Abstract
Background:
Adoption of digital images for pathological specimens has been slower than adoption of digital images in radiology, despite a number of anticipated advantages for digital images in pathology. In this paper, we explore the factors that might explain this slower rate of adoption.
Materials and Method:
Semi-structured interviews on barriers and facilitators to the adoption of digital images were conducted with two radiologists, three pathologists, and one pathologist's assistant.
Results:
Barriers and facilitators to adoption of digital images were reported in the areas of performance, workflow-efficiency, infrastructure, integration with other software, and exposure to digital images. The primary difference between the settings was that performance with the use of digital images as compared to the traditional method was perceived to be higher in radiology and lower in pathology. Additionally, exposure to digital images was higher in radiology than pathology, with some radiologists exclusively having been trained and/or practicing with digital images. The integration of digital images both improved and reduced efficiency in routine and non-routine workflow patterns in both settings, and was variable across the different organizations. A comparison of these findings with prior research on adoption of other health information technologies suggests that the barriers to adoption of digital images in pathology are relatively tractable.
Conclusions:
Improving performance using digital images in pathology would likely accelerate adoption of innovative technologies that are facilitated by the use of digital images, such as electronic imaging databases, electronic health records, double reading for challenging cases, and computer-aided diagnostic systems.
Keywords: Computer-aided diagnostic, electronic health records, informatics, pathology, soft copy
INTRODUCTION
Digital imaging has been accepted as the standard for clinical care for most of the current radiology practice in the United States for most modalities.[1] At some institutions, radiologists are trained exclusively using digital images and several radiology departments are completely digital. In comparison, the use of digital images for pathological specimens is still relatively rare in current practice. Nevertheless, many pathologists predict that digital images will eventually become standard practice. Anticipated advantages of digital slides over glass slides include easier long-term storage, access to historical images, comparison with alternative images of the same specimen with different stains or immunoreagents, collaborations with colleagues for challenging cases, and use of computer-aided diagnostic (CAD) support.[2]
In this work, we explored the factors that might explain the slower adoption rate of digital images in pathology as compared to radiology. We have identified possible lessons learned from radiology for pathology, and compared our insights with findings from prior research on adoption of innovative health information technologies.
MATERIALS AND METHOD
We conducted fix 1 hour semi-structured interviews on barriers and facilitators to the use of digital images in clinical practice between February and September 2010.The interviewees were selected as a convenience sample from personal networks and represent four different healthcare organizations in the Midwest and one in the United Kingdom. They were as follows.
Radiology MD who specializes in mammography and was in charge of implementing digital imaging over the last 3years; she has exclusively used digital images in her practice for a year,
Radiology RN who specializes in lung disorders and has used digital imaging exclusively in her practice for over 3 years,
Pathology MD who specializes in hematopathology, practices with glass slides, and has conducted research on digital pathology for 3 years,
Pathology MD/PhD who specializes in veterinary medicine, practices with glass slides, and has taught residents using both glass slides and digital images for the last 2 years,
Pathology MD/MS researcher who specializes in gastrointestinal cancer and conducts research on digital pathology, and Pathologist's Assistant/PhD who specializes in breast cancer and has created an online curriculum for medical and dental students.
Barriers and facilitators to adoption of digital images were identified via standard qualitative techniques that iteratively identify patterns bottom up from the interview data while also being guided top-down by a conceptual framework.[3] During analysis, investigators highlighted areas of disagreement, which were then resolved via group discussion. Data collection and analysis was guided by a theoretical framework of human factors concepts[4] developed for research on barriers and facilitators to the use of computerized clinical reminders for physicians treating patients with infectious diseases in the outpatient setting [Figure 1]. During analysis, the primary themes that emerged were performance, workflow-efficiency, infrastructure, integration with other software, and exposure to digital images.
Figure 1.
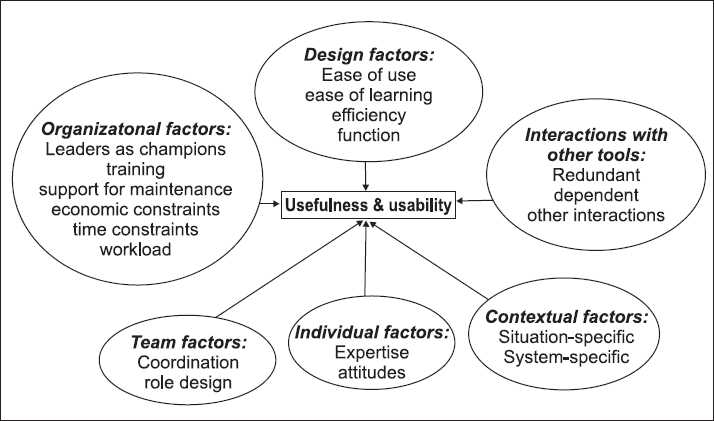
Theoretical framework of factors impacting the usefulness and usability of new technologies
After analysis was completed, one final iteration on the analytic findings was conducted following an explicit comparison with findings from prior research. Specifically, the categories, barriers, and facilitators were compared with prior categories, barriers, and facilitators to adoption of three other health information technologies: the electronic Intensive Care Unit,[5,6] Bar Code Medication Administration,[7] and computerized clinical reminders.[8]
RESULTS
Table 1 details the findings regarding barriers and facilitators to the use of digital images in radiology and pathology, respectively. The most striking difference is the perception of relative performance using digital images as compared to the traditional approaches: a hard film copy of an x-ray image in radiology, and glass slides and a microscope in pathology. The two practitioners in radiology felt that performance was improved using the digital images. The improvement was largely attributed to the higher resolution quality of the images, as well as easier manipulation of the image. These perceptions are corroborated by the findings of a large study funded by the National Cancer Institute, the Digital Mammographic Imaging Screening Trial (DMIST), for particularly challenging populations: women with extremely dense breasts, women under 50 years old, and in premenopausal or perimenopausal women.[9] In contrast, the three pathologists, but not the pathologist's assistant, felt that diagnostic performance was inferior using digital images. Although no rigorous, large-scale studies have been conducted in pathology regarding performance, one publication suggests that the common perception among pathologists is that performance is reduced using a digital image.[10] Note that these findings do not include the use of CAD support, which require the use of digital images and are anticipated to improve diagnostic performance.
Table 1.
Barriers and facilitators to digital images in radiology and pathology
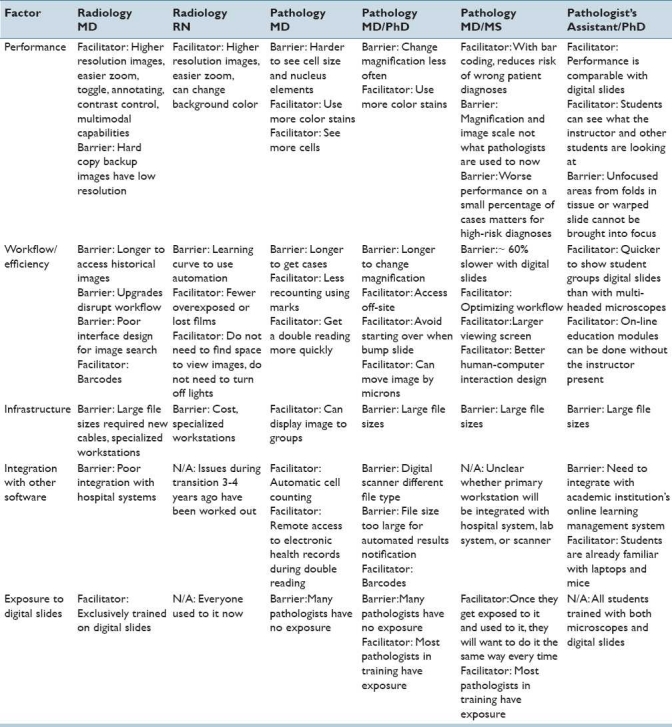
In both radiology and pathology, there seems to be the potential for both efficiency gains and losses following a transition to soft copy reading. With soft copies, there is the potential for a workflow transition from batch processing of multiple images to ‘just in time’ availability of individual soft copy images. Two studies from radiology support these impressions. The first, an observational time motion study,[11] found that soft copy interpretation takes longer to read primarily due to longer computer manipulation times (bringing up the images, enlarging them to 100% resolution, and panning through the image) and increased time gazing at the image. The second study[12] found that the overall productivity of the radiologists increased 10-30% after the conversion, likely due to more rapid access to old images and reports, elimination of interruptions by personnel looking for films, better ability to distribute the workload across all radiologists, and constant displays of unread examinations making remaining workload more observable. While the overall efficiency was increased, some efficiency losses were identified in one paper following the transition due to a longer time reading each case, slower image retrieval time from the database, and needing breaks every 40-50 min rather than every 1-2 h. The fatigue was presumed to be higher with the digital slides due to relatively decreased brightness of the monitors (true at that time, but not with newer hardware), monitor flicker, small cursor, and active role in image manipulation. On the other hand, as sharing radiologic images has now become feasible via direct electronic exchange even with large files,[13] there appears to be a greater use of radiology services.[14]
Most of the other findings from Table 1 were similar in radiology and pathology, with the exception of more widespread exposure to digital images in radiology as compared to pathology. The finding that trainees are more exposed to digital images in pathology is supported by the results of a recent survey; of those using a digital system, 72% are using it for education and/or training.[15]
The findings from Table 1, and particularly the groupings and factor labels, were informed by a comparison with barriers and facilitators to adoption of other health information technologies. The methodologies and detailed findings from studies are detailed elsewhere for the electronic Intensive Care Unit (e-ICU),[5,6] Bar Code Medication Administration (BCMA),[7] and computerized clinical reminders (CCRs).[8] An overview of the findings from these prior studies is provided in Table 2.
Table 2.
Barriers and facilitators to health information technologies
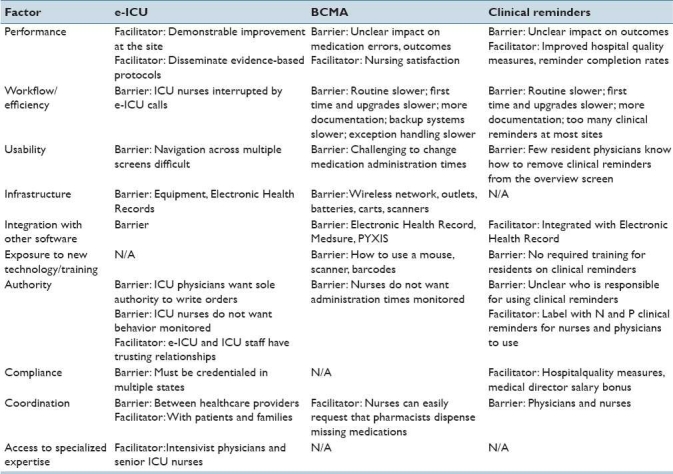
There are some interesting differences between Tables 1 and 2, including that none of these technologies had definitive evidence of improving performance in the published literature, all of them incurred efficiency costs, were perceived as having poor usability, and were perceived to reduce the authority for making clinical decisions. Overall, these summary findings suggest that if the use of digital images in pathology could be clearly demonstrated to improve diagnostic performance, overall there might be fewer, or at least more tractable, barriers to adoption than for these three other health information technologies.
An important limitation of this work is that the pathologists who were interviewed had no personal experience implementing or using digital images in a clinical setting, unlike the radiology practitioners and users of the other health information technologies. Although, to our knowledge, there are few pathologists with extensive and long-term experience using soft copies for clinical purposes, the findings are likely to be biased. First, it is possible that the pathologists might be relatively poorly calibrated to the relative importance of the reported barriers and facilitators during adoption. Similarly, the informatics systems, scanning technologies, image repository software products, connectivity speed, and hardware are rapidly changing, and therefore perceptions of barriers and facilitators may quickly become outdated, particularly in relation to identifying lessons learned from the practice of radiology for pathology from a decade ago. In addition, there are likely barriers and facilitators to adoption about which they are unaware. For example, additional barriers which were not mentioned likely include: (1) infrastructure barrier: access to digital scanners to create the digital images is limited and mostly for research or quality assessment purposes in many institutions, (2) software integration barrier: although a supplement to the Digital Imaging and Communications in Medicine (DICOM) standard has recently been approved for whole-slide images (Supplement 145), it has not yet been widely adopted for distributing and viewing any kind of medical image regardless of the origin, although a working group (DICOM WG-26) has been working to increase the potential for widespread adoption, and (3) regulatory barrier: digital-based systems will likely need to receive Food and Drug Administration (FDA) approval prior to use in any United States clinical setting. Similar, prior research in transitioning to soft copy reading in radiology identified factors that did not emerge as themes during analysis, but they might be important. Factors that were identified on a survey as important for improving the effectiveness of soft copy reading room designs in radiology included room lighting, number of monitors and their resolution, size and brightness, chair design (lumbar support, wheels, swivel, frequent height adjustment), compartmentalization of the reading room, and availability of the hospital/radiology information system at the workstation.[16] Finally, the pathologists represent a wide variety of clinical domains, and therefore likely have different needs, particularly with respect to the scale and dimensionality of the abnormalities that they are detecting.
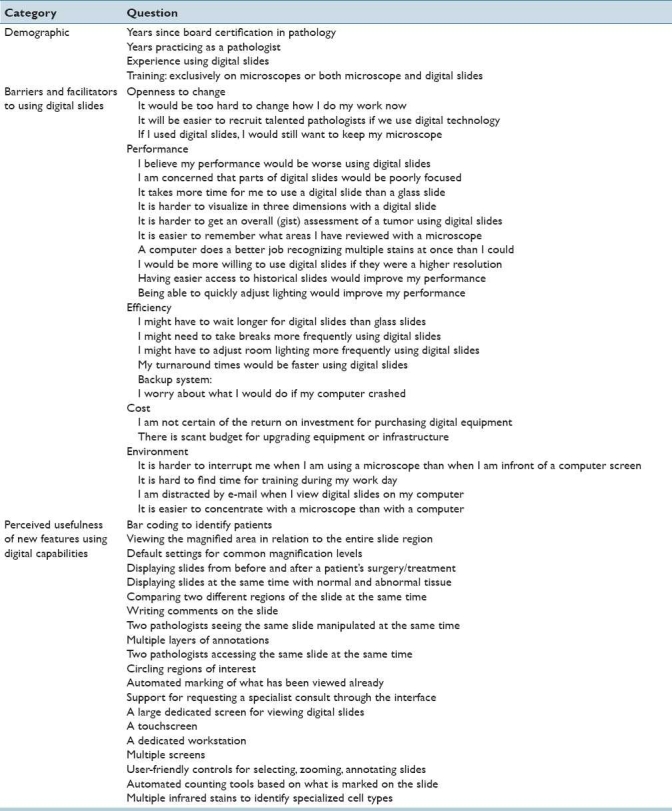
Finally, another limitation of this study is that the interviewees represent a small, convenience sample of participants from three organizations. The pathologists and the pathologist's assistant are likely biased toward the adoption of digital images since they have some experience using them, which is not representative of pathologists in general. We believe that we have partially addressed this limitation by comparing the findings with barriers and facilitators to adoption of other transformative health information technologies that are farther along the adoption curve. In future research, we intend to further triangulate these findings with a survey from a larger, more representative group of pathologists. In Table 3, we have provided the survey items that we have piloted with five pathologists recruited during a recent pathology informatics conference. Most responses are on the same 1-7 Likert scale from “strongly disagree” to “strongly agree.” In addition to demographic questions about experience in general and with the use of digital images, the questions represent (1) barriers and facilitators to the use of digital slides, and (2) perceived usefulness of new features using digital capabilities.
Table 3.
Survey questions
CONCLUSIONS
This work represents findings from an initial exploration of the factors that might be important for adopting digital imaging in pathology as it becomes more widespread. Future research is planned regarding how to increase the effectiveness of the technology and accelerate adoption based upon these findings and additional studies.
Overall, the primary insights from this exploratory study are that the performance factor on challenging high-risk diagnostic cases might be the most important barrier to the adoption of digital slides in clinical settings, that digital slides are being adopted more quickly in educational than clinical settings, and that barriers to adoption of digital slides are anticipated to be easier to address than for three other transformative health information technologies. These insights resonate with the findings from prior research detailed in Table 2 in that demonstrable benefits to performance at either an individual or organizational level or unique access to specialized expertise likely increase the willingness to adopt a new technology. It is possible that the performance barrier could be addressed in pathology by providing more images at more magnification levels, thereby more closely matching what is possible by using the fine focus adjustment on a microscope. Doing this would require interaction features to easily allow this as well as significantly larger digital storage space. Alternatively, new technologies such as iPad applications that magnify digital images with high resolutions or computer-aided diagnostic (CAD) support might dramatically increase performance.[17–23]
Interestingly, after our first interview with the first pathologist, we had identified potential barriers to adoption that we thought might be difficult to address that appeared more tractable after the other interviews. For example, supporting task immersion by having a dark surrounding field and reducing interruptions seemed less important based on the other interviews. Similarly, keeping roles the same before and after the technology and using the same workflow strategies such as hanging protocols seemed to be less critical.
As many have pointed out, there is often a first-time adoption cost that is higher than after a system has been implemented. Our findings provide support for this pattern, particularly with relation to infrastructure costs and integration with other software.
Finally, there seemed to be a sense of inevitability about the use of digital images for routine clinical practice in both radiology and pathology. In particular, training and recruiting talent seemed to encourage more digital image use in that trainees want to be perceived as being current on the latest technological developments when they enter the workforce.
In summary, the slower adoption rate for digital images in pathology appears to be primarily explained by a perception of decreased individual performance with their use for challenging high-risk diagnoses. On the other hand, there seems to be a sense of inevitability regarding eventual adoption of digital images as a standard for clinical practice. Improving performance using digital images in pathology would likely accelerate adoption of digital images as well as other innovative technologies that require the use of digital images, including electronic imaging databases, electronic health records, double reading as a best practice for challenging cases, and Computer-Aided Diagnostic (CAD) systems.
Acknowledgments
The project described was supported in part by Award Number R01CA134451 from the National Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute, or the National Institutes of Health. We thank the interviewees for sharing their time and expertise, Dr. Lisa Lee for reviewing the proposed survey questions in Table 3, and Dr. Treanor Darren, Dr. Khan Siddiqui, and two anonymous reviewers for helpful suggestions on an earlier draft of this paper.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp? 2011/1/2/1/74940
REFERENCES
- 1.Siegel EL. Current state of the art and future trends. In: Siegel EL, Kolodner RM, editors. Filmless Radiology. New York: NY:Springer-Verlag; 1999. pp. 3–20. [Google Scholar]
- 2.Barbareschi M, Demichelis F, Forti S, Dalla Palma P. Digital Pathology: Science Fiction? Int J Surg Pathol. 2000;8:261–3. doi: 10.1177/106689690000800401. [DOI] [PubMed] [Google Scholar]
- 3.Spradley JP. The Ethnographic Interview. CA: Wadsworth Group/Thomson Learning. 1979 Belmont, CA: Wadsworth Group/Thomson Learning. [Google Scholar]
- 4.Patterson ES, Nguyen AD, Bozzette SA, Gomes JO, Asch SM. Comparing findings from cognitive engineering evaluations.Proceedings of the Human Factors and Ergonomics Society 47th annual meeting. 2003 Oct 13-17;:483–7. Denver, CO. [Google Scholar]
- 5.Anders S, Patterson ES, Woods DD, Ebright P. Projecting Trajectories for a New Technology Based on Cognitive Task Analysis and Archetypal Patterns: The Electronic ICU. Proceedings of the 8th Annual NDM Conference. 2007 Asilomar, CA. [Google Scholar]
- 6.Anders S, Patterson ES, Woods DD, Schweikhart S. Proceedings of the HFES 52nd Annual Meeting. New York, NY: 2008. Shifts in functions of a new technology over time: An analysis of logged electronic Intensive Care Unit (e-ICU) interventions. [Google Scholar]
- 7.Patterson ES, Rogers ML, Render ML. Fifteen best practice recommendations to improve the effectiveness of bar code medication administration. JtComm J QualSaf. 2004;30:355–65. doi: 10.1016/s1549-3741(04)30041-9. [DOI] [PubMed] [Google Scholar]
- 8.Patterson ES, Doebbeling BN, Fung CH, Militello L, Anders S, Asch SM. Identifying barriers to the effective use of clinical reminders: Bootstrapping multiple methods. J Biomed Inform. 2005;38:189–99. doi: 10.1016/j.jbi.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 9.Pisano ED, Gatsonis C, Hendrick E, Yaffe M, Baum JK, Acharyya S, et al. Diagnostic Performance of Digital versus Film Mammography for Breast-Cancer Screening. N Engl J Med. 2005;353:1773–83. doi: 10.1056/NEJMoa052911. [DOI] [PubMed] [Google Scholar]
- 10.Molnar B, Berczi L, Diczhazy C, Tagscherer A, Varga SV, Szende B, et al. Digital slide and virtual microscopy based routine and telepathology evaluation of routine gastrointestinal biopsy specimens. J ClinPathol. 2003;56:433–8. doi: 10.1136/jcp.56.6.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haygood TM, Wang J, Lane D, Galvan E, Neely Atkinson E, Stephens T, et al. Why does it take longer to read digital than film-screen screening mammograms.A partial explanation? J Digit Imaging. 2010;23:170–80. doi: 10.1007/s10278-009-9177-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Siegel EL, Diaconis JN, Pomerantz S, Allman R, Briscoe B. Making filmless radiology work. J Digit Imaging. 1995;8:151–5. doi: 10.1007/BF03168713. [DOI] [PubMed] [Google Scholar]
- 13.Mendelson DS, Bak PR, Menschik E, Segel E. Informatics in radiology: Image exchange—IHE and the evolution of image sharing. RadioGraphics. 2008;28:1817–33. doi: 10.1148/rg.287085174. [DOI] [PubMed] [Google Scholar]
- 14.Siegel EL, Reiner BI, Khan MS. Ten filmless years and ten lessons: A 10th-anniversary retrospective from the Baltimore VA Medical Center. J Am CollRadiol. 2004;1:824–33. doi: 10.1016/j.jacr.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 15.Adoption Trends in Digital Pathology. [Last accessed on 2010 Jul 22];Laboratory Economics. 2010 5:6. Available from: http://labsoftnews.typepad.com/lab_soft_news/2010/06/adoption-trends-in-digital-pathology.html . [Google Scholar]
- 16.Siegel E, Reiner B, Abiri M, Chacko A, Morain R, Ro DW, et al. The filmless radiology reading room: A survey of established picture archiving and communication system sites. J Digit Imaging. 2000;13:22–3. doi: 10.1007/BF03167618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gurcan M, Boucheron L, Can A, Madabhushi A, Rajpoot N, Yener B. Histopathological image analysis: A review. IEEE Rev Biomed Eng. 2009;2:147–71. doi: 10.1109/RBME.2009.2034865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ruiz A, Kong J, Ujaldon M, Boyer K, Saltz J, Gurcan M. Pathological image segmentation for neuroblastoma using the GPU. 2008 IEEE IntSymp Biomed Imaging. 2008;1(4):296–9. [Google Scholar]
- 19.Sertel O, Kong J, Catalyurek U, Lozanski G, Saltz J, Gurcan M. Histopathological Image Analysis using Model-based Intermediate Representations and Color Texture: Follicular Lymphoma Grading. J Signal Process Syst. 2009;2:147–71. [Google Scholar]
- 20.Sertel O, Kong J, Catalyurek U, Lozanski G, Shana'ah A, Saltz J, Gurcan MN. Texture classification using nonlinear color quantization: Application to histopathological image analysis. Las Vegas. 2008 NV: IEEE ICASSP; 2008. [Google Scholar]
- 21.Sertel O, Kong J, Lozanski G, Shimada H, Catalyurek U, Saltz J, Gurcan MN. Texture characterization for whole-slide histopathological image analysis: Applications to neuroblastoma and follicular lymphoma. Pittsburg. 2007 PA:APIII. [Google Scholar]
- 22.Sertel O, Kong J, Shimada H, Catalyurek U, Saltz JH, Gurcan MN. Computer-aided prognosis of neuroblastoma: Classification of stromal development on whole-slide images - art.no. 69150P. Med Imaging. 2008;6915:P9150. doi: 10.1016/j.patcog.2008.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sertel O, Kong J, Shimada H, Catalyurek UV, Saltz JH, Gurcan MN. Computer-aided prognosis of neuroblastoma on whole-slide images: Classification of stromal development. Pattern Recognit. 2009;42:1093–103. doi: 10.1016/j.patcog.2008.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]


