Abstract
Research has documented the significant challenges of engaging individuals with comorbid serious mental illness (SMI) and substance use disorders (SUDs) in substance abuse treatment. To date it is unclear which factors predict treatment initiation and engagement in this group of individuals with SUDs. In this study we conducted two analyses using data from a randomized trial of substance abuse treatment in outpatients with SMI: the first examining predictors (collected during screening) of completing an initial intake assessment and the second examining predictors (collected during the intake assessment) of becoming engaged in treatment. Results indicated that males and those with schizophrenia spectrum diagnoses were less likely to complete the intake assessment. Participants who reported more positive feelings about their family were more likely to engage in substance abuse treatment. Participants who were recently arrested were less likely to engage in treatment. Those who met criteria for current drug dependence were less likely to engage in treatment. Overall, these findings are a useful step in determining factors that predict substance abuse treatment initiation and engagement in individuals with SMI and SUDs.
1. Introduction
Treatment of substance use disorders (SUDs) in people with co-occurring serious mental illness (i.e. those with “dual” diagnoses) is a critical public health need. People with serious mental illness (SMI) show alarmingly high rates of SUDs (Mueser, Bennett, & Kushner, 1995; Regier et al., 1990; Winokur et al., 1998) and experience a range of negative consequences of substance use that impact almost every area of functioning (Bennett & Gjonbalaj, 2007). While treatment programs that are tailored to meet the unique psychiatric, social, and cognitive challenges presented by this group of substance abusers have been developed and are showing success (Bellack, Bennett, Gearon, Brown, & Yang, 2006), questions remain on how best to get individuals with SMI to initiate and engage in substance abuse treatment.
Treatment initiation generally refers to beginning the treatment process and can vary by treatment setting but can be thought to include presenting for and completing an initial assessment and returning for some follow-up contact within a specified period of time (Garnick, Horgan, & Chalk, 2006). Treatment engagement has generally been thought of as a step somewhere in between initiation and full participation in treatment, and has been defined by attendance at a specified number of treatment sessions, often 2 to 4 treatment sessions, within a specified number of weeks (e.g. Siqueland et al., 2002). Treatment adherence generally refers to complying with a plan for treatment that has been formulated by a treatment team with a client’s participation. While each of these processes is critical, initiation of and engagement in substance abuse treatment are often the first hurdles that must be overcome in order for an individual with dual SMI and SUDs to receive stable and effective care.
Not surprisingly, both initiation of and engagement in substance abuse treatment are considerably affected by dual disorders (see Daley & Zuckoff, 1998 for a review), especially for individuals with psychotic disorders (Corrigan, Liberman, & Engel, 1990; Nose, Barbui, & Tansella, 2003), and have been widely regarded as critical problems (Miner, Rosenthal, Hellerstein, & Muenz, 1997). For example, in a large naturalistic study of dually diagnosed veterans referred for outpatient treatment (Sekerka, Goldsmith, Brandewie, & Somoza, 1999), 53% failed to become engaged in treatment. Similar results were reported: for a dually diagnosed state hospital sample where 42% attended their first outpatient visit (Appleby, Luchins, Dyson, Fanning, & Freels, 2001); for patients discharged from a community hospital where 35% attended their first outpatient treatment session (Pantalon and Swanson, 2003), and for patients entering a therapeutic community where 49% were lost within the first two weeks (Guydish, Werdegar, Sorensen, Clark, & Acampora, 1998).
Despite the scope of the problem, there has been relatively little empirical work examining methods to increase substance abuse treatment engagement in people with dual SMI and SUDs. A good amount of research has examined the effect of structural procedures - providing reminders of upcoming appointments, initial orientation sessions or written contracts for attending treatment, and scheduling sessions quickly after initial contact - on substance abuse treatment engagement in primary SUD samples. Such strategies have been found to be effective in increasing substance abuse treatment engagement among individuals with primary SUDs (Comfort, Loverro, & Kaltenbach, 2000; Lash, 1998; Lash & Blosser, 1999) and those with primary SUDs and co-occurring psychiatric disorders (DeMarce et al., 2008). Such strategies have become the standard of care in community mental health systems that serve people with SMI (Smith et al., 2010), and research on their utility in increasing rates of engagement in mental health treatment is promising (see Kreyenbuhl, Nossel, & Dixon, 2009 for a review). However, such procedures are generally not sufficient to promote engagement in either mental health or substance abuse treatment in those with dual SMI and SUDs, who often show high levels of functional impairment and are at greatest risk for treatment dropout (Kreyenbuhl et al., 2009). Approaches based on the Transtheoretical Model of Change (Bellack & DiClemente, 1999; Prochaska, DiClemente, & Norcross, 1992) hypothesize that unengaged patients need encouragement to move from the Pre-contemplation or Contemplation stage to the Action stage of change. This has led to a number of trials that employ versions of motivational enhancement therapy (Miller & Rollnick, 1991) to foster engagement by increasing motivation to change. To date, published results in SMI populations for motivational approaches to enhance substance abuse treatment engagement have been encouraging but modest (Baker et al., 2002; Carey, Carey, Maisto, & Purnine, 2002; Swanson, Pantalon, & Cohen, 1999; Ziedonis & Trudeau, 1997). Assertive outreach and other intensive interventions such as case management and assertive community treatment have been found to enhance rates of mental health and substance abuse treatment engagement in individuals with dual SMI and SUDs (see Drake, Mueser, Brunette, & McHugo, 2004 and Kreyenbuhl et al., 2009 for reviews), but due to their intensity are not standard practice for most individuals with dual SMI and SUDs living in the community.
A first step in improving rates of substance abuse treatment initiation and engagement would be to better understand the factors associated with each in individuals with dual SMI and SUDs. In work with primary substance abusers, several studies (sometimes with conflicting results) have found a range of factors associated with non-initiation and non-engagement, including male or female gender, younger age, having a psychiatric diagnosis, more days of recent drug use, unemployment, and non-Caucasian or African American race (e.g. Claus & Kindleberger, 2002; Claus, Kindleberger, & Dugan, 2002; McCaul, Svikis, & Moore, 2001; Siqueland et al., 2002). Having a psychotic disorder in particular has been found to be associated with poor treatment engagement among primary substance abusers (Curran, Stecker, Han, & Booth, 2007). Likewise research on clients with SMI has found a range of predictors associated with non-adherence with mental health treatment referral or nonattendance at a first outpatient psychiatric appointment, including younger age, not taking psychotropic medications, family problems, and low motivation (Compton, Rudisch, Craw, Thompson, & Owens, 2006; Kruse, Rohland, & Wu, 2002; Peeters & Bayer, 1999). Studies of psychiatric samples (i.e. samples of individuals who are identified in mental health settings and have some form of SMI) have found that comorbid substance abuse is one of the strongest factors associated with noninitiation and nonengagement in mental health treatment (El-Mallakh et al., 2004; Fischer et al., 2008; see Kreyenbuhl, Nossel, & Dixon, 2009 and O'Brien, Fahmy, & Singh, 2009 for reviews). Factors related to the context of treatment, including dissatisfaction with care and service providers, have been reported by individuals with SMI as reasons for nonengagement or disengagement in mental health treatment (see Kreyenbuhl, Nossel, & Dixon, 2009 and O'Brien, Fahmy, & Singh, 2009 for reviews).
Research on predictors of initiation and engagement in mental health or substance abuse treatment in individuals with dual SMI and SUDs is more limited. Wolpe, Gorton, Serota, and Sanford (1993) examined predictors of adherence with aftercare (attending 3 or more aftercare appointments) among 48 inpatients with dual SMI and SUDs. Nonadherence was related to cocaine dependence diagnosis (as opposed to abuse), discharge diagnosis of depression, and behavior on the inpatient unit that was “more volatile or erratic” (p. 48). Miner, Rosenthal, Hellerstein, and Muenz (1997) examined a range of psychiatric and psychosocial variables as predictors of compliance with outpatient referral (defined as attending the first two scheduled outpatient appointments following inpatient hospitalization) in 49 individuals with dual schizophrenia and SUDs who were assessed while hospitalized for inpatient psychiatric treatment. Females and individuals with predominantly negative symptoms were more likely to adhere to outpatient referral, whereas men, individuals with mixed-syndrome schizophrenia, and those with fewer negative symptoms were most likely to be non-adherent. Bogenschutz and Siegfreid (1998) examined predictors of treatment engagement (defined as attending 3 or more appointments) in individuals referred to an outpatient dual diagnosis treatment program. Comparisons of those who engaged to those who did not showed that participants referred from inpatient treatment were more likely to engage than those referred from outpatient treatment. In a sample of 120 individuals with dual diagnosis who were inpatients at a state psychiatric hospital, Appleby, Luchins, Dyson, Fanning and Freels (2001) examined predictors of keeping an initial outpatient appointment as well as making two or more outpatient visits within 30 days after discharge. Predictors of attendance at these appointments included “in-person linkage” with aftercare staff and a diagnosis of a psychotic disorder. Mueser and colleagues (2009) examined predictors of engagement (attending at least 2 treatment sessions) as part of a randomized trial comparing two family-based interventions for substance abuse in outpatients with SMI and SUDs. They found that the greater the family member’s perceived benefit of his or her relationship with the client, the less likely the client would engage in SUDs treatment.
Overall, demographic (gender), diagnostic (cocaine dependence, depression diagnosis, days of drug use), and clinical and family factors (behavior while in inpatient treatment; relationship with family) have been associated with treatment engagement in dually diagnosed samples. While informative, the lack of research overall and the variability from study to study in the predictors that are assessed, the samples included, and the focus on treatment initiation versus engagement makes it difficult to draw any general conclusions about the factors that put SMI patients most at risk for failing to engage in substance abuse treatment. In addition, much of the research examining predictors of substance abuse treatment engagement in individuals with dual SMI and SUDs is over a decade old. Changes in our recognition and understanding of the unique needs of these clients (integrated mental health and substance abuse treatment, tailored to address mental health issues such as symptoms and medication, focus on support and motivational enhancement, harm reduction focus; Drake et al., 2004) and current day services that reflect these changes may impact the factors that are associated with substance abuse treatment engagement. In addition, several domains important to treatment outcome and overall functioning in people with SMI – including psychiatric symptoms, patterns of substance use, social and family functioning, and motivation to change – have not been examined as predictors.
The aim of the present study was to address these limitations. We used data from a randomized trial of a behavioral intervention for substance abuse to identify variables which could serve as useful independent predictors of who would initiate treatment and who would engage in treatment (the latter among those who completed the initiation phase, were eligible for the trial, and were randomized to treatment). We have included, along with demographic and diagnostic variables, a range of predictors that could be especially relevant to individuals with SMI and SUDs – including psychiatric symptoms, patterns of substance use, social and family functioning, and motivation to change – that have not been included in previous research. In addition, we have examined predictors of both initiation and engagement, allowing for an examination of whether completing these initial phases of treatment is influenced by the same or different factors.
2. Methods
2.1 The Parent Study
2.1.1 Overview
Data for this project were taken from a randomized trial of a behavioral intervention for substance abuse in a treatment-seeking sample of people with SMI (Behavioral Treatment of Substance Abuse in Schizophrenia (BTSAS)). The BTSAS program (Bellack et al., 2006) included: (1) motivational interviewing; (2) a urinalysis contingency program; (3) goal setting and problem solving in each session; (4) social and coping skills training; (5) education; and (6) relapse prevention. Study participants were randomly assigned to BTSAS or a comparison treatment called Supportive Treatment in Addiction Recovery (STAR) each of which were designed to meet twice per week for six months. Participants were recruited from several community, university-based, and VA mental health and substance abuse treatment clinics in the Baltimore metropolitan area, and were individuals who were diagnosed with a serious mental illness (Lehman, Dixon, Kernan, DeForge, & Postrado, 1997) and a recent drug use disorder (defined as meeting criteria for DSM-IV drug abuse or dependence within the previous 6 months for marijuana, cocaine, or heroin). Participants completed assessments at baseline (intake), post-treatment, and at 6- and 12-months post treatment. Attendance at treatment sessions was tracked for all participants. Assessments included measures of psychiatric symptoms, substance use, psychosocial functioning, and motivation to change. BTSCS was designed to be integrated within mental health care, and participants received mental health care from their regular clinic treatment teams throughout their participation in the study.
2.1.2 Intake Procedures
Individuals were referred for possible study participation by their treatment team and their medical charts were screened to determine preliminary eligibility. Individuals who met preliminary eligibility criteria were contacted, informed about the study, and asked to complete informed consent. The procedure for obtaining informed consent was reviewed and approved by the University of Maryland, School of Medicine Institutional Review Board. Those who consented to participate were asked to complete a baseline intake assessment that consisted of two appointments (each lasting about 2.5 hours) that were typically scheduled a week apart. During the first intake appointment, participants completed a diagnostic assessment that formally determined study eligibility. Those who were eligible for the study and completed the intake phase were subsequently randomized to one of the two substance abuse treatment groups. Overall, 257 participants signed consent and were eligible to participate in the parent study. Six of these were subsequently administratively removed from the study due to personal circumstances that lead to them being unable to continue to participate (e.g. moving out of state) leaving 251 participants eligible to participate. Further details about the parent study can be found in Bellack et al., 2006.
2.2 The Present Study - Analysis of Two Samples
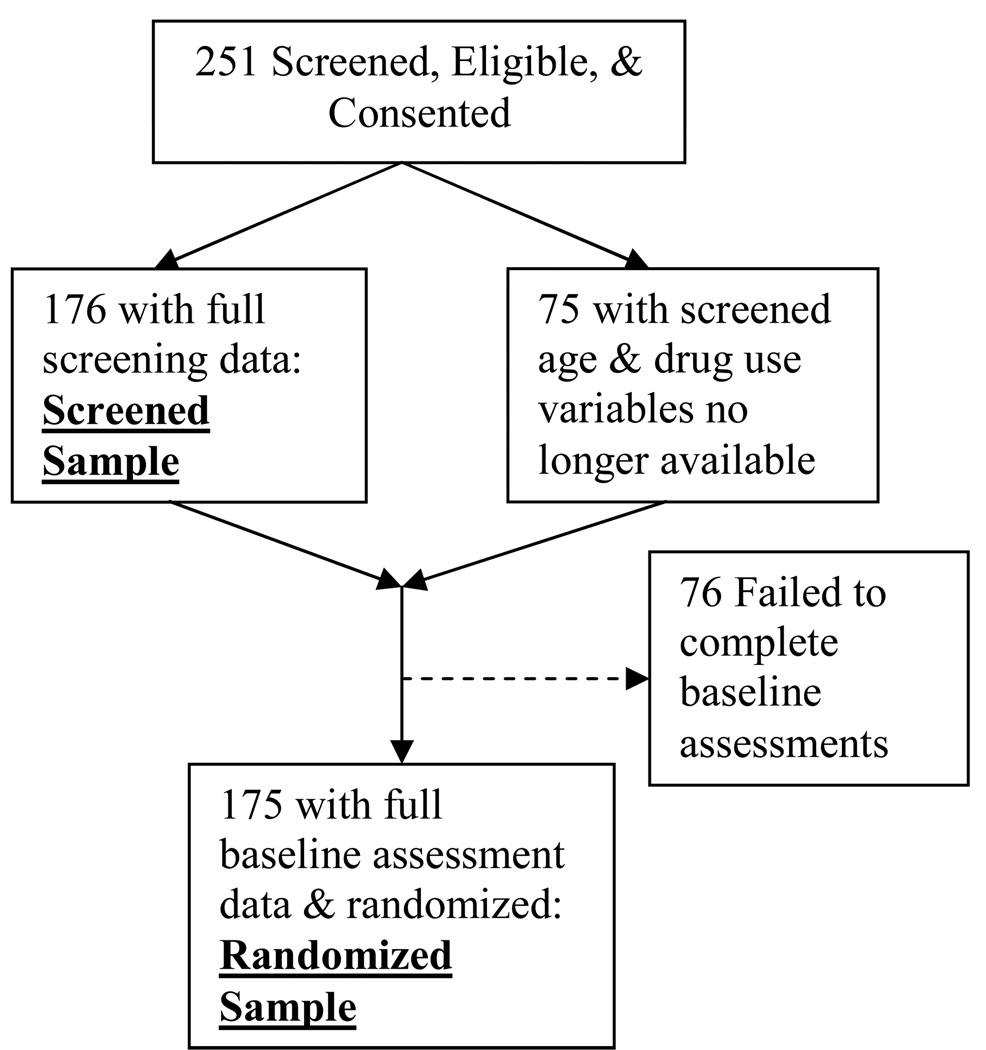
The present study performed analyses on two subsamples from the parent study (Figure 1). The Screened Sample consisted of individuals who were eligible for study participation, provided informed consent, and for whom full screening data were available (n=176 of the 251 eligible to participate in the trial.) Seventy-five of the 251 were not included in the analysis of the Screened Sample because age and indicators for recent cocaine, heroin, and marijuana use were not available. The Screened Sample was 65% male, 77% non-Caucasian and had a mean age of 42.1 (sd = 7.9) and a mean of 11.6 years of education (sd = 2.5). The distribution of psychiatric diagnoses in the Screened Sample was: 20% (n = 36) schizophrenia or schizoaffective disorder, 38% (n = 67) major depression, 20% (n = 35) bipolar disorder, 20% (n = 34) some other form of serious mental illness (with diagnoses for 2 individuals missing.) Thirty-four percent were veterans.
Figure 1.
Formation of the randomized and screened samples.
The Randomized Sample consisted of individuals who were eligible for study participation, provided informed consent, completed the intake assessment phase, and were randomized to a treatment group (n=175 of 251). The Randomized Sample was 63% male, 78% non-Caucasian, had a mean age of 42.7 (sd = 7.1) and a mean of 11.7 years of education (sd = 2.3). These summary statistics match closely those of the Screened Sample. The distribution of participant primary psychiatric diagnosis in the Randomized Sample was: 38% schizophrenia or schizoaffective disorder, 38% major depression, 17% bipolar disorder, and 7% some other form of serious mental illness. Hence, there were somewhat more schizophrenia participants in the Randomized Sample than in the Screened Sample. Forty-one percent were veterans.
2.3 Measures and Variables
2.3.1 Candidate Variables for Predicting Treatment Initiation
Candidate variables for prediction of treatment initiation consisted of those collected during eligibility screening: age, gender, race (Caucasian/Non-Caucasian), education (high school (HS) graduate/not HS graduate), marital history (ever married/never married), veteran status, schizophrenia spectrum disorder (SSD) diagnosis in medical chart, and indication in medical chart of use of cocaine, heroin, and/or marijuana. Treatment initiation was defined as completing the pre-treatment intake assessment phase of the study (2 visits about a week apart).
2.3.2 Intake Measures
Current and lifetime DSM-IV psychiatric and substance use diagnoses were evaluated with the Structured Clinical Interview for DSM-IV-Patient Version (SCID-P; First, Spitzer, Gibbon, & Williams, 1994). A clinical psychologist, social worker, or doctoral student in clinical psychology completed the diagnostic interviews after extensive training that included viewing standard SCID training tapes, viewing and rating videotaped assessments of individual with SMI available in our laboratory, direct observation and rating of at least two live interviews administered by a trained assessor, and completion of two face to face interviews while being observed by a trained assessor. Inter-rater reliability (kappa) for both psychiatric and substance use diagnoses were “very good” both exceeding 0.80 (Altman, 1991). Psychiatric symptoms were assessed with the Positive and Negative Syndrome Scale (PANSS; Opler, Kay, Lindenmayer, & Fiszbein, 1992). Separate ratings were made for positive symptoms, negative symptoms, and general psychopathology. The PANSS has good reliability and validity (Kay, Fiszbein, & Opler, 1987). Substance use and substance use severity were assessed with the Drug/Alcohol section of the Addiction Severity Index (ASI; McLellan et al., 1992), which has high internal consistency (Cronbach’s alpha = 0.79).
Measures of motivation for change included the University of Rhode Island Change Assessment Scale (URICA; McConnaughy, DiClemente, Prochaska, & Velicer, 1989), a 32-item questionnaire with four subscales: precontemplation, contemplation, action, and maintenance. Respondents rate each item on a 5-point Likert scale ranging from "strongly disagree" to "strongly agree". We used an overall continuous readiness to change score calculated as: mean contemplation score + mean action score + mean maintenance score – mean pre-contemplation score (Project MATCH Research Group, 1997). Participants also completed the Temptation to Use Drugs Scale (DiClemente, Carbonari, Montgomery, &, Hughes, 1994), a 20-item measure that assesses the degree to which the participant feels "tempted" to use drugs in different situations. Items rated by the participant for this measure are 5-point scales (1 = not very tempted, 5 = extremely tempted). In our analyses we used the overall scale score.
Social functioning and quality of life variables were assessed using the Brief Quality of Life Interview (BQOL; Lehman, 1995). The BQOL provides a global measure of satisfaction, as well as objective and subjective indicators of quality of life, with ratings that cover multiple life domains. In the analyses of the Randomized Sample, four subscale scores were used: (1) Objective Family Subscale (In the past year, how often did you talk to a family member on the telephone? In the past year, how often did you get together with a family member?); (2) Objective Social Subscale (How often do you visit with someone who does not live with you? How often do you telephone someone who does not live with you? How often do you do something with another person that you planned ahead of time? How often do you spend time with someone you consider more than a friend, like a spouse, a boyfriend or a girlfriend?); (3) Subjective Family Subscale (How do you feel about the way you and your family act toward each other? How do you feel about the way things are in general between you and your family?); and (4) Subjective Social Subscale (How do you feel about the things you do with other people? How do you feel about the amount of time you spend with other people? How do you feel about the people you see socially?) For the subjective indicators, participants rate their feelings regarding different family and social variables on a 7-point terrible-to-delighted scale (1 = terrible, 7 = delighted).
Section 2.3.3 Candidate Variables for Predicting Treatment Engagement
Based on prior research and clinical expertise, we identified 30 candidate variables potentially predictive of treatment engagement from demographic variables and the above measures. These variables could be organized under six domains: demographics, psychiatric clinical, substance abuse clinical, legal trouble, family and social, and readiness to change (Table 1). Treatment engagement was defined as attending at least three treatment sessions.
Table 1.
Candidate predictors of treatment engagement by domain.
| Domain | Variable |
|---|---|
| Demographics | Age |
| Race (Caucasian/Non-Caucasian) | |
| Gender (male/female) | |
| Education (HS graduate/Not HS graduate) | |
| Veteran status (veteran/not veteran) | |
| Psychiatric/clinical | Diagnosis (schizophrenia spectrum disorder vs. other) |
| Days of hospitalization, past 90 days | |
| PANSSa Positive Subscale | |
| PANSS negative subscale | |
| PANSS general subscale | |
| PANSS depression subscale | |
| Substance abuse/clinical | Current/recent drug dependence |
| Current alcohol dependence | |
| Heroin use, years | |
| Cocaine use, years | |
| Marijuana use, years | |
| Days of drug useb, last month | |
| Days of drug problems, last month | |
| Days drug treatment, last month | |
| Legal trouble | Arrested in last 90 days (yes/no) |
| Number of arrests/charges (lifetime) | |
| Family/social | Independent living situation (yes/no) |
| Subjective family BQOLc subscale | |
| Objective family BQOL subscale | |
| Subjective social BQOL subscale | |
| Objective social BQOL subscale | |
| Days of family conflict, last month | |
| Days of other conflict, last month | |
| Motivation to change | Readiness to change |
| Temptation to use drugs |
Positive and negative syndrome scale.
Days of drug use = number of days of cocaine use + number of days of heroin use + number of days of marijuana use in the past 30 days.
Brief quality of life inventory.
2.4 Data Analysis
2.4.1 Treatment initiation prediction model
Data analyses were conducted separately for the Screened and Randomized samples. For the Screened Sample (n=176), two steps were taken to construct a multivariate model for predicting completion of the intake assessment phase (i.e. completing treatment initiation). In the first step, univariate comparisons were made between those who completed the intake assessment (n=120) and those who did not (n=56) on 10 available and plausible predictors of treatment initiation collected during screening using chi-square tests. In the second step, variables that differed at the p < 0.10 significance level were then entered into a multivariate logistic regression model. To construct a parsimonious model, non-significant predictors were removed from the model one at a time using backward selection until all remaining predictors had p-values less than .10 (2-sided). Predictors with p-values less than .05 were considered statistically significant.
In the Screened sample, all variables had only 1 or 2 missing values except for Education and Marital history which had 19 (10.8% of the sample) and 9 (5.1%) missing values, respectively. Overall, since there were relatively few missing data values, no missing data procedures (such as imputation) were used in these analyses.
Nagelkerke’s R2 (a “pseudo” R2) for logistic regression (Nagelkerke, 1991; Cragg & Uhler, 1970) was calculated to assess relative improvement in prediction over the null model (i.e. intercept only model). We calculated the Nagelkerke R2, an adjusted version of the Cox and Snell R2 because it has the property that the maximum possible value is 1, as does the R2 for ordinary least squares regression.
2.4.2 Treatment engagement prediction model
Similar steps were taken to construct a multivariate logistic regression model for predicting treatment engagement from the Randomized Sample. After examining frequency distributions and inter-correlations (to assess potential collinearity) among the 30 candidate predictor variables, we made univariate comparisons between those who became engaged in treatment (n=110) versus those who did not (n=75) using chi-square and t tests. In the second step, variables that differed at the p < 0.10 significance level were then entered into a multivariate logistic regression model. To construct a parsimonious model, predictors were removed from the model one at a time using backward selection until all remaining predictors were significant at the p < .10 level. Predictors with p-values less than .05 were considered statistically significant. Continuous scale predictors were centered at the mean and if significant, linearity in the model was checked by adding the square term for the predictor into the model and checking its significance.
The number of missing values was very low (usually 1 or 2 and at most 5) for all of the variables in these analyses except one, Independent Living Status which had 17 missing values (9.7% of the sample). Overall, due to low numbers of missing values, no missing data procedures were used.
The pseudo R2 was computed for the final engagement model.
3. Results
3.1 Treatment initiation prediction model
Of the 176 participants in the Screened Sample, 120 (68%) completed the baseline intake and 56 (32%) did not. Univariate comparisons between these groups identified three candidate predictors for the multivariate model: gender, schizophrenia spectrum diagnosis, and chart indication of recent cocaine use (Table 2). All three of these predictors remained in the multivariate model after backward selection (Table 3). After accounting for the other predictors in the model, males had only 46% of the odds that females had of initiating treatment, and participants with a schizophrenia spectrum diagnosis had just 44% of the odds that those with other psychiatric diagnoses had of initiating treatment. Those with a chart indication of recent cocaine use had a 2.09 times greater odds of completing intake than those with indication of recent heroin or marijuana use, although this result fell short of the .05 significance level (p=.059). The pseudo R-square for the final model was 0.10 suggesting a small degree of improved prediction over having no predictors.
Table 2.
Comparison of screening variables between participants who initiated treatmenta and those who did not in the Screened Sample (n=176)b.
| Screening variable |
Completed intake phase (n = 120)c |
Did not complete intake phase (n = 56) |
Statistic | DFd | P-valuee |
|---|---|---|---|---|---|
| Age | 42.6 ± 7.5 | 41.0 ± 8.8 | t = 1.23 | 173 | 0.22 |
| Gender (male) | 71 (59%) | 43 (77%) | χ2 = 5.19 | 1 | 0.02 |
| Race (Caucasian) | 28 (23%) | 13 (24%) | χ2 = 0.00 | 1 | 0.97 |
| Education (high school grad)f | 78 (65%) | 26 (70%) | χ2 = 0.35 | 1 | 0.55 |
| Marital history (ever married)f | 51 (42%) | 26 (55%) | χ2 = 2.23 | 1 | 0.13 |
| SSDg in medical chart | 19 (16%) | 17 (32%) | χ2 = 5.56 | 1 | 0.02 |
| Cocaine use in medical chart | 98 (82%) | 38 (68%) | χ2 = 4.15 | 1 | 0.04 |
| Heroin use in medical chart | 53 (44%) | 25 (45%) | χ2 = 0.00 | 1 | 0.95 |
| Marijuana use in medical chart | 26 (22%) | 11 (20%) | χ2 = 0.09 | 1 | 0.76 |
| Veteran | 37 (31%) | 22 (39%) | χ2 = 1.22 | 1 | 0.27 |
Initiated treatment = completed two intake assessment visits.
Recent cocaine, heroin, and marijuana use and age not available for 75 of the 251 eligible participants.
Two assessments separated by about a week.
Degrees of freedom.
Variables with p-value < 0.10 to be entered into multivariate model for predicting completion of intake.
There were 19 missing values for Education; 9 missing values for Marital history.
SSD = schizophrenia spectrum disorder.
Table 3.
Multivariate logistic regression model for predicting treatment initiation using the Screened Sample (N = 176)a, b.
| Variable | Beta estimate | Standard error (SE) | Wald χ2 statisticc | P-value | Adjusted odds ratio | 95% Confidence interval |
|---|---|---|---|---|---|---|
| Intercept | 0.96 | 0.42 | 5.13 | 0.023 | – | – |
| Gender (male) | −0.78 | 0.38 | 4.23 | 0.040 | 0.46 | (0.22, 0.96) |
| Psychiatric diagnosis (SSD)d | −0.81 | 0.39 | 4.25 | 0.039 | 0.44 | (0.20, 0.96) |
| Cocaine use indicated | 0.74 | 0.39 | 3.58 | 0.059 | 2.09 | (0.97, 4.48) |
Two observations were dropped from the regression analysis due to missing values.
Treatment initiation defined as attending and completing both days of intake assessment.
Degrees of freedom = 1 for all tests.
SSD = Schizophrenia spectrum disorder.
3.2 Engagement prediction model
Of the 175 participants in the Randomized Sample, 110 (63%) became engaged in treatment and 65 (37%) did not become engaged in treatment. Univariate comparisons between these groups identified 8 candidate baseline predictors for the multivariate model: psychiatric hospitalization in the past 90 days, drug dependence status, number of days of drug use, number of days of drug treatment, subjective family quality of life subscale, subject social quality of life subscale, and the temptation to use drugs subscale (Table 4). After backward selection, three of these variables remained as independent predictors in the multivariate model, all significant: arrest in the prior 90 days, drug dependence status, and the subjective family quality of life subscale (Table 5).
Table 4.
Domain comparisons and descriptive statistics for those who engaged and did not engage in treatment in the Randomized Sample (N = 175).
| Domain | Variable | Not engaged (N = 65) |
Engageda (N = 110) |
Comparison | p | ||
|---|---|---|---|---|---|---|---|
| Test | df | Test value | |||||
| Demographics | Age | 42.49 ± 7.25 | 42.78 ± 7.04 | t | 173 | −0.26 | 0.795 |
| Caucasian | 14 (21.5%) | 25 (22.7%) | χ2 | 1 | 0.03 | 0.855 | |
| Male | 38 (58.5%) | 73 (66.4%) | χ2 | 1 | 1.10 | 0.294 | |
| Education (high school graduate) | 38 (60.3%) | 74 (67.3%) | χ2 | 1 | 0.85 | 0.357 | |
| Veteran | 27 (41.5%) | 45 (40.9%) | χ2 | 1 | 0.01 | 0.935 | |
| Psychiatric/clinical | Psychiatric diagnosis (SSDb vs other) | 25 (38.5%) | 42 (38.2%) | χ2 | 1 | 0.00 | 0.971 |
| Psychiatric hospitalization, past 90 days | 25 (39.1%) | 26 (23.9%) | χ2 | 1 | 4.49 | 0.034 | |
| PANSSc Positive subscale | 1.84 ± 0.59 | 1.83 ± 0.7 | t | 173 | 0.05 | 0.962 | |
| PANSS negative subscale | 1.78 ± 0.67 | 1.78 ± 0.57 | t | 173 | 0.04 | 0.972 | |
| PANSS general subscale | 1.87 ± 0.36 | 1.84 ± 0.4 | t | 173 | 0.40 | 0.689 | |
| PANSS depression subscale | 2.87 ± 0.9 | 2.73 ± 0.91 | t | 173 | 0.95 | 0.343 | |
| Substance | Drug dependence statusd | 54 (83.1%) | 60 (54.5%) | χ2 | 1 | 14.65 | <0.001 |
| Abuse/clinical | Current alcohol dependence | 21 (32.3%) | 24 (22.0%) | χ2 | 1 | 2.25 | 0.134 |
| Heroin use, years | 0.8 ± 3.42 | 0.84 ± 3.6 | t | 172 | −0.08 | 0.937 | |
| Cocaine use, years | 9.41 ± 8.43 | 10.75 ± 8.08 | t | 172 | −1.04 | 0.298 | |
| Marijuana use, years | 9.42 ± 10.42 | 10.68 ± 10.39 | t | 173 | −0.78 | 0.437 | |
| Days of drug use, last monthe | 9.57 ± 12.5 | 5.61 ± 9.63 | t | 109 | 2.35 | 0.030 | |
| Days of drug problems, last month | 10.34 ± 11.47 | 8.75 ± 11.25 | t | 173 | 0.90 | 0.370 | |
| Days of drug treatment, last month | 11.52 ± 10.25 | 16.17 ± 11.66 | t | 171 | −2.65 | 0.009 | |
| Legal trouble | Number of arrests/charges, lifetime | 6.51 ± 8.56 | 4.68 ± 7.89 | t | 173 | 1.43 | 0.154 |
| Arrested in last 90 days | 14 (21.9%) | 10 (9.2%) | χ2 | 1 | 5.44 | 0.020 | |
| Family/Social | Independent living situation (yes/no) | 26 (47.3%) | 36 (35.0%) | χ2 | 1 | 2.28 | 0.131 |
| Subjective family BQOLf subscale | −0.5 ± 1.75 | 0.3 ± 1.72 | t | 168 | −2.92 | 0.004 | |
| Objective family BQOL subscale | 3.25 ± 1.1 | 3.3 ± 1.1 | t | 168 | −0.27 | 0.787 | |
| Subjective social BQOL subscale | −0.27 ± 1.4 | 0.17 ± 1.22 | t | 168 | −2.15 | 0.033 | |
| Objective social BQOL subscale | 0.14 ± 1 | −0.09 ± 1.03 | t | 168 | 1.46 | 0.147 | |
| Days of family conflict, last month | 3.71 ± 7.88 | 2.88 ± 7.6 | t | 173 | 0.69 | 0.494 | |
| Days of conflict w/others, last month | 2.83 ± 6.8 | 2.65 ± 6.62 | t | 173 | 0.18 | 0.860 | |
| Motivation to Change | Readiness to change | 10.39 ± 1.59 | 10.5 ± 1.65 | t | 170 | −0.41 | 0.683 |
| Temptation to use drugs | 3.1 ± 0.94 | 2.68 ± 0.95 | t | 172 | 2.83 | 0.005 | |
Engaged defined as attending 3 or more treatment sessions.
Schizophrenia spectrum disorder.
Positive and negative syndrome scale.
Current versus recent drug dependence.
Days of drug use = number of days of cocaine use + number of days of heroin use + number of days of marijuana use in the past 30 days.
Brief quality of life interview.
Table 5.
Full multivariate logistic regression model predicting engagement for the Randomized Sample (n = 175)a.
| Baseline variable |
Estimate | SE | Wald χ2 statisticb |
P-value | Adjusted odds ratio (AOR) |
95% Confidence interval (AOR) |
|---|---|---|---|---|---|---|
| Intercept | 1.53 | 0.35 | 19.4 | <0.001 | – | – |
| Drug dependence statusc | −1.19 | 0.40 | 9.02 | 0.003 | 0.30 | (0.14, 0.66) |
| Subjective family BQOLd scalee | 0.24 | 0.10 | 5.64 | 0.018 | 1.27 | (1.04, 1.55) |
| Arrested in past 90 days (y/n) | −0.99 | 0.48 | 4.24 | 0.039 | 0.37 | (0.15, 0.95) |
Six observations were dropped from the regression analysis due to missing values.
Degrees of freedom = 1.
Current versus recent drug dependence.
BQOL = brief quality of life interview.
Centered at the mean.
The final engagement model indicates that after adjusting for the other predictors, those with current drug dependence had only 30% the odds of engaging in treatment versus those with recent drug dependence. Also, a participant who rated their positive feelings towards their family one point higher than another individual on the 7-point terrible-to-delighted scale would, on average, have a 27% greater odds of engagement. Furthermore, the relative odds is increased another 27% for every 1-point increase in the difference between the two individuals. Those with an arrest in the 90 days prior to the baseline assessment had 37% the odds of engaging in treatment versus those who had not had an arrest in that time period.
The pseudo R-square for the engagement model was 0.184 indicating a 18.4% improvement in prediction versus the intercept only model.
4. Discussion
The present study examined predictors of initiating treatment for substance abuse in individuals with dual diagnosis, with initiation defined as completing a pre-treatment intake assessment. Male gender and schizophrenia spectrum diagnosis were associated with a decreased likelihood of initiating treatment. Several studies have found that males, both in primary substance abusing samples (Claus & Kindleberger, 2002) and in samples of individuals with dual disorders (Bogenschutz & Siegfreid, 1998; Miner et al., 1997) are less likely to initiate substance abuse treatment. While men and women with dual SMI and SUDs have been found to show similar substance abuse severity (Brunette & Drake, 1997; Drapalski, Bennett, & Bellack, in press), dually diagnosed men have been found to report lower motivation to change at the start of substance abuse treatment (Drapalski, et al., in press). It is possible that lower readiness to change in dually diagnosed men reflects less of a willingness to seek help for substance abuse. Similarly, individuals with schizophrenia spectrum diagnoses experience a range of difficulties that can impact their ability to complete a substance abuse treatment intake assessment, including low readiness to change (Ziedonis & Trudeau, 1997), negative symptoms that can interfere with treatment initiation (Blanchard, Mueser, & Bellack, 1998), and cognitive impairments that can make it difficult to attempt intentional behavior change (Bellack & DiClemente, 1999). Other studies have found that some subgroups of individuals with schizophrenia, such as those with mixed-syndrome schizophrenia and fewer negative symptoms (Miner et al., 1997) are less likely to initiate or engage in substance abuse treatment. It could be that individuals with more positive or less well-controlled symptoms of schizophrenia are less likely to follow through with an initial substance abuse treatment appointment. As we did not breakdown schizophrenia diagnoses in this way, and we did not collect data on symptoms until the intake assessment, our results cannot speak directly to this. However, these findings match what we have found working clinically with this population.
Among those who initiated treatment, we then analyzed predictors of engaging in treatment, defined as attending three or more treatment sessions. In the treatment engagement prediction model, current drug dependence and recent arrest were associated with lowered odds of engaging in treatment, findings that are consistent with others in the literature. Current drug dependence is associated with many factors that make scheduling and attending treatment appointments difficult for people with SMI, including more severe symptoms, more chaotic living situations, and poorer self care and life functioning (Swartz et al., 2006). Poorer functioning and poorer symptom management have been found to be related to treatment nonattendance (Killaspy, Banerjee, King, & Lloyd, 2000). Legal problems such as arrests often signal that an individual with SMI is involved in activities related to drug procurement and use and so either may not be seriously considering substance abuse treatment or may not be able to attend the first few treatment sessions due to court and other legal requirements. Research has found relationships between arrests and poor treatment engagement in dually diagnosed samples (Clark, Ricketts, & McHugo, 1999).
Positive feelings about time spent and interactions with family members was related to greater odds of engaging in treatment. These findings are in line with a range of research that highlights the benefits of family relationships in terms of getting people into treatment both in primary substance abusers (Copello, Templeton, & Velleman, 2006) and among those with SMI (see Dixon et al, 2009 for a review; Fischer et al., 2008; Harvery, Jefferys, McNaught, Blizard, & King, 2007; Mueser et al., 2009) and first-episode psychosis (Compton, Goulding, Gordon, Weiss, & Kaslow, 2009). Often individuals seek substance abuse treatment specifically at the request of relatives or because of the damage their substance use is doing to relationships with family members. Likewise family members may provide tangible support so those with dual disorders can make and keep treatment appointments. Positive feelings about family may be a sign that the individual is receiving support from others that serves to help him or her engage in substance abuse treatment. Alternatively, positive feelings may reflect emotional support from others that helps the client believe that he/she is accepted or valued or understood. It could be that these positive emotions are integral to treatment engagement.
Psychiatric symptom and motivation to change variables were not related to treatment engagement in the sample. Research on the relationship between symptoms and nonengagement in or dropout from mental health treatment in individuals with SMI has been mixed (see O'Brien, Fahmy, & Singh for a review). Miner and colleagues (1997) found that levels of negative symptoms were related to substance abuse treatment engagement in a dual diagnosis sample. Our results suggest that psychiatric symptoms may be less important than drug dependence to substance abuse treatment engagement. It is possible that symptoms in the sample were better managed due to the fact that all participants continued to see their regular mental health treatment teams and the substance abuse treatment program under study was integrated with their mental health care. As integrated care becomes the norm for individuals with dual SMI and SUDs, research can further examine whether symptoms have less of an impact on substance abuse treatment engagement.
Readiness to change and temptation to use were also not related to treatment engagement in the sample, findings that differ from research with primary substance abusers (see Nidecker et al., 2009 for a brief review). Our work has shown that measures tapping motivation to change perform well in samples of individuals with SMI (Nidecker, DiClemente, Bennett, & Bellack, 2008) and are related in expected ways to other indicators of substance use in these samples (Bennett, Bellack, Brown, & DiClemente, 2009; Nidecker et al., 2009). In the present study, readiness to change scores were similar for engaged and nonengaged participants. It is possible that during the intake assessment, when readiness was assessed, all participants reported similar readiness, but that readiness dropped off for some once the time to actually engage in treatment was at hand. As we do not have reassessments of readiness closer to the time of the start of treatment, we cannot directly test this hypothesis, but it is plausible that readiness may change as the start of treatment approaches. It is also possible that readiness to change can be overshadowed by, or is less important than, the practical difficulties of starting substance abuse treatment for many individuals with SMI, such as remembering a new treatment group, securing additional transportation to the clinic to attend the new group, and fitting a new group into an existing treatment schedule. Such practical considerations may pose barriers to treatment engagement for some individuals with SMI despite their reported desire to make a change.
Overall, these results illustrate two important points. First, the results for the engagement model are interesting in their similarity to predictors of engagement in substance abuse treatment more generally. That is, of the variables identified as significant predictors of nonengagement (drug dependence, legal problems) or engagement (positive feelings about family), none were uniquely important to individuals with SMI, such as negative symptoms, positive symptoms, past hospitalization, or independent living. Rather, drug dependence (or similar variables tapping greater drug use and severity) and legal issues impact many groups of substance abusers, not just those with SMI. Similarly, the beneficial impact of positive feelings about family relationships to the treatment process is not unique to individuals with dual SMI and SUDs. These findings raise the possibility that substance abusers with SMI may be more similar to other groups of substance abusers in terms of the factors that promote or inhibit engagement in substance abuse treatment. Overall, greater severity of drug use and legal problems may signal that an individual is not likely to commit to substance abuse treatment. Second, even though we included a range of variables across a number of domains in the engagement model, our ability to predict engagement overall was not high. This suggests that more work needs to be done in order to better predict which individuals with SMI are most likely to initiate and engage in substance abuse treatment.
These results have clinical implications. Males with schizophrenia may be especially likely to not initiate substance abuse treatment. Service providers who work with individuals with dual SMI and SUDs may need to identify incentives such as assistance with legal problems, housing and homelessness, or other issues that can convince men with SMI that substance abuse treatment can be worthwhile. That is, treatment goals centered on reducing the negative consequences from substance use, rather than targeting the drug use per se, may allow individuals with SMI to build trust with treatment providers and become comfortable with treatment, setting the stage for working to reduce or stop drug use in the future. A focus on the benefits of substance abuse treatment as a way to improve mental health functioning may be less useful early in the treatment engagement process, as symptoms are not the reason that people fail to engage in treatment. In addition, connecting to supportive family members at the start of treatment may help individuals with SMI engage in substance abuse treatment.
This study had several limitations. Our sample was unique in that it included a high proportion of veterans and all participants consented to receive substance abuse treatment as part of a clinical research trial. It is possible that these factors impact generalizability of the findings to other groups of individuals with SMI and SUDs. Veterans with SMI may be more connected to care at Veterans Affairs Medical Centers than non-veterans with SMI, and there may be factors associated with agreeing to participate in research - such as reimbursement for completion of research assessments, contact with research staff in addition to clinical contact - that make the situation different from seeking substance abuse treatment in community or other non-research settings. Interestingly, even with such factors that would presumably enhance treatment initiation and engagement, our rates of failure to complete intake (32%) and nonengagement in the study intervention (37%) illustrate the challenges in promoting substance abuse treatment engagement even with individuals who might have incentives or benefits not found in other settings. Moreover, veteran status did not emerge as a significant predictor of engagement. In addition, the intake assessment consisted of two appointments (each lasting about 2.5 hours); such an extended assessment phase could have impacted participants’ willingness to further engage in the treatment phase of the parent study. Complete screening data were not available on all participants in the parent study; it is unclear if those with complete screening data were somehow different from those without it. In addition, as is typical, only a small set of variables were collected during screening. There are likely other factors associated with completion or non-completion of the intake assessment phase that were not assessed at screening. While the variables selected to predict engagement were selected based on prior research and clinical expertise, it is possible that other important variables were not included. In addition, successfully predicting substance abuse treatment initiation and engagement may require a combination of variables that differ for subgroups of abusers. Hellemann, Conner, Anglin, and Longshore (2009) describe their analysis of 195 variables to create decisions trees that take into account different predictors for different sorts of substance abuse treatment clients in predicting treatment retention. Their analyses identified five variables that, in various combinations, characterized six different groups of abusers, three of which were associated with treatment retention and three with treatment dropout. This sort of conceptualization that takes into account different paths into and out of treatment seems to be a potentially useful way to understand the different factors that may be associated with treatment initiation and engagement for different individuals.
5. Conclusion
This study identified separate predictors for substance abuse treatment initiation and engagement in a sample of individuals with SMI and SUDs. Male gender and schizophrenia spectrum diagnosis were both associated with a decreased likelihood of initiating treatment, while current drug dependence and recent arrest were associated with lowered odds of engaging in treatment. In addition, positive feelings about family relationships were related to greater odds of engaging in treatment. Overall, these findings are a useful step in determining factors that predict substance abuse treatment initiation and engagement in individuals with SMI and SUDs.
Acknowledgements
This research was supported by Grant RO1 DA 012265 from the National Institute on Drug Abuse to Alan S. Bellack, and by the VA Capitol Healthcare Network Mental Illness Research Education and Clinical Center (MIRECC, A.S. Bellack, Ph.D., Director).
Role of Funding Sources
Funding for this study was provided by NIDA Grant R01-DA012265. NIDA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Dr’s Bellack, Bennett, and Brown designed the study and planned the analysis. Dr. Bennett conducted literature searches and provided summaries of previous research studies. Dr. Brown and Ms. Li conducted the statistical analysis and interpreted results. Dr’s Brown and Bennett wrote the first draft of the manuscript and all authors contributed to and have approved the final manuscript.
Conflict of Interest
All authors declare that they have no conflicts of interest.
References
- Altman DG. Practical Statistics for Medical Research. New York: Chapman & Hall; 1991. [Google Scholar]
- Appleby L, Luchins DJ, Dyson V, Fanning T, Freels S. Predischarge linkage and aftercare contact among dually-diagnosed public psychiatric patients. Journal of Nervous and Mental Disease. 2001;189:265–267. doi: 10.1097/00005053-200104000-00010. [DOI] [PubMed] [Google Scholar]
- Baker A, Lewin T, Reichler H, Clancy R, Carr V, Garrett R, et al. Motivational interviewing among psychiatric inpatients with substance use disorders. Acta Psychiatrica Scandinavica. 2002;106:233–240. doi: 10.1034/j.1600-0447.2002.01118.x. [DOI] [PubMed] [Google Scholar]
- Bellack AS, Bennett ME, Gearon JS, Brown CH, Yang Y. A randomized clinical trial of a new behavioral intervention for drug abuse in people with severe and persistent mental illness. Archives of General Psychiatry. 2006;63:426–432. doi: 10.1001/archpsyc.63.4.426. [DOI] [PubMed] [Google Scholar]
- Bellack AS, DiClemente CC. Treating substance abuse among patients with schizophrenia. Psychiatric Services. 1999;50:75–80. doi: 10.1176/ps.50.1.75. [DOI] [PubMed] [Google Scholar]
- Bennett ME, Bellack AS, Brown CH, DiClemente C. Substance dependence and remission in schizophrenia: A comparison of schizophrenia and affective disorders. Addictive Behaviors. 2009;34(10):806–814. doi: 10.1016/j.addbeh.2009.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett ME, Gjonbalaj S. The Problem of Dual Diagnosis. In: Hersen M, Turner S, Beidel D, editors. Adult Psychopathology and Diagnosis. 5th ed. New York: John Wiley and Sons; 2007. pp. 34–77. [Google Scholar]
- Blanchard JJ, Mueser KT, Bellack AS. Anhedonia, positive and negative affect, and social functioning in schizophrenia. Schizophrenia Bulletin. 1998;24:413–424. doi: 10.1093/oxfordjournals.schbul.a033336. [DOI] [PubMed] [Google Scholar]
- Bogenschutz MP, Siegfreid SL. Factors affecting engagement of dual diagnosis patients in outpatient treatment. Psychiatric Services. 1998;49:1350–1352. doi: 10.1176/ps.49.10.1350. [DOI] [PubMed] [Google Scholar]
- Brunette MF, Drake RE. Gender differences in patients with schizophrenia and substance abuse. Comprehensive Psychiatry. 1997;38:109–116. doi: 10.1016/s0010-440x(97)90090-0. [DOI] [PubMed] [Google Scholar]
- Carey KB, Carey MP, Maisto SA, Purnine DM. The feasibility of enhancing psychiatric outpatients' readiness to change their substance use. Psychiatric Services. 2002;53:602–608. doi: 10.1176/appi.ps.53.5.602. [DOI] [PubMed] [Google Scholar]
- Clark RE, Ricketts SK, McHugo GJ. Legal system involvement and costs for persons in treatment for severe mental illness and substance use disorders. Psychiatric Services. 1999;50:641–647. doi: 10.1176/ps.50.5.641. [DOI] [PubMed] [Google Scholar]
- Claus RE, Kindleberger LR. Engaging substance abusers after centralized assessment: Predictors of treatment entry and dropout. Journal of Psychoactive Drugs. 2002;34:25–31. doi: 10.1080/02791072.2002.10399933. [DOI] [PubMed] [Google Scholar]
- Claus RE, Kindleberger LR, Dugan MC. Predictors of attrition in a longitudinal study of substance abusers. Journal of Psychoactive Drugs. 2002;34:69–74. doi: 10.1080/02791072.2002.10399938. [DOI] [PubMed] [Google Scholar]
- Comfort M, Loverro J, Kaltenbach K. A search for strategies to engage women in substance abuse treatment. Social Work in Health Care. 2000;31:59–70. doi: 10.1300/J010v31n04_04. [DOI] [PubMed] [Google Scholar]
- Compton MT, Goulding SM, Gordon TL, Weiss PS, Kaslow NJ. Family-level predictors and correlates of the duration of untreated psychosis in African American first episode patients. Schizophrenia Research. 2009;115:338–345. doi: 10.1016/j.schres.2009.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton MT, Rudisch BE, Craw J, Thompson T, Owens DA. Predictors of missed first appointments at community mental health centers after psychiatric hospitalization. Psychiatric Services. 2006;57:531–537. doi: 10.1176/ps.2006.57.4.531. [DOI] [PubMed] [Google Scholar]
- Copello AG, Templeton L, Velleman R. Family interventions for drug and alcohol misuse: Is there a best practice? Current Opinion in Psychiatry. 2006;19:271–276. doi: 10.1097/01.yco.0000218597.31184.41. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Liberman RP, Engel JD. From noncompliance to collaboration in the treatment of schizophrenia. Hospital and Community Psychiatry. 1990;41:1203–1211. doi: 10.1176/ps.41.11.1203. [DOI] [PubMed] [Google Scholar]
- Cragg J, Uhler R. The demand for automobiles. Canadian Journal of Economics. 1970;3:386–406. [Google Scholar]
- Curran GM, Stecker T, Han X, Booth BM. Individual and program predictors of attrition from VA substance use treatment. Journal of Behavioral Health Services Research. 2007;36(1):25–34. doi: 10.1007/s11414-007-9093-z. [DOI] [PubMed] [Google Scholar]
- Daley DC, Zuckoff A. Improving compliance with the initial outpatient session among discharged inpatient dual diagnosis clients. Social Work. 1998;43:470–473. doi: 10.1093/sw/43.5.470. [DOI] [PubMed] [Google Scholar]
- DeMarce JM, Lash SJ, Stephens RS, Grambow SC, Burden JL. Promoting continuing care adherence among substance abusers with co-occurring psychiatric disorders following residential treatment. Addictive Behaviors. 2008;33:1104–1112. doi: 10.1016/j.addbeh.2008.02.008. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Carbonari JP, Montgomery RPG, Hughes SO. The Alcohol Abstinence Self-Efficacy Scale. Journal of Studies on Alcohol. 1994;55:141–148. doi: 10.15288/jsa.1994.55.141. [DOI] [PubMed] [Google Scholar]
- Dixon LB, Dickerson F, Bellack AS, Bennett M, Dickinson D, Goldberg RW, et al. Schizophrenia Patient Outcomes Research Team. The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophrenia Bulletin. 2009;36(1):48–70. doi: 10.1093/schbul/sbp115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake RE, Mueser KT, Brunette MF, McHugo GJ. A review of treatments for clients with severe mental illness and co-occurring substance use disorder. Psychiatric Rehabilitation Journal. 2004;27:360–374. doi: 10.2975/27.2004.360.374. [DOI] [PubMed] [Google Scholar]
- Drapalski AL, Bennett ME, Bellack AS. Gender differences in substance use, consequences, motivation to change, and treatment seeking in people with serious mental illness. Substance Use and Misuse. doi: 10.3109/10826084.2010.538460. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Mallakh RS, James T, Khan T, Katz M, McGovern B, Nair S, et al. Follow-up after inpatient psychiatric hospitalization with partial control of the system responsiveness variable. Psychiatry. 2004;67(3):294–298. doi: 10.1521/psyc.67.3.294.48985. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for axis I DSM-IV. New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1994. [Google Scholar]
- Fischer EP, McSweeney JC, Pyne JM, Williams DK, Naylor AJ, Blow FC, et al. Influence of family involvement and substance use on sustained utilization of services for schizophrenia. Psychiatric Services. 2008;59:902–908. doi: 10.1176/ps.2008.59.8.902. [DOI] [PubMed] [Google Scholar]
- Garnick DW, Horgan CM, Chalk M. Performance measures for alcohol and other drug services. Alcohol Research and Health. 2006;29:19–26. [PMC free article] [PubMed] [Google Scholar]
- Guydish J, Werdegar D, Sorensen JL, Clark W, Acampora A. Drug abuse day treatment: A randomized clinical trial comparing day and residential treatment programs. Journal of Consulting and Clinical Psychology. 1998;66:280–289. doi: 10.1037//0022-006x.66.2.280. [DOI] [PubMed] [Google Scholar]
- Harvey CA, Jeffreys SE, McNaught AS, Blizard RA, King MB. The Camden Schizophrenia Surveys. III: Five-year outcome of a sample of individuals from a prevalence survey and the important of social relationships. International Journal of Social Psychiatry. 2007;53:340–356. doi: 10.1177/0020764006074529. [DOI] [PubMed] [Google Scholar]
- Hellemann G, Conner BT, Anglin MD, Longshore D. Seeing the trees despite the forest: Applying recursive partitioning to the evaluation of drug treatment retention. Journal of Substance Abuse Treatment. 2009;36:59–64. doi: 10.1016/j.jsat.2008.03.005. [DOI] [PubMed] [Google Scholar]
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophrenia Bulletin. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Killaspy H, Banerjee S, King M, Lloyd M. Prospective controlled study of psychiatric outpatient nonattendance: Characteristics and outcomes. British Journal of Psychiatry. 2000;176:160–165. doi: 10.1192/bjp.176.2.160. [DOI] [PubMed] [Google Scholar]
- Kreyenbuhl J, Nossel IR, Dixon LB. Disengagement from mental health treatment among individuals with schizophrenia and strategies for facilitating connections to care: A review of the literature. Schizophrenia Bulletin. 2009;35(4):696–703. doi: 10.1093/schbul/sbp046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruse GR, Rohland BM, Wu X. Factors associated with missed first appointments at a psychiatric clinic. Psychiatric Services. 2002;53:1173–1176. doi: 10.1176/appi.ps.53.9.1173. [DOI] [PubMed] [Google Scholar]
- Lash SJ. Increasing participation in substance abuse aftercare treatment. American Journal on Drug Abuse. 1998;24:31–36. doi: 10.3109/00952999809001697. [DOI] [PubMed] [Google Scholar]
- Lash SJ, Blosser SL. Increasing adherence to substance abuse aftercare group therapy. Journal of Substance Abuse Treatment. 1999;16:55–60. doi: 10.1016/s0740-5472(98)00015-4. [DOI] [PubMed] [Google Scholar]
- Lehman AF. Evaluating Quality of Life for Persons with Severe Mental Illness: Assessment toolkit. Cambridge, Massachusetts: The Evaluation Center at Health Services Research Institute; 1995. [Google Scholar]
- Lehman AF, Dixon LB, Kernan E, DeForge BR, Postrado LT. A randomized trial of assertive community treatment for homeless persons with severe mental illness. Archives of General Psychiatry. 1997;54:1038–1043. doi: 10.1001/archpsyc.1997.01830230076011. [DOI] [PubMed] [Google Scholar]
- McCaul ME, Svikis DS, Moore RD. Predictors of outpatient treatment retention: Patient versus substance use characteristics. Drug and Alcohol Dependence. 2001;62:9–17. doi: 10.1016/s0376-8716(00)00155-1. [DOI] [PubMed] [Google Scholar]
- McConnaughy EA, DiClemente CC, Prochaska JO, Velicer WF. Stages of change in psychotherapy: A follow-up report. Psychotherapy. 1989;26:494–503. [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behaviors. New York: Guilford Press; 1991. [Google Scholar]
- Miner CR, Rosenthal RN, Hellerstein DJ, Muenz LR. Prediction of compliance with outpatient referral in patients with schizophrenia and psychoactive substance use disorders. Archives of General Psychiatry. 1997;54:706–712. doi: 10.1001/archpsyc.1997.01830200030005. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Bennett M, Kushner MG. Epidemiology of substance use disorders among persons with chronic mental illnesses. In: Lehman AF, Dixon LB, editors. Double jeopardy: chronic mental illness and substance use disorders. Vol. 3. Longhorne, PA: Harwood Academic Publishers; 1995. pp. 9–25. [Google Scholar]
- Mueser KT, Glynn SM, Cather C, Zarate R, Fox L, Feldman J, et al. Family intervention for co-occurring substance use and severe psychiatric disorders: Participant characteristics and correlates of initial engagement and more extended exposure in a randomized controlled trial. Addictive Behaviors. 2009;34:867–877. doi: 10.1016/j.addbeh.2009.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagelkerke N. A note on a general definition of the coefficient of determination. Biometrika. 1991;78:691–692. [Google Scholar]
- Nidecker M, Bennett ME, Gjonbalag-Marovic S, Rachbeisel J, Bellack AS. Relationships among motivation to change, barriers to care, and substance-related negative consequences in people with dual disorders. Journal of Dual Diagnosis. 2009;5(–4):375–391. [Google Scholar]
- Nidecker M, DiClemente C, Bennett ME, Bellack AS. Application of the Transtheoretical Model of change: psychometric properties of leading measures in patients with co-occurring drug abuse and severe mental illness. Addictive Behaviors. 2008;33(8):1021–1030. doi: 10.1016/j.addbeh.2008.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosé M, Barbui C, Tansella M. How often do patients with psychosis fail to adhere to treatment programmes? A systematic review. Psychological Medicine. 2003;33:1149–1160. doi: 10.1017/s0033291703008328. [DOI] [PubMed] [Google Scholar]
- O'Brien A, Fahmy R, Singh SP. Disengagement from mental health services. Social Psychiatry and Psychiatric Epidemiology. 2009;44:558–568. doi: 10.1007/s00127-008-0476-0. [DOI] [PubMed] [Google Scholar]
- Opler LA, Kay SR, Lindenmayer JP, Fiszbein A. Structured Clinical Interview for the Positive and Negative Syndrome Scale. New York: Multi-Health Systems; 1992. [Google Scholar]
- Pantalon MV, Swanson AJ. Use of the University of Rhode Island Change Assessment to measure motivational readiness to change in psychiatric and dually diagnosed individuals. Psychology of Addictive Behavior. 2003;17:91–97. doi: 10.1037/0893-164x.17.2.91. [DOI] [PubMed] [Google Scholar]
- Peeters FP, Bayer H. “No-show” for initial screening at a community mental health centre: Rate, reasons, and further help-seeking. Social Psychiatry and Psychiatric Epidemiology. 1999;34:323–327. doi: 10.1007/s001270050151. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Diclemente CC, Norcross JC. In search of how people change: Applications to addictive behaviors. In: Marlatt AG, VandenBos GR, editors. Addictive behaviors: Readings on etiology, prevention, and treatment. Washington, DC: American Psychological Association; 1992. pp. 671–696. [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH post-treatment drinking outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Journal of the American Medical Association. 1990;264:2511–2518. [PubMed] [Google Scholar]
- Sekerka R, Goldsmith RJ, Brandewie L, Somoza E. Treatment outcome of an outpatient treatment program for dually-diagnosed veterans: The Cincinnati Veterans Affairs Medical Center. Journal of Psychoactive Drugs. 1999;31:85–94. doi: 10.1080/02791072.1999.10471729. [DOI] [PubMed] [Google Scholar]
- Siqueland L, Crits-Christoph P, Gallop B, Gastfriend D, Lis J, Frank A, et al. Who starts treatment: engagement in the NIDA collaborative cocaine treatment study. American Journal on Addiction. 2002;11:10–23. doi: 10.1080/10550490252801602. [DOI] [PubMed] [Google Scholar]
- Smith TE, Burgos J, Dexter V, Norcott J, Pappas SV, Shuman E, et al. Best practices for improving engagement of clients in clinic care. Psychiatric Services. 2010;61(4):343–345. doi: 10.1176/ps.2010.61.4.343. [DOI] [PubMed] [Google Scholar]
- Swanson AJ, Pantalon MV, Cohen KR. Motivational interviewing and treatment adherence among psychiatric and dually diagnosed clients. Journal of Nervous and Mental Disease. 1999;187:630–635. doi: 10.1097/00005053-199910000-00007. [DOI] [PubMed] [Google Scholar]
- Swartz MS, Wagner HR, Swanson JW, Stroup TS, McEvoy JP, Canive JM, et al. Substance use in persons with schizophrenia: Baseline prevalence and correlates from the NIMH CATIE study. Journal of Nervous and Mental Disease. 2006;194:164–172. doi: 10.1097/01.nmd.0000202575.79453.6e. [DOI] [PubMed] [Google Scholar]
- Winokur G, Turvey C, Akiskal H, Coryell W, Solomon D, Leon A, et al. Alcoholism and drug abuse in three groups - bipolar I, unipolars, and their acquaintances. Journal of Affective Disorders. 1998;50:81–89. doi: 10.1016/s0165-0327(98)00108-6. [DOI] [PubMed] [Google Scholar]
- Wolpe PR, Gorton G, Serota R, Sanford B. Predicting compliance of dual diagnosis inpatients with aftercare treatment. Hospital and Community Psychiatry. 1993;44:45–49. doi: 10.1176/ps.44.1.45. [DOI] [PubMed] [Google Scholar]
- Ziedonis DM, Trudeau K. Motivation to quit using substances among individuals with schizophrenia: Implications for a motivation-based treatment model. Schizophrenia Bulletin. 1997;23:229–238. doi: 10.1093/schbul/23.2.229. [DOI] [PubMed] [Google Scholar]