In the current issue of Mayo Clinic Proceedings, Blackshear et al1 report on 5 patients who underwent surgical repair of hypertrophic obstructive cardiomyopathy (HOCM). In all 5 patients, the clinical course was complicated by spontaneous gastrointestinal (GI), mucosal, or excessive postoperative bleeding associated with acquired von Willebrand syndrome (AvWS); surgical septal myectomy, used to treat HOCM, produced resolution of the bleeding diathesis. Although such case histories tend to be dismissed as a chance association, the association of HOCM repair and resolution of von Willebrand syndrome parallels the experience after cardiac valve replacement in aortic stenosis (AS).2 As such, the report by Blackshear et al provides valuable validation of existing theories linking blood flow conditions of high shear stress (ie, increased velocity between adjacent layers of blood flowing within the vasculature) to AvWS. The physiology underlying this phenomenon will be briefly reviewed.
von Willebrand factor (vWF), a large multimeric glycoprotein, is synthesized in bone marrow megakaryocytes and vascular endothelial cells. Extensive posttranslational modification of the primary gene product results in vWF multimers ranging in size from 500 kD to 10 million kD or larger (unusually large multimers).3 After endothelial secretion, ADAMTS-13 (a disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13) cleaves vWF at the Tyr 1605-Met 1606 bond within the A2 domain,4 preferentially under blood flow conditions of high intravascular shear stress, resulting in cleavage of the vWF multimers, especially the larger or high-molecular-weight multimers (HMWMs). Thus, circulating plasma vWF multimers reflect an equilibrium between secretion of vWF containing large and unusually large multimers and their cleavage into smaller derivatives, which, when visualized on agarose electrophoretic gels,5,6 are categorized as low-molecular-weight multimers (<6 bands), intermediate-molecular-weight multimers (6-10 bands), and large multimers or HMWMs (>10 bands).7
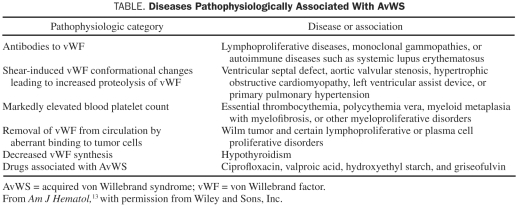
von Willebrand disease (vWD), the most common congenital autosomal bleeding disorder, is caused by quantitative and qualitative defects of vWF but may also be acquired (AvWS).8 An increasing number of medical disorders associated with AvWS are being recognized9; however, AvWS pathogenesis has been elucidated in only a few associated disorders (Table). Investigations into the association between AS and GI hemorrhage have shed light on the role of increased shear stress and loss of vWF HMWMs.2 The observed vWF abnormalities were reversed after aortic valve replacement surgery and recurred in selected patients with mismatched prostheses and in patients in whom AS recurred. Similarly, other cardiovascular disorders associated with increased intravascular shear stress could result in AvWS. One such disorder, HOCM, is associated with vWF abnormalities similar to those in AS.10 However, it remained unknown whether HOCM-associated acquired vWF abnormalities have clinical consequences (ie, whether they cause AvWS with a propensity for clinical bleeding). Blackshear et al clearly identified consequential AvWS-associated GI hemorrhage in patients with HOCM and showed that septal myectomy resulted in normalization of the vWF multimers and subsequent resolution of GI hemorrhage, similar to the experience with AS.2 Collectively, the data confirm the association between loss of vWF HMWMs and conditions of high intravascular shear stress and imply a potential, or at least a partial, causal relationship between acquired vWF abnormalities and GI hemorrhage in this group of patients.
TABLE.
Diseases Pathophysiologically Associated With AvWS
See also page 219
It has been well demonstrated that patients with hereditary vWD and those with AvWS have a propensity to develop GI arteriovenous malformation (AVM)–associated hemorrhage,11 but the link between abnormalities of vWF and bleeding GI AVMs has remained elusive. The recent report by Starke et al12 sheds light on the role of endothelial vWF in angiogenesis. The authors demonstrated that small interfering RNA–mediated inhibition of vWF expression in endothelial cells increased in vitro angiogenesis and release of angiogenic factors. These observations were confirmed in experiments using endothelial cells from patients with vWD and in a mouse model of vWD, thus identifying a novel angiogenesis regulatory function for vWF. Although vWF multimerization was not studied by Starke et al, it is tempting to speculate that it plays a role in angiogenesis regulation and that vWF HMWMs are of particular importance.
This association between AvWS and cardiovascular disorders raises several important questions for the clinician, regarding patient selection for testing, and for the performing laboratory, regarding the extent of laboratory testing that is warranted. Should all patients with predisposing cardiovascular disorders undergo comprehensive testing for vWD? If so, what extent of testing is warranted? Should all patients undergo vWF multimer analysis, which is a labor-intensive assay with limited clinical availability? And finally, how will laboratory test results influence patient management?
Currently suggested initial laboratory work-up for patients with vWD consists of the following: (1) measurement of plasma vWF antigen (vWF:Ag); (2) assays of plasma vWF activity, most commonly the vWF ristocetin cofactor activity (vWF:RCo) assay; and (3) the plasma coagulation factor VIII activity assay. Reduced vWF levels and/or abnormal vWF:RCo/vWF:Ag ratios typically prompt reflexive analysis of vWF multimers for the purpose of subtyping vWD.13 Limitations of current technologies preclude reliance solely on the vWF:RCo/vWF:Ag ratio and levels to evaluate for vWD and AvWS.14 Indeed, in the Blackshear et al series of patients, vWF:RCo/vWF:Ag ratios and levels were normal, raising the question of whether all such patients should undergo vWF multimer analysis.
A reasonable approach to patient selection for laboratory testing is to pursue initial vWD laboratory testing on the basis of published algorithms and recommendations for patients with symptomatic bleeding or increased risk of bleeding. However, for selected patients, such as those with cardiovascular disorders causing the increased intravascular shear flow conditions associated with AvWS pathogenesis, supplemental vWF multimer analysis should be considered despite normal vWF levels and ratios.13 When more reliable assays for vWF activity are readily available,15 vWF multimer analysis can be mostly confined to patients with low levels of plasma vWF or abnormal vWF activity to vWF:Ag ratios.
Regarding the effect on patient management, the diagnosis of AvWS may explain hemorrhagic symptoms in the group of patients with predisposing cardiovascular disorders, and AvWS may be an additional indication for consideration of surgical correction of the underlying cardiovascular disorder. Monitoring for reversal of the acquired abnormalities of vWF may provide an additional tool to evaluate the efficacy of surgical management. Thus, patients with cardiovascular disorders associated with increased intravascular shear stress have a propensity for acquired loss of vWF HMWMs and also for AvWS, the latter patients often exhibiting GI AVM–associated hemorrhage that may primarily reflect altered vWF influences on angiogenesis. Blackshear et al have reported yet another etiologic association for AvWS, and additional associations will likely continue to evolve.
References
- 1. Blackshear JL, Schaff HV, Ommen SR, Chen D, Nichols WL. Hypertrophic obstructive cardiomyopathy, bleeding history, and acquired von Willebrand syndrome: response to septal myectomy. Mayo Clin Proc. 2011;86(3)219-224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Vincentelli A, Susen S, Le Tourneau T, et al. Acquired von Willebrand syndrome in aortic stenosis. N Engl J Med. 2003;349:343-349 [DOI] [PubMed] [Google Scholar]
- 3. Wagner DD. Cell biology of von Willebrand factor. Annu Rev Cell Biol. 1990;6:217-246 [DOI] [PubMed] [Google Scholar]
- 4. Zheng X, Chung D, Takayama TK, Majerus EM, Sadler JE, Fujikawa K. Structure of von Willebrand factor-cleaving protease (ADAMTS13), a metalloprotease involved in thrombotic thrombocytopenic purpura. J Biol Chem. 2001;276(44)41059-41063 [DOI] [PubMed] [Google Scholar]
- 5. Ledford-Kraemer MR. Analysis of von Willebrand factor structure by multimer analysis. Am J Hematol. 2010;85:510-514 [DOI] [PubMed] [Google Scholar]
- 6. Pruthi RK, Daniels TM, Heit JA, Chen D, Owen WG, Nichols WL. Plasma von Willebrand factor multimer quantitative analysis by in-gel immunostaining and infrared fluorescent imaging. Thromb Res. 2010;126:543-549 [DOI] [PubMed] [Google Scholar]
- 7. Budde U, Pieconka A, Will K, Schneppenheim R. Laboratory testing for von Willebrand disease: contribution of multimer analysis to diagnosis and classification. Semin Thromb Hemost. 2006;32:514-521 [DOI] [PubMed] [Google Scholar]
- 8. Nichols WL, Hultin MB, James AH, et al. von Willebrand disease (VWD): evidence-based diagnosis and management guidelines, the National Heart, Lung, and Blood Institute (NHLBI) Expert Panel report (USA). Haemophilia. 2008;14:171-232 [DOI] [PubMed] [Google Scholar]
- 9. Mohri H. Acquired von Willebrand syndrome: features and management. Am J Hematol. 2006;81:616-623 [DOI] [PubMed] [Google Scholar]
- 10. Le Tourneau T, Susen S, Caron C, et al. Functional impairment of von Willebrand factor in hypertrophic cardiomyopathy: relation to rest and exercise obstruction. Circulation. 2008;118:1550-1557 [DOI] [PubMed] [Google Scholar]
- 11. Fressinaud E, Meyer D. International survey of patients with von Willebrand disease and angiodysplasia [letter]. Thromb Haemost. 1993;70:546 [PubMed] [Google Scholar]
- 12. Starke RD, Ferraro F, Paschalaki KE, et al. Endothelial von Willebrand factor regulates angiogenesis. Blood. 2011;20;117(3)1071-1080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nichols WL, Rick ME, Ortel TL, et al. Clinical and laboratory diagnosis of von Willebrand disease: a synopsis of the 2008 NHLBI/NIH guidelines. Am J Hematol. 2009;84:366-370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kitchen S, Jennings I, Woods TA, Kitchen DP, Walker ID, Preston FE. Laboratory tests for measurement of von Willebrand factor show poor agreement among different centers: results from the United Kingdom National External Quality Assessment Scheme for Blood Coagulation. Semin Thromb Hemost. 2006;32:492-498 [DOI] [PubMed] [Google Scholar]
- 15. Chen D, Daigh CA, Hendricksen JI, et al. A highly-sensitive plasma von Willebrand factor ristocetin cofactor (VWF:RCo) activity assay by flow cytometry. J Thromb Haemost. 2008;6:323-330 [DOI] [PubMed] [Google Scholar]