Abstract
OBJECTIVE: To determine whether standardized admissions data in residents' Electronic Residency Application Service (ERAS) submissions were associated with multisource assessments of professionalism during internship.
PARTICIPANTS AND METHODS: ERAS applications for all internal medicine interns (N=191) at Mayo Clinic entering training between July 1, 2005, and July 1, 2008, were reviewed by 6 raters. Extracted data included United States Medical Licensing Examination scores, medicine clerkship grades, class rank, Alpha Omega Alpha membership, advanced degrees, awards, volunteer activities, research experiences, first author publications, career choice, and red flags in performance evaluations. Medical school reputation was quantified using U.S. News & World Report rankings. Strength of comparative statements in recommendation letters (0 = no comparative statement, 1 = equal to peers, 2 = top 20%, 3 = top 10% or “best”) were also recorded. Validated multisource professionalism scores (5-point scales) were obtained for each intern. Associations between application variables and professionalism scores were examined using linear regression.
RESULTS: The mean ± SD (minimum-maximum) professionalism score was 4.09±0.31 (2.13-4.56). In multivariate analysis, professionalism scores were positively associated with mean strength of comparative statements in recommendation letters (β=0.13; P=.002). No other associations between ERAS application variables and professionalism scores were found.
CONCLUSION: Comparative statements in recommendation letters for internal medicine residency applicants were associated with professionalism scores during internship. Other variables traditionally examined when selecting residents were not associated with professionalism. These findings suggest that faculty physicians' direct observations, as reflected in letters of recommendation, are useful indicators of what constitutes a best student. Residency selection committees should scrutinize applicants' letters for strongly favorable comparative statements.
Comparative statements in recommendation letters for internal medicine residency applicants were associated with professionalism scores during internship, suggesting that faculty physicians' direct observations are useful indicators of what constitutes a best student.
AOA = Alpha Omega Alpha; ERAS = Electronic Residency Application Service; USMLE = US Medical Licensing Examination
Professionalism is an expected attribute of all physicians and a core competency of the Accreditation Council for Graduate Medical Education.1 However, identifying residency applicants who will perform professionally is challenging. In 1995, the Association of American Medical Colleges created the Electronic Residency Application Service (ERAS) to facilitate medical students' applications to US residency programs.2 Medical school deans and medical students place application information into ERAS for electronic distribution to residency programs. The ERAS system contains data regarding applicants' medical school performance, including class rank and clerkship grades, research and volunteer experiences, recommendation letters, gaps in training, adverse actions, and academic remediation. Residency selection committees rely on these data for important decisions about selecting applicants. Unfortunately, despite the widespread use of ERAS data for resident selection, limited research exists regarding whether these data are associated with residency applicants' professional behaviors during subsequent years of training.
Lack of professionalism among medical learners carries negative consequences. For example, delinquent behaviors during preclinical years have been associated with lower professionalism scores on third-year clerkship evaluations.3 Unprofessional behaviors in both medical school and residency have been shown to predict disciplinary action by state medical licensing boards,4-6 and disruptive residents often have low professionalism scores.7 Conversely, highly professional behaviors in residency have been linked to conscientiousness, medical knowledge, and clinical skills.8
Much research has examined best practices for measuring professionalism.9,10 Experts suggest that professionalism assessments should reflect numerous observations from multiple individuals in realistic contexts over time.10 The purpose of the assessments should be transparent, and assessment standards should apply equally to all.10 We used these principles to assess residents' professionalism at Mayo Clinic via multisource ratings completed by faculty, peers, and nonphysician professionals.8 This professionalism assessment method has been shown to be reliable and valid.8
Few studies have explored the relationship between admission criteria and professional behavior among medical learners. Stern et al3 found no association between medical school admission packet materials and professionalism in medical school. We are unaware of previous studies examining associations between admission criteria for internal medicine residency applicants and subsequent professional behaviors during residency. Therefore, we determined whether selection criteria obtained from ERAS for national and international applicants to a large internal medicine residency program were associated with validated, observation-based ratings of professionalism during subsequent training.
PARTICIPANTS AND METHODS
We conducted a retrospective cohort study of all first-year categorical internal medicine residents (N=191) at Mayo Clinic who began training from July 1, 2005, through July 1, 2008 (4 consecutive classes of residents). We sought to examine associations between standard residency selection and professionalism ratings during internship. This study was deemed exempt from review by the Mayo Clinic Institutional Review Board.
Six raters (M.W.C., D.A.R., C.M.W., L.M.B.K., M.T.K., and T.J.B.) extracted internal medicine residency applicant characteristics from ERAS on a number of independent variables (Table 1). To assess the reliability of the data collection process, 15 randomly selected applications were scored by one of the 15 possible unique pairings of the 6 raters.
TABLE 1.
Independent Variables Used in Abstracting Data From ERAS Applicationsa
Assessment of Professionalism
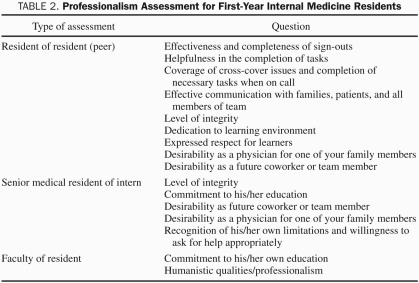
Residents' professionalism was assessed using a multisource professionalism score consisting of observation-based assessments. Scores were collected from peers who worked with the interns for at least 1 month, third-year residents who provided supervision for at least 1 month, and faculty physicians who provided supervision for at least 2 weeks. The professionalism assessment included 16 items structured on a 5-point scale (1 = needs improvement, 3 = average resident, 5 = top 10%; Table 2).Validity for this professionalism assessment has been previously demonstrated. Specifically, content validity was established by items that represent known professionalism domains and best practices.9-13 Internal structure validity was supported by items representing a multidimensional assessment of professionalism with demonstrated internal consistency reliability.8 Criterion validity was evidenced by associations between resident professionalism scores and in-training examination knowledge scores, Mini-Clinical Evaluation Exercise scores, and conscientious behaviors.8
TABLE 2.
Professionalism Assessment for First-Year Internal Medicine Residents
Statistical Analyses
Scores from professionalism assessments were averaged by resident to form a continuous overall mean professionalism score ranging from 1 to 5. Interrater reliability for abstraction of ERAS variables was determined using the Cohen κ for nominally scaled variables and intraclass correlation coefficients for ordinally scaled variables.
Associations between data abstracted from ERAS applications (the independent variables) and mean professionalism score (the dependent variable) were examined using simple and multiple linear regression. Given the large number of study participants assigned to the 50th percentile because of unreported data, a multiple linear regression model ignoring class rank was also fit. Medical school rankings from U.S. News & World Report were available for US medical school graduates only. They were assessed in a secondary analysis restricted to this subset of residents. To account for multiple comparisons, an α level of .01 was used to determine statistical significance. This sample of 191 residents provided 84% power to detect a Cohen f2 effect size of 0.15 in the multiple linear regression model associating each resident's mean professionalism score with his or her 13 ERAS variable values. All calculations were performed using SAS statistical software, version 9.1 (SAS Institute, Cary, NC).
RESULTS
This study included 191 interns and 36,512 professionalism assessments from the 2005-2006 through 2008-2009 academic years. The sample included all eligible residents from the 4 classes studied. The mean ± SD age of the study population was 28.4±3.0 years. Each resident's mean professionalism score was based on a mean ± SD (range) of 191.2±25.1 (30-248) evaluations. For the 191 residents, the mean ± SD (minimum-maximum) professionalism score was 4.09±0.31 (2.13-4.56). The sample included 68 female residents (35.6%) and 35 international medical school graduates (18.3%).
Interrater agreement for the nominally scaled variables,14 including Alpha Omega Alpha (AOA) membership, presence of advanced degree, indication of career choice, and presence of red flags was good (mean Cohen κ, 0.66).15 Interrater agreement for the ordinally scaled variables, including number of awards, volunteer experiences, research experiences, first author publications, medicine clerkship percentile, class rank, and average strength of comparative statements in letters, was excellent (mean intraclass correlation coefficient, 0.92).15
ERAS Application Variables
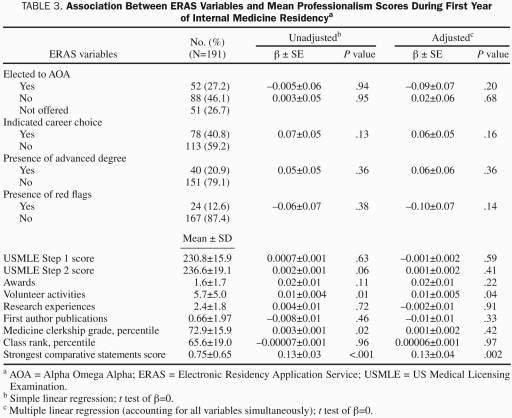
Table 3 provides the mean ± SD for each of the ERAS application variables. The ERAS applications of the 191 residents in our cohort contained 725 distinct letters of recommendation. Of those 725 letters, 115 (15.9%) received a score of “3” for most enthusiastic comparative statement, 97 (13.4%) received a score of “2” for moderately enthusiastic comparative statement, and 10 (1.4%) received a score of “1” for a neutral comparative statement. The remainder of the letters of recommendation (503, 69.4%) contained no comparative statements. Of the 191 applicants, 37 (19.4%) received a score of “3” as their strongest comparative statement, 23 (12.0%) received a score of “2,” and 25 (13.1%) received a score of “1.” No comparative statement was available for the remaining 106 residents (55.5%).
TABLE 3.
Association Between ERAS Variables and Mean Professionalism Scores During First Year of Internal Medicine Residencya
Information on the academic rank of the letter writer was available for 573 of the 725 recommendation letters: 264 (46.1%) were authored by full professors, 120 (20.9%) by associate professors, 149 (26.0%) by assistant professors, 13 (2.3%) by instructors, and 27 (4.7%) by community physicians. Using generalized estimating equations to account for the correlation of letters within each application, no association between the strongest comparative statement and academic rank of the letter writer was found (all, P>.13).
Associations Between ERAS Application Variables and Mean Professionalism Scores
In the unadjusted model, volunteer activities (P=.01) and the average strongest comparative statement (P<.001) were significantly associated with mean professionalism score. In multivariate analysis, only the strongest comparative statement in letters of recommendation remained significant (P=.002). A 1-point increase in the average strongest comparative statement was associated with a 0.13-point increase in mean professionalism score (β=0.13; 95% confidence interval, 0.05-0.20). Thus, a 1-unit increase in the rating of comparative statements was associated with a 0.13 increase in the mean professionalism score during internship. This regression estimate approximates one-half the SD of the mean professionalism scores in the sample. This finding remained unchanged in the multiple linear regression model excluding class rank.
Results were unchanged after incorporating the U.S. News and World Report medical school rankings into an analysis of the 156 US medical school graduates. Medical school ranking was not significantly associated with mean professionalism scores in either unadjusted (P=.91) or adjusted (P=.65) models. In the adjusted model, the average strongest comparative statement remained the only independent variable significantly associated with mean professionalism scores (P=.001; β=0.14; 95% confidence interval, 0.06-0.23).
DISCUSSION
This study demonstrated that the strength of comparative statements in applicants' letters of recommendation were positively associated with professionalism during internship, whereas other variables traditionally examined among applicants were not. To our knowledge, this is the first study to assess the association between comprehensive ERAS application variables and validated professionalism scores during subsequent training in internal medicine.
It is noteworthy that most of the application variables that residency programs typically consider when choosing residents, such as medical school reputation, AOA status, US Medical Licensing Examination (USMLE) scores, and clerkship grades, were not associated with professionalism during internship. This finding challenges the role of these variables in the selection of professional residents. Standard application variables (eg, USMLE scores and clerkship grades) predict medical knowledge and clinical performance16-19 and should thus be appraised during the selection process. However, such variables may not be sufficiently robust for identifying residents who will consistently uphold professional values. Residency programs are best served to identify professionalism during the application process because patients highly value professionalism among physicians1,20 and residents who cause disruptions often demonstrate deficiencies in professionalism.7
Although most ERAS variables were not associated with professionalism, this study identified an association between comparative statements in letters of recommendation and multisource professionalism ratings during internship. This association was independent of writer experience because no relationship was found between letter writers' academic ranks and their strongest comparative statements. Our findings underscore the strength of observation-based assessment.21 Previous work has found a low frequency of comparative statements in letters of recommendation22,23 and little correlation between letters of recommendation and subsequent clinical performance.24-27 This lack of correlation is likely because these studies did not specifically identify comparative statements within letters25-27 or did not examine associations between letter content and professionalism scores that reflected observations of learners in realistic settings.24 Our study specifically analyzed statements in letters that compared students to their peers. Furthermore, both letters of recommendation and our multisource professionalism ratings are based on first-hand observations of learners in clinical contexts over time. Our findings suggest that letters of recommendation can be strong markers of observation-based assessment in a residency application. Conversely, most other ERAS variables, such as USMLE scores, AOA status, and medical school reputation, do not involve direct observations of learners and thus may be less useful indicators of subsequent professional behavior. Therefore, residency program selection committees should consider scrutinizing letters of recommendation for observation-based comparative statements.
Our study extends the literature on application variables and trainee performance. Most prior research has involved medical students.3,28-30 Studies of residents have focused on medical knowledge and clinical skills.16,19,31 In the domain of professionalism, negative comments in the Medical Student Performance Evaluation have been associated with poor professionalism among psychiatry residents.32 Additionally, third-year medicine clerkship grades have been associated with professionalism ratings during internship.18 However, this study incorporated fewer independent variables and measured professionalism using a one-time survey of program directors.18 In contrast, our study examined a wide range of application variables and used a multisource mean professionalism score consisting of numerous observation-based assessments of residents over the course of the internship. Furthermore, our validated professionalism assessment contains authoritative item content, reliable scores, and demonstrated associations between professionalism ratings and medical knowledge, clinical competence, and dutifulness.8
This study has some limitations. First, it was conducted at a single institution, and so additional studies are needed to further generalize the findings. However, the independent variables in this study, obtained from ERAS, are widely used by US residency programs. Second, some independent variables were not available for all candidates (ie, AOA status). Third, U.S. News & World Report rankings have been criticized for lacking objective quality measurements.33 Nonetheless, these rankings are commonly used to judge medical school quality. Fourth, grading the strength of comparative statements in candidates' letters of recommendation may be labor intensive. However, given the meaningful association with subsequent professionalism, we suggest that inspecting letters of recommendation for strongly positive comparative statements will enhance the ability to select highly professional residents. Fifth, comparative statements in clerkship directors' and department chairs' letters may not have involved direct observation. However, these comparative statements did reflect direct observations from the writers' colleagues, and the letters by clerkship directors and department chairs represented only a minority of the sample. Sixth, although we assumed that faculty members routinely observed the students assigned to them on clinical rotations, it is possible that, in rare instances, only limited amounts of observation occurred. Seventh, few applicants had information regarding “red flags” and specific career intent in their applications, which limited our ability to detect associations for these variables. Finally, although the professionalism outcome in this study was based on multisource assessments, which is a single method of measuring professionalism, our multisource assessment represents a best practice10 and was previously validated.8
CONCLUSION
We found that strongly favorable comparative statements in the recommendation letters for internal medicine residency applicants were associated with multisource assessments of professionalism during internship. This finding suggests that faculty members' observation-based assessments of students are powerful indicators of what constitutes a best student. Furthermore, this finding offers residency selection committees a useful tool for selecting applicants who may perform professionally during internship. Future research should examine associations between variables in ERAS and professionalism in later years of training and practice. Future work should also determine the relationships between these variables and other outcomes, including medical knowledge and clinical skills.
REFERENCES
- 1. Accreditation Council for Graduate Medical Education (ACGME) ACGME Outcome project. http://www.acgme.org/outcome/implement/rsvp.asp Accessed January 18, 2011
- 2. Association of American Medical Collegers (AAMC) Electronic Residency Application Service. https://www.aamc.org/services/eras/ Accessed January 18, 2011
- 3. Stern DT, Frohna AZ, Gruppen LD. The prediction of professional behaviour. Med Educ. 2005;39(1)75-82 [DOI] [PubMed] [Google Scholar]
- 4. Papadakis MA, Teherani A, Banach MA, et al. Disciplinary action by medical boards and prior behavior in medical school. N Engl J Med. 2005;353(25):2673-2682 [DOI] [PubMed] [Google Scholar]
- 5. Papadakis MA, Hodgson CS, Teherani A, Kohatsu ND. Unprofessional behavior in medical school is associated with subsequent disciplinary action by a state medical board. Acad Med. 2004;79(3)244-249 [DOI] [PubMed] [Google Scholar]
- 6. Papadakis MA, Arnold GK, Blank LL, Holmboe ES, Lipner RS. Performance during internal medicine residency training and subsequent disciplinary action by state licensing boards. Ann Intern Med. 2008;148(11)869-876 [DOI] [PubMed] [Google Scholar]
- 7. Yao DC, Wright SM. National survey of internal medicine residency program directors regarding problem residents. JAMA. 2000;284(9)1099-1104 [DOI] [PubMed] [Google Scholar]
- 8. Reed DA, West CP, Mueller PS, Ficalora RD, Engstler GJ, Beckman TJ. Behaviors of highly professional resident physicians. JAMA. 2008;300(11):1326-1333 [DOI] [PubMed] [Google Scholar]
- 9. Arnold L. Assessing professional behavior: yesterday, today, and tomorrow. Acad Med. 2002;77(6)502-515 [DOI] [PubMed] [Google Scholar]
- 10. Stern DT. Measuring Medical Professionalism. New York, NY: Oxford University Press Inc; 2006. [Google Scholar]
- 11. American Board of Internal Medicine (ABIM) Project Professionalism. Philadelphia, PA: American Board of Internal Medicine; 2002. [Google Scholar]
- 12. Arnold L, Stern DT. What is Medical Professionalism? New York, NY: Oxford University Press; 2006. [Google Scholar]
- 13. Norcini J. Faculty observations of student professional behavior. In: Stern DT, ed. Measuring Medical Professionalism. New York, NY: Oxford University Press; 2006:147-157 [Google Scholar]
- 14. Kundel HL, Polansky M. Measurement of observer agreement. Radiology. 2003;228(2)303-308 [DOI] [PubMed] [Google Scholar]
- 15. Landis JR, Koch GG. The measure of observer agreement for categorical data. Biometrics. 1977;33(1)159-174 [PubMed] [Google Scholar]
- 16. Andriole DA, Jeffe DB, Whelan AJ. What predicts surgical internship performance? Am J Surg. 2004;188(2)161-164 [DOI] [PubMed] [Google Scholar]
- 17. Durning SJ, Pangaro LN, Lawrence LL, Waechter D, McManigle J, Jackson JL. The feasibility, reliability, and validity of a program director's (supervisor's) evaluation form for medical school graduates. Acad Med. 2005;80(10)964-968 [DOI] [PubMed] [Google Scholar]
- 18. Greenburg DL, Durning SJ, Cohen DL, Cruess D, Jackson JL. Identifying medical students likely to exhibit poor professionalism and knowledge during internship. J Gen Intern Med. 2007;22(12)1711-1717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hamdy H, Prasad K, Anderson MB, et al. BEME systematic review: predictive values of measurements obtained in medical schools and future performance in medical practice. Med Teach. 2006;28(2)103-116 [DOI] [PubMed] [Google Scholar]
- 20. Bendapudi NM, Berry LL, Frey KA, Parish JT, Rayburn WL. Patients' perspectives on ideal physician behaviors. Mayo Clin Proc. 2006;81(3)338-344 [DOI] [PubMed] [Google Scholar]
- 21. Durning SJ, Cation LJ, Markert RJ, Pangaro LN. Assessing the reliability and validity of the mini-clinical evaluation exercise for internal medicine residency training. Acad Med. 2002;77(9)900-904 [DOI] [PubMed] [Google Scholar]
- 22. Fortune JB. The content and value of letters of recommendation in the resident candidate evaluative process. Curr Surg. 2002;59(1)79-83 [DOI] [PubMed] [Google Scholar]
- 23. O'Halloran CM, Altmaier EM, Smith WL, Edmund A, Franken J. Evaluation of resident applicants by letters of recommendation: a comparison of traditional and behavior-based formats. Invest Radiol. 1993;28(3)274-277 [DOI] [PubMed] [Google Scholar]
- 24. Boyse TD, Patterson SK, Cohan RH, et al. Does medical school performance predict radiology resident performance? Acad Radiol. 2002;9(4)437-445 [DOI] [PubMed] [Google Scholar]
- 25. DeZee KJ, Thomas MR, Mintz M, Durning SJ. Letters of recommendation: rating, writing, and reading by clerkship directors of internal medicine. Teach Learn Med. 2009;21(2)153-158 [DOI] [PubMed] [Google Scholar]
- 26. Greenburg AG, Doyle J, McClure DK. Letters of recommendation for surgical residencies: what they say and what they mean. J Surg Res. 1994;56(2):192-198 [DOI] [PubMed] [Google Scholar]
- 27. Leichner P, Eusebio-Torres E, Harper D. The validity of reference letters in predicting resident performance. J Med Educ. 1981;56(12)1019-1021 [DOI] [PubMed] [Google Scholar]
- 28. Huff KL, Koenig JA, Treptau MM, Sireci SG. Validity of MCAT scores for predicting clerkship performance of medical students grouped by sex and ethnicity. Acad Med. 1999;74(10):S41-S44 [DOI] [PubMed] [Google Scholar]
- 29. Julian ERP. Validity of the medical college admission test for predicting medical school performance. Acad Med. 2005;80(10)910-917 [DOI] [PubMed] [Google Scholar]
- 30. Silver B, Hodgson CS. Evaluating GPAs and MCAT scores as predictors of NBME I and clerkship performances based on students' data from one undergraduate institution. Acad Med. 1997;72(5)394-396 [DOI] [PubMed] [Google Scholar]
- 31. Markert RJ. The relationship of academic measures in medical school to performance after graduation. Acad Med. 1993;68(2):S31-S34 [DOI] [PubMed] [Google Scholar]
- 32. Brenner AM, Mathai S, Jain S, Mohl PC. Can we predict “problem residents”? Acad Med. 2010;85(7)1147-1151 [DOI] [PubMed] [Google Scholar]
- 33. Sehgal AR. The role of reputation in U.S. News & World Report's rankings of the top 50 American hospitals. Ann Intern Med. 2010;152(8)521-525 [DOI] [PubMed] [Google Scholar]