Abstract
OBJECTIVE: To describe the views of residency program directors regarding the effect of the 2010 duty hour recommendations on the 6 core competencies of graduate medical education.
METHODS: US residency program directors in internal medicine, pediatrics, and general surgery were e-mailed a survey from July 8 through July 20, 2010, after the 2010 Accreditation Council for Graduate Medical Education (ACGME) duty hour recommendations were published. Directors were asked to rate the implications of the new recommendations for the 6 ACGME core competencies as well as for continuity of inpatient care and resident fatigue.
RESULTS: Of 719 eligible program directors, 464 (65%) responded. Most program directors believe that the new ACGME recommendations will decrease residents' continuity with hospitalized patients (404/464 [87%]) and will not change (303/464 [65%]) or will increase (26/464 [6%]) resident fatigue. Additionally, most program directors (249-363/464 [53%-78%]) believe that the new duty hour restrictions will decrease residents' ability to develop competency in 5 of the 6 core areas. Surgery directors were more likely than internal medicine directors to believe that the ACGME recommendations will decrease residents' competency in patient care (odds ratio [OR], 3.9; 95% confidence interval [CI], 2.5-6.3), medical knowledge (OR, 1.9; 95% CI, 1.2-3.2), practice-based learning and improvement (OR, 2.7; 95% CI, 1.7-4.4), interpersonal and communication skills (OR, 1.9; 95% CI, 1.2-3.0), and professionalism (OR, 2.5; 95% CI, 1.5-4.0).
CONCLUSION: Residency program directors' reactions to ACGME duty hour recommendations demonstrate a marked degree of concern about educating a competent generation of future physicians in the face of increasing duty hour standards and regulation.
The reactions of residency program directors to the ACGME duty hour recommendations demonstrate a marked degree of concern about educating a competent generation of future physicians in the face of increasing duty hour standards and regulation.
ACGME = Accreditation Council for Graduate Medical Education; CI = confidence interval; IOM = Institute of Medicine; OR = odds ratio; PGY = postgraduate year
A mid intense debate regarding the effect of duty hour limitations for resident physicians on patient safety1,2 and on residents' education,3 well-being,3-6 and professional identity,7 the Accreditation Council for Graduate Medical Education (ACGME) is planning to implement substantial changes to resident duty hours.8 The new recommendations, which include increased supervision, 16-hour shift maximum for postgraduate year (PGY) 1 residents, and recommended strategic napping, have been met with differing levels of agreement based on specialty and size and type of program.9 The ACGME solicited public comment from the graduate medical education community and based on that input would consider further modifications to the recommendations.10
The current debate over resident duty hours and resident fatigue can be traced to the untimely death of Libby Zion in 1984, which prompted the State of New York to pass legislation regulating resident working conditions.11-13 In 2003, the ACGME issued the first duty hour regulations14; however, approximately 5 years later the Institute of Medicine (IOM) called for further modifications to resident duty hours.15 The new 2010 recommendations reflect ongoing efforts by the ACGME to address the concerns raised by the IOM and others regarding the effect of resident fatigue on patient safety as well as the quality of the overall graduate medical education experience.16-18
For editorial comment, see pages 176 and 179
Around the same time that the ACGME was developing initial duty hour restrictions, it sought to describe the multidimensional nature of a competent physician. The ACGME ultimately selected 6 core competencies—patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice—that were believed to reflect “elements of medical practice common across specialties.”19 However, since the adoption of the core competencies by the ACGME and several medical boards during the past 10 years, concerns have arisen regarding both specialty-specific competency needs and the challenge of how to accurately measure the core competencies.19-21
In this article, we describe the perspectives of residency program directors regarding the potential implications of the 2010 duty hour recommendations for meeting the 6 core competencies of graduate medical education as well as for affecting patient safety as potentially impacted by discontinuity of inpatient care and by resident fatigue.
METHODS
The study's methods have been published.9 From July 8 through July 20, 2010, 1 month after the ACGME released its duty hour recommendations,8 we sent a confidential Web-based survey to all publicly available e-mails for all US pediatrics, internal medicine, and general surgery program directors using REDCap (Research Electronic Data Capture) Survey (Nashville, TN) distributed by Mayo Clinic in Rochester, MN.22 We identified e-mail addresses from the American Medical Association FREIDA list of accredited programs, the ACGME list of accredited programs, and specific program Web sites. This study was approved by the Mayo Clinic Institutional Review Board.
Survey Instrument
As part of a larger self-administered survey on the proposed duty hour changes, program directors completed 8 items on how they believe the new duty hour requirements will affect various aspects of graduate medical education, including the 6 core competencies, continuity of care, and resident fatigue. Content validity of the instrument items is supported by the iterative development of items using specific language taken from the ACGME proposed recommendations and the ACGME General Competency Standards document,23 with minor modifications as needed. The survey items were reviewed and modified by individuals with content expertise in duty hours, graduate medical education, and survey development.
The specific duty hour changes in the new ACGME regulations8 that respondents were asked to consider were as follows: PGY-1 residents must have direct supervision from a physician physically present with the resident or the supervising physician must be on site and available to provide direct supervision; learning objectives must not be compromised by excessive nonphysician service obligations; maximum duty hours of 80 per week, averaged over 4 weeks; duty period for PGY-1 residents must not exceed 16 hours; PGY-2 and higher: in-hospital on-call frequency every third night, no averaging; residents should have 10 hours off between duty shifts and must have 8 hours free of duty between duty periods; residents must not be scheduled for more than 6 consecutive nights of night duty; 24 hours off per 7-day period, when averaged over 4 weeks; PGY-1 residents must not be permitted to moonlight; duty hour exceptions to 88 hours per week averaged are permissible for select programs with a sound educational rationale; and time spent on being on call at home by residents must count toward the 80-hour maximum weekly limit.
First, we asked participants to rate how the duty hour changes would likely affect the 6 following areas, representative of the 6 ACGME core competencies: “quality and safety of patient care” (patient care); “educational experience” (medical knowledge); “investigation and self-evaluation of own patient care” (practice-based learning and improvement); “effective communication with patients, families, and other health care professionals” (interpersonal and communication skills); “responsiveness to patient needs that supersedes self-interest” (professionalism); and “coordination of patient care” (systems-based practice).
Second, we asked program directors to rate how the changes would likely affect “continuity with hospitalized patients” and “resident fatigue.” Program directors' beliefs regarding the implications of the new duty hour regulations on all 8 items previously described were measured using 5-point scales (strongly increase, moderately increase, no change, moderately decrease, or strongly decrease). To encourage participation, nonresponders were contacted with up to 3 electronic mailings.
We also asked respondents questions regarding their demographic characteristics, clinical specialty (medicine, pediatrics, surgery), academic rank (instructor, assistant professor, associate professor, professor, other), years as program director (0-5, 6-10, 11-15, 16-20, and >20 years), average number of hours per week of direct teaching or supervision of residents (0-5, 6-10, 11-15, 16-20, and >20 hours), and self-reported program type (large university-based, small university-based, large community-based, small community-based, university-affiliated community hospital, military, and other).
Statistical Analyses
Survey items were summarized with frequencies and percentages. Response rates were compared among the 3 specialty groups with a Pearson χ2 test. Each of the responses to the survey items of interest was dichotomized as “decrease” (moderately or strongly decrease) vs “no change/increase” (no change or moderately or strongly increase). Logistic regression models were used to compare these responses between groups. The first set of models (unadjusted) included the predictors one at a time. The second set of models included each predictor along with age, sex, and geographic region as adjustment variables. Each set of models was summarized with odds ratios (ORs) and 95% confidence intervals (CIs). Two-sided P<.05 was considered statistically significant. No adjustments for multiple comparisons were made, and all analyses were unweighted. All analyses were performed using SAS version 9.1 (SAS Institute, Cary, NC).
RESULTS
Program Director Characteristics
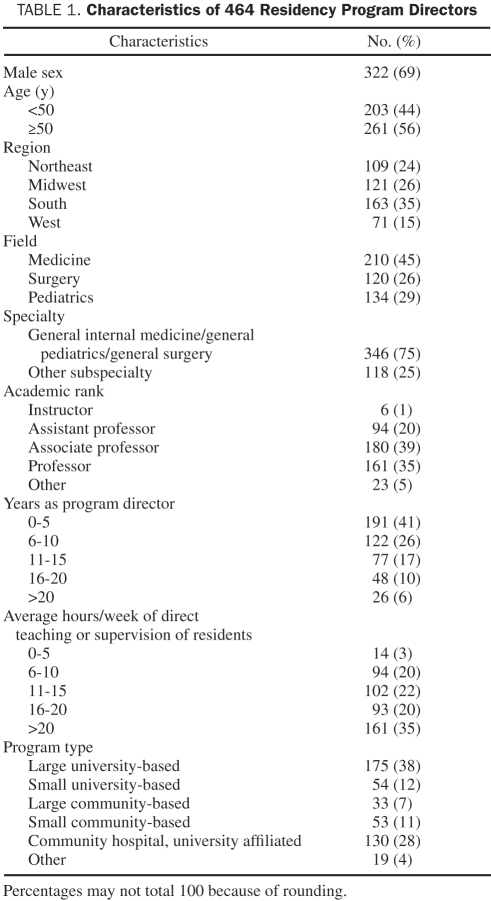
Of the 823 total programs in medicine, pediatrics, and surgery in the United States,24 we successfully identified publicly available e-mail addresses for 742 program directors. Of the 742 potential respondents, 23 (3%) could not be contacted because of nonfunctional e-mail addresses. Of the remaining 719 eligible participants, 464 returned completed surveys within 3 weeks, for a response rate of 65%. The characteristics of the respondents are shown in Table 1. Response rates did not differ significantly among specialties: medicine, 213 (69%) of 308; pediatrics, 127 (67%) of 189; and surgery, 138 (62%) of 222 (χ2 test, P=.24; pair-wise comparisons: medicine vs pediatrics, P=.65; medicine vs surgery, P=.09; pediatrics vs surgery, P=.29).
TABLE 1.
Characteristics of 464 Residency Program Directors
Faculty Views of the Implications of New Duty Hour Recommendations for Core Competencies
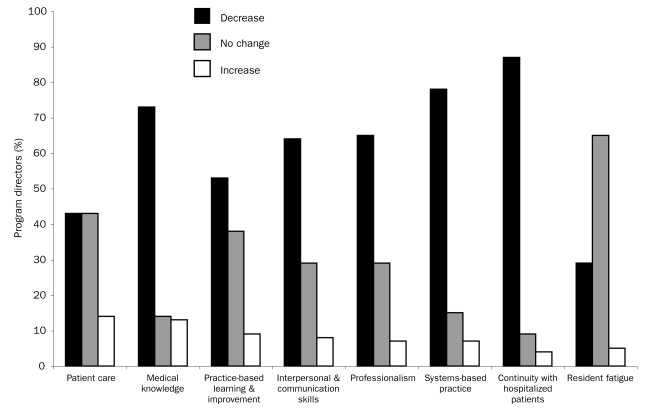
As the Figure shows, most respondents believe that the new ACGME recommendations will decrease residents' ability to achieve continuity with hospitalized patients (404/464 [87%]) and will have no change on (303/464 [65%]) or will actually increase (26/464 [6%]) resident fatigue.
FIGURE.
Faculty views of the implications of new duty hour recommendations for core competencies.
Regarding the 6 ACGME core competencies, the vast majority of program directors believe that the new duty hour regulations will decrease both the coordination of patient care (363/464 [78%]) and residents' overall educational experience (337/464 [73%]). Over half of the directors reported that there will likely be a decrease in residents' responsiveness to patient needs (301/464 [65%]); residents' ability to effectively communicate with patients, families, and other health care professionals (293/464 [63%]); and residents' investigation and self-evaluation of their own patient care (249/464 [54%]). Residency program directors were evenly divided regarding how changes in the ACGME recommendations would affect quality and safety of patient care, with 43% (199/464) believing that the changes will result in a decrease in quality and safety and 43% (200/464) believing that no change will occur.
Factors Associated With Program Directors' Views of the Implications of New Duty Hour Recommendations for Core Competencies. In univariate logistic regression models, age and sex of program directors were not significantly associated with beliefs about changes due to ACGME proposals. However, program directors' specialty (ie, medicine, pediatrics, or surgery) was related. Program directors from the Northeast were less likely than program directors from the South to believe that residents' overall educational experience would decrease (OR, 0.6; 95% CI, 0.3-1.0). Also, program directors from the Midwest and Northeast were significantly less likely than program directors from the South to believe that the ACGME policy changes would decrease residents' interpersonal and communication skills (OR, 0.6; 95% CI, 0.3-1.0; for both Midwest and Northeast).
In multivariate logistic regression models, adjusting for age, sex, and geographic region, academic rank and years as program director were not significantly associated with beliefs about changes due to ACGME recommendations. However, program directors' specialty, average hours per week of direct teaching or supervision of residents, and self-reported program type were associated with the directors' ratings of how the ACGME recommendations will affect components of residency programs.
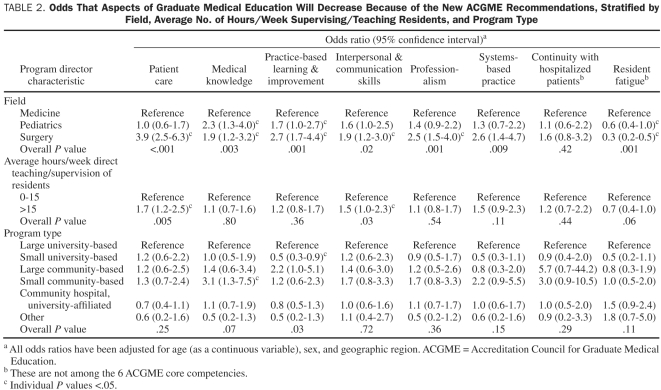
As shown in Table 2, general surgery program directors were significantly more likely than internal medicine program directors to believe that the ACGME recommendations will decrease the quality of patient care (OR, 3.9; 95% CI, 2.5-6.3), residents' overall educational experience (OR, 1.9; 95% CI, 1.2-3.2), practice-based learning and improvement (OR, 2.7; 95% CI, 1.7-4.4), interpersonal and communication skills (OR, 1.9; 95% CI, 1.2-3.0), and responsiveness to patients' needs (OR, 2.5; 95% CI, 1.5-4.0). They were also 70% less likely than internal medicine directors to believe the ACGME recommendations will improve resident fatigue (OR, 0.3; 95% CI, 0.2-0.5). Similarly, pediatrics program directors were significantly more likely than internal medicine directors to believe that the recommendations will decrease residents' overall educational experience (OR, 2.2; 95%, CI 1.3-4.0) and interpersonal and communication skills (OR, 1.6; 95% CI, 1.0-2.5), but they were significantly less likely to believe they would decrease resident fatigue (OR, 0.6; 95% CI, 0.4-1.0).
TABLE 2.
Odds That Aspects of Graduate Medical Education Will Decrease Because of the New ACGME Recommendations, Stratified by Field, Average No. of Hours/Week Supervising/Teaching Residents, and Program Type
Compared with those who reported spending little time in direct teaching or supervision of residents, program directors spending more than 15 hours per week in this capacity were significantly more likely to believe that the ACGME recommendations will decrease the quality and safety of patient care (OR, 1.7; 95% CI, 1.2-2.5) as well as residents' ability to effectively communicate with patients, families, and other health care professionals (OR, 1.5; 95% CI, 1.0-2.3).
Finally, directors who identified their programs as being small community-based were more likely to believe that the ACGME recommendations would decrease residents' overall educational experience (OR, 3.1; 95% CI, 1.3-7.5); however, directors of small university-based programs were less likely to believe that the changes would result in diminished practice-based learning and improvement among residents (OR, 0.5; 95% CI, 0.3-0.9) compared with directors of large university-based programs.
DISCUSSION
The results of this study provide important insight into the concerns of those who are most directly responsible for implementing the proposed ACGME duty hour recommendations while maintaining a high-quality graduate medical educational experience for residents. In this nationwide assessment of program directors' reactions to ACGME duty hour recommendations, we found a marked degree of concern about educating a competent generation of future physicians in the face of increasing duty hour standards and regulation.
The large majority of residency program directors reported that continuity with hospitalized patients will decrease under the new ACGME recommendations. As duty hours are reduced, it logically follows that transfers of care will increase25 and that continuity will decrease. These data are consistent with previous research that showed that faculty and residents believed that the 80-hour work week compromised continuity of care.26-29 As duty hour restrictions increase, teamwork, communication, and coordination will be essential to lessen the effects of decreased continuity of care.
We were somewhat surprised to learn that a substantial proportion of program directors believed that further reductions in duty hours will not reduce resident fatigue. Pri- or studies show that residents report less fatigue with duty hour limits.30-33 However, research that objectively quantifies residents' sleep shows only modest gains in sleep time with shift reduction34 and strategic napping.35,36 A recent study of pediatric interns at the Cincinnati Children's Hospital Medical Center found that residents who followed the 2008 IOM duty hour guidelines increased their sleep by only 0.2 hours per 24-hour period.37 However, the actual effects of sleep deprivation on patient care remain to be determined. Although several studies have documented adverse effects of sleep deprivation on clinical performance38-40 and a recent study suggested an association between fatigue and self-perceived medical errors,41 whether a reduction in duty hours will actually translate into better outcomes for patients is still unclear. Studies that examined the effects of the ACGME's 2003 duty hour recommendations on patient safety have shown mixed results, with some studies reporting improvements in patient outcomes and other studies showing worsening of outcomes.42-48
Over half of the program directors believe that the new duty hour restrictions will decrease residents' ability to develop competency in 5 of the 6 core areas (all but the patient care competency, in which views were divided). This troubling finding highlights program directors' appreciable concerns about the implications of the new recommendations on residents' education. Although program directors in all 3 specialties reported some degree of concern, the differing responses from internal medicine, pediatrics, and general surgery program directors prompt the question of whether the different specialties may legitimately have different needs regarding patient care hours during training. Surgical program directors perceived more ill effects than did internal medicine and pediatrics program directors. Surgeons' reservations about further duty hour limits may stem from multiple studies that demonstrated reduced operative experience for residents after the 2003 duty hour regulations.49-52 Furthermore, internal medicine and pediatrics program directors may be less concerned than surgeons about duty hour changes, in part because internal medicine and pediatrics residency programs have had specialty-specific duty hour limitations predating the 2003 ACGME duty hour limitations for all residencies and fellowships.14
Directors of small community-based programs were nearly 3 times more likely to believe that the duty hour changes will decrease residents' overall educational experience compared with directors of large university-based programs. Programs with fewer residents and faculty may face greater challenges in implementing the proposed recommendations, especially shift length restrictions and supervision standards, which may require additional personnel to achieve compliance. To meet prior duty hour standards, many programs implemented night float rotations or hired midlevel professionals1,3; however, it may be difficult to make night float rotations educationally valuable,53,54 and smaller programs may not have sufficient resources to hire additional personnel or cover other costs of the proposed reforms.55
Our study has several important limitations to consider when assessing the generalizability of the results. Attitudinal associations found in this cross-sectional study may not be stable. If we surveyed program directors after the recommendations take effect (July 2011), they may have adjusted to those recommendations more than in the immediate weeks after the recommendations were released. Also, respondents may be susceptible to how items were worded. Nevertheless, given that the measures adapt existing ACGME language, we believe our approach has face validity. Moreover, although we achieved a two-thirds response rate, it is possible that the responses from the program directors who did not respond to the survey or the 10% of program directors who could not be contacted because their e-mail addresses were not publicly available may differ from those who did respond. However, there are no a priori reasons to suggest that these program directors would significantly differ from our sample. Furthermore, these data reflect only the views of program directors in internal medicine, pediatrics, and general surgery. As the new recommendations are weighed for adoption and implementation, it will be important to consider the perspectives and needs of program directors across all medical specialties. Finally, to decrease survey burden, we limited ourselves to measuring only 1 statement that represented each of the 6 core competencies.
CONCLUSION
Notwithstanding the limitations of our study, the results suggest that the new duty hour restrictions have the potential to create serious difficulties for residency programs to ensure that their trainees are meeting the ACGME core competencies. These data also suggest that programs may be differentially affected on the basis of specialty and program size. Although serious challenges remain regarding the necessary funding of duty hour regulations55 and enforcing those regulations,56 more work that specifically addresses “residency as a time for learning”14 is required to build evidenced-based work hour regulations to ensure the development of the next generation of highly competent medical professionals.57
Supplementary Material
Acknowledgments
We thank Sarah M. Jenkins, MS, for statistical review of the manuscript, and Furman S, McDonald, MD, MPH, for review of the manuscript and suggestions.
REFERENCES
- 1. Fletcher KE, Davis SQ, Underwood W, Mangrulkar RS, McMahon LF, Jr, Saint S. Systematic review: effects of resident work hours on patient safety. Ann Intern Med. 2004;141(11)851-857 [DOI] [PubMed] [Google Scholar]
- 2. Hutter MM, Kellogg KC, Ferguson CM, Abbott WM, Warshaw AL. The impact of the 80-hour resident workweek on surgical residents and attending surgeons. Ann Surg. 2006;243(6)864-871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fletcher KE, Underwood W, III, Davis SQ, Mangrulkar RS, McMahon LF, Jr, Saint S. Effects of work hour reduction on residents' lives: a systematic review. JAMA. 2005;294(9)1088-1100 [DOI] [PubMed] [Google Scholar]
- 4. Barrack RL, Miller LS, Sotile WM, Sotile MO, Rubash HE. Effect of duty hour standards on burnout among orthopaedic surgery residents. Clin Orthop Relat Res. 2006;449:134-137 [DOI] [PubMed] [Google Scholar]
- 5. Gopal R, Glasheen JJ, Miyoshi TJ, Prochazka AV. Burnout and internal medicine resident work-hour restrictions. Arch Intern Med. 2005;165(22)2595-2600 [DOI] [PubMed] [Google Scholar]
- 6. Martin–i S, Arfken CL, Balon R. Comparison of burnout among medical residents before and after the implementation of work hours limits. Acad Psychiatry. 2006;30(4)352-355 [DOI] [PubMed] [Google Scholar]
- 7. Rybock JD. Residents' duty hours and professionalism. N Engl J Med. 2009;361(9)930-931 [DOI] [PubMed] [Google Scholar]
- 8. Accreditation Council for Graduate Medical Education Common Program Requirements 2010. ACGME Web site. http://acgme-2010standards.org Accessed November 5, 2010
- 9. Antiel RM, Thompson SM, Reed DA, et al. ACGME duty-hour recommendations—findings from a national survey of residency program directors. N Engl J Med. 2010;363:e12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nasca T, Day S, Amis EJ, ACGME Duty Hour Task Force The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;363(2):e3 [DOI] [PubMed] [Google Scholar]
- 11. Asch DA, Parker RM. The Libby Zion case: one step forward or two steps backward? N Engl J Med. 1988;318(12)771-775 [DOI] [PubMed] [Google Scholar]
- 12. Brensilver JM, Smith L, Lyttle CS. Impact of the Libby Zion case on graduate medical education in internal medicine. Mt Sinai J Med. 1998;65(4)296-300 [PubMed] [Google Scholar]
- 13. Reiner SC. The impact of the new code regulations on postgraduate medical education in New York State. N Y State J Med. 1989;89(8)457-461 [PubMed] [Google Scholar]
- 14. Philibert I, Friedmann P, Williams WT. New requirements for resident duty hours. JAMA. 2002;288(9)1112-1114 [DOI] [PubMed] [Google Scholar]
- 15. Institute of Medicine Resident Duty Hours: Enhancing Sleep, Supervision, and Safety. Washington, DC: National Academies Press; 2008. [PubMed] [Google Scholar]
- 16. Okie S. An elusive balance—residents' work hours and the continuity of care. N Engl J Med. 2007;356(26)2665-2667 [DOI] [PubMed] [Google Scholar]
- 17. Potee RA. Limiting residents' work hours [letter]. JAMA. 2002;288(23)2973-2974 [PubMed] [Google Scholar]
- 18. Steinbrook R. The debate over residents' work hours. N Engl J Med. 2002;347(16)1296-1302 [DOI] [PubMed] [Google Scholar]
- 19. Batalden PB, Leach DC. Sharpening the focus on systems-based practice [editorial]. J Grad Med Educ. 2009;1(1)1-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Green ML, Holmboe E. Perspective: the ACGME toolbox: half empty or half full? Acad Med. 2010;85(5)787-790 [DOI] [PubMed] [Google Scholar]
- 21. Lurie SJ, Mooney CJ, Lyness JM. Measurement of the general competencies of the Accreditation Council for Graduate Medical Education: a systematic review. Acad Med. 2009;84(3)301-309 [DOI] [PubMed] [Google Scholar]
- 22. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2)377-381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Accreditation Council for Graduate Medical Education Common program requirements: general competencies. Published February 13, 2007. http://www.acgme.org/outcome/comp/GeneralCompetenciesStandards21307.pdf Accessed November 24, 2010
- 24. Accreditation Council for Graduate Medical Education List of ACGME Accredited Programs and Sponsoring Institutions. http://www.acgme.org/ads-public Accessed November 24, 2010
- 25. Horwitz LI, Krumholz HM, Green ML, Huot SJ. Transfers of patient care between house staff on internal medicine wards: a national survey. Arch Intern Med. 2006;166(11)1173-1177 [DOI] [PubMed] [Google Scholar]
- 26. Barden CB, Specht MC, McCarter MD, Daly JM, Fahey TJ., III Effects of limited work hours on surgical training. J Am Coll Surg. 2002;195(4)531-538 [DOI] [PubMed] [Google Scholar]
- 27. Cohen-Gadol AA, Piepgras DG, Krishnamurthy S, Fessler RD. Resident duty hours reform: results of a national survey of the program directors and residents in neurosurgery training programs. Neurosurgery. 2005;56(2)398-403 [DOI] [PubMed] [Google Scholar]
- 28. Lieberman JD, Olenwine JA, Finley W, Nicholas GG. Residency reform: anticipated effects of ACGME guidelines on general surgery and internal medicine residency programs. Curr Surg. 2005;62(2)231-236 [DOI] [PubMed] [Google Scholar]
- 29. Lin GA, Beck DC, Garbutt JM. Residents' perceptions of the effects of work hour limitations at a large teaching hospital. Acad Med. 2006;81(1)63-67 [DOI] [PubMed] [Google Scholar]
- 30. Basu CB, Chen LM, Hollier LH, Jr, Shenaq SM. The effect of the Accreditation Council for Graduate Medical Education Duty Hours Policy on plastic surgery resident education and patient care: an outcomes study. Plast Reconstr Surg. 2004;114(7)1878-1886 [DOI] [PubMed] [Google Scholar]
- 31. Goldstein MJ, Kim E, Widmann WD, Hardy MA. A 360 degrees evaluation of a night-float system for general surgery: a response to mandated work-hours reduction. Curr Surg. 2004;61(5)445-451 [DOI] [PubMed] [Google Scholar]
- 32. Kort KC, Pavone LA, Jensen E, Haque E, Newman N, Kittur D. Resident perceptions of the impact of work-hour restrictions on health care delivery and surgical education: time for transformational change. Surgery. 2004;136(4)861-871 [DOI] [PubMed] [Google Scholar]
- 33. Seelig CB. Changes in residents' attitudes in response to residency program modifications: a prospective study. South Med J. 1992;85(10)972-975 [DOI] [PubMed] [Google Scholar]
- 34. Lockley SW, Cronin JW, Evans EE, et al. Effect of reducing interns' weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351(18)1829-1837 [DOI] [PubMed] [Google Scholar]
- 35. Arora V, Dunphy C, Chang VY, Ahmad F, Humphrey HJ, Meltzer D. The effects of on-duty napping on intern sleep time and fatigue. Ann Intern Med. 2006;144(11)792-798 [DOI] [PubMed] [Google Scholar]
- 36. Richardson GS, Wyatt JK, Sullivan JP, et al. Objective assessment of sleep and alertness in medical house staff and the impact of protected time for sleep. Sleep. 1996;19(9)718-726 [PubMed] [Google Scholar]
- 37. Auger KA, Sieplinga KR, Simmons JM, Gonzalez del Rey JA. Educational implications and sleep and fatigue implications of the 2008 proposed work hour regulations: pilot studies. Academic Pediatrics. 2010;10(4):e5 [Google Scholar]
- 38. Koslowsky M, Babkoff H. Meta-analysis of the relationship between total sleep deprivation and performance. Chronobiol Int. 1992;9(2)132-136 [DOI] [PubMed] [Google Scholar]
- 39. Leung L, Becker CE. Sleep deprivation and house staff performance: update 1984-1991. J Occup Med. 1992;34(12)1153-1160 [PubMed] [Google Scholar]
- 40. Samkoff JS, Jacques CH. A review of studies concerning effects of sleep deprivation and fatigue on residents' performance. Acad Med. 1991;66(11)687-693 [DOI] [PubMed] [Google Scholar]
- 41. West CP, Tan AD, Habermann TM, Sloan JA, Shanafelt TD. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302(12)1294-1300 [DOI] [PubMed] [Google Scholar]
- 42. Bhavsar J, Montgomery D, Li J, et al. Impact of duty hours restrictions on quality of care and clinical outcomes. Am J Med. 2007;120(11)968-974 [DOI] [PubMed] [Google Scholar]
- 43. Prasad M, Iwashyna TJ, Christie JD, et al. Effect of work-hours regulations on intensive care unit mortality in United States teaching hospitals. Crit Care Med. 2009;37(9)2564-2569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Volpp KG, Rosen AK, Rosenbaum PR, et al. Mortality among patients in VA hospitals in the first 2 years following ACGME resident duty hour reform. JAMA. 2007;298(9)984-992 [DOI] [PubMed] [Google Scholar]
- 45. Landrigan CP, Fahrenkopf AM, Lewin D, et al. Effects of the Accreditation Council for Graduate Medical Education duty hour limits on sleep, work hours, and safety. Pediatrics. 2008;122(2)250-258 [DOI] [PubMed] [Google Scholar]
- 46. Rosen AK, Loveland SA, Romano PS, et al. Effects of resident duty hour reform on surgical and procedural patient safety indicators among hospitalized Veterans Health Administration and Medicare patients. Med Care. 2009;47(7)723-731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Shetty KD, Bhattacharya J. Changes in hospital mortality associated with residency work-hour regulations. Ann Intern Med. 2007;147(2)73-80 [DOI] [PubMed] [Google Scholar]
- 48. Volpp KG, Rosen AK, Rosenbaum PR, et al. Mortality among hospitalized Medicare beneficiaries in the first 2 years following ACGME resident duty hour reform. JAMA. 2007;298(9)975-983 [DOI] [PubMed] [Google Scholar]
- 49. Carlin AM, Gasevic E, Shepard AD. Effect of the 80-hour work week on resident operative experience in general surgery. Am J Surg. 2007;193(3)326-329 [DOI] [PubMed] [Google Scholar]
- 50. Damadi A, Davis AT, Saxe A, Apelgren K. ACGME duty-hour restrictions decrease resident operative volume: a 5-year comparison at an ACGME-accredited university general surgery residency. J Surg Educ. 2007;64(5)256-259 [DOI] [PubMed] [Google Scholar]
- 51. Kairys JC, McGuire K, Crawford AG, Yeo CJ. Cumulative operative experience is decreasing during general surgery residency: a worrisome trend for surgical trainees? J Am Coll Surg. 2008;206(5)804-811 [DOI] [PubMed] [Google Scholar]
- 52. Weatherby BA, Rudd JN, Ervin TB, Stafford PR, Norris BL. The effect of resident work hour regulations on orthopaedic surgical education. J Surg Orthop Adv. 2007;16(1)19-22 [PubMed] [Google Scholar]
- 53. Jasti H, Hanusa BH, Switzer GE, Granieri R, Elnicki M. Residents' perceptions of a night float system. BMC Med Educ. 2009;9:52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Rosenberg M, McNulty D. Beyond night float? the impact of call structure on internal medicine residents. J Gen Intern Med. 1995;10(2)95-98 [DOI] [PubMed] [Google Scholar]
- 55. Nuckols TK, Bhattacharya J, Wolman DM, Ulmer C, Escarce JJ. Cost implications of reduced work hours and workloads for resident physicians. N Engl J Med. 2009;360(21)2202-2215 [DOI] [PubMed] [Google Scholar]
- 56. Accreditation Council for Graduate Medical Education The ACGME's approach to limit resident duty hours 2007-08: a summary of achievements for the fifth year under the common requirements. http://www.acgme.org/acwebsite/dutyhours/dh_achievesum0708.pdf Accessed November 24, 2010
- 57. Volpp KG, Landrigan CP. Building physician work hour regulations from first principles and best evidence. JAMA. 2008;300(10)1197-1199 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.