Abstract
Traditional orthodontic treatments do not adequately address the skeletal problems of retrognathic, hyperdivergent, Class II adolescents; the few approaches that do require long-term patient compliance. This paper introduces a novel approach using miniscrew implants (MSIa) and growth to treat retrognathic hyperdivergent adolescents. Nine consecutive patients were evaluated at the start of treatment (13.2 ±1.1 years of age) and again at the end of the orthopedic phase (after 1.9 ±0.3 years). Each patient had two MSIs placed in either side of the palate. Coil springs (150 g) extended from the MSIs to a RPE, which served as a rigid segment for intruding the maxillary premolar and molars. Two additional MSIs were placed between the first mandibular molars and second premolars; coil spring (150 g) extended from the MSIs to hold or intrude the mandibular molars. Prior to treatment, the patients exhibited substantial and significant mandibular retrusion (Z-score=−1.0), facial convexity (Z-score=0.7), and hyperdivergence (Z-score=1.6). Treatment produced consistent and substantial orthopedic effects. The chin was advanced an average of 2.4 mm, the SNB angle increased by 2.1°, the mandibular plane angle decreased 3.9°, and facial convexity decreased by approximately 3.2°. Questionnaires showed that this treatment approach was not painful or uncomfortable; the majority of the patients indicated that they were very likely to recommend the treatment to others. Treatment was accomplished by titrating the amount of orthodontic intrusion performed based on the individuals’ growth potential.
Introduction
Growing individuals with Class II malocclusions comprise a large segment of the population requiring orthodontic treatment for both esthetic and functional reasons. Approximately 15% of untreated adolescents in the United States have Class II malocclusion.1,2 Treatment is necessary to correct the malocclusion and to straighten the profile, which tends to be convex. Among Caucasian, convex profiles are among the least favored, while straighter profiles with prominent chins are the most favored.3 Changing retrusive profiles to straighter, less retruded profiles, significantly increases attractiveness. 4 Individuals with Class II malocclusion also have functional deficits and impaired masticatory function,5,6 which have been directly related to their malocclusion.7
Class II patients often have retrognathic mandibles and hyperdivergent growth tendencies, which make them among the most difficult to treat orthodontically. The skeletal problems associated with Class II’s are primarily mandibular; the mandible becomes retrusive and hyperdivergent throughout childhood and adolesence.8,9 Importantly, Class II patients with hyperdivergent tendencies have additional morphological characteristics, the correction of which make treatment more difficult, including excessive anterior and posterior dentoalveolar heights, open bites, increased lower face heights, steeper mandibular planes and larger gonial angles.10–19
To address the myriad of problems associated with hyperdivergent Class II patients, forward mandibular rotation must be incorporated into any treatment plan attempting to address the skeletal dysmorphology. Björk and Skieller’s landmark studies were among the first to show that true forward rotation (as defined by Solow and Houston20) is associated with greater chin projection, reductions in the gonial angle, redirection of condylar growth and control of vertical eruption.21–22 True mandibular rotation has repeatably been shown to be the most important determinant of the anteroposterior position of the chin in untreated23 and treated subjects.24,25
Current orthodontic treatment approaches for growing hyperdivergent Class II’s do not control rotation and therefore, cannot adequately address the skeletal dysmorphology. Because vertical control is especially difficult for hypdivergent patients,18 established treatment mechanics often impede improvements of the profile.26–29 The most common orthodontic treatment approaches for hyperdivergent Class II’s produce mainly dental corrections. LaHaye et al.25 recently showed that the three most common treatment approaches for such patients (head-gear with extractions, head-gear without extractions, and the Herbst appliance) corrected the Class II malocclusions, but not consistently improve the chin projection or hyperdivergent tendencies. The literature clearly shows that traditional treatment approaches to Class II hyperdivergent patients have little or no effect on the mandible (Table 1).
Table 1.
Changes (deg) of SNA, SNB, and MPA for traditional headgear non-extraction and extraction treatments
| Non-extraction Treatments | Extraction Treatment | |||||
|---|---|---|---|---|---|---|
| Reference | SNA | SNB | MPA | SNA | SNB | MPA |
| LaHaye et al25 | −2.0 | 0.4 | 0.6 | −3.7 | 0.6 | 0.6 |
| Haralabakis et30 | −1.5 | 0.7 | −0.4 | - | - | - |
| Gandini et al31 | −2.1 | 0.8 | −0.3 | - | - | - |
| Bishara32 | −0.6 | 0.8 | −1.4 | - | - | - |
| Hubbard et al33 | −2.1 | −0.4 | 0.1 | - | - | - |
| Luppanapornlarp & Johnson34 | −1.4 | −0.3 | 0.7 | −1.8 | −0.1 | −0.2 |
| Paquette et al35 | −1.5 | 0.2 | −2.0 | −2.3 | −1.8 | 0.3 |
| Congiolosi et al36 | −1.1 | 0.5 | −0.3 | |||
| Brown37 (HPHG) | −0.7 | −0.2 | 0.9 | −0.1 | 0.5 | −0.3 |
| Brown37 (CPHG) | −0.9 | 0.1 | 0.8 | −1.2 | −0.1 | 0.7 |
| Taner-Sarisoy et al38 | - | - | - | −1.2 | −0.3 | 0.1 |
| Bishara et al39 | - | - | - | −2.3 | −0.2 | −1.4 |
| Average | −1.4 | 0.3 | −0.1 | −1.8 | −0.2 | −0.1 |
In contrast, vertical pull chin cup appliances are effective in producing true anterior mandibular rotation and decreasing the anterior facial height.44–42 For example, young patients treated with anterior-pull chin-cup therapy show twice as much forward movement of the chin, and almost three times as much true mandibular forward rotation, than matched controls.42 Such findings support the notion that rotation is the key mechanism in treating hyperdivergent Class II’s. However, vertical pull chin cup depends heavily on patient compliance, which makes treatment results unpredictable.
Currently, surgery is the most effective approach for treating moderate-to -severely hyperdivergent Class II patients. While case studies have shown more spectacular results, the existing cohort studies evaluating maxillary impaction have shown clinically significant increases of the SNB angle(0.4–2.6°),43–45 decreases in the mandibular plane angle (3.4–3.5°),43,45 and decreases in gonial angulation (0.2–1.6°), 43,45 all of which address the underlying skeletal problems. However, LeFort surgical procedures are substantially more expensive than orthodontics alone and can only be performed on non-growing individuals.
With the incorporation of fixed anchorage devices, patient compliance has been almost eliminated and force magnitudes can be better controlled.46 Of all the fixed anchorage devices, miniscrew implants (MSIs) are the least invasive, most conservative in terms of placement and removal, the most flexible with respect to implantation site, and the least expensive. MSIs are also esthetically more acceptable than extraoral appliances and they are especially well suited for non-compliant patients.
While miniscrew implants have been used for various orthodontic treatments, there is only limited information available on their use as anchorage for intrusive mechanics in growing patients The existing studies, which pertain to adults (Table 2), have shown 1.7–3.3° decreases in the mandibular plane angle, 1.6–3.7 mm decreases in lower face height, 1.8–3.4 mm and 0.1–1.3 mm of upper and lower molar intrusion, respectively, and 1.5–1.8° decreases in the SNB angle.47–50 However, these findings provide no guidelines for growing adolescents, who comprise most of the orthodontic cases being treated, and who might be expected to respond differently to treatment than adults.
Table 2.
Summary statistics for hyperdivergent adults treatment with intrusion of teeth with miniscrew implants
| N | MPA (°) | SNB (°) | U6PP (mm) | L6MP (mm) | Gonial Angle (°) | ANS-Me (mm) | |
|---|---|---|---|---|---|---|---|
| Erverdi et al47 | 10 | −1.7 | +1.8 | −2.6 | −0.1 (NS) | ------ | ------ |
| Kuroda et al48 | 10 | −3.3 | +1.5 | −2.3 | −1.3 | −0.3 (NS) | ------ |
| Xun et al49 | 12 | −2.3 | +1.6 | −1.8 | −1.2 | −1.0 (NS) | −1.6 |
| Akay et al50 | 10 | −3.0 | +1.6 | −3.4 | ------ | ------ | −3.7 |
NS=no statistically significant change
The fact that miniscrew implants make it possible for orthodontists to apply forces more effectively is important because it allows the application of light forces produce intrusion, thereby reducing the potential of root resorption. Our experimental and histological studies have shown that light forces and miniscrews can be used to intrude multiple multiradicular teeth (segmental intrusion) without significant root resorption.51–53
The foregoing, prospective, feasibility study was designed to evaluate the skeletal and dental effects of intruding segments of teeth in a controlled fashion using miniscrew implants. By intruding maxillary and mandibular teeth in a controlled fashion, we expected to produce mandibular forward rotation and remodeling changes that address both the skeletal and dental problems associated with growing Class II hyperdivergent patients.
Study Design
The sample consists of nine consecutive patients (8 ♀ and 1 ♂) recruited during screenings held at the Graduate Orthodontic Clinic of Baylor College of Dentistry. The patients met the following selection criteria:
Inclusion Criteria
Early permanent dentition (premolars and permanent canines emerged)
Lower anterior facial height greater than age and sex specific mean values (based on reference data reported by Riolo et al.54)
Retrognathic mandible with the SNB angle being 1 SD or more below age and sex specific values (based on reference data reported by Riolo et al.54)
End-on or greater bilateral Class II canine and/or molar relationships
Exclusion Criteria
Inability to attain acceptable hygiene levels before starting orthodontic treatment.
Second molars fully erupted into occlusion (the mesial marginal ridge of all second molars should be at least 2 mm apical to the distal marginal ridge of the first molar).
IRB approval was obtained and all of the subjects have been recruited into the study. The overall study included 20 patients; the present preliminary report pertains to the nine patients for whom complete pre- and post-treatment records have been obtained.
The appliances used for skeletal anchorage were IMTEC (IMTEC Corporation; Ardmore, OK) miniscrew implants (1.8 × 8 mm). Sentalloy® coil springs (GAC international, Bohemia, NY) were used to intrude and hold the posterior teeth; each spring was calibrated using a gram force gauge (Correx, Haag-Streit, Switzerland) to deliver a constant force of approximately 150 g. A rapid palatal expander (RPE) (Variety SP, Dentaurum, Germany) was used to hold the premolars and molars as a rigid segment during intrusion. Fixed orthodontic appliances (0.018 Slot, SPEED Industries, Canada) were used to complete the orthodontic phase of treatment.
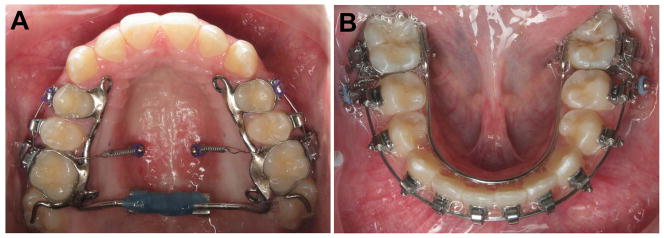
After approximately two months of treatment and retention, the RPE was sealed, and the two maxillary MSI’s were placed in the parasagital region of the palate mesial to the first molars. Vertically, the MSIs were placed where the palatal roof and lingual walls meet (Figure 1A). The patients rinsed with clorhexidine (Peridex, Zila Pharmaceuticals, Inc, Fort Collins, CO ) for 30 seconds immediately before MSI insertion, and 2 or 3 times per day for the next 3–5 days. Each patient was previously anesthetized using topical anesthesia followed by local infiltration of ¼ cartidrge of lidocaine with epinephrine. A periodontal probe was used to puncture the palatal tissues in the parasaggital region mesial to the maxillary first molar. Once firm contact with the cortical bone had been made, the tissue thickness at the implantation site was assessed. Using a manual contraangle, each miniscrew (1.8 mm × 8 mm) was inserted perpendicular to the cortical bone following the palate’s anatomy. They were inserted without a pilot hole or a tissue punch. Both MSI’s were immediately loaded with an intrusive force of 150 g using calibrated Sentalloy® coils that extended directly to the RPE frame between the first molar and second premolar, following the protocol previously described.55
Figure 1.
A) Maxillary and B) mandibular appliances used for the mini-screw implant treatment.
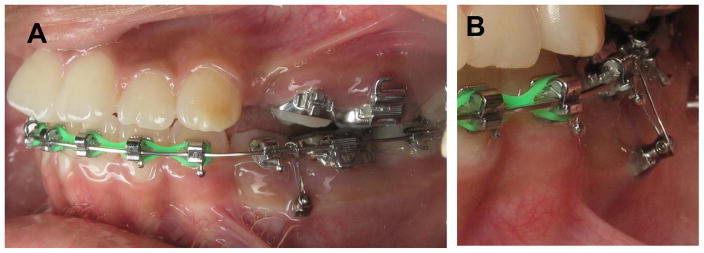
The sites for the mandibular MSIs were prepared by bonding brackets to diverge the roots between the first molars and second premolars. The objective was to widen the site for MSI insertion using a 0.016×0.022 stainless steel wire. After approximately one month, a periapical radiograph was taken to evaluate the increase of interradicular space attained. If the space was determined to be sufficient for implant placement, the patient was scheduled for MSI insertion; if not, adjustments were made to further widen the implant site. The lower MSIs were placed following the same clorhexidine rinse protocol used for the maxillary MSIs. The mandibular MSIs were also placed without pilot holes and tissue punch. A double insertion technique was used in order to insert the MSIs at an angle, with the head of the screw positioned at the level of the mucogingival junction (Figure 2). The lower MSIs were loaded immediately using calibrated 150g coils, following the same protocol as in the maxilla. The lower molars bands were prepared for insertion of a removable lower lingual arch, if needed to control molar torque. Lingual arches were only installed in a few of the cases, especially those who mandibular teeth were actively intruded.
Figure 2.
A) Buccal view location of mandibular MSIs, B) frontal view showing insertion angle.
To prevent their extrusion while intruding the posterior teeth, the upper anterior teeth (canine to canine) were not initially bonded with fixed appliances. They were bonded once the upper anterior teeth made contact with the lower teeth, which prevented them from interfering with mandibular autorotation.
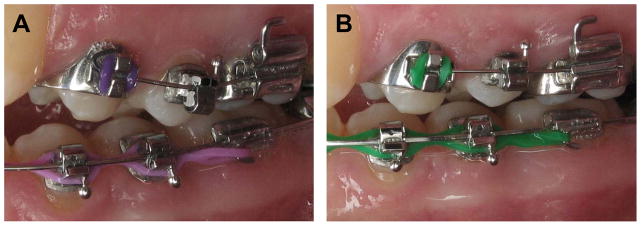
Periodontal health was closely monitored during intrusion. The need for the patients to maintain proper hygiene was emphasized throughout treatment. Importantly, there was a temporary shortening of the clinical crowns of the teeth that had been intruded (Figure 3); there was also some tissue bulging, especially on the palate. This was deemed to be temporary gingival overgrowth that disappeared in all cases after intrusion had been stopped and the teeth had been held in place for 2–3 months.
Figure 3.
Maxillary first molar clinical crown height A) before and B) during active orthodontic intrusion
After the required amount of posterior intrusion had been attained, or when the maxillary anterior and posterior occlusal planes had been leveled, the RPE was removed and fixed orthodontic appliances were bonded onto all of the maxillary posterior teeth. After the RPE was removed, a transpalatal arch (TPA) was fitted to the maxillary first molars to hold the transverse dimension and prevent any unwanted torque of the posterior teeth. The maxillary and mandibular MSI’s remained in place until full treatment was completed. They held the vertical dimension of the posterior teeth using an 0.010 in stainless steel ligature tied to the palatal sheath in the maxilla and to the archwire mesial to the first molar band in the mandible.
Treatment Results and Discussion
The subjects were 13.2 ±1.1 years old at the start of treatment. The orthopedic phase of treatment lasted for an average of 1.9 ±0.3 years; the shortest and longest treatment durations were 1.4 and 2.5 years, respectively. Longer treatment time were required for patients who had impacted canines (N=2) and extractions (N=2).
Of the 54 MSI that have been placed so far, only two have failed (Table 3), with one failure in each jaw. A failure was defined as an MSI that was unable to hold the force of the coil spring or steel ligature without noticeable mobility of its head. This resulted in an success rate of 96.3%, which is considerable higher than previously reported for miniscrew implants, and more closely approximates the success rates of endosseous implants.
Table 3.
Numbers of implants placed, the number that failed, and the relative stability of the miniscrew implants used in the present study
| # Placed | # Failed | % Stability | |
|---|---|---|---|
| Maxilla | 32 | 1 | 96.9% |
| Mandible | 22 | 1 | 95.4% |
| Total | 54 | 2 | 96.3% |
Prior to treatment, patients presented with greater mandibular retrusion (SNB= 73.8°; Z-score= −1.0), greater facial convexity (N-A-Pg = 9.2°; Z-score= 0.7) and substantially more hyperdivergence (MPA=43.3°; Z-score=1.6) than exhibited by untreated controls. They also had substantially larger gonial angles (Ar-Go-Me=134°; Z-score= 1.4) than controls.54
The treatments produced consistent and substantial effects, which were statistically significant despite the small size of the sample (Table 4). The chin moved forward an average of 2.4 mm; the maximum anterior movement of the chin was 7.1 mm. The SNB angles increased by 2.1 ±1.3°and the mandibular plane angle decreased an average of 3.9 ±1.8°. Hard- and soft tissue facial convexities decreased by approximately 3.2°, and the gonial angle decreased by 2.4 ±1.8°.
Table 4.
Orthopedic changes of nine consecutive Class II hyperdivergent adolescents treated with miniscrew implants
| Units | Minimum | Mean | Standard Deviation | Maximum | Probability of Changes | |
|---|---|---|---|---|---|---|
| Pg_hor | mm | −0.7 | 2.4 | 2.3 | 7.1 | .020 |
| SNB | deg | −0.1 | 2.1 | 1.3 | 4.2 | .002 |
| MPA | deg | −1.0 | −3.9 | 1.8 | −6.5 | .001 |
| HT Convexity | deg | 1.3 | −3.2 | 2.4 | −6.1 | .007 |
| ST Convexity | deg | −0.9 | 3.15 | 2.9 | 8.7 | .017 |
| Gonial Angle | deg | 0.8 | −2.4 | 1.8 | −5.3 | .018 |
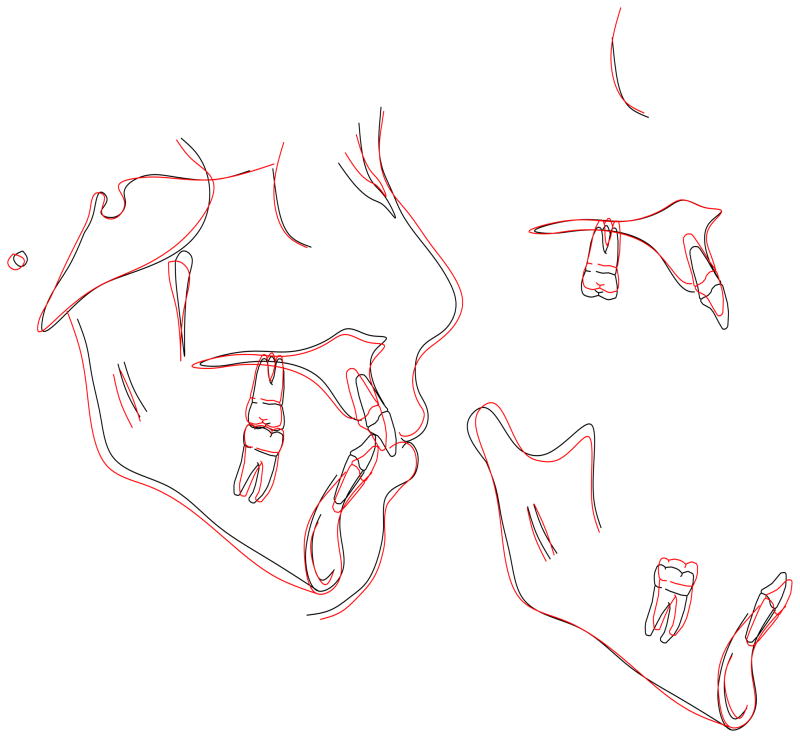
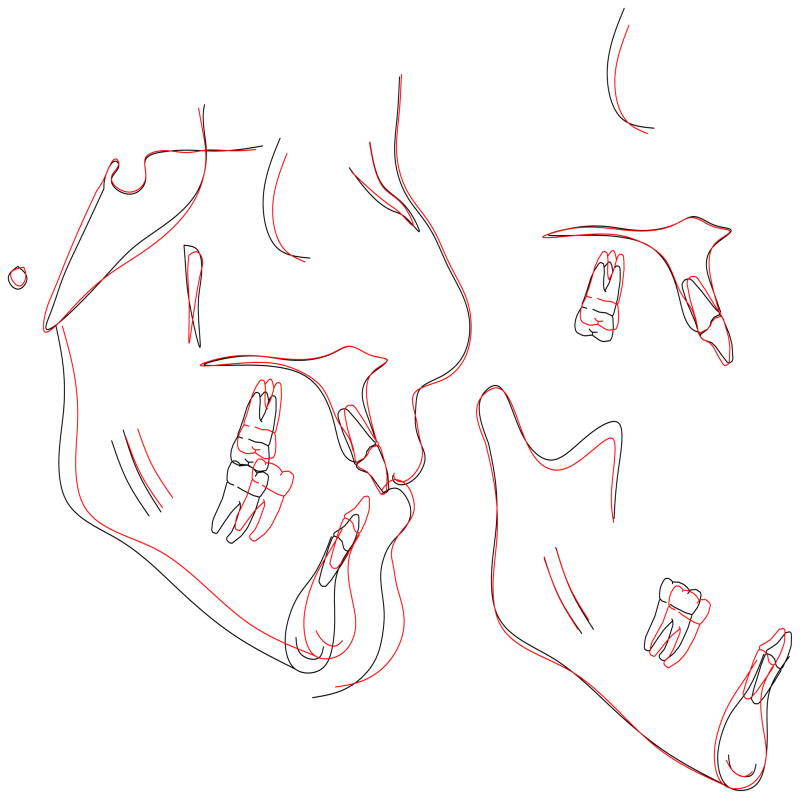
Cranial base superimpositions showed positive orthopedic treatment results for all but one of the females, who was 12.2 years of age at the start of her non-extraction treatment (Figure 4A). She showed only limited amounts of growth, and her lower molars erupted by approximately the same amount that the upper molars were intruded, which explains why she did not display the forward rotation and chin projection that was planned for. Approximately half of the remaining subjects exhibited forward rotation and anterior chin projection with little or no growth. The positive treatment effects that they exhibited were due primarily to intrusion of the upper molars and either relative intrusion (i.e. holding the vertical dimension) (Figure 4B) or actual intrusion (Figure 4C) of the lower molars. The remaining subjects showed positive treatment effects due to good growth, intrusion of the upper molar, and intrusion or relative intrusion of the lower molars. For example, a 13 year-old female treated for 1.7 years with extractions showed a substantial decrease in her mandibular plane angle and over 5 mm of chin projection (Figure 4D). Due to her good growth potential, she actually needed less intrusion of her upper molars and only relative intrusion of the lower molars.
Figure 4.
Figure 4A. Changes between 12.2–13.5 years of age for a female patient (#1) treated nonextraction.
Figure 4B. Changes between 13.7–15.8 years of age for a female patient (#3) treated with extractions.
Figure 4C. Changes between 14.2–15.9 years of age for a female patient (#4) treated with extractions.
Figure 4D. Changes between 13.0–14.7 fora female patient (#4) treated with extractions.
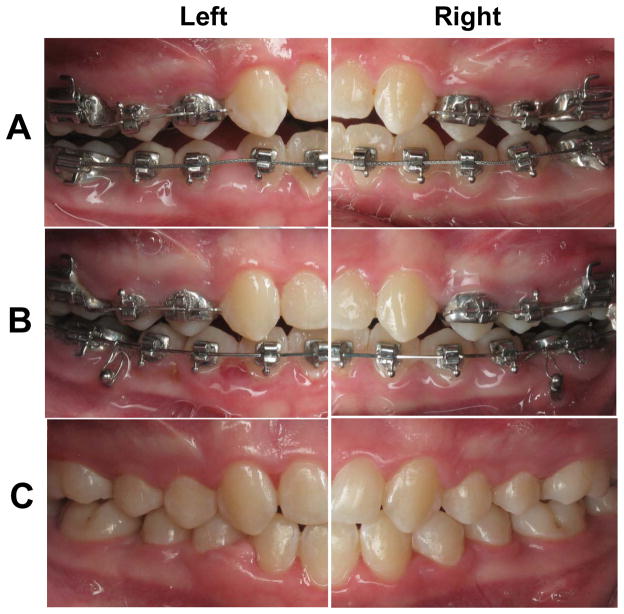
Orthodontist need to closely and continuously monitor these cases to determine if they are exhibiting the desired treatment changes. This is done clinically by evaluating changes in interarch dental and overbite/overjet relationships. If growth or intrusion are occurring, the case should exhibit a shift of the molar and premolar relationships from Class II to Class I (Figure 5). If such a shift is not evident within 4–6 months, then the orthodontist should plan on greater amounts of intrusion of the upper, and perhaps, even intrusion of the lower molars. In actively growing individuals, it is usually sufficient to intrude the upper posterior teeth and hold the lower posterior teeth in place so as to prevent them from erupting.
Figure 5.
Clinically assessment of treatment effects A) on the day of RPE cementation, B) after 5 months of active intrusion (2 months with maxillary MSI and 5 months of mandibular MSIs), C) at debond. Note deepening of the bite and Class II correction associated with autorotation of the mandible.
Subjective Self-Assessments
When the patients were initially asked about each of the appliances that were to be used, they substantially overestimated the amounts of pain that they expected to have with each appliance (Table 5). Approximately 36% 45% and 50% of the patients expected braces, expanders, and MSIs, respectively, to be be moderately or very painful. At the end of treatment, none of the patients reported that MSIs were either moderately or very painful; about 8% reported that braces were moderately painful and 17% felt that the expanders were moderately or very painful.
Table 5.
Pretreatment (PreTx) and post-treatment (PostTx) percentages of subjects reporting pain and discomfort associated with braces, expanders, and miniscrew implants, along with post-treatment percentages of how much they would recommend their treatment to friends and family
| How painful are the appliances? | ||||||||
|---|---|---|---|---|---|---|---|---|
| Not at all | Somewhat | Moderately | Very | |||||
| PreTx | PostTx | PreTx | PostTx | PreTx | PostTx | PreTx | PostTx | |
| Braces | 22.7 | 58.3 | 40.9 | 33.3 | 22.7 | 8.3 | 13.6 | 0 |
| Expander | 27.3 | 41.7 | 27.3 | 41.7 | 31.8 | 8.3 | 13.6 | 8.3 |
| MSIs | 9.1 | 91.7 | 40.9 | 8.3 | 13.6 | 0 | 36.4 | 0 |
| How uncomfortable are the appliances? | ||||||||
| Not at all | Somewhat | Moderately | Very | |||||
| Braces | 4.5 | 8.3 | 36.4 | 83.3 | 27.3 | 8.3 | 13.6 | 0 |
| Expander | 22.7 | 16.7 | 22.7 | 50.0 | 27.3 | 25.0 | 27.3 | 8.3 |
| MSIs | 4.5 | 66.7 | 36.4 | 25.0 | 27.3 | 8.3 | 31.8 | 0 |
| How much would you recommend your treatment to your friends and family? | ||||||||
| Not at all | Somewhat | Moderately | Very Much | Extremely | ||||
| 0 | 16.7 | 25.0 | 16.7 | 41.7 | ||||
The patients also initially overestimated the amounts of discomfort that they associated with each of the appliances, especially for the MSIs and expanders. Approximately 59% of the patients thought that the MSIs would be moderately or very uncomfortable; 55% thought that the expanders would be moderately or very uncomfortable, and; 41% felt that the braces would be moderately or very uncomfortable. After treatment, only 8% of the patients thought that the MSIs and braces were uncomfortable; none reported them to be very uncomfortable. Approximately 25% and 8% thought that the expanders were moderately and very uncomfortable, respectively.
Perhaps most important, the majority of the patients indicated that they would recommend the treatment that they had received to their friends and relatives. Approximately 17% said they would recommend the treatment “very much” and 42% said that they would recommend it “extremely much”. No-one said that they would not recommend the treatment.
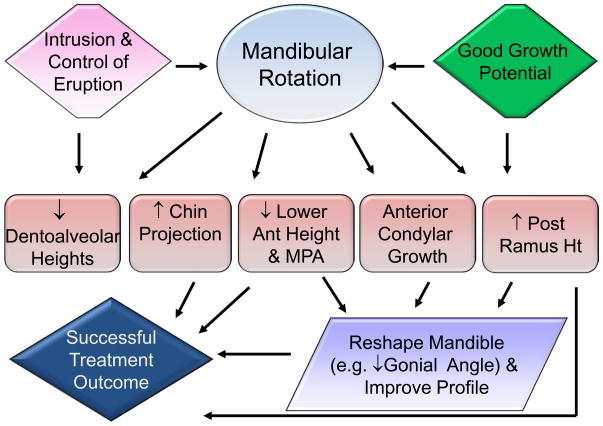
Conclusions
These preliminary results indicate that our novel approach is effective for addressing the primary skeletal treatment objectives of growing hyperdivergent, retrognathic, patients (Figure 6). Major orthopedic changes were produced, including substantial advancement of the chin and autorotation of the mandible, along with decreases in the gonial angle, all of which combined to reshape the mandible and improve facial profile. The treatment was accomplished by titrating the amount of orthodontic intrusion performed based on the individuals’ growth potential. This treatment approach was not painful or uncomfortable; the majority of the patients indicated that they were very likely to recommend the treatment to others.
Figure 6.
Treatment and growth related mandibular rotation, producing orthopedic effects that reshape the mandible and improve facial profile
Acknowledgments
This research was funded by NIDCR RFA-DE-06-007. We express our thanks to the Drs. Robert Gallagher, Monte Collins, J. Moody Alexander, and C. Moody Alexander for donated their cases, particularly to Dr. Phillip Campbell for helping to complete the sample.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Peter H. Buschang, Department of Orthodontics, Baylor College of Dentistry, Texas A&M University Health Science Center, Dallas, Texas.
Roberto Carrillo, Department of Orthodontics, Baylor College of Dentistry, Texas A&M University Health Science Center, Dallas, Texas.
P. Emile Rossouw, Department of Orthodontics, University of North Carolina, Chapel Hill, NC.
References
- 1.Kelly JE, Harvey CR. DHEW Publication No. (HRA) 77–1644. National Center for Health Statistics; Rockville, Md: 1977. An assessment of the occlusion of the teeth of youths 12–17 years; pp. 1–65. [PubMed] [Google Scholar]
- 2.Proffit WR. The Orthodontic Problem. In: Contemporary Orthodontics. 3. Mosby; 2000. pp. 9–13. [Google Scholar]
- 3.Czarnecki ST, Nanda RS, Currier GF. Perceptions of a balanced facial profile. Am J Orthod Dentofac Orthop. 1993;104:180–7. doi: 10.1016/S0889-5406(05)81008-X. [DOI] [PubMed] [Google Scholar]
- 4.Spyropoulos MN, Halazonetis DJ. Significance of the soft tissue profile on facial esthetics. Am J Orthod Dentofac Orthop. 2001;119:464–71. doi: 10.1067/mod.2001.113656. [DOI] [PubMed] [Google Scholar]
- 5.English JD, Buschang PH, Throckmorton GS. Does malocclusion affect masticatory performance? Angle Orthod. 2002;72:21–7. doi: 10.1043/0003-3219(2002)072<0021:DMAMP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Toro A, Buschang PH, Throckmorton GS, Roldan SR. Masticatory performance in children and adolescents with malocclusions. Eur J Orthod. 2006;28:112–9. doi: 10.1093/ejo/cji080. [DOI] [PubMed] [Google Scholar]
- 7.Owens S, Buschang PH, Throckmorton GS, Palmer L, English JD. Masticatory performance and areas of occlusal contact and near contact in subjects with normal occlusion and malocclusion. Am J Orthod Dentofac Orthop. 2002;121:602–9. doi: 10.1067/mod.2002.122829. [DOI] [PubMed] [Google Scholar]
- 8.McNamara JA. Components of Class II malocclusion in children 8–10 years of age. Angle Orthod. 1981;51:177–85. doi: 10.1043/0003-3219(1981)051<0177:COCIMI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Buschang PH, Martins J. Childhood and adolescent changes of skeletal relationships. Angle Orthod. 1998;68:199–208. doi: 10.1043/0003-3219(1998)068<0199:CAACOS>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Fields H, Proffit W, Nixon W. Facial pattern differences in long-faced children and adults. Am J Orthod. 1984;85:217–23. doi: 10.1016/0002-9416(84)90061-7. [DOI] [PubMed] [Google Scholar]
- 11.Janson GR, Metaxas A, Woodside DG. Variation in maxillary and mandibular molar ans incisor vertical dimension in 12 year old subjects with excess, normal, and short lower anterior facial height. Am J Orthod. 1994;106:409–18. doi: 10.1016/S0889-5406(94)70063-X. [DOI] [PubMed] [Google Scholar]
- 12.Subtenly JD, Sakuda M. Open-bite: Diagnosis and treatment. J Dent Child. 1993;60:392–8. [Google Scholar]
- 13.Isaacson JR, Isaacson RJ, Speidel TM. Extreme variation in vertical facial growth and associated variation in skeletal and dental relations. Angle Orthod. 1971;41:219–29. doi: 10.1043/0003-3219(1971)041<0219:EVIVFG>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Haralabakis NB, Yiagtzis SC, Toutountzakis NM. Cephalometric characteristics of open bite in adults: A three dimensional Cephalometric evaluation. Int J Adult Orthod Orthognath Surg. 1994;9:223–31. [PubMed] [Google Scholar]
- 15.Lopez-Gavito G, Wallen TR, Little RM, Joondeph DR. Anterior open-bite malocclusion: A longitudinal 10-year postretention evaluation of orthodontically treated patients. Am J Orthod. 1985;87:175–86. doi: 10.1016/0002-9416(85)90038-7. [DOI] [PubMed] [Google Scholar]
- 16.Nahoum HI, Horowitz SL, Benedicto EA. Varieties of anterior open-bite. Am J Orthod. 1972;61:486–92. doi: 10.1016/0002-9416(72)90153-4. [DOI] [PubMed] [Google Scholar]
- 17.Bell WB, Creekmore TD, Alexander RG. Surgical correction of the long face syndrome. Am J Orthod. 1977;71:40–67. doi: 10.1016/0002-9416(77)90176-2. [DOI] [PubMed] [Google Scholar]
- 18.Cangialosi TJ. Skeletal morphologic features of anterior open-bite. Am J Orthod. 1984;85:28–36. doi: 10.1016/0002-9416(84)90120-9. [DOI] [PubMed] [Google Scholar]
- 19.Lundström A, Woodside DG. A comparison of various facial and occlusal characteristics in mature individuals with vertical and horizontal growth direction expressed at the chin. Eur J Orthod. 1981;3:227–35. doi: 10.1093/ejo/3.4.227. [DOI] [PubMed] [Google Scholar]
- 20.Solow B, Houston WJB. Mandibular rotations: Concepts and terminology. Eur J Orthod. 1988;10:177–9. doi: 10.1093/ejo/10.3.177. [DOI] [PubMed] [Google Scholar]
- 21.Björk A, Skieller V. Facial development and tooth eruption. An implant study at the age of puberty. Am J Orthod. 1972;62:339–83. doi: 10.1016/s0002-9416(72)90277-1. [DOI] [PubMed] [Google Scholar]
- 22.Björk A, Skieller V. Normal and abnormal growth of the mandible. A synthesis of longitudinal cephalometric implant studies over a period of 25 years. Eur J Orthod. 1983;5:1–46. doi: 10.1093/ejo/5.1.1. [DOI] [PubMed] [Google Scholar]
- 23.Buschang PH, Santos-Pinto A. Multivariate models for AP movments of the bony chin. J Dent Res. 1979;76:31. [Google Scholar]
- 24.Thompson MA, Buschang RG, Ceen RF, English JD, Harper RP. Unpublished Master’s thesis. Baylor College of Dentistry Department of Orthodontics; 1997. The determinates of antero-posterior movement of mandibular structures. [Google Scholar]
- 25.LaHaye MB, Buschang PH, Alexander RG, Boley JC. Orthodontic Treatment Changes of Chin Position in Class II, Division 1 Patients. Am J Orthod Dentofac Orthop. 2006;130:732–41. doi: 10.1016/j.ajodo.2005.02.028. [DOI] [PubMed] [Google Scholar]
- 26.Phan XL, Schneider BJ, Sadowsky C, BeGole EA. Effects of orthodontic treatment on mandibular rotation and displacement in angle Class II Division 1 malocclusions. Angle Orthod. 2004;74:174–83. doi: 10.1043/0003-3219(2004)074<0174:EOOTOM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 27.Taner-Sarisoy L, Darendeliler N. The influence of extraction orthodontic treatment on craniofacial structures: Evaluation according to two different factors. Am J Orthod Dentofac Orthop. 1999;115:508–14. doi: 10.1016/s0889-5406(99)70272-6. [DOI] [PubMed] [Google Scholar]
- 28.Mair AD, Hunter WS. Mandibular growth direction with conventional Class II nonextraction treatment. Am J Orthod Dentofac Orthop. 1992;101:543–9. doi: 10.1016/0889-5406(92)70129-x. [DOI] [PubMed] [Google Scholar]
- 29.Baumrind S, Molthen R, West EE, Miller DM. Mandibular plane changes during maxillary retraction. Am J Orthod. 1978;74:32–40. doi: 10.1016/0002-9416(78)90043-x. [DOI] [PubMed] [Google Scholar]
- 30.Haralabakis NB, Halazonetis DJ, Sifakakis IB. Activator versus cervical headgear: superimpositional cephalometric comparison. Am J Orthod Dentofac Orthop. 2003;123:296–305. doi: 10.1067/mod.2003.20. [DOI] [PubMed] [Google Scholar]
- 31.Gandini MR, Gandini LG, Martins JC, Del Santo M. Effects of cervical headgear and edgewise appliances on growing patients. Am J Orthod Dentofac Orthop. 2001;119:531–9. doi: 10.1067/mod.2001.113266. [DOI] [PubMed] [Google Scholar]
- 32.Bishara SE. Mandibular changes in persons with untreated and treated Class II Division 1 malocclusion. Am J Orthod Dentofac Orthop. 1998;113:661–73. doi: 10.1016/s0889-5406(98)70227-6. [DOI] [PubMed] [Google Scholar]
- 33.Hubbard GW, Nanda RS, Currier GF. A cephalometric evaluation of nonextraction cervical headgear treatment in class II malocclusions. Angle Orthod. 1994;64:359–70. doi: 10.1043/0003-3219(1994)064<0359:ACEONC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 34.Luppanapornlarp S, Johnston LE. The effects of premolar-extraction: A long-term comparison of outcomes of “clear-cut” extraction and nonextraction class II patients. Angle Orthod. 1993;63:257–72. doi: 10.1043/0003-3219(1993)063<0257:TEOPAL>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 35.Paquette D, Beattie JR, Johnston LE. A long-term comparison of nonextraction and premolar extraction edgewise therapy in “borderline” class II patients. Am J Orthod Dentofac Orthop. 1992;102:1–14. doi: 10.1016/0889-5406(92)70009-Y. [DOI] [PubMed] [Google Scholar]
- 36.Cangialosi TJ, Meistrell ME, Leung MA, Ko JY. A cephalometric appraisal of edgewise class II nonextraction treatment with extraoral force. Am J Orthod Dentofac Orthop. 1988;93:15–24. doi: 10.1016/0889-5406(88)90162-x. [DOI] [PubMed] [Google Scholar]
- 37.Brown P. A cephalometric evaluation of high-pull molar headgear and face-bow neck strap therapy. Am J Orthod. 1978 Dec;:621–32. doi: 10.1016/0002-9416(78)90002-7. [DOI] [PubMed] [Google Scholar]
- 38.Taner-Sarisoy L, Darendeliler N. The influence of extraction orthodontic treatment on craniofacial structures: Evaluation according to two different factors. Am J Orthod Dentofac Orthop. 1999;115:508–14. doi: 10.1016/s0889-5406(99)70272-6. [DOI] [PubMed] [Google Scholar]
- 39.Bishara SE, Cummins DM, Jakobsen JR, Zaher AR. Dentofacial and soft tissue changes in class II, division 1 cases treated with and without extractions. Am J Orthod Dentofac Orthop. 1995;107:28–37. doi: 10.1016/s0889-5406(95)70154-0. [DOI] [PubMed] [Google Scholar]
- 40.Schulz SO, McNamara JA, Jr, Baccetti T, Franchi L. Treatment effects of bonded RME and vertical-pull chin cup followed by fixed appliances in patients with increased vertical dimension. Am J Orthod Dentofac Orthop. 2005;128:326–36. doi: 10.1016/j.ajodo.2004.03.039. [DOI] [PubMed] [Google Scholar]
- 41.Iscan HN, Dincer M, Gultan A, Meral O, Taner-Sarisoy L. Effects of vertical chincap therapy on the mandibular morphology in open-bite patients. Am J Orthod Dentofac Orthop. 2002;122:506511. doi: 10.1067/mod.2002.128643. [DOI] [PubMed] [Google Scholar]
- 42.Sankey WL, Buschang PH, English J, Owen AH., 3rd Early treatment of vertical skeletal dysplasia: the hyperdivergent phenotype. Am J Orthod Dentofac Orthop. 2000;118:317–27. doi: 10.1067/mod.2000.106068. [DOI] [PubMed] [Google Scholar]
- 43.Mojdehi M, Buschang PH, English JD, Wolford LM. Postsurgical growth changes in the mandible of adolescents with vertical maxillary excess growth patterns. Am J Orthod Dentofacial Orthop. 2001;119:106–16. doi: 10.1067/mod.2001.112115. [DOI] [PubMed] [Google Scholar]
- 44.Steinhäuser S, Richter U, Richter F, Bill HJ, Rudzki-Janson I. Profile changes following maxillary impaction and autorotation of the mandible. J Orthofacial Orthop. 2008;69:31–41. doi: 10.1007/s00056-008-0723-8. [DOI] [PubMed] [Google Scholar]
- 45.Zarrinkelk HM, Throckmorton GS, Ellis E, Sinn DP. Functional and morphologic alterations secondary to superior repositioning of the maxilla. J Oral Maxillofac Surg. 1995;53:1258–67. doi: 10.1016/0278-2391(95)90581-2. [DOI] [PubMed] [Google Scholar]
- 46.Southard TE, Buckley MJ, Spivey JD, Krizan KE, Casko JS. Intrusion anchorage potential of teeth versus rigid endosseous implants: A clinical and radiographic evaluation. Am J Orthod Dentofac Orthop. 1995;107:115–120. doi: 10.1016/s0889-5406(95)70125-7. [DOI] [PubMed] [Google Scholar]
- 47.Erverdi N, Keles A, Nanda R. The use of skeletal anchorage in open bite treatment: a cephalometric evaluation. Angle Orthod. 2004;74:381–390. doi: 10.1043/0003-3219(2004)074<0381:TUOSAI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 48.Kuroda S, Sakai Y, Tamamura N, Deguchi T, Takano-Yamamoto T. Treatment of severe anterior open bite with skeletal anchorage in adults: Comparison with orthognathic surgery outcomes. J Orthod Dentofacial Orthop. 2007;132:599–605. doi: 10.1016/j.ajodo.2005.11.046. [DOI] [PubMed] [Google Scholar]
- 49.Xun C, Zeng X, Wang X. Microscrew anchorage in skeletal anterior open-bite treatment. Angle Orthodontist. 2007;77:47–56. doi: 10.2319/010906-14R.1. [DOI] [PubMed] [Google Scholar]
- 50.Akay MC, Aras A, Günbay T, Akyalcin S, Koyuncue BO. Enhanced effect of combined treatment With corticotomy and skeletal snchorage in open bite correction. J Oral Maxillofac Surg. 2009;67:563–569. doi: 10.1016/j.joms.2008.06.091. [DOI] [PubMed] [Google Scholar]
- 51.Carrillo R, Rossouw PE, Franco PF, Opperman LA, Buschang PH, et al. Intrusion of multiradicular teeth and related root resorption with mini-screw implant anchorage: a radiographic evaluation. Am J Orthod Dentofac Orthop. 2007;132:647–55. doi: 10.1016/j.ajodo.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 52.Carrillo R, Buschang PH, Opperman LA, Franco PF, Rossouw PE. Segmental intrusion with mini-screw implant anchorage: a radiographic evaluation. Am J Orthod Dentofacial Orthop. 2007;132:576. e1–6. doi: 10.1016/j.ajodo.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 53.Ramirez-Echave JI, Buschang PH, Carrillo R, Rossouw PE, Nagy WW, Opperman LA. Histological evaluation of root response to intrusion in mandibular teeth in beagle dogs. Am J Orthod Dentofac Orthop. doi: 10.1016/j.ajodo.2009.07.014. In Press. [DOI] [PubMed] [Google Scholar]
- 54.Riolo ML, Moyers RE, McNamara JA, Jr, Hunter WS. An atlas of craniofacial growth Monograph #2. Center for Human Growth and Development, University of Michigan; Ann Arbor: 1974. [Google Scholar]
- 55.Carrillo R, Carrillo RJ, Rossouw PE, Buschang PH. Closed-coil springs for intrusión mechanics with miniscrew anchorage. J Clin Orthod. 2008;42:17–8. [PubMed] [Google Scholar]