Abstract
We report a case of a 51-year-old man with a first panic attack associated with high serum lactate due to hyperventilation induced alkalosis. Hyperlactataemia may trigger somatically oriented tests and divert attention from diagnosing panic disorder (PD). Factors associated with underdiagnosis of PD as well as pathophysiology of hyperlactataemia will be discussed.
Background
Knowledge of the physiologic rise in lactate concentrations during hyperventilation is very educating, because with raised lactate most doctors suspect tissue hypoxia (as a ‘conditioned reflex’); we hope that this case report can help to keep an open mind for ‘other’ diagnoses such as panic disorder (PD), even when presenting with high lactate concentrations.
PD must be recognised early as it influences cardiac morbidity and mortality.
Case presentation
A 51-year old man without any past medical history or medication presented early one morning in August to the first heart aid with acute onset shortness of breath. The complaints had started approximately 1 h before presentation, when the patient got out of bed in the morning and he experienced dizzy spells and nausea. This led to anxiety, because a friend of his had recently died suddenly following a cardiac event.
The patient was brought to the first heart aid by ambulance and was moderately ill, but haemodynamically stable with a blood pressure of 130/80 mm Hg (left and right) and a pulse rate of 75 beats/min There was a slightly raised respiratory frequency of 25/min and profuse perspiration without complaints of pain.
On physical examination there were no further abnormalities, especially no signs of bronchial spasm. The electrocardiogram (ECG) showed sinus rhythm of 72 beats/min an intermediate electrical axis without any abnormalities.
Arterial blood gas analysis showed a respiratory alkalosis (pH 7.51, Paco2 3.4 kPa, Pao2 13.2 kPa, bicarbonate 19.7 mmol/l, base excess 23 mmol/l, HbO2 98%) and a raised lactate concentration of 7.5 mmol/l (reference value 0.6–2.4 mmol/l). Kidney function and liver enzymes were normal.
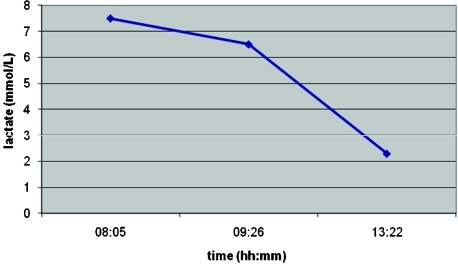
Considering the initial presentation with shortness of breath and hyperventilation, an acute pulmonary embolus was excluded using chest computed tomography (CT) angiography. Supportive treatment for hyperventilation was started with rest and rebreathing in a semi-sealed paper bag. This manoeuvre was also attempted by the patient at home shortly after the onset of complaints without success. After 4 h in the emergency department a second blood gas analysis was obtained in which the lactate concentration had decreased to 2.3 mmol/l with normal blood gas values (fig 1). He had no further complaints and was discharged.
Figure 1.
Lactate clearance during >5 h of observation
After several weeks, the patient was seen at the outpatient clinic of the cardiopsychiatry department. This is a tertiary cardiological unit specialised in the relationship between cardiology and psychiatry/psychology. He stated that he had not experienced any complaints since. On further questioning it appeared that the patient experienced a lot of stress in the period before presenting to the first heart aid, mainly triggered by work stress and the recent cardiac death of a close friend. At that moment the Hospital Anxiety and Depression Scale (HADS) was obtained and the score on the anxiety subscale was 3 and the depression subscale was 0 (normal <8).
The patient was reassured and discharged with the diagnosis of a single panic attack.
Differential diagnosis
Heat stress may cause hyperventilation that may cause respiratory alkalosis, positive Chvostek or Trousseau sign, laryngospasm, or spontaneous carpopedal spasm (heat tetany).
Also a variety of acid–base disturbances can occur with salicylate intoxication. Salicylates stimulate the respiratory centre directly, resulting in an early fall in the Paco2 and respiratory alkalosis. An anion gap metabolic acidosis then follows, due primarily to the accumulation of organic acids, including lactic acid and ketoacids.1
Biguanide (metformin) treatment for type 2 diabetes can lead to hyperlactataemia or lactic acidosis.
Discussion
Hyperventilation is ventilation that exceeds metabolic demands, which results in a decline of arterial partial pressure of carbon dioxide (Paco2) and a rise in pH of the body fluids (respiratory alkalosis).
If hyperventilation is sustained for some time, secondary physiological changes take place and can lead to symptoms such as dizziness, paresthesias, stiff muscles, cold hands or feet, and trembling.2
The symptoms patients experience during hyperventilation—for example, shortness of breath, chest pain, dizziness, nausea and palpitations—appear to be similar to the symptoms during a panic attack. For that reason there is a theory that hyperventilation plays a pathophysiological role in the onset of panic attacks.3
The prevalence of PD is 1.5–2.3% of the general population and is associated with substantial functional limitations.4 A first (isolated) panic attack can occur in patients up to the age of 50–60 years. During summer months there is a higher incidence of first panic attacks.5
PD is characterised by a short episode of fear in which a number of symptoms (⩾4) occur (table 1).
Table 1.
Symptoms of panic attacks (Diagnostic and statistical manual, 4th revision (DSM-IV) criteria)
| 1. Palpitations, pounding heart, or accelerated heart rate |
| 2. Sweating |
| 3. Trembling or shaking |
| 4. Sensations of shortness of breath or smothering |
| 5. Feeling of choking |
| 6. Chest pain or discomfort |
| 7. Nausea or abdominal distress |
| 8. Feeling dizzy, unsteady, lightheaded, or faint |
| 9. Derealisation (feelings of unreality) or depersonalization (being detached from oneself) |
| 10. Fear of losing control or going crazy |
| 11. Fear of dying |
| 12. Paresthesias |
| 13. Chills or hot flushes |
A previous study showed that anger/hostility was also associated with PD, with a 20% increased risk of both incident coronary heart disease (CHD) in initially healthy individuals and poor prognosis in CHD patients.6
There is a suggestion that moderately elevated anxiety is associated with a modest risk of myocardial infarction (MI), and severe anxiety represents an MI risk that may warrant clinical attention. Anxiety represents an independent, prospective, and unique risk factor for MI.7
To diagnose PD there must have been at least two acute and spontaneous panic attacks that reach their peak within 10 min, and the patient displays characteristic concerns or attributions for at least a month about the implications or consequences of the panic attacks, which can lead to avoidance behaviour.8
PD is only recognised in a limited number of patients in a non-psychiatric environment.9 Recognition, however, is of crucial importance because early diagnosis and treatment can benefit patients and society. Early and adequate recognition prevents unnecessary suffering of patients and their relatives, work absence, consultation and medical investigations. This would lead to referral to the psychiatrist or a specialised facility for adequate therapy.10 PD can be treated well and a multidisciplinary approach can benefit these patients.11
Identification of those patients, who may require more detailed consultations and more intensive intervention to deal with concerns and fears about their condition—for example, in chest pain clinics—has been widely recommended. The benefit is reduction of symptoms and more appropriate use of healthcare resources.12
New onset panic attacks/disorder were associated with an increased hazard of subsequent CHD/MI diagnosis in younger people, with less effect in people over 50. This may be due to initial misdiagnosis of CHD as panic attacks or an underlying increased risk of CHD with panic attacks/disorder in younger people.13
Lactic acid is a normal product of glucose metabolism. Under hypoxic conditions the cell switches to anaerobic metabolism, further increasing lactic acid formation. Lactic acid concentration can reveal a disbalance of oxygen demand and oxygen supply.
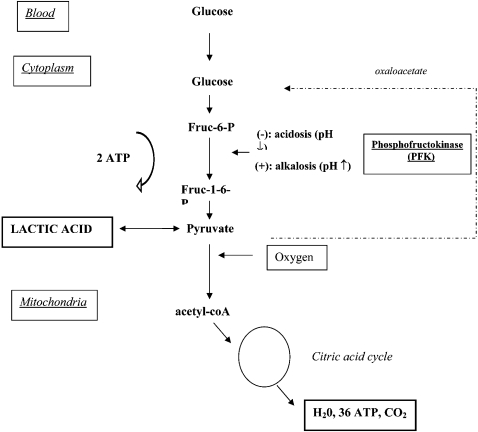
Lactic acid is formed out of pyruvate in the metabolism of glucose (fig 2). All cells can produce lactic acid but tissues with high metabolism (intestines, brain, skin, muscle, and red blood cells) produce the most lactic acid on a daily basis.
Figure 2.
Schematic reproduction of the metabolism of glucose and lactic acid. The glycolytic pathway transforms glucose to pyruvate, and pyruvate is oxygenated through acetyl-coA which is transformed into carbon dioxide and water in the mitochondria. There is in total 38 mol ATP release with the glycolysis of 1 mol glucose. Metabolism of lactic acid back into pyruvate can form glucose, again through oxaloacetate. The rate limiting step in glycolysis is the reaction catalysed by phosphofructokinase (PFK) through conversion of fructose-6-phosphate. Cellular acidosis inhibits, and alkalosis disinhibits, the glycolysis. Intracellular alkalosis disinhibits the glycolysis through PFK with raised concentrations of end product (eg, lactic acid).10
Lactic acid is metabolised mainly in the liver (50%) and the kidneys (25–30%) into glucose. The lactic acid concentration is the net result of production and clearance of the pyruvate metabolism.14
The limiting step in glycolysis is the reaction catalysed by phosphofructokinase (PFK). PFK is the primary site of action of several mechanisms regulating the rate of glycolysis.
The activity of PFK is also regulated by the concentration of H+ ions. Lactic acid production decreases when intracellular pH is low (acidosis), and increases when intracellular pH is high (alkalosis). This effect of pH on lactic acid production provides a homeostatic mechanism for generating H+ ions to rapidly counteract a state of intracellular alkalosis. Because CO2 is a source of acid that rapidly crosses cell membranes the respiratory alkalosis resulting from hyperventilation induced hypocapnia causes an immediate intracellular alkalosis.15
Our patient presented with an acute respiratory alkalosis based on a hyperventilation induced hypocapnia with excessive lactic acid formation.
One hypothesis is that intracellular alkalosis has a disinhibiting action on pyruvate metabolism, which promotes rapid glycolysis by the catalysing PFK. The net result will be lactic acid formation. Another hypothesis is the prolonged hyperventilation with inadequate rebreathing therapy that the patient did at home.
An interesting question is how much lactic acid formation there will be, and if there is a difference between subjects with or without PD. For a long period of time, only hypoxia was thought to raise lactic acid concentrations, but nowadays it is clear that under normal aerobic conditions lactic acid can accumulate in serum, brain and other tissues.16
Maddock et al conducted the first study designed specifically to investigate the effects of respiratory alkalosis on glycolytic metabolism and net lactate production in PD. In this study, PD patients and controls underwent hyperventilation, which resulted in a significantly greater increase in serum lactate concentration in response to hyperventilation among PD patients compared to controls. With short duration of hyperventilation (8 min), the maximum lactate concentration was 2.0 mmol/l.17
Meanwhile, one of the hypotheses is that PD patients have a metabolic disturbance in lactate formation and clearance, causing the raised lactate response.16 Lactate and other substances, like caffeine, isoproterenol, cholecystokinin (CCK) and epinephrine, can provoke a panic attack in susceptible individuals.18
Learning points
The number of patients presenting to the healthcare system with hyperventilation is high; hardly any further investigation is done to reveal an underlying psychiatric diagnosis, such as panic disorder (PD). This leads to delayed recognition of possible PD with all its consequences, mainly prolonged suffering for patients as well as more burden on the health care system.
Knowledge of the physiologic rise in lactate during hyperventilation is very informative, because with raised lactate concentrations most doctors suspect tissue hypoxia (as a ‘conditioned reflex’), while from the literature it is clear that this is certainly not always the case.
Knowing that PD has a negative influence on cardiac prognosis, an early recognition will be beneficial for the patient.
We hope that this case report can encourage readers to keep an open mind for ‘other’ diagnoses such as PD, even when patients present with high lactate concentrations.
Footnotes
Competing interests: None.
Patient consent: Patient/guardian consent was obtained for publication.
REFERENCES
- 1.Traub SJ. Aspirin poisoning in adults. : Basow DS, ed. UpToDate. Waltham, Massachusetts: UpToDate, 2009 [Google Scholar]
- 2.Hornsveld HK, Garssen B, Fiedeldij Dop MJC, et al. Double blind placebo controlled study of the hyperventilation provocation test and the validity of the hyperventilation syndrome. Lancet 1996; 348: 154–8 [DOI] [PubMed] [Google Scholar]
- 3.Beurs de E. The assessment and treatment of panic disorder and agoraphobia. Thesis, University of Amsterdam, 1993 [Google Scholar]
- 4.Weinstein RS. Panic disorder. Am Fam Physician 1995; 52: 2055–63 [PubMed] [Google Scholar]
- 5.Faravelli C, Paionni A. Panic disorder: clinical course, morbidity and comorbidity. : Griez EJL, Faravelli C, Nutt D, Zohar J, eds. Anxiety disorders. Chichester, 2001 [Google Scholar]
- 6.Chida Y, Steptoe A. The association of anger and hostility with future coronary heart disease: a meta-analytic review of prospective evidence. J Am Coll Cardiol 2009; 53: 936–46 [DOI] [PubMed] [Google Scholar]
- 7.Shen BJ, Avivi YE, Todaro JF, et al. Anxiety characteristics independently and prospectively predict myocardial infarction in men the unique contribution of anxiety among psychologic factors. J Am Coll Cardiol 2008; 2: 113–9 [DOI] [PubMed] [Google Scholar]
- 8.American Psychiatry Association Diagnostic and statistical manual of mental disorders DSM-IV-TR. APA, 2000 [Google Scholar]
- 9.Fleet RP, Dupuis G, Marchand A, et al. Panic disorder in emergency department chest pain patients: prevalence, comorbidity, suicidal ideation, and physician recognition. Am J Med 1996; 101: 371–80 [DOI] [PubMed] [Google Scholar]
- 10.Vliet van IM, Balkom van AJLM, Schruers KRJ. ‘Hyperventilation syndrome’: often an easy to treat panic disorder. Ned Tijdschr Geneeskd 2004; 28: 1369–72 [PubMed] [Google Scholar]
- 11.Raedt de C, Kuijpers P, Honig A. Chest pain due to a panic disorder: the significance of a multidisciplinary approach. Ned Tijdschr Geneeskd 2007; 151: 2417–20 [PubMed] [Google Scholar]
- 12.Robertson N, Javed N, Samani NJ, et al. Psychological morbidity and illness appraisals of patients with cardiac and non-cardiac chest pain attending a rapid access chest pain clinic, a longitudinal cohort study. Heart 2008; 94: e12. [DOI] [PubMed] [Google Scholar]
- 13.Walters K, Rait G, Petersen I, et al. Panic disorder and risk of new onset coronary heart disease, acute myocardial infarction, and cardiac mortality: cohort study using the general practice research database. Eur Heart J 2008; 24: 2981–8 [DOI] [PubMed] [Google Scholar]
- 14.Bakker J, Schieveld SJM, Brinkert W. Serum lactate level as a measure of tissue hypoxia in severely ill patients. Ned Tijdschr Geneeskd 2000; 16: 737–41 [PubMed] [Google Scholar]
- 15.Maddock RJ. The lactic acid response to alkalosis in panic disorder: an integrative review. J Neuropsychiatry Clin Neurosci 2001; 13: 22–34 [DOI] [PubMed] [Google Scholar]
- 16.Maddock RJ, Buonocore MH, Copeland LE, et al. Elevated brain lactate responses to neural activation in panic disorder: a dynamic 1H-MRS study. Mol Psychiatry 2008: 1–9 [DOI] [PubMed] [Google Scholar]
- 17.Maddock RJ, Matteo-Bermundez J. Elevated serum lactate following hyperventilation during glucose infusion in panic disorder. Biol Psychiatry 1990; 27: 411–18 [DOI] [PubMed] [Google Scholar]
- 18.Barlow DH. Anxiety and its disorders. Chapter 5: Provoking panic in the laboratory. New York: The Guildford Press, 2004 [Google Scholar]