Abstract
The objective of this study was to compare the diagnostic accuracy in the interpretation of chest nodules using original CT images versus enhanced CT images based on the wavelet transform. The CT images of 118 patients with cancers and 60 with benign nodules were used in this study. All images were enhanced through an algorithm based on the wavelet transform. Two experienced radiologists interpreted all the images in two reading sessions. The reading sessions were separated by a minimum of 1 month in order to minimize the effect of observer’s recall. The Mann–Whitney U nonparametric test was used to analyze the interpretation results between original and enhanced images. The Kruskal–Wallis H nonparametric test of K independent samples was used to investigate the related factors which could affect the diagnostic accuracy of observers. The area under the ROC curves for the original and enhanced images was 0.681 and 0.736, respectively. There is significant difference in diagnosing the malignant nodules between the original and enhanced images (z = 7.122, P < 0.001), whereas there is no significant difference in diagnosing the benign nodules (z = 0.894, P = 0.371). The results showed that there is significant difference between original and enhancement images when the size of nodules was larger than 2 cm (Z = −2.509, P = 0.012, indicating the size of the nodules is a critical evaluating factor of the diagnostic accuracy of observers). This study indicated that the image enhancement based on wavelet transform could improve the diagnostic accuracy of radiologists for the malignant chest nodules.
Key words: Wavelet transform, chest nodules, enhanced CT
Introduction
Currently, both of the morbidity and mortality of bronchogenic lung cancer rank first in malignant tumors. The overall 5-year survival rate of lung cancer patients is only 14% and remained at this level for the past two decades. However, it is estimated that only 15% of early-stage lung cancer could be detected by means of chest radiography. Although findings from comparative studies of chest radiography and computed tomography (CT) have shown CT to be the best imaging modality for the detection of pulmonary nodules, the original images of CT are still not good enough in quality to satisfy the requirement of interpretation in certain conditions. For example, the sensitivity of plain CT is not high enough to show spiculation sign, vacuole sign, and pleural indentation, which could bring difficulties in differentiating small peripheral lung cancer from benign nodules.1 In addition, the application of low-dose protocol for the screening early-stage lung cancer with spiral CT may cause the degradation of image quality .The visibility of some structures in medical images, especially the details that may be conveying diagnostic information, may have a vital role in providing sufficient visual information for the clinician.2 The visibility of relatively smaller and nonsignificant details may be extremely important, especially in early diagnosis of cancer.
The application of wavelet analysis in enhancing medical images is the focus of international interest. For example, Hakan Öktem introduces a local adaptive image enhancement and simultaneous denoising algorithm which is based on the modification of wavelet transform coefficients.3 The result showed that this algorithm could increase the visibility of relatively nonsignificant details without distorting the image. Yang used a hybrid structural filtering technique which is based on wavelet reconstruction of feature extreme to enhance the feature differences between normal and diseased lung parenchyma.4 The thorax includes information on many different tissues with different X-ray transmittance, which would have a major impact on identification of early signs of lung cancer.5
This paper aims to assert the better effect of using wavelet transformation and combining other enhancement or noise removal methods to enhance CT images of early-stage peripheral lung cancers.
Material and Methods
Materials
Our Institutional Review Board approved this study. The CT images of 118 patients with cancers and 60 with benign nodules were used in this study. Of them, there were 73 men and 105 women (age range, 19–80 years; mean age, 58 years). The final diagnosis of 118 small peripheral lung cancers (diameter range, 0.6–3.0 cm; mean diameter, 2.0 cm) was determined by either an operation or biopsy. The diagnosis of benign nodule (diameter range, 1.0–3.0 cm; mean diameter, 2.0 cm) was confirmed either by pathology or by a 2-year follow-up. A total of 2,058 CT digital images obtained from 178 patients were made available in the study.
Image Acquisition
All images were acquired with an eight-slice helical CT scanner (GE/Light speed ultra System CT99, USA) using a tube voltage of 120 kV and current of 200 mA. Slice thickness and reconstruction intervals for routine scanning were 5.0 mm and those for high-resolution CT were 1 mm. CT images were displayed at fixed setting (lung window center, −600 HU; lung window width, 1,600 HU; mediastinum window center, 40 HU; mediastinum window width, 400 HU). The images were reconstructed with a matrix of 512 × 512.
Main Steps of Image Enhancement
Base on relative study and our pilot trials, the sym8 function was selected to perform multiscale wavelet decomposition.6 The decomposed high-frequency coefficients were enhanced, and the wavelet reconstruction was carried out depending on the high- and low-frequency coefficients to obtain the enhanced images. Then, the CLAHE or Wiener-2 adaptive filter was used to improve the quality of images. One radiologist who did not participate in the process of evaluation read the image quality after the process of enhancement. When the image quality was regarded as not meeting the requirement of interpretation by this radiologist, the experience value of CLAHE or Wiener-2 adaptive filter was used to improve the image quality.
Image Interpretation
Each of the images was evaluated by two experienced radiologists, and the results were obtained by the consensus conclusion. In cases of discrepancy, conclusions were reached by interrater consensus in the presence of a third experienced radiologist. The reading sessions were separated by a minimum of 1 month in order to minimize the effect of observer’s recall. In the first reading session, each reader interpreted the original images, and in the second session, the enhanced images were interpreted. Cases were presented in a randomized order in each reading session. All radiologists were blinded to the patients’ clinical history, physical findings, patient identity, and final diagnostic results. The observers were told that the purpose of the study was to distinguish benign from malignant lesions. Images were displayed in a one-by-one format using a monochrome monitor (BARCO MGD221, Barcoview, Kortrijk, Belgium) with a matrix size of 1,280 × 1,600. All annotations and labels in the images were toggled off. The readers were instructed to determine the characteristics of each chest mass. A five-point malignancy scale was used, with a score of 1 defining a definitely malignant pulmonary mass, a score of 2 characterizing probably a malignant pulmonary nodule, a score of 3 referring equivocal, a score of 4 describing a probably benign nodule, and a score of 5 being a definitely benign nodule. All processes of images enhancement were performed with the software of MATLAB (version 7.3.0), including wavelet enhancement, the Wiener-2 adaptive filer and the CLAHE. The operating system was Windows 2000.
Data Analysis
The Mann–Whitney U nonparametric test was used to analyze the interpretation results between the original and enhanced images. The Kruskal–Wallis H nonparametric test of K independent samples was used to investigate the related factors which could affect the diagnostic accuracy of lung diseases. Analysis was performed using SPSS, version 14.0, software (SPSS, Inc., Chicago, IL).
Results
Parameters Selection Results
The sym8 function was selected for image decomposition and reconstruction. The decomposition coefficients enhancement threshold k of wavelet ranges from 300 to 500, and the enhanced multiple of coefficients vary from 0.9 to 1.3. The neighborhood size of CLAHE is 8 × 8, and the extent of local contrast enhancement is within the scope from 0.001 to 0.002. The experience value was used to implement CLAHE and (or) Wiener-2 adaptive filter in accordance with the size of image contrast or the magnitude of noise intensity.
Interpretation Results of Original and Enhanced Images
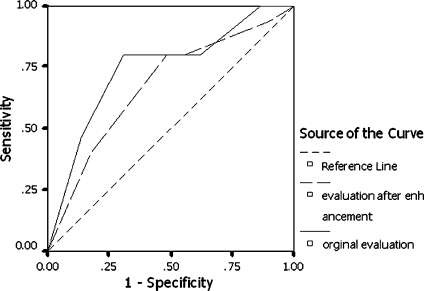
The observer interpretation results of the original and enhanced images are shown in Tables 1 and 2, which were used to draw ROC curves, as shown in Fig. 1. The area under the ROC curves for the original and enhanced images is 0.681 and 0.736, respectively. The Mann–Whitney U nonparametric test was used to analyze the interpretation results between original and enhanced images. There is significant difference in diagnosing the malignant nodules between original and enhanced images (z = 7.122, P < 0.001).Whereas there is no significant difference in diagnosing the benign nodules (z = 0.894, P = 0.371).
Table 1.
Observers’ Interpretation Results Using Original Images
| Characteristic of chest nodules | Interpretation results of original images (N, %) | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | Total | |
| Benign | 3 (5.00) | 10 (16.67) | 5 (8.33) | 21 (35.00) | 21 (35.00) | 60 (100.00) |
| Malignant | 24 (20.34) | 36 (30.51) | 14 (11.86) | 22 (18.64) | 22 (18.65) | 118 (100.00) |
| Total | 27 (15.17) | 46 (25.84) | 19 (10.67) | 43 (24.16) | 43 (24.16) | 178 (100.00) |
Table 2.
Observers’ Interpretation Results Using Enhanced Images
| Characteristic of chest nodules | Interpretation results of enhanced images | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | Total | |
| Benign | 5 (8.33) | 13 (21.67) | 1 (1.67) | 18 (30.00) | 23 (38.33) | 60 (100.00) |
| Malignant | 41 (34.75) | 38 (32.20) | 3 (2.54) | 23 (19.49) | 13 (11.02) | 118 (100.00) |
| Total | 46 (25.84) | 51 (28.65) | 4 (2.45) | 41 (23.03) | 36 (20.22) | 178 (100.00) |
Fig. 1.
Source of the curve.
For evaluating the related factors which could affect the diagnostic accuracy of observers, the interpretation results were compared between the original and enhanced images according to patients’ gender, patients’ age, location of nodules, and size of nodules. The results showed that there is significant difference between the original and enhancement images when the size of nodules was larger than 2 cm (Z = −2.509, P = 0.012). There was no significant difference in other aspects (Table 3).
Table 3.
The Interpreting Results between Original and Enhancement Images According to Patients’ Gender, Patients’ Age, Location, and Size of Chest Nodules
| Factors | Evaluation | Interpretation results | Z value | P value | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | Total | ||||
| Gender | |||||||||
| Men | Original | 10 | 22 | 6 | 18 | 17 | 73 | −1.545 | 0.122 |
| After enhancement | 20 | 22 | 0 | 16 | 15 | 73 | |||
| Women | Original | 17 | 24 | 13 | 25 | 26 | 105 | −1.552 | 0.121 |
| After enhancement | 26 | 29 | 4 | 25 | 21 | 105 | |||
| Age | |||||||||
| <60 | Original | 16 | 18 | 13 | 17 | 18 | 82 | −.172 | 0.864 |
| After enhancement | 19 | 20 | 4 | 20 | 19 | 82 | |||
| ≥60 | Original | 11 | 28 | 6 | 26 | 25 | 96 | −2.808 | 0.005 |
| After enhancement | 27 | 31 | 0 | 21 | 17 | 96 | |||
| Location | |||||||||
| Upper | Original | 13 | 19 | 14 | 26 | 25 | 97 | −1.847 | 0.065 |
| After enhancement | 22 | 27 | 2 | 28 | 18 | 97 | |||
| Middle lobe or tongue lobe | Original | 1 | 5 | 2 | 4 | 3 | 15 | −1.240 | 0.215a |
| After enhancement | 4 | 5 | 1 | 3 | 2 | 15 | |||
| Lower lobe | Original | 13 | 22 | 3 | 13 | 15 | 66 | −.821 | 0.412 |
| After enhancement | 20 | 19 | 1 | 10 | 16 | 66 | |||
| Nodule size | |||||||||
| <1.0 cm | Original | 4 | 10 | 9 | 10 | 11 | 44 | −.245 | 0.807 |
| After enhancement | 4 | 12 | 2 | 15 | 11 | 44 | |||
| 1.0∼1.9 cm | Original | 13 | 28 | 7 | 25 | 23 | 96 | −1.378 | 0.168 |
| After enhancement | 25 | 25 | 2 | 23 | 21 | 96 | |||
| 2.0∼3.0 cm | Original | 10 | 8 | 3 | 8 | 9 | 38 | −2.509 | 0.012 |
| After enhancement | 17 | 14 | 0 | 3 | 4 | 38 | |||
| Total | Original | 27 | 46 | 19 | 43 | 43 | 178 | −2.174 | 0.030 |
| After enhancement | 46 | 51 | 4 | 41 | 36 | 178 | |||
aExact Sig. [2 × (1-tailed Sig.)] = 0.233
Discussion
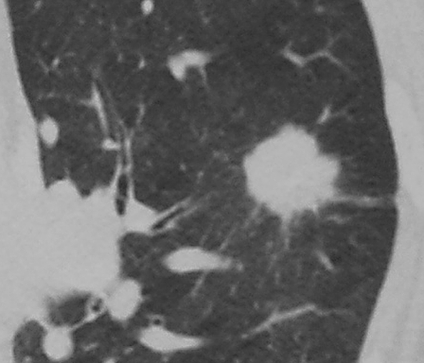
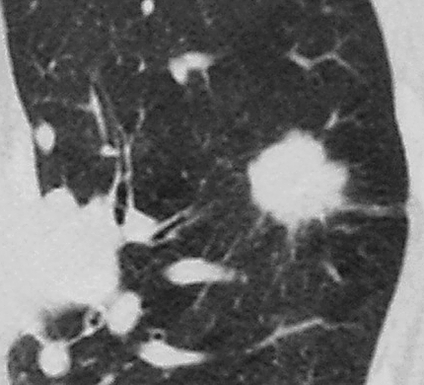
Lung cancer is the most common fatal malignancy in both men and women.7 More than 50% of patients will have distant metastases at diagnosis, and only 20%–25% of patients will have lesions that are localized and potentially respectable for cure.8 Some studies have suggested that spiral CT can depict lung cancers that are of a smaller size (<2 cm in diameter) and earlier stage (85%–93% at stage I) than those observed at chest radiography in current clinical practice.9 This study mainly focused on the detect ability of chest nodules but did not consider the characterization of the lesions although which is important for patients’ treatment and prognosis. The details of images, such as the size, location, margin and internal density, and peripheral signs of chest nodules, were very important for the final diagnosis.10 The evaluation of the characteristic of chest nodules was a subjective task. In some conditions, for example, the low-dose CT screening, the observers’ decision may be affected by the degradation of image quality. Image enhancement techniques base on wavelet transform have been the main tools to improve the quality and appearance of images by changing contrast and the other parameters (Figs. 2 and 3).
Fig. 2.
The original image of lung carcinoma.
Fig. 3.
The enhanced image of lung carcinoma.
The results of our study showed that the z values of original and enhanced images are 0.681 and 0.736, respectively. There are significant differences in ROC performance between the original images and enhanced images for the malignant nodules. The diagnostic performance of enhanced images is superior to that of original images. In addition, the main factors which could affect the final decision of observers were also evaluated. Our results suggested that when the size of chest nodules is larger than 2 cm, the diagnostic accuracy of observers have been greatly improved using the enhanced images. We believe that the most important reason is that enhancement based on wavelet transform could improve the image quality. While more details of images could be observed, especially for the chest nodules with larger size, more confidence of the observers for the characterization of chest nodules is increased.
Certainly, there are some limitations in this study. The noise of images is slightly fortified when the high-frequency component is enhanced by wavelet transformation. We also observed that CLAHE could magnify the background noise at the same time of improving the image contrast and enhancing the image details. In addition, many parameters such as wavelet decompose scale size, threshold k, and enhanced multiples are involved in wavelet transform enhancement. The process of selection is a subjective task which could be affected by the experience of observers. All these factors could decrease the diagnostic performance of enhanced images. This algorithm of enhancement should be improved further.
In conclusion, this study indicates that the image enhancement based on wavelet transform could improve the diagnostic accuracy of radiologists and could be deemed as a useful reference to the equivalent studies.
Footnotes
Program of Funds: The program of Natural Science Fund of China (Serial Number: 30972550); the program of Natural Science Fund of Beijing (Serial Number: 7092010)
Contributor Information
Zhigang Liang, Phone: +86-10-13693219153, Email: zg_liang@yahoo.com.cn.
Wei Wang, Phone: +86-10-83911504, Email: wei6014@gscas.ac.cn.
References
- 1.Li F, Sone S, Abe H, Macmahon H, Doi K. Malignant versus benign nodules at CT screening for lung cancer: comparison of thin-section CT findings. Radiology. 2004;233(3):793–798. doi: 10.1148/radiol.2333031018. [DOI] [PubMed] [Google Scholar]
- 2.Öktem H, Egiazarian K, Niittylahti J, Lemmetti J, Latvala J: A wavelet based algorithm for simultaneous x-ray image de-noising and enhancement. In Proc. 2nd International Conference on Information, Communications & Signal Processing (ICICS ’99), Singapore, December 1999
- 3.Öktem H, Egiazarian K, Niittylahti J, Lemmetti J. An approach to adaptive enhancement of diagnostic x-ray images. EURASIP J Appl Signal Process. 2003;5:430–436. [Google Scholar]
- 4.Yang GZ, Hansell DM. Hansell: CT image enhancement with wavelet analysis for the detection of small airways disease. IEEE Trans Med Imag. 1997;16(6):953–961. doi: 10.1109/42.650893. [DOI] [PubMed] [Google Scholar]
- 5.Birring SS. Symptoms and the early diagnosis of lung cancer. Thorax. 2005;60:268–269. doi: 10.1136/thx.2004.032698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jin ATB, Ling DNC, Song OT. An efficient fingerprint verification system using integrated wavelet and Fourier-Mellin invariant transform. Image Vis Comput. 2004;22:503–513. doi: 10.1016/j.imavis.2003.12.002. [DOI] [Google Scholar]
- 7.Swensen SJ, Jett JR, Sloan JA, Midthun DE, Hartman TE, Sykes AM, et al. Screening for lung cancer with low-dose spiral computed tomography. Am J Respir Crit Care Med. 2002;165(4):508–513. doi: 10.1164/ajrccm.165.4.2107006. [DOI] [PubMed] [Google Scholar]
- 8.Swensen SJ, Jett JR, Hartman TE, Midthun DE, Sloan JA, Sykes AM, Aughenbaugh GL, Clemens MA. Lung cancer screening with CT: Mayo Clinic experience. Radiology. 2003;226(3):756–761. doi: 10.1148/radiol.2263020036. [DOI] [PubMed] [Google Scholar]
- 9.Sone S, Li F, Yang ZG, Takashima S, Maruyama Y, Hasegawa M, Wang JC, Kawakami S, Honda T. Characteristics of small lung cancers invisible on conventional chest radiography and detected by population based screening using spiral CT. Br J Radiol. 2000;73(866):137–145. doi: 10.1259/bjr.73.866.10884725. [DOI] [PubMed] [Google Scholar]
- 10.Sluimer I, Schilham A, Prokop M, Ginneken B. Computer analysis of computed tomography scans of the lung: a survey. IEEE Trans Med Imag. 2006;25(4):385–405. doi: 10.1109/TMI.2005.862753. [DOI] [PubMed] [Google Scholar]