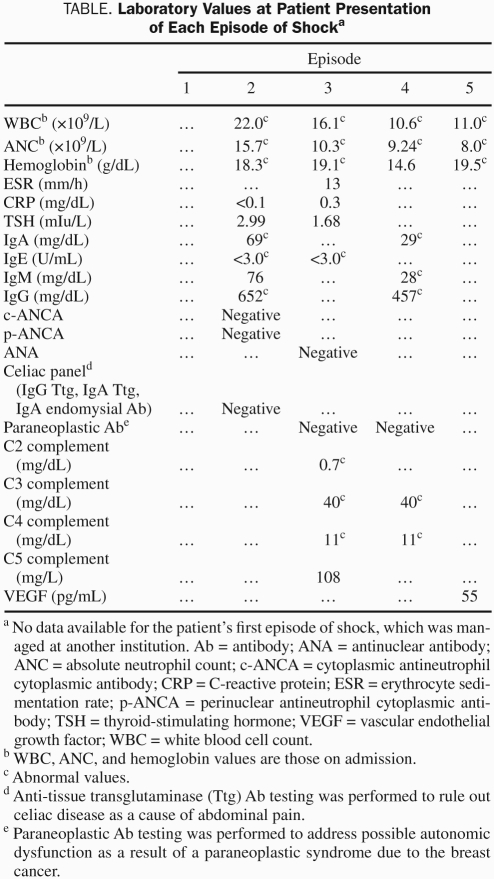
To the Editor: A 43-year-old woman presented with 3 episodes of shock within a 6-month period (Table); all episodes occurred after symptoms of nonspecific abdominal pain. During the second episode of shock, an infiltrating lobular carcinoma of the breast (estrogen receptive–positive, progesterone receptor–negative, human epidermal growth factor 2–positive [T3,N1,M0]) was diagnosed. After resolution of the third episode of shock, a standard regimen consisting of paclitaxel, carboplatin, and trastuzumab was instituted; the patient had no further episodes of shock for the next 9 months.
TABLE.
Laboratory Values at Patient Presentation of Each Episode of Shocka
Three months after the patient underwent a modified radical mastectomy and completed chemotherapy, she experienced 4 episodes of hypotension within a 3-week period, the last of which resulted in refractory shock. On the basis of her history of unexplained shock with prodromal symptoms and an IgG κ monoclonal gammopathy, idiopathic systemic capillary leak syndrome (SCLS) was diagnosed. Prophylactic therapy with terbutaline and theophylline was initiated. Eighteen months later, the patient experienced 1 episode of shock, with a concurrently low level of serum theophylline (7.7 μg/mL). In addition to resuscitation with 10 L of normal saline in the first 24 hours, she was given increasing doses of theophylline and treated with albumin infusion and montelukast; symptoms resolved after 1 day of this therapeutic regimen.
Idiopathic SCLS is a rare and life-threatening disorder, with only 100 to 125 cases published worldwide since the first report in 1960.1-6 The shock that patients with SCLS experience, with associated hemoconcentration and hypoalbuminemia, is caused by sudden, massive leakage of proteins and serum into the extravascular space.1,7 Plasma proteins up to 200 kDa or, in some cases, 900 kDa escape the capillary bed, resulting in an intravascular loss of up to 70% of plasma volume.2,8,9 Most patients have an associated IgG κ or λ monoclonal gammopathy,1,10 although its importance remains unknown.
Idiopathic SCLS has been reported preceding hematologic malignancy11 but not in association with a solid tumor; it should be distinguished from drug-induced SCLS that may occur after treatment of other malignancies. In addition to the classic findings, our patient had neutrophilia at the outset of each attack, which lasted 24 to 48 hours and was as high as 40 × 109/L during one episode. Given that neutrophilia has been observed in patients with SCLS, it is notable that no episodes of SCLS occurred in our patient while receiving chemotherapy, and routine laboratory testing during that time revealed low or normal white blood cell counts. Demargination due to endothelial damage could be responsible for the neutrophilia, but a pathologic role of the neutrophils is also a possibility.
Although the mechanism behind capillary leak in idiopathic SCLS is unknown, evidence supports endothelial apoptosis, rather than endothelial contraction or widened cell-cell junctions, as the cause.1,13,14 Use of numerous investigational drugs has been reported with variable outcomes.6,15-20 Traditional prophylactic therapies, theophylline/aminophylline and terbutaline, have been reported to achieve durable success,3,6,9,21 despite a lack of understanding of their mode of action. Spironolactone, hydrocortisone, progesterone, and dexamethasone all appear to protect against endothelial cell apoptosis in response to serum deprivation,22 whereas albumin inhibits endothelial cell apoptosis when there is intact endothelial cell adhesion,23 suggesting that these therapies have potential benefit.
Neutrophil-mediated endothelial apoptosis has been described in patients with other inflammatory disorders.24,25 Given the neutrophilia seen in SCLS and the quiescence of SCLS in our patient while receiving neoadjuvant chemotherapy, one area of interest may involve neutrophil regulation. Although the chemotherapeutic benefit may have been due to general immunosuppression, there may be mechanism-specific similarities between theophylline, paclitaxel, and carboplatin. In addition to decreasing endothelial permeability through elevation of intracellular cyclic adenosine monophosphate5,26 and offering immune-modulatory effects,26 theophylline may affect neutrophil life span. Theophylline causes granulocyte apoptosis in vitro, even in the presence of granulocyte-macrophage colony-stimulating factor,27 with B-cell lymphoma 2 (bcl-2) down-regulation involved in theophylline-induced apoptosis of eosinophilic granulocytes.28 Granulocyte life span is determined by a balance of proapoptotic and antiapoptotic gene expression, with down-regulation of the inducible and short-lived anti-apoptotic bcl-2 family member expression sufficient for neutrophil apoptosis.29,30 Both paclitaxel and carboplatin also affect bcl-2 down-regulation in other settings.31,32 Given these observations, future studies should investigate whether neutrophils obtained during acute attacks are sufficient to cause endothelial apoptosis, whether bcl-2 or its family members are aberrantly expressed, and whether the aforementioned drugs alter bcl-2 family member expression.
We offer special thanks to all the physicians and nurses involved in the diagnosis and treatment of the patient.
References
- 1. Assaly R, Olson D, Hammersley J, et al. Initial evidence of endothelial cell apoptosis as a mechanism of systemic capillary leak syndrome. Chest. 2001;120(4):1301-1308 [DOI] [PubMed] [Google Scholar]
- 2. Clarkson B, Thompson D, Horwith M, Luckey EH. Cyclical edema and shock due to increased capillary permeability. Am J Med. 1960;29(2):193-216 [DOI] [PubMed] [Google Scholar]
- 3. Dhir V, Arya V, Malav ICC, et al. Idiopathic systemic capillary leak syndrome (SCLS): case report and systematic review of cases reported in the last 16 years. Intern Med. 2007;46(12)899-904 [DOI] [PubMed] [Google Scholar]
- 4. Hollenberg J, Frykman J, Lundberg LG, Forsberg S. A case report of systemic capillary leak syndrome (Clarkson's disease). Acta Anaesthesiol Scand. 2010;54(5)649-652 [DOI] [PubMed] [Google Scholar]
- 5. Bonadies N, Baud P, Peter HJ, et al. A case report of Clarkson's disease: if you don't know it, you'll miss it. Eur J Intern Med. 2006;17(5)363-365 [DOI] [PubMed] [Google Scholar]
- 6. Druey KM, Greipp PR. Narrative review: the systemic capillary leak syndrome. Ann Intern Med. 2010;153(2)90-98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. De Martino M, Sasso L, Pirozzi F, Bonaduce D. Systemic capillary leak syndrome or Clarkson's disease: a case report. Intern Emerg Med. 2009;4(4):357-358 [DOI] [PubMed] [Google Scholar]
- 8. Atkinson JP, Waldman TA, Stein SF, et al. Systemic capillary leak syndrome and monoclonal IgG gammopathy: studies in a sixth patient and a review of the literature. Medicine. 1977;56(3)225-239 [DOI] [PubMed] [Google Scholar]
- 9. Tahirkheli NK, Greipp PR. Treatment of the systemic capillary leak syndrome with terbutaline and theophylline: a case series. Ann Intern Med. 1999;130(11):905-909 [DOI] [PubMed] [Google Scholar]
- 10. Chihara R, Nakamoto H, Arima H, et al. Systemic capillary leak syndrome. Intern Med. 2002;41(11)953-956 [DOI] [PubMed] [Google Scholar]
- 11. Ghosh K, Madkaikar M, Iyer Y, et al. Systemic capillary leak syndrome preceding plasma cell leukaemia. Acta Haematol. 2001;106(3)118-121 [DOI] [PubMed] [Google Scholar]
- 12. Zhang W, Ewan PW, Lachmann PJ. The paraproteins in systemic capillary leak syndrome. Clin Exp Immunol. 1993;93(3)424-429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cicardi M, Berti E, Caputo V, et al. Idiopathic capillary leak syndrome: evidence of CD8-positive lymphocytes surrounding damaged endothelial cells. J Allergy Clin Immunol. 1997;99(3)417-419 [DOI] [PubMed] [Google Scholar]
- 14. Johansson BR, Lofdahl CG. Ultrastructure of the microvessels in skeletal muscle in a case of systemic capillary leak syndrome. Acta Med Scand. 1979;206(5)413-416 [DOI] [PubMed] [Google Scholar]
- 15. Teelucksingh S, Padfield PL, Edwards CRW. Systemic capillary leak syndrome. Q J Med. 1990;75(277)515-524 [PubMed] [Google Scholar]
- 16. Lassoued K, Clauvel JP, Similowski T, et al. Pulmonary infections associated with systemic capillary leak syndrome attacks in a patient with hypogammaglobulinemia. Intensive Care Med. 1998;24(9)981-983 [DOI] [PubMed] [Google Scholar]
- 17. Dowden AM, Rullo OJ, Aziz N, Fasano MB, Chatila T, Ballas ZK. Idiopathic systemic capillary leak syndrome: novel therapy for acute attacks [letter]. J Allergy Clin Immunol. 2009;124(5)111-113 [DOI] [PubMed] [Google Scholar]
- 18. Lilly CM, Silverman ES, Sheffer AL. Systemic capillary leak syndrome, leukotrienes, and anaphylaxis. J Intensive Care Med. 2002;17(4)189-194 [Google Scholar]
- 19. Shin JI, Lee JS. Beneficial effect of intravenous immunoglobulins on systemic capillary leak syndrome in patients with monoclonal gammopathy [letter]. Crit Care Med. 2009;37(2):795 [DOI] [PubMed] [Google Scholar]
- 20. Lesterhuis WJ, Rennings AJ, Leenders WP, et al. Vascular endothelial growth factor in capillary leak syndrome. Am J Med. 2009;122(6):e5-e7 [DOI] [PubMed] [Google Scholar]
- 21. Kapoor P, Greipp PT, Schaefer EW, et al. Idiopathic systemic capillary leak syndrome (Clarkson's disease): the Mayo Clinic experience. Mayo Clin Proc. 2010;85(10)905-912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Williams TA, Verhovez A, Milan A, et al. Protective effect of spironolactone on endothelial cells. Endocrinology. 2006;147(5)2496-2505 [DOI] [PubMed] [Google Scholar]
- 23. Zoellner H, Hofler M, Beckmann R, et al. Serum albumin is a specific inhibitor of apoptosis in human endothelial cells. J Cell Sci. 1996;109(10):2571-2580 [DOI] [PubMed] [Google Scholar]
- 24. Bratt J, Palmblad J. Cytokine-induced neutrophil-mediated injury of human endothelial cells. J Immunol. 1997;159(2)912-918 [PubMed] [Google Scholar]
- 25. Joussen AM, Murata T, Tsujikawa A, et al. Leukocyte-mediated endothelial cell injury and death in the diabetic retina. Am J Pathol. 2001;158(1)147-152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vassallo R, Lipsky JL. Theophylline: Recent advances in the understanding of its mode of action and uses in clinical practice. Mayo Clin Proc. 1998;73(4)346-354 [DOI] [PubMed] [Google Scholar]
- 27. Yasui K, Hu B, Nakazawa T, et al. Theophylline accelerates human granulocyte apoptosis not via phosphodiesterase inhibition. J Clin Invest. 1997;100(7):1677-1684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chung IY, Nam-Kung EK, Lee NM, et al. The downregulation of Bcl-2 expression is necessary for theophylline-induced apoptosis of eosinophil. Cell Immunol. 2000;203(2)95-102 [DOI] [PubMed] [Google Scholar]
- 29. Simon HU. Regulation of eosinophil and neutrophil apoptosis: similarities and differences. Immunol Rev. 2001;179(1)156-162 [DOI] [PubMed] [Google Scholar]
- 30. Moulding DA, Akgul C, Derouet M, White MR, Edwards SW. Bcl-2 Family Expression in human neutrophils during delayed and accelerated apoptosis. J Leukoc Biol. 2001;70(5)783-792 [PubMed] [Google Scholar]
- 31. Singh S, Bhat MK. Carboplatin induces apoptotic cell death through downregulation of constitutively active nuclear factor-κB in human HPV-18 E6-positive HEp-2 cells. Biochem Biophys Res Commun. 2004;318(2)346-353 [DOI] [PubMed] [Google Scholar]
- 32. Cao W, Shiverick KT, Namiki K, et al. Docetaxel and bortezomib down-regulate Bcl-2 and sensitize PC-3-Bcl-2 expressing prostate cancer cells to irradiation. World J Urol. 2008;26(5)509-516 [DOI] [PubMed] [Google Scholar]