Abstract
The aim of this study was to assess the image display of a web-based teleradiology system that uses a common web browser and has no need of proprietary applets, plug-ins, or dedicated software for DICOM display. The teleradiology system (TS) is connected to the Internet by ADSL and to radiological modalities using the DICOM standard with TCP/IP. Images were displayed on a PC through Internet connection with the remote TS using a common web browser. MS lesion number and volume in T1- and T2-weighted images (T1w and T2w, respectively) of 30 brain MR studies were quantified using both the TS and a conventional software. Wilcoxon signed ranks test and intraclass correlation coefficient (ICC) were used to assess the variability and concordance between intra- and inter-observer and TS and conventional DICOM viewer, setting significance at p < 0.05. No significant differences in T1w and T2w volumes between the TS and the conventional software were found by either operator. The ICC results showed a high level of inter-operator agreement in volume estimation in T1w and T2w images using the two systems. Quantitative assessment of MS lesion volumes in T1w and T2w images with a user interface of a teleradiology system that allows the consultation by means of a common web browser, without the need for proprietary plug-ins, applets, or dedicated software for DICOM display showed no significant differences from, and almost complete agreement with, conventional DICOM viewers.
Key words: Computer applications-teleradiology, clinical image viewing, image distribution, internet, medical displays, web technology, multiple sclerosis
Introduction
Magnetic resonance (MR) imaging is currently used in patients with multiple sclerosis (MS) for diagnosis, to assess disease progression and to depict active lesions. MR examination should be performed possibly by experienced neuroradiologists. In addition, quantitative assessment of MS lesions, when possible, may be useful, particularly in multicentric scientific studies, in which neuroimaging represents a tool to measure the outcome1,2. However, in several clinical settings a neuroradiologist, is not available and the quantitative assessment of MR exams cannot be performed because it is time-expensive, it requires advanced techniques and trained personnel.
Improvements in information technology have led to a rapid development of teleradiology, the electronic transmission of radiological images from one location to another for a variety of purposes, mainly interpretation/consultation and scientific studies3–5. Teleradiology may be useful in the above-mentioned cases in which an experienced neuroradiologist is not available for second opinion or for centralizing image analysis.
The research in teleradiology is focused mainly on three objectives. The first objective is to reduce the amount of memory required for the encoding of radiological images, preserving information, through the enhancement of the Digital Images and Communications in Medicine (DICOM) 3.0 standard6. The second objective is to increase the transmission rate of the networks. Although there is a great distribution of broadband Internet connections in western countries, the transmission rates varies in relation to regions and may be suboptimal in non-western countries7.
The third objective is to improve the display of DICOM images. Web-based teleradiology systems use common web browsers that are present in all personal computers (PCs), although plug-ins, applets, or more advanced software are needed to display DICOM images. Allowing all PCs to display images in an easy, secure, and reliable way is crucial for image distribution because dedicated workstations are expensive and available only in the radiological departments with a suitable budget, which is not always the case.
Image compression, Internet connection, and standard file format may be useful to reach these objectives. These three concepts have together been implemented in a low-cost solution for the remote consultation of images that uses a common web browser without the need for applets, plug-ins, or dedicated software for DICOM display. This solution may be of great interest in non-western countries, or in remote sites where broad-band connections are unavailable, for second opinion, or centralized quantification.
The aim of this study is to quantitatively assess MR examination of MS patients by using a teleradiology system. The majority of the previous studies have focused on specific aspects of teleradiology, such as image compression algorithms8–20, transmission rates and architecture5,21, ergonomics, patient management and practical/economic/legal aspects 22,23, but, to our knowledge, none of them assessed teleradiology user interface in MR of MS patients.
This paper focuses on the last of these aspects, aiming to assess the quantification of multiple sclerosis (MS) lesions in brain magnetic resonance (MR) studies using the above-mentioned teleradiology system, in comparison with that of a professional DICOM viewer.
Materials and methods
Image Display Systems
The teleradiology system (TS; Dilogix, Italy) is installed in the radiology department and is connected to radiological modalities (i.e., computed tomography (CT), magnetic resonance imaging (MR), digital radiology (DR), ultrasound imaging) or a picture archiving and communicating system (PACS) directly or through the local radiology network. Images are sent from these modalities to the TS using the DICOM standard with Transmission Control Protocol/Internet Protocol (TCP/IP), the same procedure used for transferring images to the local PACS. Images are stored in the TS in non-compressed DICOM format.
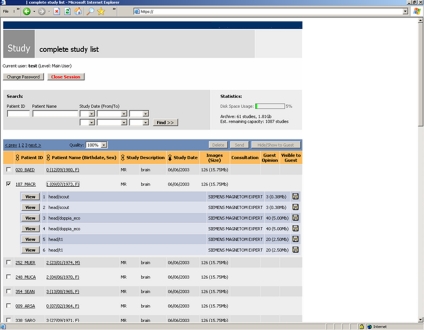
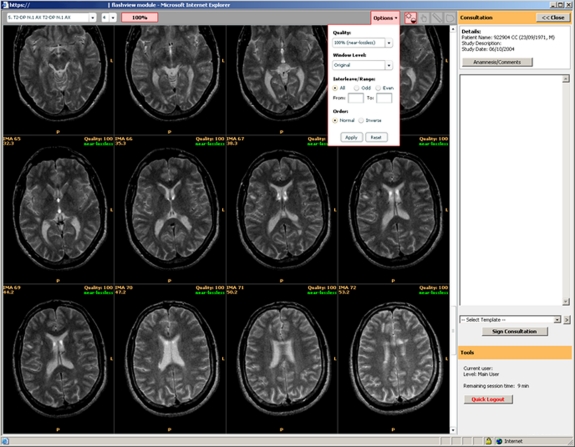
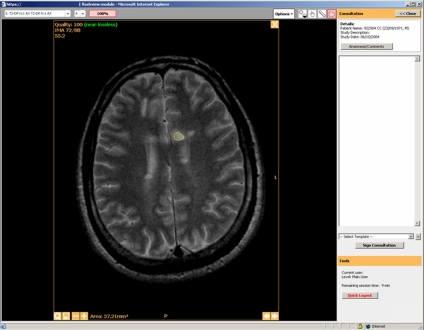
TS software is programmed in C language integrated with Flash Player Adobe®. TS is connected to the Internet through at least an asymmetric digital subscriber line (ADSL). Images can be displayed in a remote PC through Internet connection with the TS. When a study is accessed, TS produces a compressed copy of the requested images using the 8-bit Joint Photographic Expert Group (JPEG) algorithm24,25. Compression reduces memory requirements, thereby allowing rapid visualization even using a normal dial-up connection (with a speed of under 56 kb/s). In other words, whereas ADSL connection between TS and Internet is needed, even a normal dial-up connection is necessary to connect to TS for image display from the remote PC. Using a standard 8-bit lossless JPEG compression with a quality factor of 95% and a standard 2 Mb/s ADSL connection, 44 MR images of the brain 256 matrix were visualized in almost 30 s. Images are displayed using a common web browser without proprietary plug-ins, applets, or dedicated software for DICOM. Once logged in, consultants select the patient’s study (Figs. 1, 2, 3) and series of images are displayed directly in the web browser. Images are displayed with the same window settings used by the technologist in the scanner console. TS allows the operator to adjust brightness and contrast. When applicable, upon request, new grayscale window settings can be set; in this case, DICOM images with new window settings are compressed and re-displayed in the web browser. Measurement tools and DICOM information are available. Previous examinations can be displayed in a separate window. A box allows the operator to write reports, which are sent as encrypted e-mails to the radiology department, with a feedback system ensuring correctness of transmission. Reports are automatically archived and linked to patient’s study. Security authentication and encryption using 128-bit secure socket layer (SSL) technology are implemented, and each access to the system is detected and recorded.
Fig 1.
Teleradiology system user interface: patient list with the examination sequences.
Fig 2.
Teleradiology system user interface: display of a T2-weighted MR sequence of a patient with MS.
Fig 3.
Teleradiology system user interface: segmentation of a MS lesion.
The other systems for DICOM display was JIM (Xinapse, Northants, U.K.), a radiological image (DICOM, Analyze, UNC) viewer and analysis tool written in Java, and designed for MS lesion quantification.
Assessment of the Software
The assessment of these image display systems was carried out using a professional workstation in the analysis laboratory, with an HDSL connection to Internet (2 Mb/s). The computer monitor was a high-resolution, 22″ CRT (cathode ray tube) monitor capable of displaying 2,048 × 1,536 pixels with a dot pitch of 0.24 mm and a refresh rate of 80 Hz. These specifications meet the standards for primary teleradiology interpretation developed by the American College of Radiology3. In addition, the standard quality procedures of the analysis laboratory included the calibration of the display systems for DICOM images. In the workstation, Internet Explorer 6.0 (Microsoft, IL, USA) web browser was also present.
JIM viewer was installed in the workstation which was also utilized for image display with the TS.
For the purpose of the current study, the TS was installed in a radiology department situated 1.1 miles from the image analysis laboratory. The radiology department and laboratory both had a 2 Mb/s ADSL Internet connection. In the assessment with TS, image display and lesion segmentation were done with maximum lossless JPEG image quality (>95%). Due to the lack of absolute signal references, optimal grayscale values for assessing MS lesions were set arbitrarily on the MR console, but operators were free to adjust window settings.
To summarize, the same above-mentioned workstation was used for the assessment of TS and JIM. Images were displayed on the PC in two ways: by means of Internet link-up between the laboratory and the remote TS; or by the loading of local DICOM images onto JIM.
MR Studies
Thirty MR studies of patients with MS were randomly selected from a clinical study database. This database included brain MR studies performed on relapsing–remitting MS patients with varying degrees of neurological impairment and an Expanded Disability Status Scale (EDSS) score >326,27. This study was approved by the local ethics committee and the patients involved gave their informed consent. From each MR study, two series of 44 images (slice thickness 3 mm; slice gap 0 mm; FOV, 250 mm; image matrix, 256 × 256), respectively, T1w (TR/TE, 600/15 ms) and T2w (TR/TE, 2,500/87 ms), were utilized for the present study. MR images were anonymized, randomized, and stored in the TS hard disk in the radiology department and in the workstation in the laboratory.
Lesion Quantification
Two trained operators, both radiologists with more than 2 years experience in lesion volume quantification (Operator 1, 4 years and Operator 2, 2.5 years), quantified lesion in T1- and T2-weighted image series (T1w and T2w, respectively). The lesions were assessed in number and size.
Lesions in T1w images were identified as hypointense areas (black holes) with respect to normal-appearing white matter. Lesions in T2w images were identified as hyperintense areas with respect to normal-appearing white matter. T1w and T2w lesion volumes (in cubic millimeters) were obtained through manual segmentation, defining lesion margins with the mouse cursor. Operators were allowed to magnify and scroll images in order to discriminate lesions from partial volumes of ventricles, and to adjust window display settings.
To overcome the problem of potential variability due to the use of different hardware, the operators used the same workstation to link-up with the TS and to carry out measurements using JIM.
Statistical Analysis
Statistical analysis was carried out using the SPSS 11.0.0 package (SPSS Inc, Chicago, IL, USA), using the Wilcoxon signed rank test (U test), two-way intraclass correlation coefficients (ICCs). Statistical significance was set at p < 0.05 with 95% confidence interval (CI).
The measurements of lesion number and volume were obtained in T1w and T2w using two software by two observers. The following analyses were done:
Comparison between software: for each observer, the difference and correlation of the between TS and JIM measurements of T1w and T2w lesion number and volume.
Interobserver variability: for each software (TS and JIM, respectively), the difference and correlation between observers of the measurements of T1w and T2w lesion number and volume.
Results
No error of transmission occurred in any case. MS lesions were distributed in the white matter, mainly paraventricular.
The pooled mean of the number of lesions in T1w images per patient (obtained from both observers and with all methods) was 3.16, ranging from 0 to 21; the mean lesion volume was 265 mm3 (with a standard deviation of 412.92 mm3), ranging from 0 mm3 to 1837 mm3.
The pooled mean of the number of lesions in T2w images per patient (obtained from both observers and with all methods) was 17.87, ranging from 2 to 43; the mean lesion volume was 2,277 mm3 (with a standard deviation of 2097.48 mm3), ranging from 232 mm3 to 10936 mm3.
The results are summarized in Tables 1 and 2.
Table 1.
Wilcoxon Signed Rank Test, Intraclass Correlation Coefficients (ICCs) and 95% Confidence Interval (IC) Between Systems
| Image weighting | Paired samples | Wilcoxon test | ICC | 95% CI of ICC | |
|---|---|---|---|---|---|
| Oper.1 | T1w | JIM1–TS1 | 0.052 | 0.978a | 0.955; 0.99 |
| T2w | JIM1–TS1 | 0.262 | 0.986a | 0.97; 0.993 | |
| Oper. 2 | T1w | JIM2–TS2 | 0.046 | 0.964a | 0.925; 0.982 |
| T2w | JIM2–TS2 | 0.894 | 0.975a | 0.949; 0.988 |
The first column shows the operators and the second column the image weighting of the dataset in which measurements were carried out. The numbers under the software acronyms indicate the operator who performed the measurements. For each operator and image weighting, no significant differences were observed between measurements obtained with each system
aThe ICC was significant in all cases
Table 2.
Wilcoxon Signed Rank Test, Intraclass Correlation Coefficients (ICCs) and 95% Confidence Interval (IC) Between Operators
| Image weighting | Paired samples | Wilcoxon test sig. | ICC | 95% CI of ICC | |
|---|---|---|---|---|---|
| Oper. 1 vs Oper. 2 | T1w | JIM1–JIM2 | 0.361 | 0.946a | 0.888; 0.974 |
| TS1–TS2 | 0.876 | 0.928a | 0.856; 0.965 | ||
| T2w | JIM1–JIM2 | 0.001b | 0.908a | 0.712; 0.963 | |
| TS1–TS2 | 0.012b | 0.909a | 0.779; 0.96 |
The first column shows the operators and the second column the image weighting of the dataset in which measurements were carried out. The numbers under the software acronyms indicate the operator who performed the measurements. No significant differences emerged between the operators’ results when measurements were performed in T1w images
aThe ICC was significant in all cases
bSignificant differences between operators were observed in volume measurements in T2w images
The comparison between software showed, for each operator, no significant differences in T1w or T2w volumes were observed between TS and JIM (p > 0.05).
These results show a high intra-observer agreement in volume estimation of lesions in T1w and T2w images using the two systems (p < 0.05).
The inter-operator analysis showed no significant differences in T1 volumes were observed between the two operators in any case (p > 0.05). Significant differences in lesion volumes in T2w images were observed between the two operators in all cases (p < 0.05). These results show inter-operator agreement in volume estimation in T1w and T2w images using the two systems (p < 0.05).
Discussion
The TS transmits JPEG-compressed images. Compression algorithms are categorized into two groups according to their capacity to preserve image information. With “lossless” algorithms, image compression up to 2/1 or 3/1 can be obtained without loss of information. Conversely, with “lossy” algorithms, higher compression ratios are achieved, but against that, images are irreversibly altered and there is some loss of information. Diagnostic accuracy is preserved with compression ratios ranging from 10/1 to 40/1, depending on the modality (DR, CT, or MR), organ (lung, liver, or brain), and lesion composition (for example, high-contrast structures such as lung nodules and low-contrast structures such as early brain ischemia on CT)10,11,13,15,16,18,20. However, assessment of image compression algorithms is not the aim of this article; for this reason images were assessed with maximum image quality.
No significant differences emerged in the measurements in T1 and T2 images between systems or between observers; indeed, there was almost complete intra-observer agreement. This means that the TS, with the above-specified settings, is as detailed and precise as conventional DICOM viewers. The incomplete inter-observer agreement did not affect the comparison of the software systems, since each system was in any case tested in identical conditions. Operator 2 showed higher variability than operator 1, who is more experienced. It is likely that T2w images enhanced inter-observer variability because more lesions are present. Conversely, T1w images showed small inter-observer differences due to fact that MS hypointense lesions are fewer in number but more evident when present.
No MR studies of healthy individuals were assessed because the aim of this investigation was not to assess the software systems’ accuracy in the diagnosis of MS lesions but rather to quantify differences in image display between them. The assessment was performed in patients with varying degrees of neurological impairment. Had this study included only early MS, it is likely that it would have been based on fewer lesions, and that the lower number of lesions would have affected the results.
The present study assessed the first and the third above-mentioned aspect affecting teleradiology: image size and DICOM format. The TS differs both from conventional DICOM viewers and from several teleradiology systems in that no proprietary applets, plug-ins, or dedicated software for displaying DICOM images are required in the remote PC. A common web browser allows images to be displayed quickly and anywhere, thereby potentially reducing drastically the costs of image distribution within and between hospitals. From this perspective, expensive workstations would be needed only for image post-processing and analysis.
The second aspect is the use of the Internet for transmission: TS allows image display in all PCs, without the need of dedicated networks, even in suboptimal broadband connection settings as in some regions of western countries and in several non-western countries. For this reason, BB could be potentially suitable for second opinions and centralized reading.
In other words, with such image-sharing technology, the resources of centers where there is a need for radiological examinations can be optimized at very little cost.
A limitation of this study is that other aspects of teleradiology were not investigated for this TS; however, the aim of this study was not to assess the whole TS but rather an application to a disease. An additional limitation is that only MR of MS patients were assessed for the comparison. However, MR of MS patients are suitable for quantification with standard techniques that are widely accepted. In addition, testing the system with all the human diseases would be difficult and MS could represent a suitable model with lesions with high and low contrast with respect to the surrounding tissues.
In conclusion, quantitative assessment of MS lesion volumes in T1w and T2w images with a user interface of a teleradiology system that allows the consultation by means of a common web browser, without the need for proprietary plug-ins, applets, or dedicated software for DICOM display showed no significant differences from, and almost complete agreement with, conventional DICOM viewers.
References
- 1.Filippi M, Dousset V, McFarland HF, Miller DH, Grossman RI. Role of magnetic resonance imaging in the diagnosis and monitoring of multiple sclerosis: consensus report of the White Matter Study Group. J Magn Reson Imaging. 2002;15:499–504. doi: 10.1002/jmri.10097. [DOI] [PubMed] [Google Scholar]
- 2.Filippi M, Horsfield MA, Ader HJ, et al. Guidelines for using quantitative measures of brain magnetic resonance imaging abnormalities in monitoring the treatment of multiple sclerosis. Ann Neurol. 1998;43:499–506. doi: 10.1002/ana.410430414. [DOI] [PubMed] [Google Scholar]
- 3.Applegate K, Carlson R, Cawley K, et al: ACR technical standard for teleradiology. In. Reston, VA: American College of Radiology, 2005
- 4.Larson DB, Cypel YS, Forman HP, Sunshine JH. A comprehensive portrait of teleradiology in radiology practices: results from the American College of Radiology’s 1999 Survey. AJR Am J Roentgenol. 2005;185:24–35. doi: 10.2214/ajr.185.1.01850024. [DOI] [PubMed] [Google Scholar]
- 5.Kalyanpur A, Neklesa VP, Pham DT, Forman HP, Stein ST, Brink JA. Implementation of an international teleradiology staffing model. Radiology. 2004;232:415–419. doi: 10.1148/radiol.2322021555. [DOI] [PubMed] [Google Scholar]
- 6.National_Electrical_Manufacturers_Association. Digital Imaging and Communications in Medicine (DICOM). In. Rosslyn, VA: National Electrical Manufacturers Association, 1996
- 7.Eurostat. Internet usage in the EU25. Nearly half of individuals in the EU25 used the internet at least once a week in 2006. A third of households and three-quarters of enterprises had broadband internet access. In: Eurostat Press Office, 2006
- 8.Baker WA, Hearne SE, Spero LA, et al. Lossy (15:1) JPEG compression of digital coronary angiograms does not limit detection of subtle morphological features. Circulation. 1997;96:1157–1164. doi: 10.1161/01.cir.96.4.1157. [DOI] [PubMed] [Google Scholar]
- 9.Cosman PC, Davidson HC, Bergin CJ, et al. Thoracic CT images: effect of lossy image compression on diagnostic accuracy. Radiology. 1994;190:517–524. doi: 10.1148/radiology.190.2.8284409. [DOI] [PubMed] [Google Scholar]
- 10.Goldberg MA, Gazelle GS, Boland GW, et al. Focal hepatic lesions: effect of three-dimensional wavelet compression on detection at CT. Radiology. 1997;202:159–165. doi: 10.1148/radiology.202.1.8988206. [DOI] [PubMed] [Google Scholar]
- 11.Good WF, Maitz GS, Gur D. Joint photographic experts group (JPEG) compatible data compression of mammograms. J Digit Imaging. 1994;7:123–132. doi: 10.1007/BF03168505. [DOI] [PubMed] [Google Scholar]
- 12.Kalyanpur A, Neklesa VP, Taylor CR, Daftary AR, Brink JA. Evaluation of JPEG and wavelet compression of body CT images for direct digital teleradiologic transmission. Radiology. 2000;217:772–779. doi: 10.1148/radiology.217.3.r00nv22772. [DOI] [PubMed] [Google Scholar]
- 13.Ko JP, Chang J, Bomsztyk E, Babb JS, Naidich DP, Rusinek H. Effect of CT image compression on computer-assisted lung nodule volume measurement. Radiology. 2005;237:83–88. doi: 10.1148/radiol.2371041079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ko JP, Rusinek H, Naidich DP, et al. Wavelet compression of low-dose chest CT data: effect on lung nodule detection. Radiology. 2003;228:70–75. doi: 10.1148/radiol.2281020254. [DOI] [PubMed] [Google Scholar]
- 15.Ohgiya Y, Gokan T, Nobusawa H, et al. Acute cerebral infarction: effect of JPEG compression on detection at CT. Radiology. 2003;227:124–127. doi: 10.1148/radiol.2271020067. [DOI] [PubMed] [Google Scholar]
- 16.Savcenko V, Erickson BJ, Palisson PM, et al. Detection of subtle abnormalities on chest radiographs after irreversible compression. Radiology. 1998;206:609–616. doi: 10.1148/radiology.206.3.9494474. [DOI] [PubMed] [Google Scholar]
- 17.Slone RM, Foos DH, Whiting BR, et al. Assessment of visually lossless irreversible image compression: comparison of three methods by using an image-comparison workstation. Radiology. 2000;215:543–553. doi: 10.1148/radiology.215.2.r00ap47543. [DOI] [PubMed] [Google Scholar]
- 18.Uchida K, Nakamura K, Watanabe H, et al. Clinical evaluation of irreversible data compression for computed radiography in excretory urography. J Digit Imaging. 1996;9:145–149. doi: 10.1007/BF03168610. [DOI] [PubMed] [Google Scholar]
- 19.Zalis ME, Hahn PF, Arellano RS, Gazelle GS, Mueller PR. CT colonography with teleradiology: effect of lossy wavelet compression on polyp detection—initial observations. Radiology. 2001;220:387–392. doi: 10.1148/radiology.220.2.r01au33387. [DOI] [PubMed] [Google Scholar]
- 20.Savcenko V, Erickson BJ, Persons KR, et al. An evaluation of JPEG and JPEG 2000 irreversible compression algorithms applied to neurologic computed tomography and magnetic resonance images. Joint Photographic Experts Group. J Digit Imaging. 2000;13:183–185. doi: 10.1007/BF03167656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Corella F, Lewison KP, Talukder M. A teleradiology architecture featuring security and high performance. J Digit Imaging. 2002;15(Suppl 1):214–215. doi: 10.1007/s10278-002-5017-x. [DOI] [PubMed] [Google Scholar]
- 22.Walz M, Brill C, Bolte R, et al. Teleradiology requirements and aims in Germany and Europe: status at the beginning of 2000. Eur Radiol. 2000;10:1472–1482. doi: 10.1007/s003300000492. [DOI] [PubMed] [Google Scholar]
- 23.White P. Legal issues in teleradiology—distant thoughts! Br J Radiol. 2002;75:201–206. doi: 10.1259/bjr.75.891.750201. [DOI] [PubMed] [Google Scholar]
- 24.Hamilton E: JPEG file interchange format. In. Milpitas, CA: Joint Photographic Expert Group, 1992
- 25.International_Telecommunication_Union. Information technology—digital compression and coding of continous-tone still images—requirements and guidelines. In: International Telecommunication Union (ITU)—The International Telegraph and Telephone Consultative Committee (CCITT), 1992
- 26.Kurtzke JF. Disability rating scales in multiple sclerosis. Ann NY Acad Sci. 1984;436:347–360. doi: 10.1111/j.1749-6632.1984.tb14805.x. [DOI] [PubMed] [Google Scholar]
- 27.McDonald WI, Compston A, Edan G, et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann Neurol. 2001;50:121–127. doi: 10.1002/ana.1032. [DOI] [PubMed] [Google Scholar]