Abstract
Bleeding with severe aortic stenosis is linked to acquired von Willebrand syndrome and loss of high-molecular-weight multimers of von Willebrand factor. Valve replacement resolves bleeding tendency and loss of high-molecular-weight multimers. We report outcomes in 5 patients with symptomatic obstructive hypertrophic cardiomyopathy and spontaneous gastrointestinal, mucosal, or excessive postsurgical bleeding in whom acquired von Willebrand syndrome was documented. All 5 patients underwent surgical septal myectomy with resolution of acquired von Willebrand syndrome.
HMWM = high-molecular-weight multimer; HOCM = hypertrophic obstructive cardiomyopathy; vWF = von Willebrand factor; vWF:Ag = vWF antigen; vWF:RCo = vWF ristocetin cofactor activity
Severe aortic stenosis and, more recently, hypertrophic obstructive cardiomyopathy (HOCM) have been associated with clinically important bleeding.1-6 The bleeding diathesis appears to be mechanistically linked to intravascular shear-induced proteolysis of high-molecular-weight multimers (HMWMs) of von Willebrand factor (vWF).5 The strongest evidence in favor of this mechanism is the resolution of loss of HMWMs within hours of aortic valve replacement and reduced clinical bleeding postoperatively.3 The effects of surgical septal myectomy on vWF composition have not yet been described. Here, we describe 5 patients with HOCM who had histories of abnormal bleeding and demonstrable loss of HMWMs. After surgical reduction of the outflow gradient, vWF normalized in all 5 patients, and none have had recurrent hemorrhage.
PATIENTS AND METHODS
Plasma vWF antigen (vWF:Ag) and ristocetin cofactor activity (vWF:RCo) were measured in 5 patients by automated latex immunoassay and by ristocetin-dependent aggregometry of washed platelets, respectively, as described previously.7 Plasma vWF multimers were analyzed by agarose gel electrophoresis using in-gel immunostaining and infrared imaging.8
RESULTS
Case 1
A 64-year-old man with a history of hypertension and smoking presented for evaluation of recurrent overt gastrointestinal hemorrhage. He described a 7-year history of episodic melena with occasional bright red blood per the rectum but no hematemesis. He had undergone 14 upper and 8 lower gastrointestinal endoscopies and 1 capsule endoscopy with no bleeding source identified, and he received in excess of 50 units of packed red blood cells. He had experienced one episode each of effort syncope and orthostatic syncope. Effort dizziness and dyspnea 5 years previously had led to a diagnosis of HOCM, and metoprolol was prescribed.
For editorial comment, see page 181
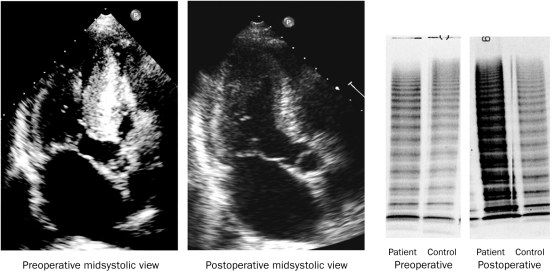
Echocardiography reconfirmed the diagnosis of HOCM (Figure 1; Table). Extended upper gastrointestinal endoscopy demonstrated fernlike vascular malformations in the proximal small bowel, which were treated with argon plasma coagulation. Both vWF:Ag and vWF:RCo were within normal limits (Table). However, analysis of vWF multimers revealed loss of HMWMs and a slight excess of low-molecular-weight multimers, consistent with an acquired abnormality of vWF or an acquired von Willebrand syndrome (Figure 2). He was offered cardiac surgery but opted for medical treatment. During the next 12 months, he had 4 additional overt hemorrhages, 1 after nephrolithotomy for symptomatic renal colic and 3 spontaneous gastrointestinal hemorrhages. After an increase in his metoprolol dosage, he underwent extended septal myectomy (Figure 1).9 Intraoperative hemodynamics detected typical gradient findings that were absent after septal myectomy (Figure 1). The reduction in vWF HMWMs was confirmed before surgery and, while he was taking the higher dose of metoprolol, appeared slightly less severe; reassessment of HMWMs postoperatively revealed a normal pattern (Figure 2).
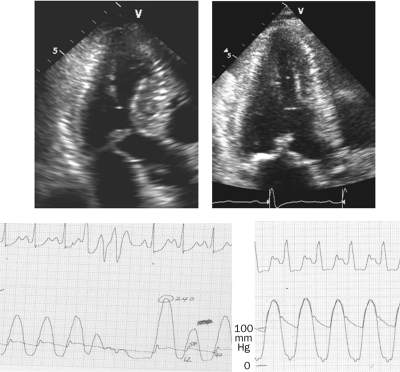
FIGURE 1.
Apical 5-chamber 2-dimensional echocardiographic view for case 1 before (upper left) and after (upper right) septal myectomy eliminating systolic anterior motion. Intraoperative arterial pressure tracings demonstrate a high left ventricular to aortic gradient and a positive Brockenbrough-Braunwald-Morrow sign before surgery (lower left) and the absence of a gradient after surgery (lower right).
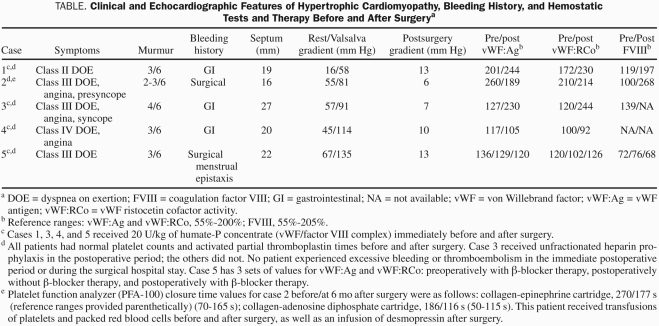
TABLE.
Clinical and Echocardiographic Features of Hypertrophic Cardiomyopathy, Bleeding History, and Hemostatic Tests and Therapy Before and After Surgerya
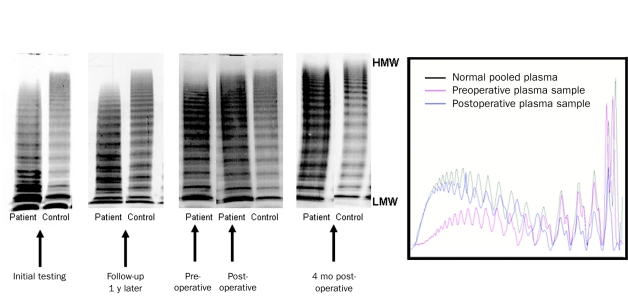
FIGURE 2.
Left, von Willebrand factor multimers and control plasma multimers for case 1 for each determination. The immediate preoperative sample was taken when the patient was taking a higher dose of β-blockers than on the previous 2 occasions. Loss of high-molecular-weight (HMW) multimers was reversed after surgery. Right, Densitometric scan of HMW multimer gels. LMW = low-molecular-weight.
The patient resumed smoking after surgery. He had an ischemic stroke 15 months after his septal myectomy but recovered neurologically. Although he began an aspirin regimen, he has not had spontaneous bleeding during the subsequent 20 months. He has undergone thyroid needle biopsy without excessive bleeding or hematoma.
Case 2
A 60-year-old woman was diagnosed as having HOCM 3 years previously. Symptoms included dyspnea when walking 50 feet, climbing stairs, or having a normal conversation, as well as postural presyncope despite medical treatment. She gave a history of postprocedural bleeding after multiple surgeries, dental extractions, and cardiac catheterization, and a platelet hypofunctional disorder was suspected. Findings on platelet aggregation studies were normal, but closure times were prolonged with the whole blood platelet function analyzer (PFA-100, Siemens USA, Deerfield, IL), both with epinephrine-collagen and adenosine diphosphate–collagen cartridges (Table). Platelet electron microscopy excluded dense granule storage pool deficiency. Although plasma vWF values were normal (Table), evaluation of vWF multimers revealed absence of HMWMs (Figure 3). However, this result was not available until a few days after surgery. After septal myectomy, HMWMs normalized, and the patient has remained free of abnormal bleeding during a 2-year follow-up.
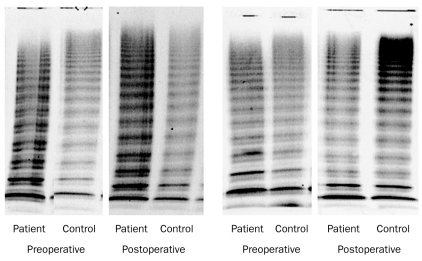
FIGURE 3.
von Willebrand factor multimers and simultaneous control plasma multimers before and after surgery in cases 2 (left) and 4 (right).
Case 3
A 66-year-old woman was referred to our institution with a 2-year history of dyspnea, chest tightness, and frequent episodes of syncope with ordinary activity. Two episodes of melena had also occurred and had been treated with colonoscopic photocoagulation of cecal vascular malformations. Echocardiography revealed typical HOCM (Figure 4). Von Willebrand factor studies, done in duplicate before surgery, revealed loss of HMWMs (Figure 4); the HMWMs were restored to normal levels when reevaluated on the sixth postoperative day. The patient has not had spontaneous hemorrhage and has had no surgical procedures during the subsequent 2.5 years.
FIGURE 4.
Echocardiographic images for case 3 before and after surgery and corresponding von Willebrand factor and control plasma multimers. Preoperative and postoperative echocardiographic results for this case are available at www.mayoclinicproceedings.com/content/86/3/219/suppl/DC1.
Case 4
A 62-year-old woman with diagnosed HOCM had a 5-year history of progressive dyspnea with ordinary activity and while at rest despite medical therapy. She described 2 episodes of frank hematochezia within the previous year. Findings on colonoscopy were unremarkable. Loss of vWF HMWMs was documented before surgery, and HMWM levels normalized after septal myectomy (Figure 3), which drastically reduced the Doppler gradient in the left ventricular outflow tract (Table). During 2 years of follow-up, she has not had abnormal bleeding, including during an emergency surgery for an incarcerated hernia.
Case 5
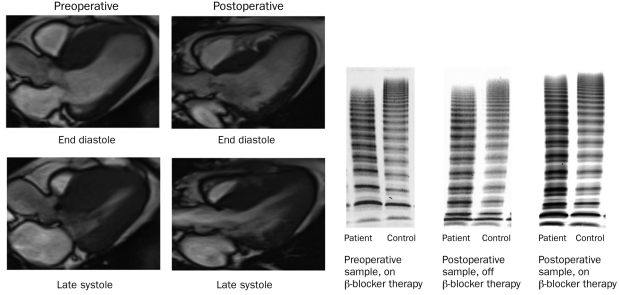
A 38-year-old woman was diagnosed as having HOCM 2 years previously. Her main symptom was dyspnea on exertion, and it eventually progressed to limit ordinary activity. She had a long history of heavy menstrual periods and recurrent epistaxis and required frequent prescriptions for iron deficiency. She eventually had a hysterectomy, after which she had excessive bleeding and required transfusion. Loss of vWF HMWMs was demonstrated while she was receiving β-blocker and verapamil therapy preoperatively. Preoperative cardiac magnetic resonance imaging demonstrated extensive systolic obstruction at the level of the basal and mid septum (Figure 5). Septal myectomy was performed. In the early postoperative period, the patient did not resume taking β-blockers, and findings on vWF multimer analysis remained abnormal. Therapy was reinitiated with 200 mg/d of long-acting metoprolol. Cardiac magnetic resonance imaging and vWF multimers were also reassessed (Figure 5), and her pattern of HMWMs normalized.
FIGURE 5.
Magnetic resonance imaging studies before and after septal myectomy in case 5. von Willebrand factor and simultaneous control plasma multimers before surgery on β-blocker therapy, after surgery off β-blocker therapy, and after surgery on β-blocker therapy. Preoperative and postoperative magnetic resonance imaging results for this case are available at www.mayoclinicproceedings.com/content/86/3/219/suppl/DC1.
DISCUSSION
An association between HOCM and gastrointestinal hemorrhage and angiodysplasia has been reported several times,10-16 and resolution of the bleeding disorder has also been reported with definitive therapies to reduce the outflow gradient, including β-blockade, alcohol septal ablation, and septal myectomy.10,15-17 Aside from one previous case report of a patient with HOCM and a history of bleeding who had confirmation of loss of HMWMs and some qualitative improvement after intensification of medical therapy,10 no reports have been published regarding the response of HMWMs to pharmacolgocial therapy, surgery, or alcohol septal ablation. Our first and fifth cases appeared to have qualitatively less severe loss of HMWMs with increased β-blocker therapy, one preoperatively and the other postoperatively (Figures 2 and 5), suggesting dynamism in HMWMs paralleling changes in gradient. Our 5 cases suggest that myectomy eliminated the loss of HMWMs in a manner similar to aortic valve replacement in aortic stenosis. These observations on the restoration of HMWMs after septal myectomy suggest that this was the likely mechanism for reduction in clinical bleeding seen after treatment in previously reported cases in which vWF studies were not performed.18,19
Le Tourneau et al6 noted a correlation between abnormalities of vWF function and severity of left ventricular outflow tract obstruction in HOCM, and other investigators have noted a similar correlation between such abnormalities and the transvalvular gradient in aortic stenosis.2-5 Sensitive indicators of impaired vWF function in aortic stenosis and HOCM were findings obtained using the whole blood platelet function analyzer (PFA-100), the ratio of vWF collagen-binding activity to vWF:Ag, and vWF multimer analysis.3,6 The usual screening tests for von Willebrand disease, ie, plasma levels of vWF:Ag and vWF:RCo and/or a ratio of vWF:RCO to vWF:Ag of less than 0.7, appear insensitive for the detection of this abnormality as exemplified by our cases (Table).
Physiologically, high intravascular shear force, such as that occurring in the microvasculature, creates a conformational change in plasma vWF multimers, enhancing surface-bound vWF hemostatic interaction with platelets while simultaneously exposing a vWF cleavage site to proteolysis by circulating ADAMTS13 (a disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13), ultimately decreasing the size of vWF multimers and down-regulating vWF hemostatic function.5,18 Pathophysiologically, vascular lesions, such as those associated with ventricular septal defects, patent ductus arteriosus,19,20 and, more recently, nonpulsatile ventricular assist devices,21,22,23 cause increased intravascular shear, enhance vWF proteolysis, decrease vWF hemostatic function, and often result in bleeding symptoms.3,19,20 Other conditions pathogenetically associated with an acquired von Willebrand syndrome often show a pattern on multimer analysis that is distinct from intravascular shear–related loss of HMWMs. These entities include plasma cell proliferative disorders, such as monoclonal gammopathy of undetermined significance, lymphoproliferative or myeloproliferative disorders, and certain other neoplastic states, autoimmune disorders, and hypothyroidism.21-26
This report has 3 potential clinical implications. First, patients with acquired mucosal bleeding tendencies and HOCM should be investigated for acquired von Willebrand syndrome with testing beyond vWF:Ag and vWF:RCo, including vWF multimers. Second, if loss of HMWMs is confirmed, use of prophylactic vWF-factor VIII concentrate should be considered for invasive procedures, including at least perioperatively for surgical septal myectomy. Finally, if bleeding is recurrent and potentially life-threatening, one might consider definitive structural therapy to eliminate the gradient for reasons other than medically refractory cardiac symptoms, as was the situation in our case 1.
CONCLUSION
Septal myectomy in severe, symptomatic HOCM appears to resolve acquired von Willebrand syndrome and abnormal bleeding in a manner analogous to aortic valve replacement for severe aortic stenosis.
Supplementary Material
REFERENCES
- 1. Pareti FI, Lattuada A, Bressi C, et al. Proteolysis of von Willebrand factor and shear stress-induced platelet aggregation in patients with aortic valve stenosis. Circulation. 2000;102(11)1290-1295 [DOI] [PubMed] [Google Scholar]
- 2. Warkentin TE, Moore JC, Anand SS, Lonn EM, Morgan DG. Gastrointestinal bleeding, angiodysplasia, cardiovascular disease, and acquired von Willebrand syndrome. Transfus Med Rev. 2003;17(4)272-286 [DOI] [PubMed] [Google Scholar]
- 3. Vincentelli A, Susen S, Le Tourneau T, et al. Acquired von Willebrand syndrome in aortic stenosis. N Engl J Med. 2003;349(4)343-349 [DOI] [PubMed] [Google Scholar]
- 4. Yoshida K, Tobe S, Kawata M, Yamaguchi M. Acquired and reversible von Willebrand disease with high shear stress aortic valve stenosis. Ann Thorac Surg. 2006;81(2)490-494 [DOI] [PubMed] [Google Scholar]
- 5. Sadler JE. New concepts in von Willebrand disease. Annu Rev Med. 2005;56:173-191 [DOI] [PubMed] [Google Scholar]
- 6. Le Tourneau T, Susen S, Caron C, et al. Functional impairment of von Willebrand factor in hypertrophic cardiomyopathy: relation to rest and exercise obstruction. Circulation. 2008;118:1550-1557 [DOI] [PubMed] [Google Scholar]
- 7. Chen D, Daigh CA, Hendricksen JI, et al. A highly-sensitive plasma von Willebrand factor ristocetin cofactor (VWF:RCo) activity assay by flow cytometry. J Thromb Haemost. 2008;6:323-330 [DOI] [PubMed] [Google Scholar]
- 8. Pruthi RK, Daniels TM, Heit JA, Chen D, Owen WG, Nichols WL. Von Willebrand factor multimer quantitative analysis by in-gel immunostaining and infrared fluorescent imaging. Thromb Res. 2010;126(6)543-549 [DOI] [PubMed] [Google Scholar]
- 9. Dearani JA, Danielson GK. Septal myectomy for obstructive hypertrophic cardiomyopathy. Oper Tech Thorac Cardiovasc Surg. 2004;9(4)278-292 [DOI] [PubMed] [Google Scholar]
- 10. Shimizu M, Masai H, Miwa Y. Occult gastrointestinal bleeding due to acquired von Willebrand syndrome in a patient with hypertrophic obstructive cardiomyopathy. Intern Med. 2007;46(8)481-485 [DOI] [PubMed] [Google Scholar]
- 11. Kimmel DJ, Paster SB, Burstein J, Stovring J, Cochran PT. Cardiac disease and recurrent gastrointestinal bleeding: angiodysplasia with accompanying hypertrophic subaortic stenosis. Rocky Mt Med J. 1977;74(6)316-319 [PubMed] [Google Scholar]
- 12. Fujita H, Tomiyama J, Chuganji Y, Momoi M, Tanaka T. Diffuse angiodysplasia of the upper gastrointestinal tract in a patient with hypertrophic obstructive cardiomyopathy. Intern Med. 2000;39(5)385-388 [DOI] [PubMed] [Google Scholar]
- 13. Marti L, Anton R, Almela P, Benages A. Intestinal angiodysplasia associated with hypertrophic subaortic stenosis: a variant of Heyde syndrome [in Spanish]? Med Clin (Barc); 2005;125(16)635-636 [DOI] [PubMed] [Google Scholar]
- 14. Bonneau A, Firouz-Abadi M, Cognault JP, Couradeau B, Dumas M. Angiodysplasia of the ileum and cardiomyopathy [in French]. Ann Cardiol Angeiol (Paris). 1984;33(6)389-394 [PubMed] [Google Scholar]
- 15. Schwartz J, Rozenfeld V, Habot B. Cessation of recurrent bleeding from gastrointestinal angiodysplasia, after beta blocker treatment in a patient with hypertrophic subaortic stenosis—a case history. Angiology. 1992;43(3, pt 1):244-248 [DOI] [PubMed] [Google Scholar]
- 16. Riis Hansen P, Hassager C. Septal alcohol ablation and Heyde's syndrome revisited. J Intern Med. 2003;253(4)490-491 [DOI] [PubMed] [Google Scholar]
- 17. Alam M, Lewis JW., Jr Cessation of gastrointestinal bleeding from angiodysplasia after surgery for idiopathic hypertrophic subaortic stenosis. Am Heart J. 1991;121(2, pt 1):608-610 [DOI] [PubMed] [Google Scholar]
- 18. Sadler JE, Budde U, Eikenboom JC, et al. Update on the pathophysiology and classification of von Willebrand disease: a report of the Subcommittee on von Willebrand Factor. J Thromb Haemost. 2006;4(10)2103-2114 [DOI] [PubMed] [Google Scholar]
- 19. Gill JC, Wilson AD, Endres-Brooks J, Montgomery RR. Loss of the largest von Willebrand factor multimers from the plasma of patients with congenital cardiac defects. Blood. 1986;67(3)758-761 [PubMed] [Google Scholar]
- 20. Rauch R, Budde U, Koch A, Girisch M, Hofbeck M. Acquired von Willebrand syndrome in children with patent ductus arteriosus. Heart. 2002;88(1)87-88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nichols WL, Hultin MB, James AH, et al. Von Willebrand disease (VWD): evidence-based diagnosis and management guidelines, the National Heart, Lung, and Blood Institute (NHLBI) Expert Panel report (USA). Haemophilia. 2008;14(2)171-232 [DOI] [PubMed] [Google Scholar]
- 22. Nichols WL, Rick ME, Ortel TL, et al. Clinical and laboratory diagnosis of von Willebrand disease: a synopsis of the 2008 NHLBI/NIH guidelines. Am J Hematol. 2009;84:366-370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tatooles AJ, Gallagher C, Stahl E, Pappas PS. Frequency and management of GI bleeding in patients with continuous flow left ventricular assist devices. Presented at: The Society of Thoracic Surgeons 47th Annual Meeting and Exhibition; January 30-February 2, 2011; San Diego, CA [Google Scholar]
- 24. Tiede A, Priesack J, Werwitzke S, et al. Diagnostic workup of patients with acquired von Willebrand syndrome: a retrospective single-centre cohort study. J Thromb Haemost. 2008;6:569-576 [DOI] [PubMed] [Google Scholar]
- 25. Veyradier A, Jenkins CS, Fressinaud E, Meyer D. Acquired von Willebrand syndrome: from pathophysiology to management. Thromb Haemost. 2000;84(2)175-182 [PubMed] [Google Scholar]
- 26. Kumar S, Pruthi RK, Nichols WL. Acquired von Willebrand disease. Mayo Clin Proc. 2002;77(2)181-187 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.