresponding to a median relative decline of 86% (range, -34–100%, Table 3). GUS quantification was not available for two patients (one with a T315I mutation, the other with a M351T mutation).
With regards to the size of the mutant clones instead of the proportion of mutant transcripts, there was less difference in the median decline after treatment cessation among the different subgroups of mutations (Figure 2B). The median relative decline of the size of mutant BCR-ABL-positive clones ranged from 70% to 97% for the different subgroups of mutations (Table 4).
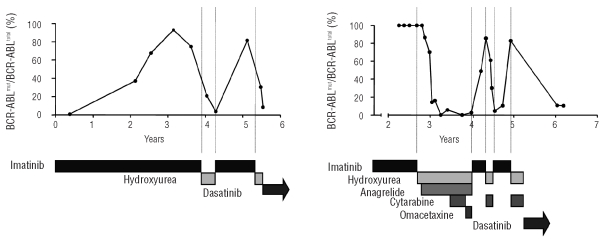
Two patients (patients # 2 and 9) showed a pattern of repeated selection and deselection of the mutant clone after resumption and second cessation of TKI treatment (Figure 3).
Figure 3.
Example of repeated selection and deselection. Patient # 9 (left, mutation E255K) and patient # 2 (right, mutation Y253H) received an alternating regimen with TKI treatment and chemotherapy. Dotted lines indicate onset and stop of TKI treatment. The mutant BCR-ABL-positive clones were outgrown by the expanding unmutated BCR-ABL-positive clone under chemotherapy. After resumption of TKI treatment clonal selection occurred. Patient # 2 showed deselection under dasatinib at the end of follow up.
Discussion
BCR-ABL mutations represent the major cause of resistance after TKI therapy.3,4 Here we describe the dynamics of mutant BCR-ABL transcripts for five common mutations in 20 cases of TKI cessation. The majority of patients showed a substantial decline of mutant BCR-ABL expression within months. This demonstrates that after stopping the selective pressure of the TKI the BCR-ABL mutation confers a proliferative disadvantage. The cases of repeated selection and deselection suggest that competing clones show a high susceptibility to the onset of TKI pressure as well as to its withdrawal. However, it has been demonstrated that clonal selection does not always occur.10,21 Indeed, in some patients we observed persistence of mutant clones. Additional factors might influence the impact of the proliferative advantage of either clone. In our series three patients harboring the T315I mutation expressed 100% mutant transcripts until the end of follow-up, whereas in two other patients this mutation disappeared completely. The deselection of a T315I mutant clone after cessation of imatinib had previously been shown in a single patient.14 A gain-of-function of the T315I mutant BCR-ABL tyrosine kinase, which might explain the persistence of the clone, has been discussed, remaining controversial.17,18 Compared to the P-loop mutations examined (Y253F/H, E255K) the median decline of the proportion of mutant transcripts was lower with the T315I and M351T mutations (Figure 2A). This difference disappeared with regard to the size of mutant clones (Figure 2B). Some patients showed a decline of the size of the mutant clone due to a declining BCR-ABL/GUS ratio while the proportion of mutant transcripts remained persistently high (patients # 11 and 13). Recently, it has been shown that the MAPK pathway is preferentially activated by imatinib in T315I mutated cells as compared to unmutated cells.27 These in vitro data suggest that TKI treatment confers the mutant cell clone with increased oncogenic fitness which is lost after cessation of treatment with the TKI. This might explain the decreasing BCR-ABL/GUS ratio after switching to chemotherapy besides the resumption of an effective therapy.
Data on non-specific salvage therapy are important for understanding the activity of second- and third-generation TKI.22,23 The reduction of mutant clones after TKI withdrawal might be due to non-specific effects or the activity of the new TKI administered.
These results are of particular importance for the activity of drugs addressing the T315I mutation.28–30 Since we observed the decline of T315I mutant transcripts to a level below the limit of detection of denaturing high performance liquid chromatography (patient n. 17) the ability of the mutant clone to regrow during treatment with another TKI remains open.
We conclude that the deselection of mutant BCR-ABL-positive clones within months after discontinuation of TKI treatment is a common and reproducible phenomenon. The decline of the proportion of mutant transcripts seems to be less frequent in patients harboring the T315I mutation than in patients with mutations of the P-loop region. However, there is hardly a difference in the regression of the calculated absolute amount of mutant transcripts. The high susceptibility of competing clones to changes in selective pressure emphasizes the need for early screening for BCR-ABL mutations in suboptimally responding patients. Discontinuation of TKI treatment might be an option for patients harboring the T315I mutation. The question of whether treatment discontinuation leads to an eradication of the mutant clone or a persistent mutant clone with the probable consequence of repeated clonal selection after resumption of TKI treatment is object of further investigations using highly sensitive methods.
Footnotes
Funding: the work was supported by the Deutsche José Carreras Leukämiestiftung (H03/01).
Authorship and Disclosures
The information provided by the authors about contributions from persons listed as authors and in acknowledgments is available with the full text of this paper at www.haematologica.org.
Financial and other disclosures provided by the authors using the ICMJE (www.icmje.org) Uniform Format for Disclosure of Competing Interests are also available at www.haematologica.org.
References
- 1.Baccarani M, Cortes J, Pane F, Niederwieser D, Saglio G, Apperley J, et al. Chronic myeloid leukemia: an update of concepts and management recommendations of European LeukemiaNet. J Clin Oncol. 2009;27(35):6041–51. doi: 10.1200/JCO.2009.25.0779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shah NP, Nicoll JM, Nagar B, Gorre ME, Paquette RL, Kuriyan J, et al. Multiple BCR-ABL kinase domain mutations confer polyclonal resistance to the tyrosine kinase inhibitor imatinib (STI571) in chronic phase and blast crisis chronic myeloid leukemia. Cancer Cell. 2002;2(2):117–25. doi: 10.1016/s1535-6108(02)00096-x. [DOI] [PubMed] [Google Scholar]
- 3.Hochhaus A, Kreil S, Corbin AS, La Rosée P, Muller MC, Lahaye T, et al. Molecular and chromosomal mechanisms of resistance to imatinib (STI571) therapy. Leukemia. 2002;16(11):2190–6. doi: 10.1038/sj.leu.2402741. [DOI] [PubMed] [Google Scholar]
- 4.Apperley JF. Part I: mechanisms of resistance to imatinib in chronic myeloid leukaemia. Lancet Oncol. 2007;8(11):1018–29. doi: 10.1016/S1470-2045(07)70342-X. [DOI] [PubMed] [Google Scholar]
- 5.O’Hare T, Eide CA, Deininger MW. Bcr-Abl kinase domain mutations, drug resistance, and the road to a cure for chronic myeloid leukemia. Blood. 2007;110(7):2242–9. doi: 10.1182/blood-2007-03-066936. [DOI] [PubMed] [Google Scholar]
- 6.Ernst T, Hoffmann J, Erben P, Hanfstein B, Leitner A, Hehlmann R, et al. ABL single nucleotide polymorphisms may masquerade as BCR-ABL mutations associated with resistance to tyrosine kinase inhibitors in patients with chronic myeloid leukemia. Haematologica. 2008;93(9):1389–93. doi: 10.3324/haematol.12964. [DOI] [PubMed] [Google Scholar]
- 7.Hochhaus A, Erben P, Ernst T, Mueller MC. Resistance to targeted therapy in chronic myelogenous leukemia. Semin Hematol. 2007;44(1 Suppl 1):S15–24. doi: 10.1053/j.seminhematol.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 8.Ernst T, Gruber FX, Pelz-Ackermann O, Maier J, Pfirrmann M, Muller MC, et al. A co-operative evaluation of different methods of detecting BCR-ABL kinase domain mutations in patients with chronic myeloid leukemia on second-line dasatinib or nilotinib therapy after failure of imatinib. Haematologica. 2009;94(9):1227–35. doi: 10.3324/haematol.2009.006981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roche-Lestienne C, Soenen-Cornu V, Grardel-Duflos N, Lai JL, Philippe N, Facon T, et al. Several types of mutations of the Abl gene can be found in chronic myeloid leukemia patients resistant to STI571, and they can pre-exist to the onset of treatment. Blood. 2002;100(3):1014–8. doi: 10.1182/blood.v100.3.1014. [DOI] [PubMed] [Google Scholar]
- 10.Willis SG, Lange T, Demehri S, Otto S, Crossman L, Niederwieser D, et al. High-sensitivity detection of BCR-ABL kinase domain mutations in imatinib-naive patients: correlation with clonal cytogenetic evolution but not response to therapy. Blood. 2005;106(6):2128–37. doi: 10.1182/blood-2005-03-1036. [DOI] [PubMed] [Google Scholar]
- 11.Komarova NL, Wodarz D. Drug resistance in cancer: principles of emergence and prevention. Proc Natl Acad Sci USA. 2005;102 (27):9714–9. doi: 10.1073/pnas.0501870102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ernst T, Erben P, Muller MC, Paschka P, Schenk T, Hoffmann J, et al. Dynamics of BCR-ABL mutated clones prior to hematologic or cytogenetic resistance to imatinib. Haematologica. 2008;93(2):186–92. doi: 10.3324/haematol.11993. [DOI] [PubMed] [Google Scholar]
- 13.Müller MC, Lahaye T, Hochhaus A. [Resistance to tumor specific therapy with imatinib by clonal selection of mutated cells] Dtsch Med Wochenschr. 2002;127 (42):2205–7. doi: 10.1055/s-2002-34939. [DOI] [PubMed] [Google Scholar]
- 14.Hayette S, Michallet M, Baille ML, Magaud JP, Nicolini FE. Assessment and follow-up of the proportion of T315I mutant BCR-ABL transcripts can guide appropriate therapeutic decision making in CML patients. Leuk Res. 2005;29(9):1073–7. doi: 10.1016/j.leukres.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 15.Gruber FX, Lamark T, Anonli A, Sovershaev MA, Olsen M, Gedde-Dahl T, et al. Selecting and deselecting imatinib-resistant clones: observations made by longitudinal, quantitative monitoring of mutated BCR-ABL. Leukemia. 2005;19(12):2159–65. doi: 10.1038/sj.leu.2403983. [DOI] [PubMed] [Google Scholar]
- 16.Gorre ME, Mohammed M, Ellwood K, Hsu N, Paquette R, Rao PN, et al. Clinical resistance to STI-571 cancer therapy caused by BCR-ABL gene mutation or amplification. Science. 2001;293(5531):876–80. doi: 10.1126/science.1062538. [DOI] [PubMed] [Google Scholar]
- 17.Yamamoto M, Kurosu T, Kakihana K, Mizuchi D, Miura O. The two major imatinib resistance mutations E255K and T315I enhance the activity of BCR/ABL fusion kinase. Biochem Biophys Res Commun. 2004;319(4):1272–5. doi: 10.1016/j.bbrc.2004.05.113. [DOI] [PubMed] [Google Scholar]
- 18.Miething C, Feihl S, Mugler C, Grundler R, von Bubnoff N, Lordick F, et al. The Bcr-Abl mutations T315I and Y253H do not confer a growth advantage in the absence of imatinib. Leukemia. 2006;20(4):650–7. doi: 10.1038/sj.leu.2404151. [DOI] [PubMed] [Google Scholar]
- 19.Griswold IJ, MacPartlin M, Bumm T, Goss VL, O’Hare T, Lee KA, et al. Kinase domain mutants of Bcr-Abl exhibit altered transformation potency, kinase activity, and substrate utilization, irrespective of sensitivity to imatinib. Mol Cell Biol. 2006;26(16):6082–93. doi: 10.1128/MCB.02202-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lange T, Park B, Willis SG, Deininger MW. BCR-ABL kinase domain mutations in chronic myeloid leukemia: not quite enough to cause resistance to imatinib therapy? Cell Cycle. 2005;4(12):1761–6. doi: 10.4161/cc.4.12.2261. [DOI] [PubMed] [Google Scholar]
- 21.Khorashad JS, Anand M, Marin D, Saunders S, Al-Jabary T, Iqbal A, et al. The presence of a BCR-ABL mutant allele in CML does not always explain clinical resistance to imatinib. Leukemia. 2006;20 (4):658–63. doi: 10.1038/sj.leu.2404137. [DOI] [PubMed] [Google Scholar]
- 22.Muller MC, Cortes JE, Kim DW, Druker BJ, Erben P, Pasquini R, et al. Dasatinib treatment of chronic-phase chronic myeloid leukemia: analysis of responses according to preexisting BCR-ABL mutations. Blood. 2009;114(24):4944–53. doi: 10.1182/blood-2009-04-214221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hughes T, Saglio G, Branford S, Soverini S, Kim DW, Muller MC, et al. Impact of base-line BCR-ABL mutations on response to nilotinib in patients with chronic myeloid leukemia in chronic phase. J Clin Oncol. 2009;27(25):4204–10. doi: 10.1200/JCO.2009.21.8230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muller MC, Gattermann N, Lahaye T, Deininger MW, Berndt A, Fruehauf S, et al. Dynamics of BCR-ABL mRNA expression in first-line therapy of chronic myelogenous leukemia patients with imatinib or interferon alpha/ara-C. Leukemia. 2003;17 (12):2392–400. doi: 10.1038/sj.leu.2403157. [DOI] [PubMed] [Google Scholar]
- 25.Emig M, Saussele S, Wittor H, Weisser A, Reiter A, Willer A, et al. Accurate and rapid analysis of residual disease in patients with CML using specific fluorescent hybridization probes for real time quantitative RT-PCR. Leukemia. 1999;13(11):1825–32. doi: 10.1038/sj.leu.2401566. [DOI] [PubMed] [Google Scholar]
- 26.Müller MC, Erben P, Saglio G, Gottardi E, Nyvold CG, Schenk T, et al. Harmonization of BCR-ABL mRNA quantification using a uniform multifunctional control plasmid in 37 international laboratories. Leukemia. 2008;22(1):96–102. doi: 10.1038/sj.leu.2404983. [DOI] [PubMed] [Google Scholar]
- 27.Härtel N, Klag T, Hochhaus A, La Rosée P. Overexpression of the IL3/IL5/GM-CSFRB as potential mechanism leading to survival factor activation in response to ABLinhibitor treatment. Haematologica. 2008;93(Suppl 1):382. [Google Scholar]
- 28.Cortes-Franco J, Khoury HJ, Nicolini FE, Corm S, Lipton JH, Jones D, et al. Safety and efficacy of subcutaneous-administered omacetaxine mepesuccinate in imatinib-resistant chronic myeloid leukemia (CML) patients who harbor the Bcr- Abl T315I mutation-results of an ongoing multicenter phase 2/3 Study. Blood. ASH Annual Meeting Abstracts. 2009;114(22):644. [Google Scholar]
- 29.Cortes-Franco J, Raghunadharao D, Parikh P, Wetzler M, Lipton JH, Jones D, et al. Safety and efficacy of subcutaneous-administered omacetaxine mepesuccinate in chronic myeloid leukemia (CML) patients who are resistant or intolerant to two or more tyrosine kinase inhibitors -results of a multicenter phase 2/3 study. Blood. ASH Annual Meeting Abstracts. 2009;114 (22):861. [Google Scholar]
- 30.O’Hare T, Shakespeare WC, Zhu X, Eide CA, Rivera VM, Wang F, et al. AP24534, a pan-BCR-ABL inhibitor for chronic myeloid leukemia, potently inhibits the T315I mutant and overcomes mutation-based resistance. Cancer Cell. 2009;16(5):401–12. doi: 10.1016/j.ccr.2009.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]